Osteoporosis
The most common bone disease
Characterized by:
• reduced bone density
• micro-architectural deterioration of bone tissue
• increased risk of fractures
The risk of osteoporosis increases markedly with age

Pathogenesis of osteoporosis
• In normal individuals, bone mass increases during skeletal growth to reach its peak at 20
– 40 years of age, and starts to fall thereafter.
• Bone remodeling (formation and resorption) is responsible for renewal and repair of
skeleton in adult life.
• Osteoporosis can occur because of a defect in attaining peak bone mass and/or because
of accelerated bone loss (bone resorption exceeding bone formation).
Bone remodeling
o It starts with attraction of osteoclast precursors from the peripheral blood to the target
sites.
o Osteoclast precursors express RANK (receptor activator of nuclear factor κB). Osteocytes
contain RANK ligand (RANKL) that activates the RANK on osteoclast precursors to
differentiate into mature osteoclasts.
o Bone formation follows with attraction of osteoblast precursors to the resorption site.
Pathogenesis of osteoporosis
• Postmenopausal osteoporosis
• Age related (senile) osteoporosis
• Osteoporosis in men
• Secondary osteoporosis
• Corticosteroid-induced osteoporosis
Postmenopausal osteoporosis
There is an accelerated phase of bone loss after menopause.
Postmenopausal bone loss is caused by oestrogen deficiency, which naturally stimulates bone
formation
Postmenopausal osteoporosis is caused by a combination of low peak bone mass and
exaggerated postmenopausal bone loss.
Individual differences in the development of postmenopausal osteoporosis are due to certain
additional factors:

• Genetic factors: account for 80% of the population variance of the risk of osteoporosis
• Environmental factors:
– exercise and calcium intake during growth
– smoking increases the risk of postmenopausal osteoporosis
– alcoholism is a recognized cause of osteoporosis
age related osteoporosis
• Gradual bone loss occurs with advancing age in both genders.
• Bone resorption is not particularly increased, but bone formation is reduced.
• The genetic and environmental factors are also responsible for the individual variation
in age related osteoporosis
Osteoporosis in men
• Osteoporosis is less common in men than in women.
• A secondary cause is identified in 50% of cases, most importantly hypogonadism,
corticosteroid treatment and alcoholism.
• The mechanism of hypogonadism-induced osteoporosis is similar to postmenopausal
osteoporosis
• In the remaining 50% of men, genetic susceptibility is probably responsible.
Secondary osteoporosis
Osteoporosis occurring as a complication of diseases or drug treatment
• Endocrine diseases: hypogonadism, hyperparathyroidism, thyrotoxicosis, Cushing's
syndrome
• Inflammatory diseases: rheumatoid arthritis, inflammatory bowel disease
• Drugs: corticosteroid, thyroid hormones, anticonvulsants and heparin
• GIT diseases: malabsorption, chronic liver disease
• Miscellaneous: anorexia nervosa, multiple myeloma, immobilization

Corticosteroid induced osteoporosis
• Corticosteroid therapy is an important cause of osteoporosis.
• Corticosteroids also directly inhibit osteoblast activity and stimulate their apoptosis.
• The risk is directly related to the dose and duration of treatment.
• Osteoporosis is less likely with inhaled corticosteroids and when corticosteroid dose is
less than 5 mg prednisolone per day.
• The risk is substantial when the dose exceeds 7.5 mg for more than 3 months.
Clinical features of osteoporosis
• Asymptomatic until fracture occurs
• Fractures due to bone fragility are the most common manifestation.
• Back pain, height loss, kyphosis and discovery of radiological osteopenia during
evaluation for other conditions are also important.
• Osteoporotic fractures can affect any bone but the most common sites are the forearm
(Colles fracture), spine (vertebral fractures) and femur (hip fracture).
Investigations
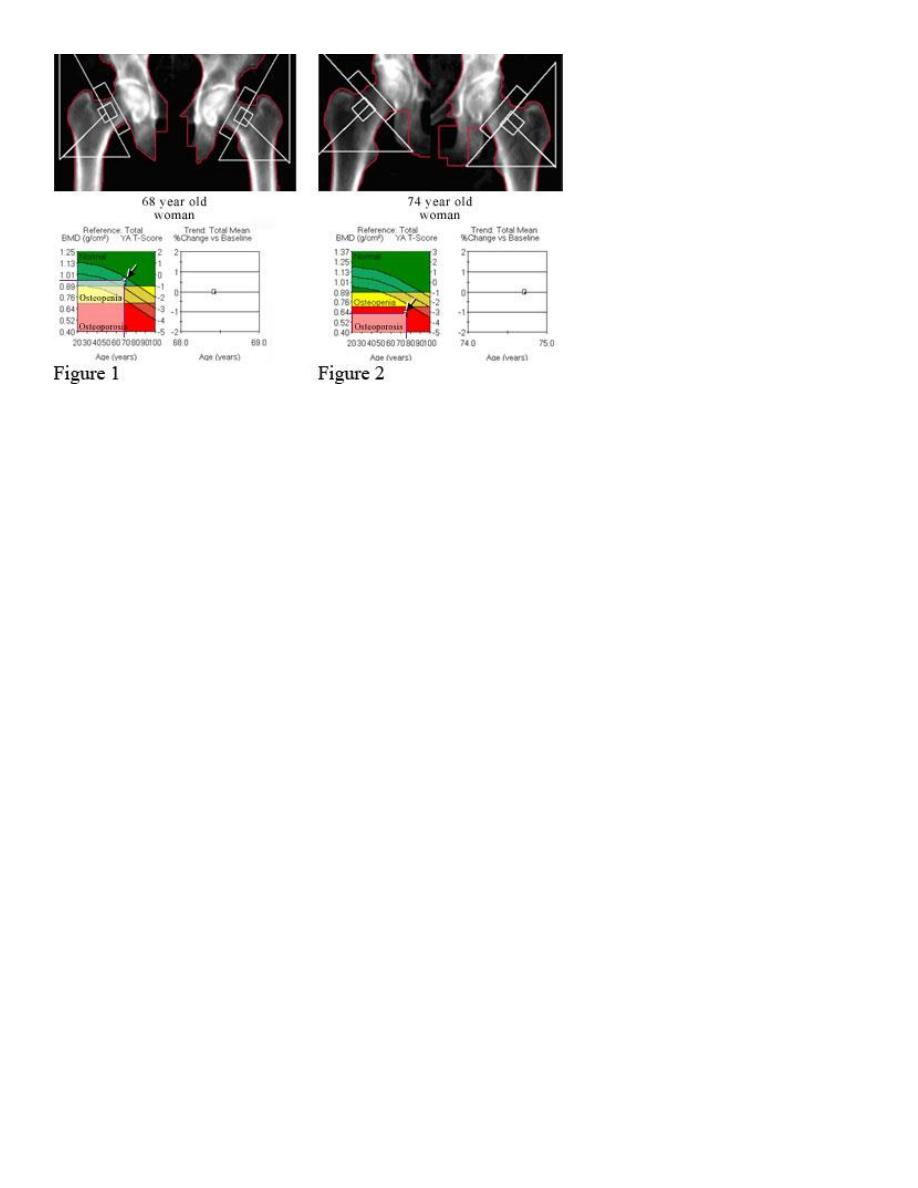
• Diagnosis of osteoporosis requires the measurement of bone mineral density (BMD).
• The preferred technique is dual energy X ray absorptiometry (DEXA) of the hip and spine
• The machine gives the result of T-score and Z-score.
Dual energy X ray absorptiometry
• T-score measures how many standard deviations (SD) the patient BMD differs from that
of a healthy control
• Z-score measures how many SD the BMD of the patients differ from that of an aged
matched control.
T-score: - 2.5 or below indicates osteoporosis between – 1.0 to – 2.5 is considered
osteopenia. Values above - 1.0 are considered normal
Indications BMD measurement include:
• low trauma fractures
• height loss and kyphosis
• osteopenia on X ray
• corticosteroid therapy
• family history of osteoporosis fracture
• BMI< 18
• menopause <45
• diseases causing osteoporosis
• high FRAX score
Osteoporosis : cause identification
• History should be taken to identify causes as early menopause, smoking, alcohol intake
and steroid therapy.
• Clinical examination should search for endocrine disorders, multiple myeloma or
inflammatory diseases.
• Routine investigations

• Sex hormones and gonadotropines should be assessed in men with osteoporosis and in
women with amenorrhoea before 50.
Management of osteoporosis
Patients with osteopenia are advised on life style modification including:
• smoking and alcohol cessation
• increasing dietary calcium
• encouragement of exercise
Indications for drug therapy
1. T-score below -2.5
2. Corticosteroid induced osteoporosis with T-score below -1.5
3. Vertebral fractures irrespective to BMD
Bisphosphanates
• The most commonly prescribed drugs for osteoporosis.
• Synthetic pyrophosphate analogues that adsorb on bone surface and inhibit osteoclast
function.
• Increase in BMD of 5 – 8 % after 2 years of therapy.
• Alendronate (70 mg/week) and risedronte (35mg/week) are the most commonly
prescribed oral bisphosphanates. Zolendronic acid (5mg IV annually) is also effective
• These drugs prevents postmenopausal bone loss and reduces the risk of vertebral and
non-vertebral fractures. Bisphosphanates are also effective in the prevention and
treatment of corticosteroid induced and male osteoporosis.
• Oral bisphosphanates are poorly absorbed from the GIT and should be taken on empty
stomach, with plain water only, avoiding food for 30-45 min. after being swallowed.
• Dyspepsia is a recognized side effect, and they should be prescribed cautiously in
patients with GERD and avoided in those with oesophageal stricture or achalasia.
• Osteonecrosis of the jaw (rare) and influenza like illness (with zolendronic acid) are
other side effects

Calcium and vitamin D supplement
• Calcium in a dose of 500 mg/day, and vitamin D in a dose of 800 unit/day are adjunctive
to other treatments.
• Monotherapy with calcium and vitamin D prevents fragility fracture in those with
vitamin D deficiency, but not in other patients.
Hormone replacement therapy (HRT)
• HRT prevents postmenopausal bone loss and reduces the risk of osteoporotic fractures.
• The use of HRT as a treatment of osteoporosis has markedly reduced after confirming
the excess risk of breast cancer, thromboembolism, stroke and CHD.
• Testosterone is indicated for male osteoporosis caused by hypogonadism.
Follow up after treatment
• Monitoring response to treatment is ideally made by repeating BMD measurement or
by measuring markers for bone turnover (like N-telopeptide) in serum or urine
• Second assessment of BMD is made after 2 – 3 years of treatment because of the slow
effect of antiresorptive therapy
