Seminar
Interpretation of abnormal liver enzymes
Liver Enzymes :
-Aminotransferases
AST (SGOT)
ALT (SGPT)
-Alkaline phosphatase
-Gamma glutamyl transpeptidase
Synthetic function
-Albumin
-Prothrombin time
-Bilirubin
History
-The use of or exposure to any chemical or medication (including
prescription and over-the-counter medications as well as herbal
therapies)
-The duration of LFT abnormalities
-The presence of any accompanying symptoms such as jaundice,
arthralgias, myalgias, rash, anorexia, weight loss, abdominal pain, fever,
pruritus, and changes in the urine and stool
-Parenteral exposures including transfusions, intravenous and intranasal
drug use, tattoos, and sexual activity.
-Recent travel history, exposure to people with jaundice, exposure to
possibly contaminated foods, occupational exposure to hepatotoxins,
and alcohol consumption.
Physical Examination
-Temporal and proximal muscle wasting suggest longstanding diseases
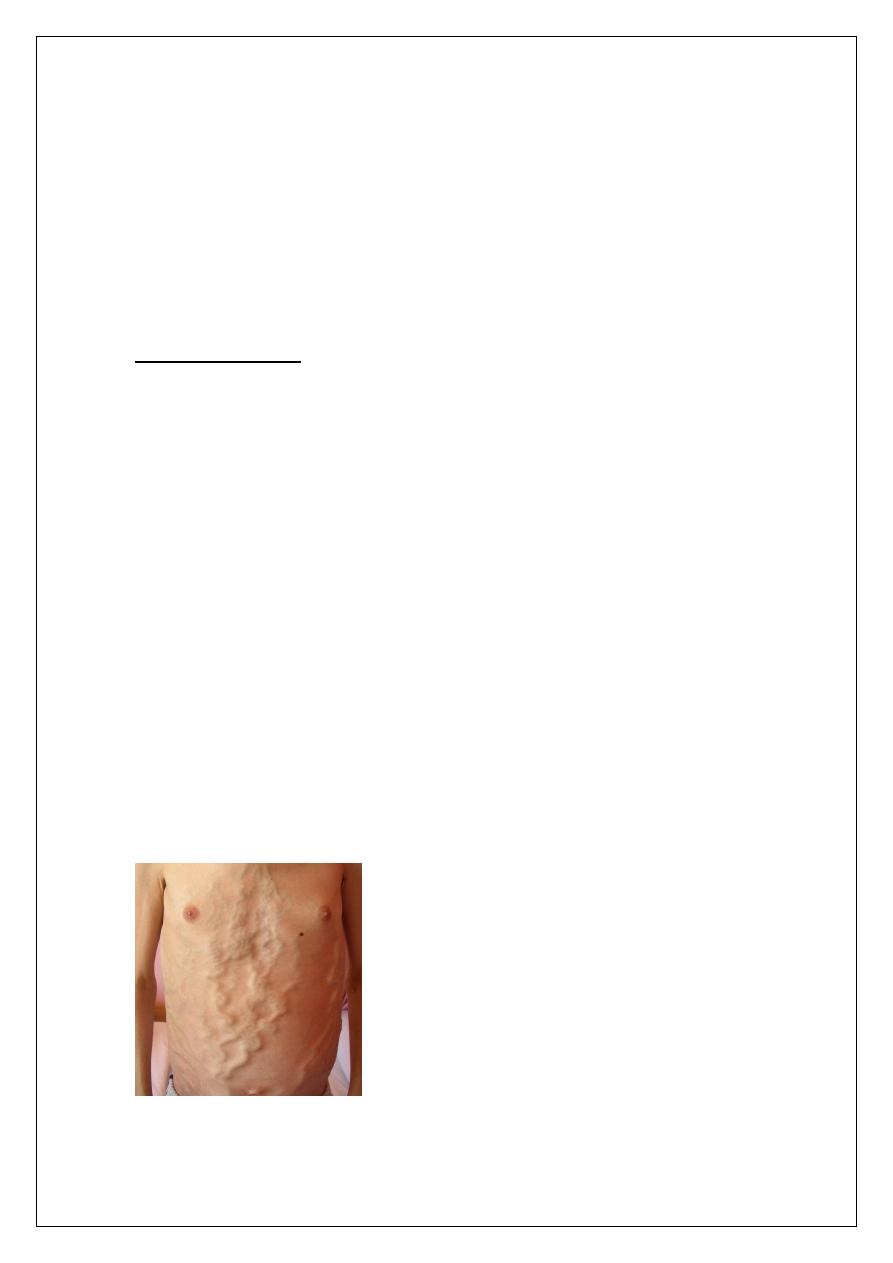
-Stigmata of chronic liver disease include spider nevi, palmar erythema,
gynecomastia, caput medusae Dupuytren's contractures, parotid gland
enlargement, and testicular atrophy
-Enlarged left supraclavicular node (Virchow's node) or periumbilical
nodule (Sister Mary Joseph's nodule) suggest an abdominal malignancy
-Jugular venous distension, a sign of right sided heart failure, suggests
hepatic congestion
Laboratory testing :
Patterns predominantly reflecting hepatocellular injury :
– Increase in AST and ALT
Patterns predominantly reflecting cholestasis :
– Increase in Alkaline phosphatase and GGTP
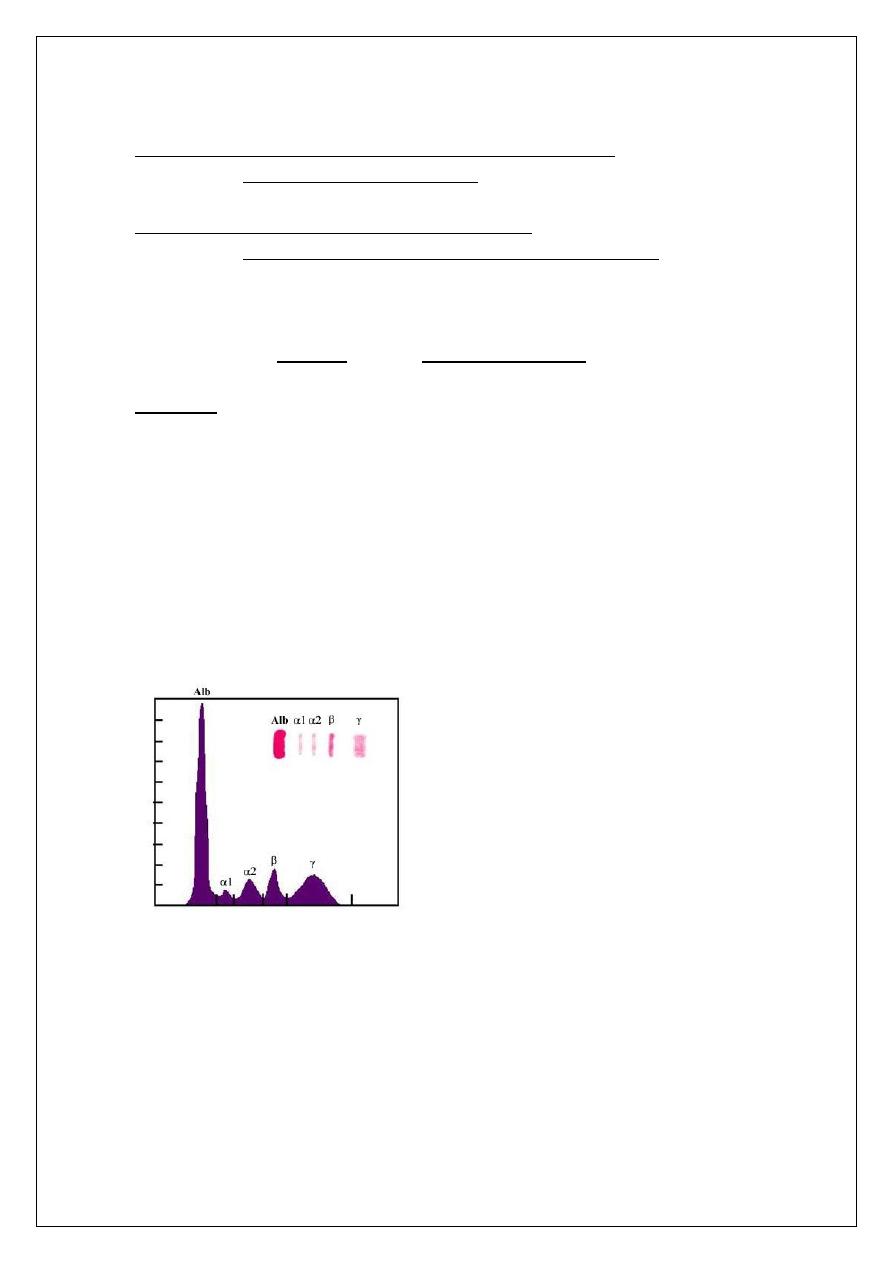
1-Serum Proteins
-The liver is the major site at which serum proteins are synthesized.
-These include albumin and the coagulation factors
Albumin :
-Average adult liver synthesizes approximately 15 g per day (200 mg/kg
per day).
-The serum albumin reflects the :
Rate of synthesis
Rate of degradation
Volume of distribution.
-Albumin synthesis is regulated by a variety of influences including :
nutritional status
Serum oncotic pressure
Cytokines, and hormones
-Hypoalbuminemia :
Systemic inflammation
Nephrotic syndrome
Malnutrition
Coagulation factors
-The liver is the major site of synthesis of 11 blood coagulation proteins.
Factor I (fibrinogen)
Factor II (prothrombin)
Factor V
Factor VII
Factor IX
Factor X
Factors XII
Factor XIII
-Prolonged Prothrombin time (PT)
Congenital or Acquired :
-Consumption of clotting factors (such as disseminated
intravascular coagulation or severe gastrointestinal bleeding)
-Certain drugs ( Warfarin)
-Vitamin K deficiency:
Inadequate dietary intake,
Prolonged obstructive jaundice,
Malabsorption
Administration of antibiotics that alter the gut flora.
*(PT typically returns to normal within 24 hours after a single parenteral
injection of vitamin K).
*Poor utilization of vitamin K due to advanced parenchymal liver
disease (Vitamin K supplementation is generally ineffective)
2-Serum Aminotransferases
-Sensitive indicators of liver cell injury.
-ALT and AST < 30 - 40 IU/L
-ALT levels are normally higher in
Men
Vary directly with body mass index
Serum lipid levels.
Elderly
Infants
? Race
-ALT levels are normally lower in
Consumption of coffee and especially caffeine
Renal Failure
-Correlate poorly with the magnitude of liver injury
-Elevated in most liver diseases.
-Extensive hepatocellular injury
Acute viral hepatitis
Shock liver (ischemic hepatitis)
Acute drug- / toxin-induced liver injury
3-Alkaline Phosphatase
-Found in many locations throughout the body
-Its precise function is not yet known
-Derived from three sources: liver, bone, and the intestinal tract.
-Retained bile acids appear to play a central role leading to increase
synthesis in the liver followed by direct release into the circulation.
-Level varies with age and gender
Higher in men than in women
Children elevated in both sexes, correlates well with the rate of
bone growth
Adolescent males may reach mean values three times greater than
in normal adults
Enzyme activity in serum may double late in normal pregnancy,
primarily because of influx from the placenta
4-Gamma-Glutamyl TransPeptidase
-Present in cell membranes in many tissues, including the kidneys,
pancreas, liver, spleen, heart, brain, and seminal vesicles.
-Serum GGT and alkaline phosphatase correlate reasonably well.
-Elevation in GGT is not completely specific for hepatobiliary disease.
-High GGT values are found in people who take medicines such as
barbiturates or phenytoin or ingest large quantities of alcohol
Caput Medusae
Case 1:
-Abnormal liver enzymes for > 6 months
AST 80
ALT 110
-Alkaline phosphatase, GGTP and Bilirubin WNL
-Mild chronic elevation of serum transaminases
Answer :
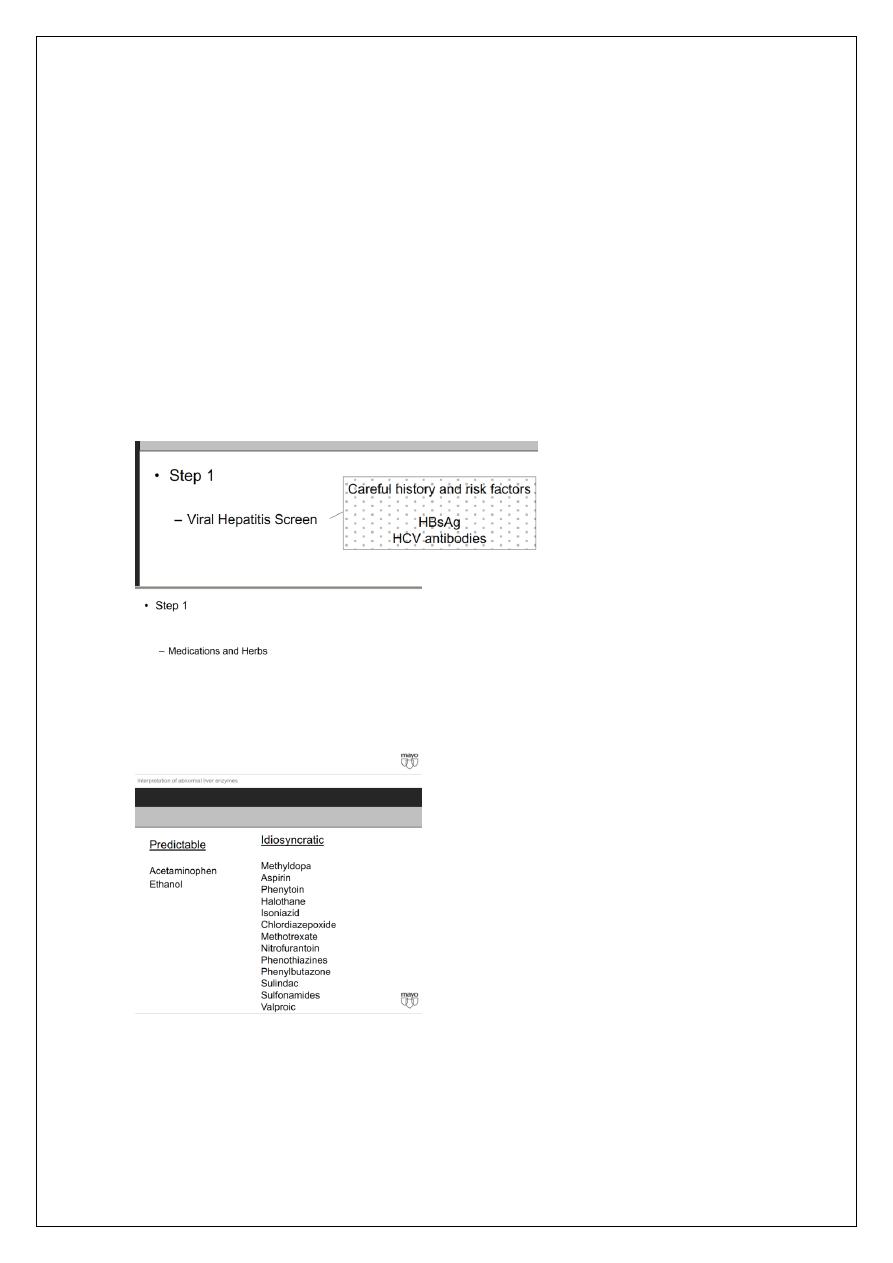
Step 1
Viral Hepatitis Screen
Medications and Herbs
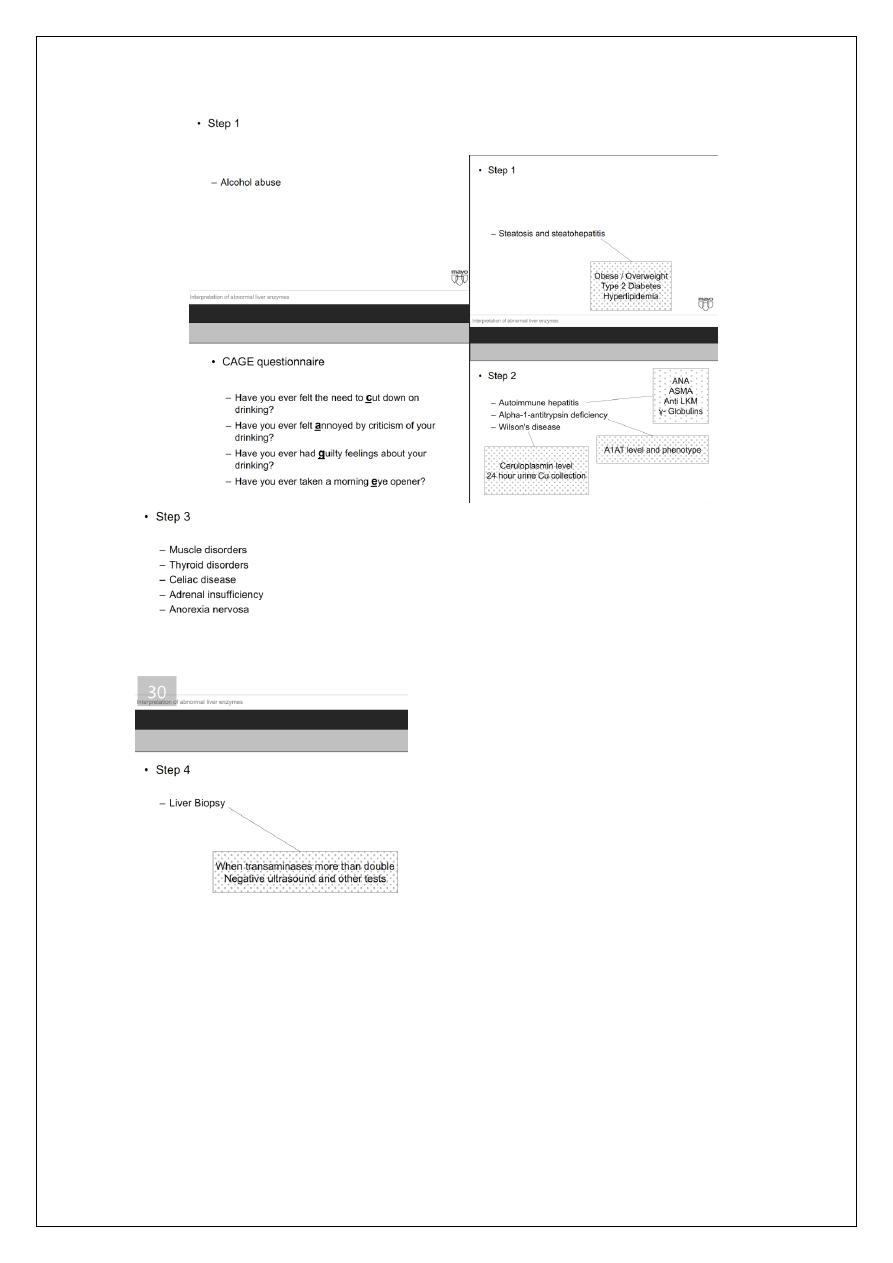
Alcohol abuse
Steatosis and steatohepat
itis
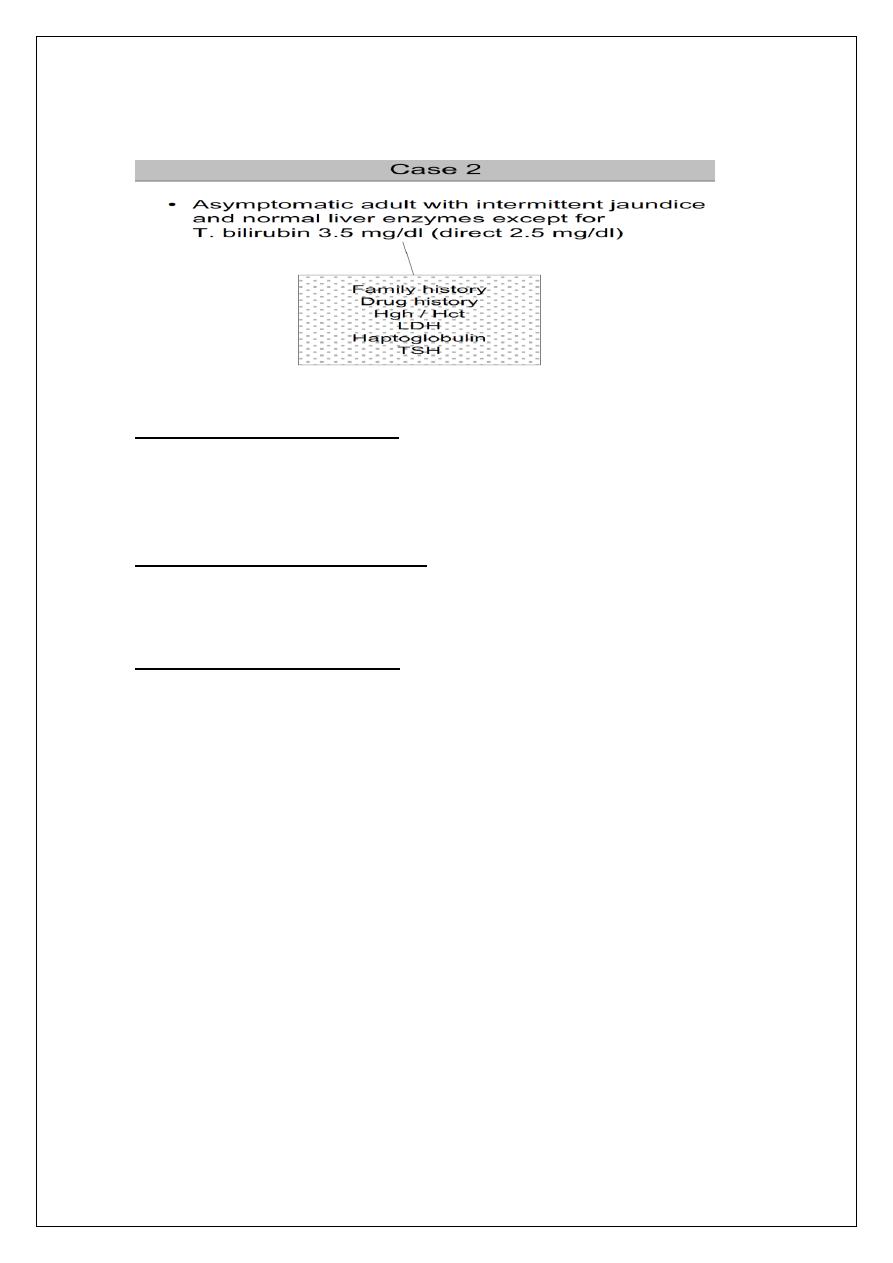
Case 2 :
Unconjugated hyperbilirubinemia :
Increased bilirubin production
Extravascular hemolysis
Extravasation of blood into tissues
Intravascular hemolysis
Dyserythropoiesis
Impaired hepatic bilirubin uptake
Congestive heart failure
Portosystemic shunts
Certain drugs - rifampin, probenecid flavaspadic acid, bunamiodyl
Impaired bilirubin conjugation
Crigler-Najjar syndrome type I and II
Gilbert's syndrome
Hyperthyroidism
Liver diseases - chronic persistent hepatitis, advanced cirrhosis,
Wilson's disease
Crigler Najjar :
-Crigler Najjar type I
– Exceptionally rare condition found in neonates
– Characterized by severe jaundice (bilirubin >20 mg/dL)
– Neurologic impairment due to kernicterus.
-Crigler-Najjar type II
– More common than Type I and can live into adulthood
– Bilirubin levels that range from 6 to 25 mg/dL.
– Bilirubin UDP glucuronosyl transferase activity is typically
reduced.
– Bilirubin UDP glucuronosyl transferase activity can be induced by
the administration of phenobarbital, which can reduce serum
bilirubin levels in these patients.
Gilbert's syndrome
-Affects approximately 3 - 7 % of the population
-Males > females (2 : 7)
-Reduced bilirubin UDP glucuronosyl transferase activity.
-Mild unconjugated hyperbilirubinemia with serum levels almost
always less than 6 mg/dL.
-The serum levels may fluctuate and jaundice is often identified only
during periods of illness or fasting.
Case 3
-AST 1200
-ALT 1450
-Bilirubin 9.5 mg/dl (direct 6 mg/dl)
-Alkaline phosphatase 230 mg/dl
*Predominantly hepatocellular pattern with jaundice
*possible causes:
Viral hepatitis
Hepatitis A, B, C, D, and E
Epstein-Barr virus
Cytomegalovirus
Drugs
Predictable, dose-dependent (eg, acetaminophen)
Unpredictable, idosyncratic (many drugs)
Environmental toxins
Vinyl chloride
Jamaica bush tea - pyrrolizidine alkaloids
Wild mushrooms - Amanita phalloides or verna
Autoimmune hepatitis
Wilson's disease
Case 4
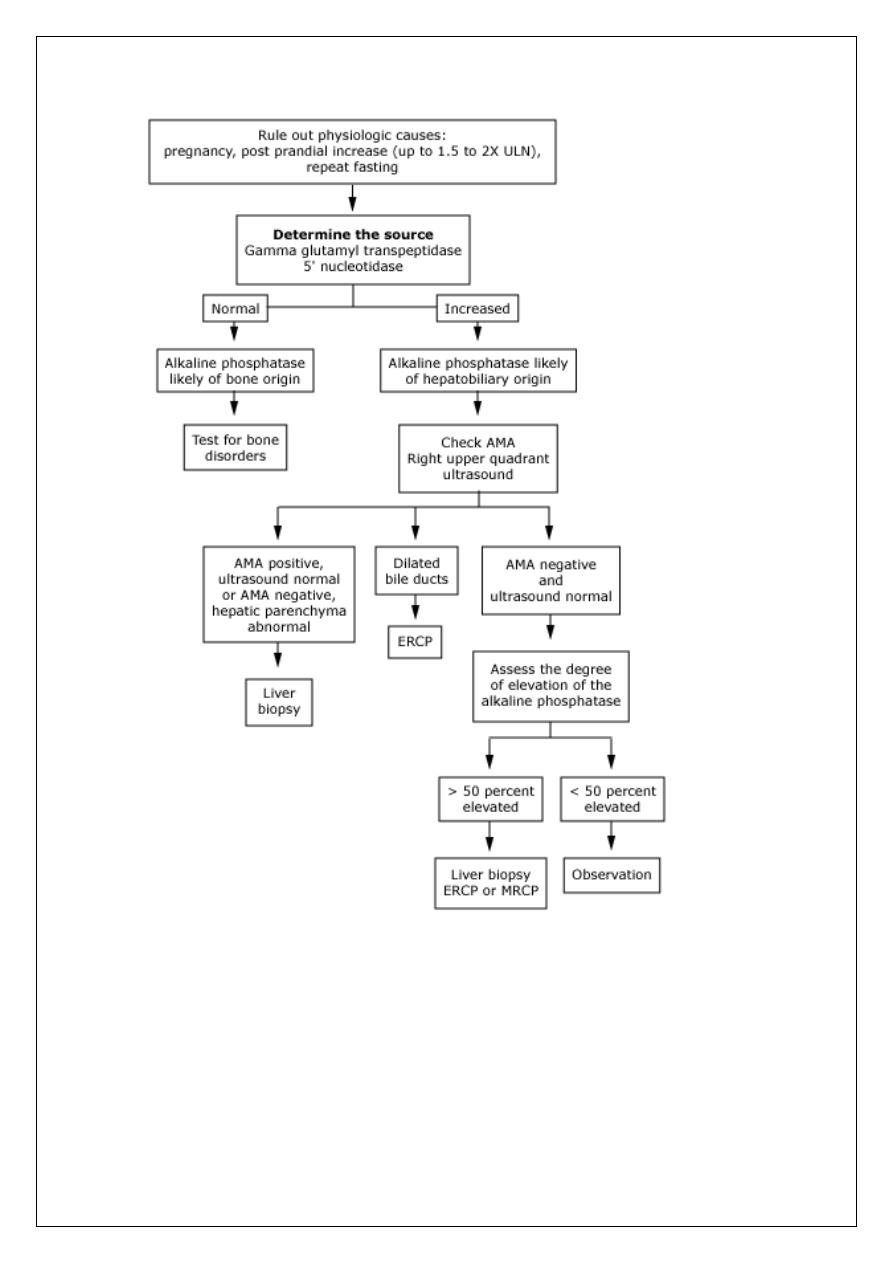
-Isolated elevation of the alkaline phosphatase and/ or GGTP
-possible causes :
Partial bile duct obstruction
Primary biliary cirrhosis (PBC)
Primary sclerosing cholangitis,
Drugs such as androgenic steroids and phenytoin.
Infiltrative diseases include sarcoidosis, other granulomatous diseases
Unsuspected cancer metastatic to the liver.
فعطرها بما تحب, ىركذ تنا نوكتس ام اموي
