Venous Diseases
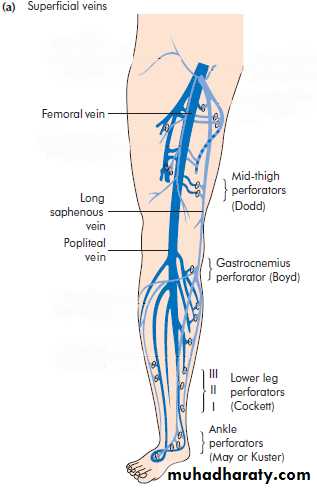
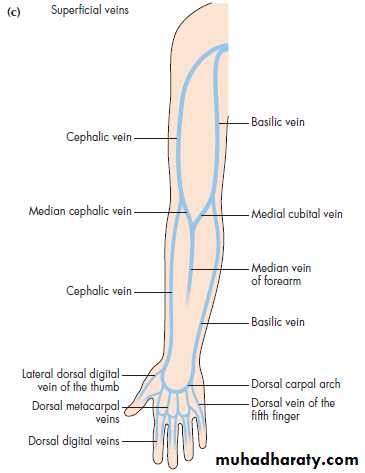
Anatomy:• Superficial and deep systems
All are valved• Important perforators
• Sinusoids.Anatomy:
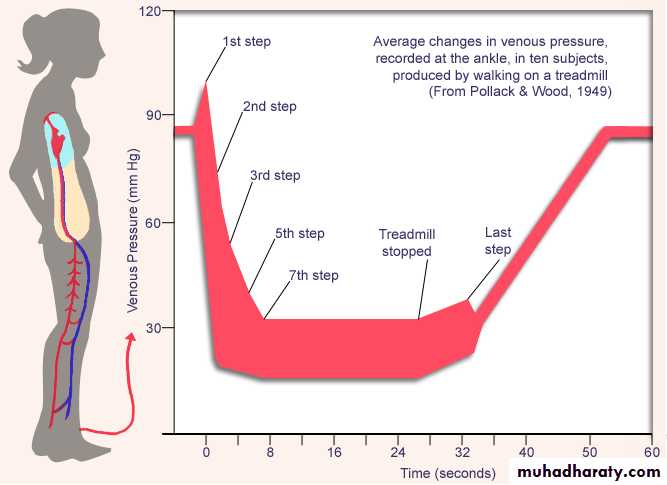
Venous pressure on standing 100 mmHg
Single calf muscle contraction empties 60% of pooled bloodAmbulatory venous
pressure 40 mmHg
Physiology:
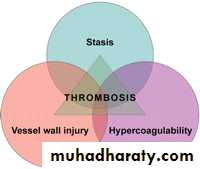
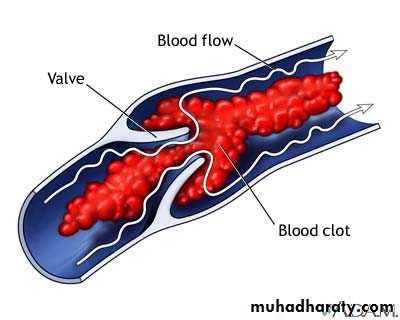
According to Virchow’s Triad
Changes in the vessel wall (endothelial damage);Changes in the blood flow (stasis);
Changes in the blood composition (hypercoagulability).
Etiology:
• Deep Vein Thrombosis (DVT)Risk factors:
Patients factors:• Age
• Obesity
• Varicose veins
• Immobility
• Pregnancy
• Puerperium
• Oral contraceptive pills
• Previous deep vein thrombosis or pulmonary embolism
• Trauma or surgery,
• Malignancy,
• Heart failure
• Recent myocardial infarction
• Paralysis of lower limb(s)
• Infection
• Inflammatory bowel disease
• Nephrotic syndrome
• Polycythaemia
• Paraproteinaemia
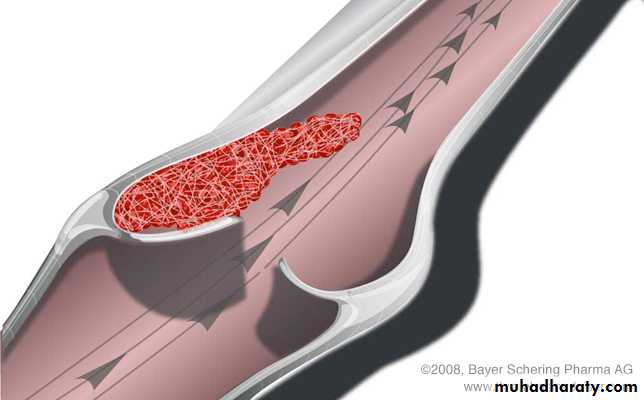
Occlusive thrombus
Pathology:Non occlusive thrombus
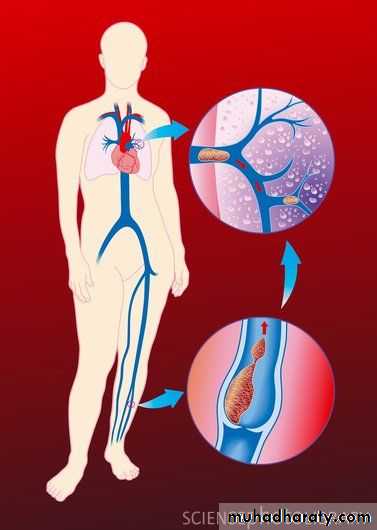
• embolism
•
• Complete resolution of thrombus
• Incomplete resolution Post phlebotic syndrome and chronic venous insufficiency• Organization of thrombus
• Embolization.
Fate of DVT:
Pain and swelling
Bilateral in 30%Asymptomatic
Chest pain, dyspnea and hemoptysis (pulmonary embolism)Phlegmasia alba dolens (white leg)
Phlegmasia cerulea dolens
Clinical presentation:
• Pitting oedema of the ankle,
• Dilated surface veins,• A larger stiff calf
• Tenderness
• Hotness
• Homans’ sign – resistance (not pain) of the calf muscles to forcible dorsiflexion
• A low-grade pyrexia may be present
• Signs of pulmonary embolism or pulmonary hypertension
On examination:
• Duplex ultrasound
• Venography• D-dimer
• If pulmonary embolism suspected:
• Ventilation / perfusion scan
• CT scan
• Pulmonary angiography
Inestigations:
• Ruptured Baker’s cyst,
• A calf muscle haematoma,
• A ruptured plantaris muscle,
• Thrombosed popliteal aneurysm
• Arterial ischemia
Differential diagnosis:
Low risk: young, with minor illnesses, who are to undergo operations lasting 30 min or less.
Moderate risk: over 40 or with a debilitating illness who are to undergo major surgery.
High risk: over 40 who have serious medical conditions, or undergoing major surgery with an additional risk factor.Prophylaxis:
Mechanical methods:
• graduated elastic compression stockings• external pneumatic compression
• passive foot movement (foot paddling machine)
• simple limb elevation
Pharmaceutical methods:
• low molecular weight heparin
• unfractionated heparin
• warfarin
Methods of prophylaxis:
• Admission to hospital and bed rest
• Anticoagulant therapy (heparin and warfarin)• Leg elevation
• Elastic compressive bandage from the toes to the upper thigh
• Patients with phlegmasia cerulea dolens need thrombolytic therapy
Medical treatment:
Venous thrombectomy:
Phlegmasia cerulea dolens with contraindication to thrombolyticsInferior vena cava filter:
Recurrent thromboembolism despite adequate anticoagulationProgressing thromboembolism despite adequate anticoagulation
Complication of anticoagulants
Contraindication to anticoagulants
Surgical treatment:
Dilated tortuous veins5% of adult population
Equal gender prevalence
Family historyIntroduction:
• Varicose Vein
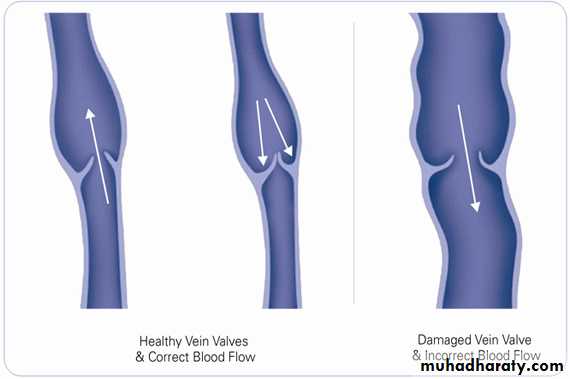
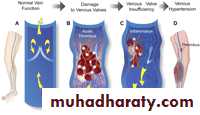
Incompetence of the venous valves
Primary venous incompetenceSecondary venous incompetence
Pathology:
Unsightly appearance
Discomfort and aching at the end of the dayAnkle swelling towards the end of the day
Complications:
Itching and eczema
Lipodermatosclerosis
Venous ulceration
Clinical manifestations:
Venous Eczema (stasis dermatitis):
Lipodermatosclerosis:
Venous Ulcer:
On examination:Great or small saphenous vein
• Incompetent saphenofemoral junction or incompetent perforators
Exclude DVT or deep vein incompetence
Usually diagnosed clinically
Investigations done to confirm and exclude• Duplex ultrasound
• Venography
• Abdominal and/or pelvic imaging
Investigations:
• Reassurance
• Elastic compression stockings
• Avoid prolong standing and change of occupation may be required
• Periodic elevation of the feet
Treatment:
• I- Conservative Treatment:
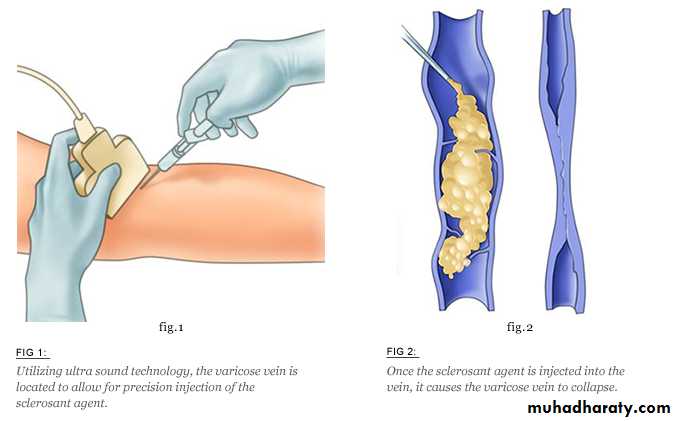
Sodium tetradecyl sulfate (STD)
II- Injection sclerotherapy:Indications for surgery:
Symptomatic varicose veinsComplicated or bleeding varicose veins
Large varicose veins
Cosmetic purposes
Surgical options include:
Ligation and stripping of the saphenous vein
Multiple subfacial perforator ligation
Combination of both.
Complications of varicose vein surgery:
Nerve injury (saphenous nerve and sural nerve)
Recurrence
III- Surgical Treatment:
Pathology:
• Deep Vein IncompetenceLeg swelling,
Discomfort on walking,Edema,
Varicose veins (which may not be present),
Ankle flare (small varices),
Lipodermatosclerosis
Ulceration
Clinical presentation
Post Phlebetic syndrome:
• Duplex ultrasound
• Venography.
Investigations:
• Elastic compression stockings
• Avoid prolong standing and change of occupation may be required• Periodic elevation of the feet
• Exercise of the calf muscles
Treatment:
• I- Conservative Treatment:
• Venous bypass procedures (e.g. Palma procedure)
• Venous valve reconstruction• Venous valve transposition
II- Surgical Treatment:
Venous disease: deep vein incompetence
Arterial ischemiaRheumatoid ulcer
Traumatic ulcer
Neuropathic ulcer (diabetic)
Neoplastic ulcer (squamous cell carcinoma and basal cell carcinoma).
Differential diagnosis of leg ulcers:
• Venous Ulceration
Not fully understood
Ambulatory venous hypertensionDue to valve incompetence:
Incompetent superficial veins
Incompetent perforator veins
Incompetent or obstructed deep veins
Etiolgy:
Site: gaiter region (between calf and ankle)
Size: usually largeDepth: usually superficial
Edges: gently sloping edges
Base: granulation tissue + slough and exudates
Discharge: pus occasionally blood
Surrounding tissue: features of chronic venous disease
Local lymph nodes: enlarged (superadded infection)
Movement of ankle joint: restricted due to pain
Clinical examination
Venous Ulcer:
• Swab and culture from the ulcer• Duplex ultrasound
• Venography
Investigations:
multilayered elastic compression bandaging system,
avoid prolong standing,periodic leg elevation
Treatment:
• I- conservative Treatment:
• Surgery for the cause of the venous ulcer (varicose vein, DVT or chronic venous insufficiency)
• Perforator vein subfacial ligation
• Skin graft to the ulcer after dealing with the underlying cause
II- Surgical Treatment:
External trauma,
Venepunctures and infusions of hyperosmolar solutions and drugs.
Intravenous cannula
Some systemic diseases: buerger’s disease, and malignancy,
Coagulation disorders: polycythaemia, thrombocytosis and sickle cell disease
Etiology:
• Superficial Thrombophlebitis• Treatment::
• Reassurance• NSAIDs
• Warm massage