1
diagnosis of epilepsy and related disorders
Introduction
• Epilepsy is one of the most common and disabling public health problems, affecting
approximately 50 million people around the world.
• The initial diagnostic approach to the patient with epilepsy and related episodic
disorders has importance for both long-term prognosis and treatment, including the
determination of whether treatment is necessary and the type(s) of therapy to be
considered.
• When evaluating a patient with possible epilepsy, the basic approach is as follows:
1. Is this epilepsy?
2. is it focal or generalized?
3. Is there is any underlying cause or Is it an epileptic syndrome?
• The basic goals of treatment for epilepsy are to help the patient achieve seizure
freedom without adverse effects of therapies, or at least minimize the frequency of
seizures with minimal adverse effects and to maximize quality of life for people with
epilepsy.
PRACTICAL DEFINITION OF EPILEPSY
• Seizures are sudden but transient behavioral, sensory, motor, or visual symptom or
sign, and caused by abnormal excessive cortical neuronal activity.
• Seizures may occur spontaneously without provocation or may be provoked by
certain influences (eg, brain trauma, hemorrhage, metabolic dyscrasias, or drug
exposures).
• In 2014, a new practical definition for epilepsy as a disease with
recurrent unprovoked seizures (ie, two or more unprovoked seizures occurring at least 24
hours apart)
CLASSIFICATION OF SEIZURES
• 1-Partial seizures
• a. Simple partial seizures (with motor, sensory, autonomic, or psychic signs)
• b. Complex partial seizures
2
• c. Partial seizures with secondary generalization
• 2. Primarily generalized seizures
• a. Absence (petit mal)
• b. Tonic-clonic (grand mal)
• c. Tonic d. Atonic
• e. Myoclonic
DIFFERENTIAL DIAGNOSIS OF SEIZURES AND RELATED EPISODIC DISORDERS
• The differential diagnosis of epilepsy is wide, since several paroxysmal disorders may
closely mimic an epileptic seizure.
• Non epileptic spells can be divided into two basic categories, physiologic and
psychogenic.
Non-neurologic Differential Diagnosis
• The most common non-neurologic disorder mimicking epilepsy is syncope.
• Syncope most frequently results from:
• Vasovagal syncope is the most common of these and is a generally benign form of
syncope characterized by prodromal subjective symptoms of lightheaded dizziness,
diaphoresis, and nausea, often provoked by triggers such as positional change,
Valsalva maneuvers (eg, lifting, toileting), physical triggers or strong emotional
triggers (eg, the sight of blood).
• Cardiogenic causes of syncope result from bradyarrhythmia or tachyarrhythmia.
• Orthostatic hypotension results from a fall in blood pressure following a positional
change to standing from a recumbent position and is a frequent cause of syncope in
patients who are elderly or diabetic with autonomic neuropathy.
• Loss of consciousness is often brief, lasting seconds to a few minutes. Convulsive-like
movements are frequent during syncopal attacks, leading to further diagnostic
confusion with epilepsy. Confusion and loss of continence following recovery of
consciousness are infrequent compared to epileptic seizures.

3
Neurologic Differential Diagnosis
• Several paroxysmal neurologic disorders can be confused with epilepsy, including:
Cerebrovascular disease
TIAs typically last from minutes to 1 hour, although prolonged TIAs are likely to show
radiographic evidence for infarction. Cerebrovascular disorders more frequently cause
“negative” symptoms, such as numbness, weakness, visual loss, or aphasia, compared to
epileptic seizures. Epileptic seizures more often involve “positive” symptoms and signs
during the ictal event.
Delirium
is a state of generalized confusion occurring when a vulnerable patient with an underlying
mild cognitive impairment or dementia is subjected to a procedure; change in medication;
infection, inflammation, or metabolic disturbance.
delirium may closely resemble ictal or postictal behavior associated with a complex partial
seizure, involving staring with disorientation, inattention, and variable responsiveness.
Encephalopathic patients may also have acute symptomatic seizures resulting in further
diagnostic confusion.
Migraine
Clinical manifestations of migraine and epilepsy are often similar, involving visual, sensory,
and cognitive symptoms. Migrainous headaches often
follow epileptic seizures, and seizures following a primary migraine may occur. During a
migraine attack.
Movement disorders
Movement disorders, including paroxysmal dystonias and dyskinesias and some tremor
disorders, may also resemble epileptic seizures.
Careful observation of clinical phenomenology is necessary to distinguish these episodes
from seizures also EEG is invariably normal during subcortically generated movement
disorders.
Sleep disorders
Nocturnal events confused with sleep epilepsies include the non-rapid eye movement
(REM) parasomnias (disorders of arousal) and REM sleep behavior disorder.
Non- REM parasomnias involve a spontaneous arousal from non-REM sleep, with
nonstereotyped confused behavior with or without vocalization or sleepwalking behavior.
4
REM sleep behavior disorder is characterized by complex motor behavior paralleling scary
dream content, they may injure themselves or a bed partner by punching, kicking, or falling
out of bed.
In distinction, nocturnal seizures demonstrate highly stereotyped complex motor behavior,
frequently with oral, limb, or trunk automatisms.
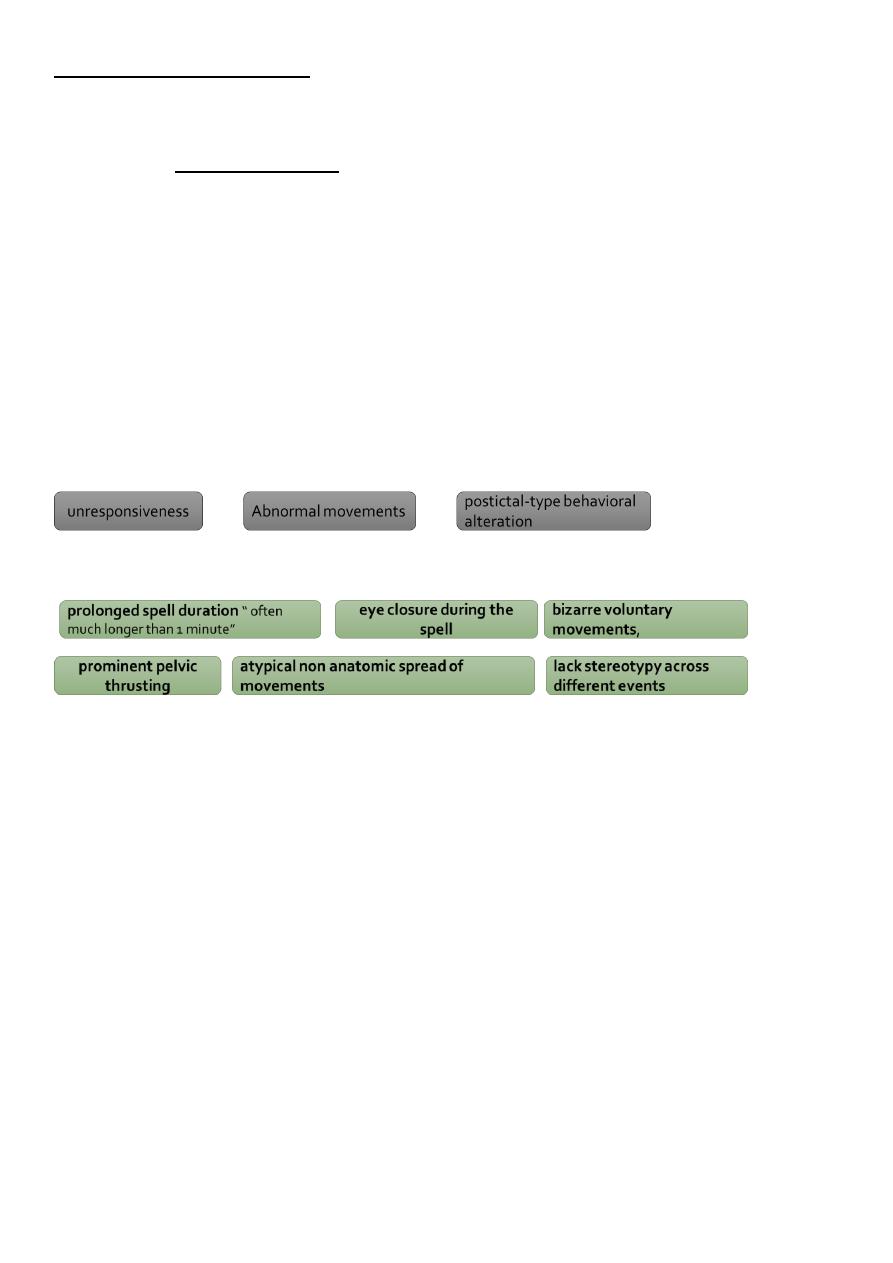
Psychogenic nonepileptic seizures (PNES)
• are frequent sources of confusion with epileptic seizures. PNES are behavioral events
closely resembling epileptic seizures but lacking the typical clinical and
electrophysiologic features of true epilepsy.
• PNES are especially common presentations in epilepsy monitoring unit practices,
accounting for 30% to 50% of admissions and Ictal video-EEG is the gold standard for
diagnosis.
• PNES resembles true epileptic seizures by:
• However, PNES can be distinguished by:
INVESTIGATION OF THE PATIENT WITH SEIZURES AND SPELLS
• Investigations with EEG and neuroimaging is essential to consider in the evaluation of
most patients presenting with seizures or spells and is an expected consideration
within the American Academy of Neurology (AAN) Epilepsy Quality Guidelines.
• These investigation aim to:
1. Diagnosis of epilepsy and possible underlying cause.
2. Diagnosis of epilepsy syndrome.
3. help determine the prognosis for future seizure recurrence.
Electroencephalography
• The EEG is the most commonly performed diagnostic study in people with epilepsy.

5
• The AAN recommends EEG in diagnosing epilepsy in adults and children, with
inclusion of photic stimulation, hyperventilation, and sleep deprivation in adults as
part of the protocol
• An epileptiform pattern seen on EEG after a first-time seizure often predicts
recurrence range from 30% to 70% in the first year.
• Therefore, when the EEG shows an epileptiform discharge after a single seizure,
treatment may be considered even before a diagnosis of epilepsy is established.
heightened tendency toward recurrent unprovoked seizures (ie, a single seizure,
accompanied by evidence from clinical, electroencephalographic, or neuroimaging
tests that a heightened risk [at least 60%] exists for future seizures over the next 10
years)
• The clinical applications of EEG include:
1. diagnosis of epilepsy.
2. selection of AED therapy.
3. evaluation of response to treatment.
4. determination of candidacy for drug withdrawal.
5. surgical localization.
Sensitivity and specificity
The sensitivity of a single EEG study to record an epileptiform abnormality may be 50% or
less in people with epilepsy. The diagnostic yield increases to 80% to 90% if three or more
serial EEGs are performed. Patients with childhood epilepsy are more likely to have
abnormal epileptiform EEG recordings than adults.
Simple facts
1. Normal interictal EEG studies do not exclude the presence of a seizure disorder.
Ultimately, epilepsy is a clinical diagnosis and the EEG serves to provide supporting
evidence; in other words, you treat the patient and not the EEG.
2. Interictal epileptiform discharges are seen rarely in adults or children without
epilepsy (0.2% to 3%).
3. The presence of an epileptiform abnormality does not always indicate a seizure
disorder. Occipital spikes have been observed in blind people, and generalized spikes

6
have been reported in relatives of patients with genetic generalized epilepsies or in
certain drugs like bupropion, cefepime, clozapine, lithium, and tramadol or in
metabolic disorders like uremia.
Limitations
Physiologic barriers
to recording the EEG include CSF, dura, bone, and scalp, and these noncerebral tissues
intervening between the brain’s surface and recording electrodes produce a marked
attenuation of spontaneous cortically generated EEG activity.
Physiologic changes
associated with head movement, tremor, eye opening and closure, sweating, nystagmus,
and myogenic activity may be difficult to differentiate from epileptiform discharges.
Technical
The EEG study is usually brief, approximately 20 to 40 minutes, and may fail to identify
epileptiform alterations in people with epilepsy.
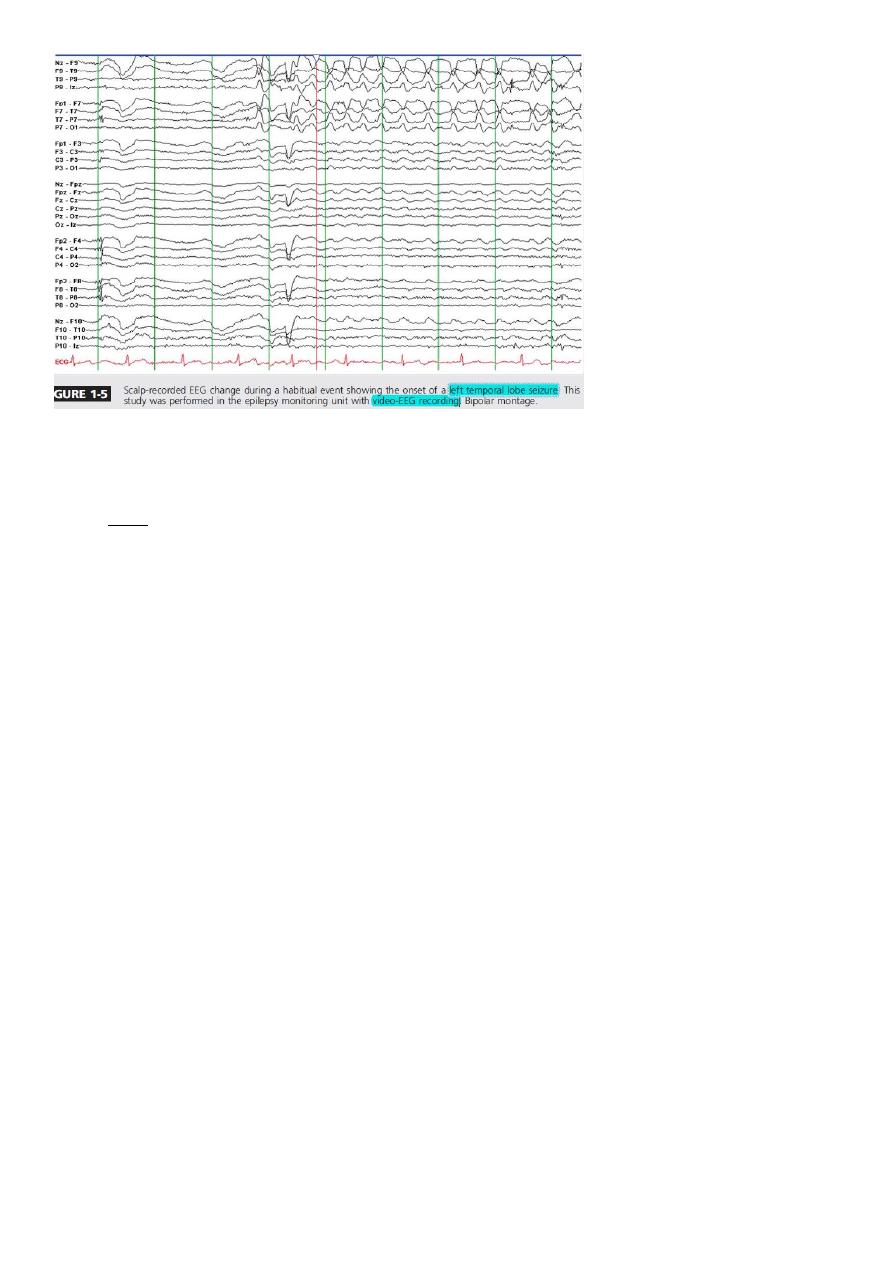
Video-Electroencephalography Recordings
• Video-EEG monitoring may be used to evaluate patients with presumed seizure
disorders.
• Uses:
1. Evaluation of spells weather it is true epileptic seizure or psychogenic non epileptic
event also 10-15% of patients with psychogenic events have coexistent seizure
disorders.
2. classification of seizures,
3. quantification of seizures,
4. assessment of seizure precipitating factors,
5. surgical localization in drug-resistant focal epilepsy.
7
Limitations:
• first The cost effectiveness of video-EEG monitoring as a diagnostic tool is more
difficult to assess than is the relevant information obtained using these studies.
Magnetic Resonance Imaging
• MRI is used for identification of the pathologic findings associated with focal or
generalized seizures, localization of the epileptogenic zone, and determination of
surgical localization in drug-resistant focal epilepsy.
• MRI is the structural neuroimaging procedure of choice in people with epilepsy.
• All individuals with seizures should undergo an MRI study unless
1. the patient has a confirmed genetic generalized epilepsy syndrome (eg, childhood
absence epilepsy)
2. or a contraindication exists that does not permit this imaging procedure to be done
safely.
• Even individuals with single seizure episodes may benefit from an MRI study because
29% of these patients may have abnormal imaging.
• he optimal MRI technique in adult patients with focal seizures includes use of a 3-
tesla study in the coronal or oblique-coronal, axial, and sagittal planes using T1-
weighted, T2-weighted, and fluid-attenuated inversion recovery (FLAIR) sequences.
MRI epilepsy protocols should include a three-dimensional (3-D) T1-weighted
volumetric acquisition with isotropic voxel size of 1 mm or 1.5 mm to enable the
reconstruction of images in any plane.
8
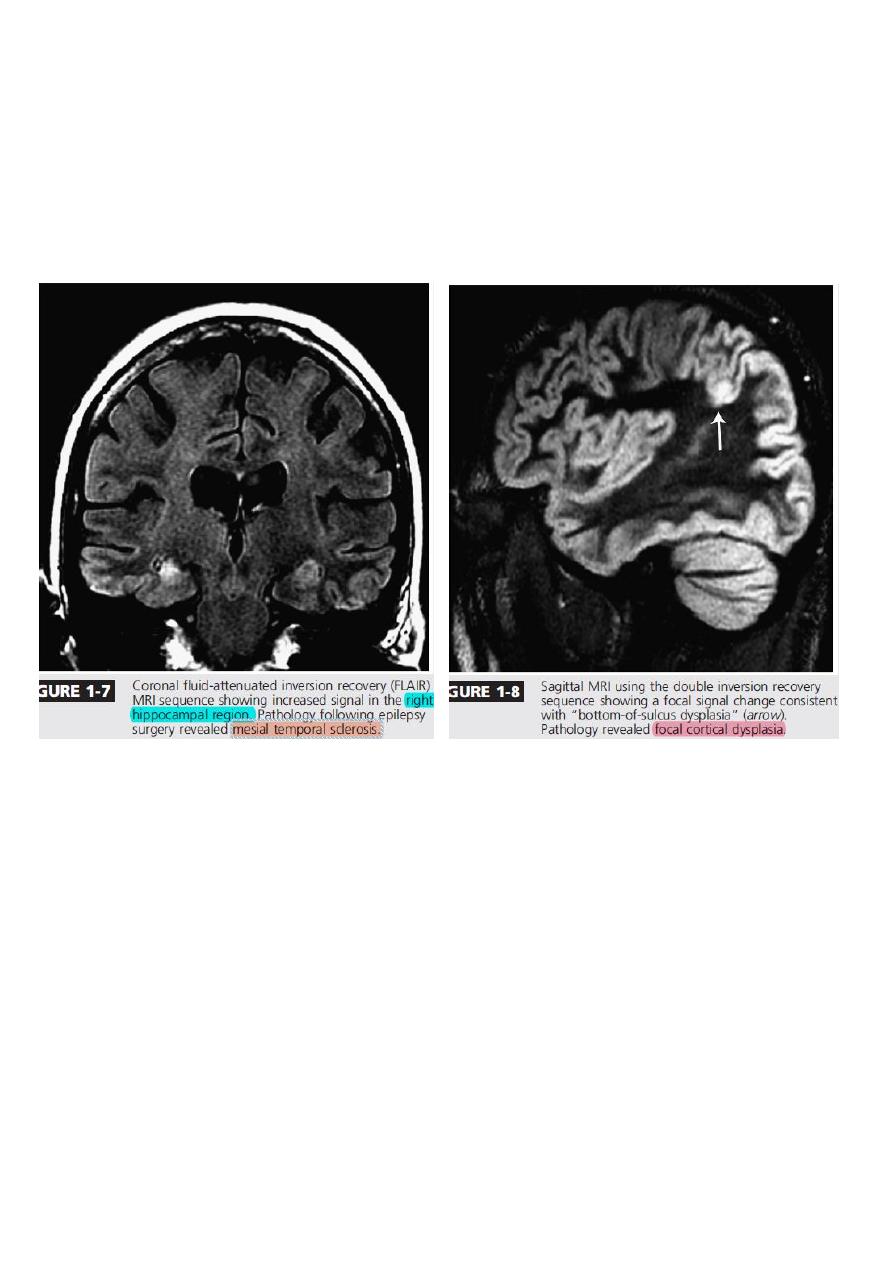
• FLAIR imaging sequences have shown an accuracy of 97% for detecting abnormalities
associated with mesial temporal sclerosis defined on histopathology (Figure 1-7),
while more sophisticated methods of image reconstruction from 3-D acquisitions
allow a better evaluation of patients with discrete structural lesions (eg, focal
cortical dysplasia) (Figure 1-8).
