Introduction
Unpleasant sensory & emotional experience associated with actual or potential tissue damage or described in terms of such damage.”• What is Pain ?
How do we feel pain?
• Specialized receptors = free nerve endings• Stimulation
• Mechanical damage
• Extreme temperature
• Chemical irritation
• Two types of neurons
• A-delta: first pain, sharp
• C: second pain, dull
Pain
How do we feel pain ?
• Four distinct processes• Transduction
• Transmission
• Modulation
• Perception
Pain
Pain classification
• Origin of pain• Nociceptive pain
• Result of mechanical, thermal or chemical
• Subdivided into
• Somatic
• Visceral
• 2) Neuropathic pain
• PNS
• CNS
• Duration of pain
• Chronic
• Acute
• Other types of pain
• Projected pain
• Referred pain
• Phantom pain
Pain
Pain
• Phantom pain:• Pain coming from a body part that's no longer exist
• Used to be considered a psychological problem, but now is recognized as real sensations originate in the spinal cord & brain
• Projected Pain:
• Pain felt at peripheral ends of nerve, while stimulus occurred along the course of that nerve.
• Example: pain in TMJ sensed as pain in ear
• Referred pain:
• Pain felt in an area distant from that in which the causative pathology is located
• Example: angina pectoris sensed as pain over the left side of the mandible / pain in lower teeth felt in upper teeth
Pain and anxiety are two sides of the same coin.
Pain & anxiety• Pain can cause a person to be anxious, and an anxious patient is likely to experience more pain than a patient who is not anxious.
• Therefore interventions that modulate anxiety reduce pain. Defining anxious patient and do the necessary to reduce its anxiety is a mean part of pain management
History &
examinationWhen investigating acute dental pain, the history should focus on the pain's:
Location
type
frequency and duration
Onset
exacerbation and remission (for example the response to heat or cold)
Severity
area of radiation.
Current Medications
History of Allergies
Associated pathology and
referred pain should also be considered.
What are structures that need to be examined ?
TongueBuccal mucosaFloor of the mouthHard palateTeeth and periodontal tissuesTonsils
Temporomandibular joints
Airway
Ears
Salivary glands
Lymph nodes.
History &
examination
The following structures need to be examined carefully in order to be sure that the pain is of dental origin:
Which tests can assist in diagnosis?
There are several simple tests that may assist in diagnosis of dental pain.Dry ice, or an ordinary ice stick (made in a plastic or glass tube), is placed on the cervical third (neck region) of the tooth crown. A response to the stimulus indicates that the pulpal tissue is capable of transmitting nerve impulses. No response may indicate pulp necrosis.
History &
examination
Pulp sensitivity test
Using an instrument handle, the tooth is tapped in the longitudinal axis. A painful response suggests possible periapical inflammation
Placing a fine, blunt probe gently into the gingival sulcus surrounding the
tooth enables the health of the gingival tissues to be assessed. Bleeding
and/or sulcus depths greater than 3-4 mm indicate gum disease
Percussion test
History &
examination
Probing
Holding a tooth firmly on the buccal and lingual sides between the two instrument handles enables mobility to be assessed. All teeth have a small amount of mobility (<0.5 mm), but visible movement suggests loss of bone support around the root of the tooth.
Careful palpation around the area of concern may reveal tenderness and the type and extent of swelling
Mobility test
Palpation
History &
examination
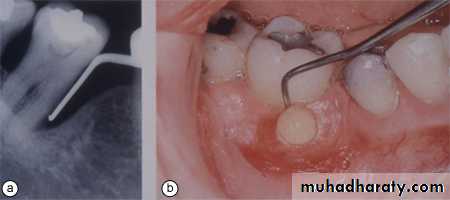
If it is possible to obtain a screening radiograph, such as an orthopantomograph (OPG), this may assist in the diagnosis and localisation of the cause of the pain. The radiograph should show clearly the apical and periapical structures of teeth and associated tissues. The relationship of the maxillary molars and premolars to the floor of the maxillary sinus can be examined, and radiographs may reveal recurrent caries or periapical radiolucencies associated with an established infection.
History &
examination
Radiographic examination
Causes of Oro-facial Pain
Teeth and supporting Tissue DiseaseDisease of the Jaw
Oral mucosal diseases
Pain in the edentulous patient
Pain triggered by mastication
Referred pain
Neurological diseases
Teeth and supporting
tissue DiseasePulpitis
Reversible pulpitis
The pulp is capable of a full recovery if the irritating factors subsided or removed
Signs and symptoms:-
The pain is moderate to sharp.
The pain is of short duration.
The pain does not occur without stimulation.
No mobility or sensitivity to percussion.
Change in the body position do not affect the nature or duration of the pain.
The pain is easily to be localized.
Irreversible pulpitis
Teeth and supportingtissue Disease
The pulp will not recover. The pulp tissue will exhibit a wide spectrum of acute and chronic inflammatory changes.
Signs and symptoms:-
Sharp sever pain on thermal stimulation.
The pain is continuous after the stimuli is removed .
The pain may be spontaneous or continous.
The pain may be exacerbated when the patient lies down.
The pain increases in intensity as a throbbing pressure that can keep the patient awake at night .
The pain is difficult to be localized.
No mobility or sensitivity to percussion.
Teeth and supporting
tissue DiseaseAcute periapical periodontitis
Pain from acute periapical periodontitis should be readily identifiable as there is precisely localised tenderness of the tooth in its socket. Radiographs are of little value in the early stages but useful after sufficient destruction shows itself as loss of definition of the periapical lamina dura.
Acute maxillary sinusitis
Acute maxillary sinusitis can rarely cause similar tenderness of a group of teeth, particularly upper molars
Teeth and supporting
tissue DiseaseLateral periodontal abscess
The tooth is tender in its socket,
It is vital and there is deep localised pocketing.
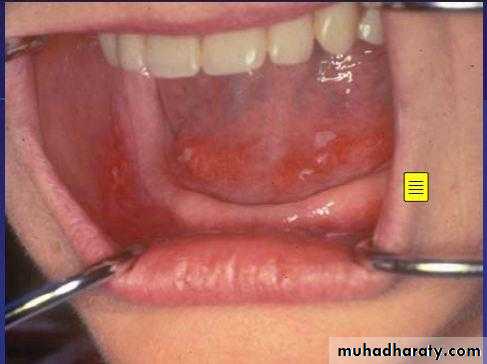
Acute necrotising ulcerative gingivitis and HIV-associated necrotising periodontitis
Acute ulcerative gingivitis usually causes soreness, but when it extends deeply and rapidly, destroying the underlying bone, there may be severe aching pain. In such cases the diagnosis is usually obvious clinically. HIV-associated periodontitis presents a somewhat similar picture and is acutely painful.
Oral mucosal
DiseasesUlcer generally cause soreness rather than pain , but deep ulceration may cause sever pain.
Carcinoma in particular causes sever pain once nerve fibers become involved.
Herpes zoster causes sever pain , sometime indistinguishable from toothache , (because of involvement of cervical ganglia.
Diseases of the
jawThe important feature of these conditions is that, as well as the history and clinical presentation, the provisional diagnosis depends on the radiographic findings.
Fractures and osteomylitis should be recognizable by radiograph.
The differentiation of infected cyst from a malignant tumor is difficult and the diagnosis depends on biopsy and histological examination.
Painful jaw diseases :
Fractures
Osteomyelitis
Infected cysts
Malignant neoplasm
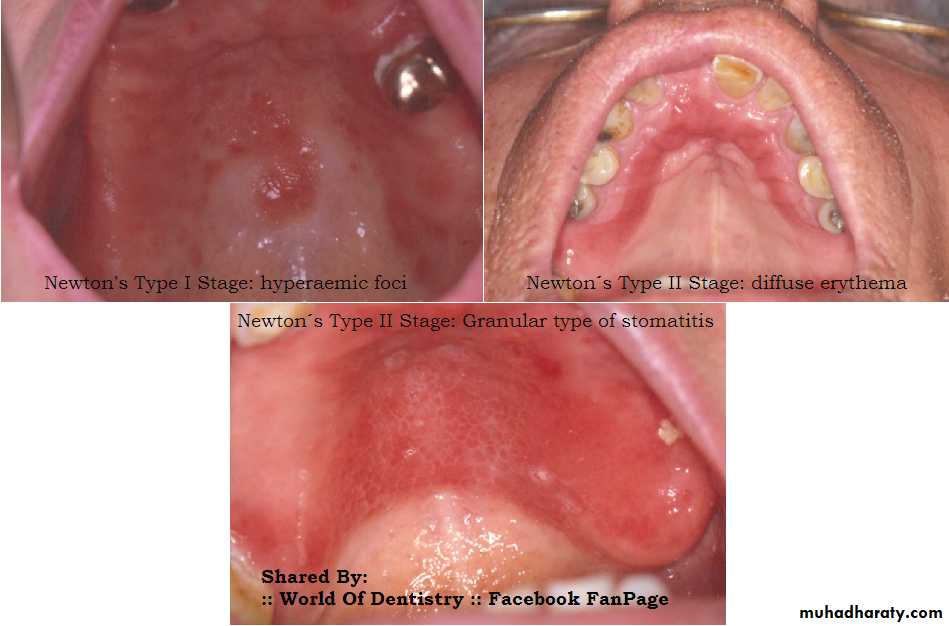
Pain in edentulous
patientsThese conditions differ from most others because dental causes can be excluded. The chief difficulty is to decide whether the pain is due to the dentures themselves, or to some condition of the mucosa or jaws on which a denture is pressing.
Denture Trauma ( traumatic ulcers)
Excessive vertical dimension (TMJ D.S.)
Diseases of denture bearing mucosa
Diseases of the jaws
Teeth or roots erupting under a denture
Pain in edentulous
patientsTraumatic ulcer
Denture induced stomatitis
Post-operative pain
Alveolar osteitis (dry socket)Dry socket
Referred pain
Diseases of the maxillary antrumAcute sinusitis
Carcinoma, particularly when it involves the
antral floor
Diseases of salivary glands
Acute parotitis
Salivary calculi
Sjogren's syndrome
Malignant neoplasms
Diseases of the ears
Otitis media
Neoplasms in this region
Myocardial infarction
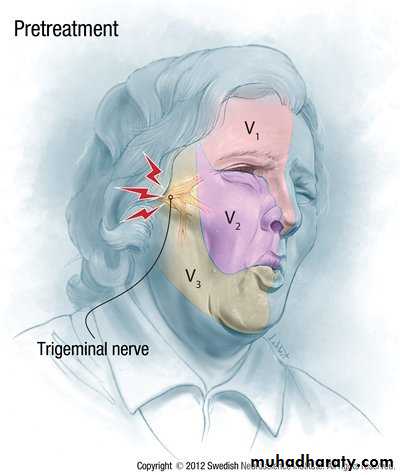
Trigeminal Neuralgia
• Clinical Presentation• Affects elderly (5th-7th decade)
• Almost always unilateral
• Usually one branch is involved
• Paroxysmal pain – seconds to < 2 min
• Distributed along 5th cranial nerve
• Pain provoked by touching, smiling, eating or cold air and teeth brushing.
• Asymptomatic between attacks
• Trigger points
Neuropathic pain
TRIGGER FACTORS
• Investigations:
• Always exclude dental origin (cracked tooth)• Full cranial nerve assessment
• Refer to neurologist if:
• patient <50y
• Bilateral presentation
• Associated neurological signs or cranial nerve defect
Neuropathic pain
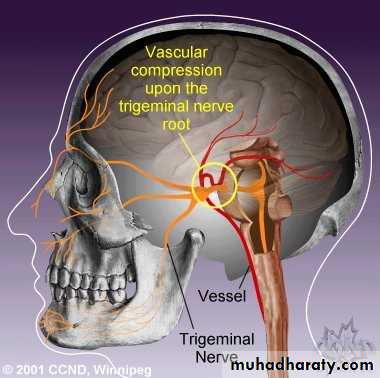
• Cause:
• Demyelination & hyper-excitability of
• the nerve induced by vascular pressure
• 2% of cases associated with posterior
• fossa tumor
Neuropathic pain
• Surgical
• for refractory cases• Simple peripheral cryotherapy or open intracranial procedure
• If these fail , micro vascular decompression of the trigeminal ganglion may be required.
Neuropathic pain
• Medical
• Anticonvulsant
• Carbamazepine (100mgX2) up to 1000 mg/day
• Gabapentin
• Start with small initial dose
• Side effects includes drowsiness , dryness of the mouth , diarrhea and nausea.
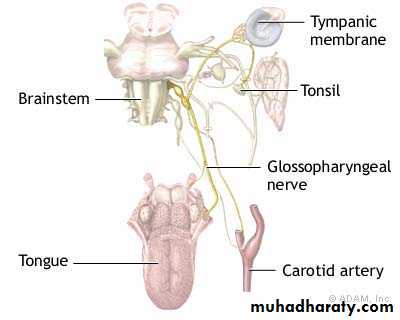
Glossopharyngeal Neuralgia
• Similar to Trigeminal Neuralgia• Less common & less severe
• The pain felt in the base of the tongue and
fauces on one side. It may also radiate
deeply into the ear.
• Unilateral pain precipitated by swallowing , chewing , and coughing.
• Pharynx
• Soft palate
• Base of tongue
• Ear
• Mastoid
• Treatment as for TN
Neuropathic pain
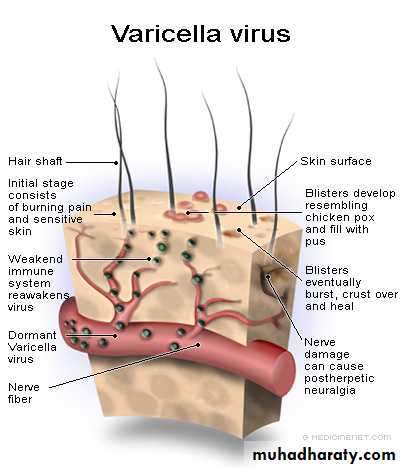
Post-herpetic neuralgia
Neuropathic pain
• Treatment
Unfortunately, postherpetic neuralgia is remarkably resistant to treatment. Nerve or root section are ineffective and the response to drugs of any type.Application of transcutaneous electrical stimulation to the affected area by the patient himself is sometimes effective.
• Anticonvulsants (Gabapentin)
• TCAs
• Antiviral in combination with TCA
• All patients with HZ infection should be vigorously treated with acyclovir to reduce risk of PHN
Neuropathic pain
The pain is more variable in character and severity than trigeminal neuralgia. It is typically persistent rather than paroxysmal.
Affect elderly & immunocompromised patients
The diagnosis is straightforward if there is a history of facial zoster or if scars from the rash are present.
Migrainous neuralgia (cluster headache)
Migrainous neuralgia is caused by vascular changes at the base of the skull and may occasionally be mistaken for trigeminal neuralgia. It is rarely seen in dental practice.Migrainous neuralgia has many features in common with classical migraine (hemicrania) and is due to oedema and dilatation of the wall of the internal carotid and probably also the external carotid arteries.
Cluster headache mainly affects men, usually young adults
but up to the age of 50.
Attacks may be precipitated by alcohol or vasodilators, or come on spontaneously one to three times a day.
Attacks sometimes recur at precisely the same time each
day or may disturb sleep.
Pain is localized to the region of the orbit, or maxilla. The duration is 0.5-2 hours.
Neuropathic pain
Cluster headache may respond to simple analgesics or to ergotamine.
Ergotamine should be given an hour before the expected attack and is most effective by subcutaneous. Alternatively, ergotamine powder can be inhaled from a spinhaler.Treatment should preferably be stopped for one day each week to see whether there has been spontaneous remission.
Neuropathic pain
The eye may become suffused and water, the nostrils may be blocked, the skin over the cheek may become red and there may be sweating on that side.
Paraesthesia &
Anaesthesia ofThe lip
Paraesthesia of the lip can cause by Osteomyelitis or Fracture of the jaw
Prolonged anaesthesia or paraesthesia of the lip can occasionally follow inferior dental blocks.
The inferior dental nerve may be compressed by a neoplasm or a tumour may infiltrate the nerve sheath.
The mental foramen can become exposed by excessive resorption of mandibular bone in an edentulous patient