THE EAR
Dr. Mohamad S. Aziz
OtolaryngologistCABMS (ORL-HNS)
ENT Dept, College of Medicine, University of Mosul
Undergraduate, The EAR, 2016/2017
3
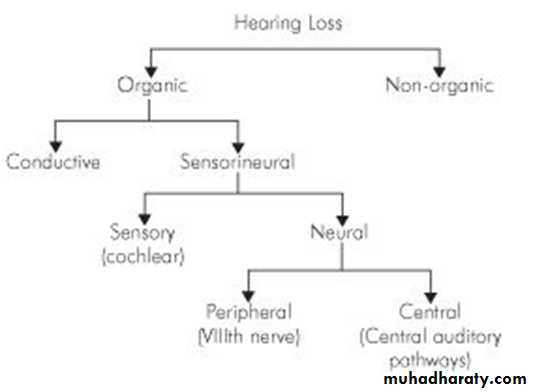
Hearing Loss
CLASSIFICATION
4
ASSESSMENT OF HEARING
A. Clinical Tests of Hearing
1. Finger Friction Test2. Watch Test
3. Speech (Whispering Voice) TestsThe distance at which conversational voice and the whispered voice are heard is measured(normally 6 metres).
4. Tuning Fork Tests
Tuning fork of 512 Hz is ideal.
lower frequencies produce sense of bone vibration
higher frequency have a shorter decay time
(a) Rinne test
AC of the ear is compared with its BC. Rinne positive when AC is longer or louder than BC. seen in normal persons or sensorineural deafness. A negative Rinne (BC > AC) conductive deafness.
5
False negative Rinne. in severe unilateral SNHL(dead ear). Patient does not perceive any sound of TF by air conduction but responds to BC testing. This response is from the opposite ear because of transcranial transmission of sound. correct diagnosis made by masking the non-test ear with Barany's noise box while testing for bone conduction. Weber test will help
(b) Weber test
Normally, TF heard equally in both ears. It is lateralized to the worse ear in conductive deafness and to the better ear in sensorineural deafness.
(c) Absolute bone conduction (ABC) test
BC is a measure of cochlear function. patient's BC is compared with that of the examiner (presuming normal hearing). EAM of both the patient and examiner should be occluded. In conductive deafness, the patient and the examiner hear the fork for the same duration of time. In sensorineural deafness, the patient hears the fork for a shorter duration.(d) Schwabach's test
BC of patient is compared with the examiner (meatus is not occluded).
(e) Bing test
(f) Gelle's test
6
B. Audiometric Tests
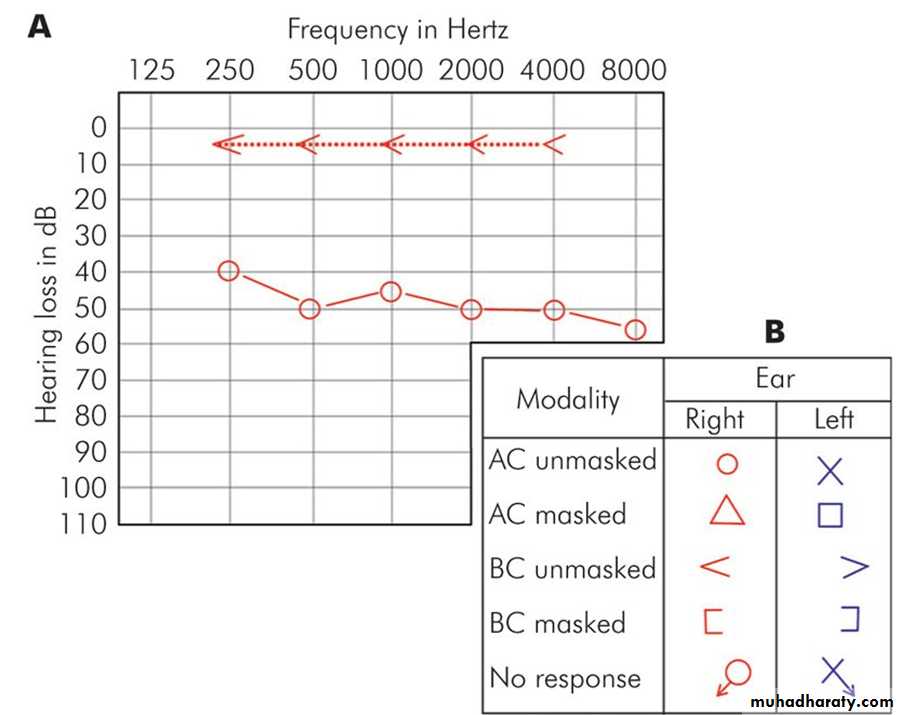
1. Pure Tone Audiometry
An audiometer is an electronic device which produces pure tones, the intensity of which can be increased or decreased in 5 dB steps.
air conduction thresholds are measured for tones of 125, 250, 500, 1000, 2000 and 4000 and 8000 Hz
bone conduction thresholds for 250, 500, 1000 and 2000 and 4000 Hz.
The intensity that has to be raised above the normal level is a measure of the degree of hearing impairment at that frequency.
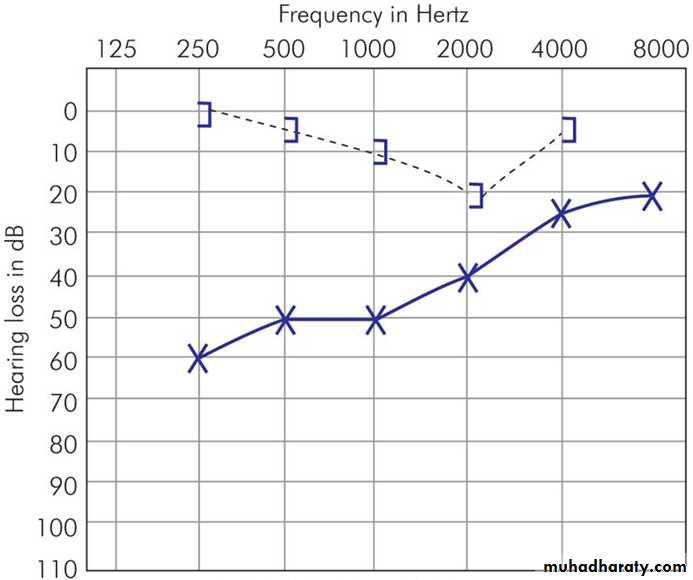
It is charted in the form of a graph called audiogram. The threshold of BC is a measure of cochlear function. The difference in the thresholds of air and bone conduction (A-B gap) is a measure of the degree of conductive deafness.
2. Speech Audiometry
In this test, the patient's ability to hear and understand speech is measured.
3. Bekesy Audiometry
7
4. Impedance Audiometry
It is an objective test, particularly useful in children. It consists of:
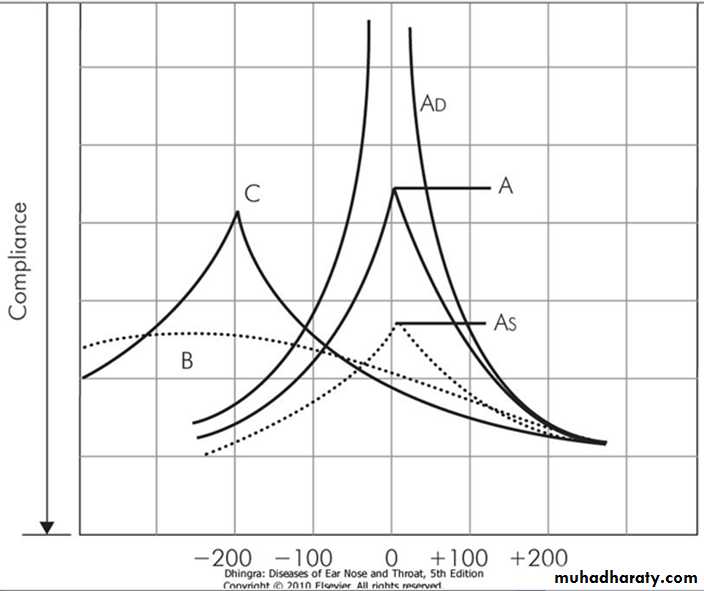
(a) Tympanometry
(b) Acoustic reflex measurements
Acoustic reflex
It is based on the fact that a loud sound, 70-100 dB above the threshold of hearing of a particular ear, causes bilateral contraction of the stapedial muscles which can be detected by tympanometry. Tone can be delivered to one ear and the reflex picked from the same or the contralateral ear.
8
Type A Normal tympanogram.
Type As Compliance is lower. Seen in fixation of ossicles, e.g. otosclerosis or malleus fixation.
Type AD High compliance . Seen in ossicular discontinuity or thin and lax tympanic membrane.
Type B A flat or dome-shaped graph. No change in compliance with pressure changes. Seen in middle ear fluid or thick tympanic membrane or TM perforation.
Type C Maximum compliance occurs with negative pressure in excess of 100 mm of H2O. Seen in retracted tympanic membrane and may show some fluid in middle ear.
9
C. Special Tests of Hearing
1. Recruitment
2. Short Increment Sensitivity Index (SISI Test)
3. Tone Decay Test
(1. , 2. & 3. Differentiate cochlear from retrocochlear lesions)
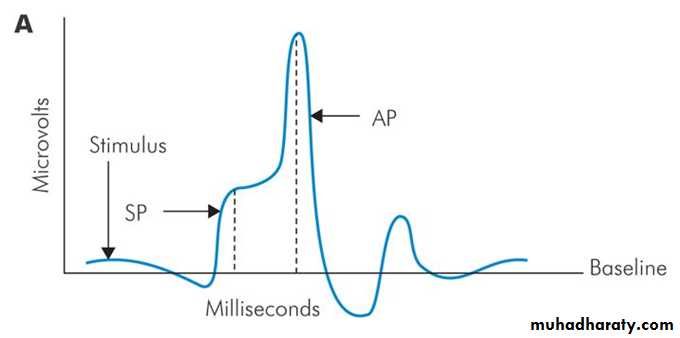
4. Evoked Response Audiometry
It is an objective test which measures electrical activity in the auditory pathways in response to auditory stimuli. They are: (a) Electrocochleography (EcoG).(b) Auditory brainstem response (ABR
5. Otoacoustic Emissions (OAEs)
They are low intensity sounds produced by outer hair cells of a normal cochlea and thus help to test the function of cochlea.6. Central Auditory Tests
10
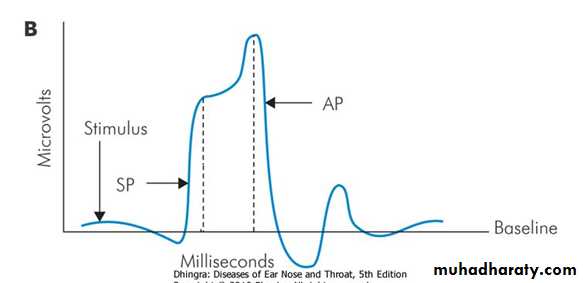
Electrocochleography (EcoG) It measures electrical potentials arising in the cochlea and CN VIII in response to auditory stimuli within first 5 milliseconds. The response is in the form of three phenomena: cochlear microphonics, summating potentials and the action potential of VIIIth nerve.
The recording electrode is a thin needle passed through TM onto the promontory. done under LA but in children or anxious persons sedation or GA is required. Normally the ratio between the amplitude of summating potential to the action potential is less than 30%. An increase in this ratio is indicative of Mèniere's disease .
11
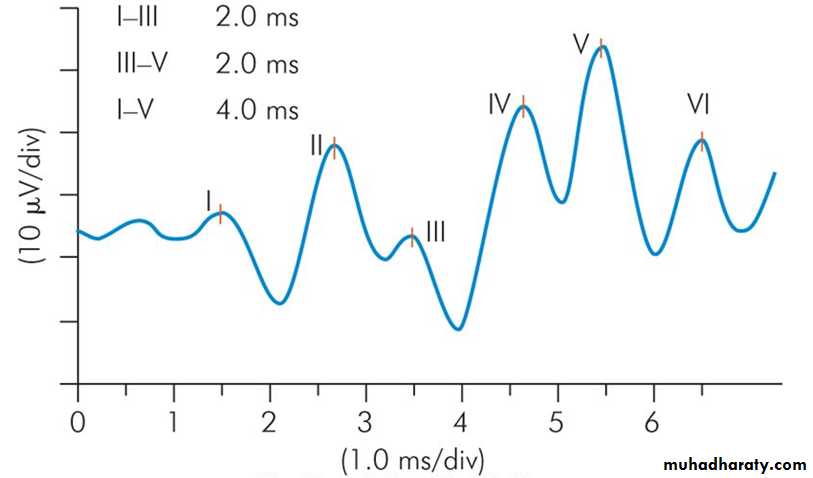
Auditory brainstem response (ABR) is to elicit brainstem responses to auditory stimulation by clicks or tone bursts. non-invasive technique to find the integrity of central auditory pathways. electrical potentials picked up from the vertex by surface electrodes. In a normal person, 7 waves are produced in the first 10 milliseconds. The first, third and fifth waves are most stable and are used in measurements.
Wave I
• Distal part of CN VIII
Wave II
Proximal part of CN VIII near the brainstem
Wave III
Cochlear nucleus
Wave IV
Superior olivary complex
Wave V
Lateral lemniscus
Waves VI and VII
Inferior colliculus
12
13
Hearing Loss
CLASSIFICATION
14
CONDUCTIVE HEARING LOSS AND ITS MANAGEMENT
Any disease process which interferes with the conduction of sound to reach cochlea causes conductive hearing loss.
The lesion may lie in the external ear and tympanic membrane, middle ear or ossicles up to stapediovestibular joint.
The characteristics of conductive hearing loss are:
1. Negative Rinne test, i.e. BC > AC.2. Weber lateralised to poorer ear.
3. Normal absolute bone conduction.
4. Low frequencies affected more.
5. Audiometry shows BC better than AC with air-bone gap.
6. Loss is not more than 60 dB.
7. Speech discrimination is good
15
16
Aetiology
Congenital :
Meatal atresia
Fixation of stapes footplate
Fixation of malleus head
Ossicular discontinuity
Congenital cholesteatoma
Acquired :
External ear: Any obstruction in the ear canal, e.g. wax, foreign body, furuncle, acute inflammatory swelling, benign or malignant tumour or atresia of canal.Middle ear
(a) Perforation of TM, traumatic or infective(b) Fluid in the middle ear, e.g. AOM, OME or haemotympanum
(c) Mass in middle ear, e.g. benign or malignant tumour
(d) Disruption of ossicles, e.g. trauma to ossicular chain, CSOM, cholesteatoma
(e) Fixation of ossicles, e.g. otosclerosis, adhesive otitis media
(f) Eustachian tube blockage, e.g. retracted TM, serous OM.
17
Management
Most cases of conductive hearing loss can be managed by medical or surgical means.
Briefly, it consists of:
1. Removal of canal obstructions, e.g. impacted wax, foreign body, osteoma or exostosis, keratotic mass, benign or malignant tumours, meatal atresia.2. Removal of fluid Myringotomy with or without grommet insertion.
3. Removal of mass from middle ear
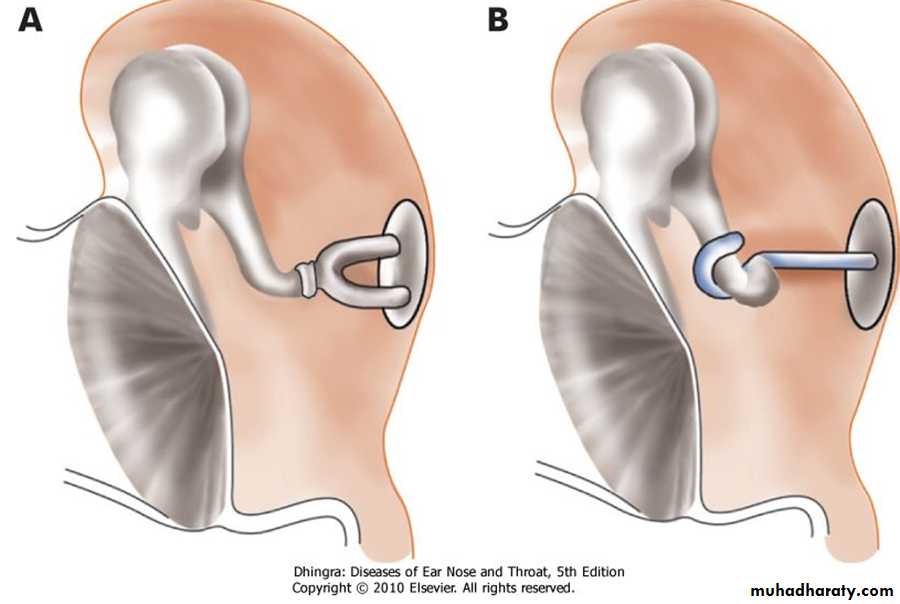
4. Stapedectomy, as in otosclerotic fixation of stapes footplate.
5. Tympanoplasty Repair of perforation, ossicular chain or both.
6. Hearing aid In cases, where surgery is not possible, refused or has failed
18
19
Otosclerosis (Syn. Otospongiosis)
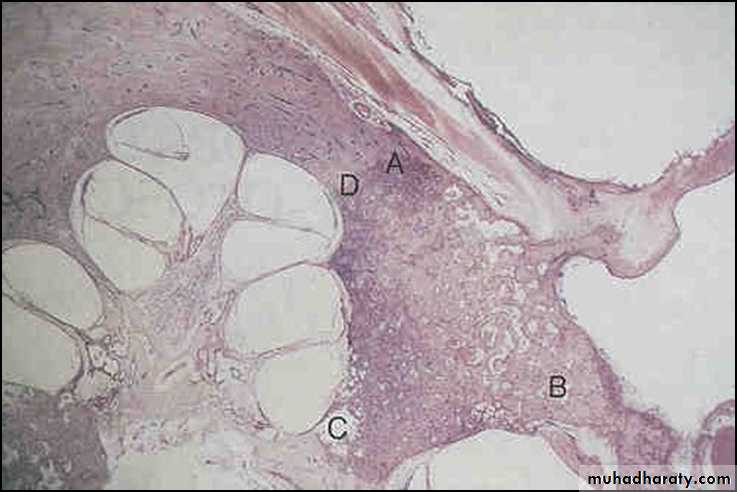
Otosclerosis is a primary disease of the bony labyrinth. one or more foci of irregularly laid spongy bone replace part of normally dense enchondral layer of bony otic capsule.
Most often, otosclerotic focus involves the stapes region leading to stapes fixation and conductive deafness. However, it may involve certain other areas of the bony labyrinth where it may cause neurosensory loss, or no symptoms at all.
Types of Otosclerosis
1. Stapedial otosclerosis
causing stapes fixation and conductive deafness is the most common variety.
2. Cochlear otosclerosis
involves round window or other areas in the otic capsule, and may cause SNHL due to liberation of toxic materials into the inner ear fluid.
3. Histologic otosclerosis
This type remains asymptomatic and causes neither conductive nor SNHL
20
Pathology للاطلاع
Grossly, otosclerotic lesion appears chalky white, greyish or yellow. Sometimes, it is red in colour due to increased vascularity, in which case, the otosclerotic focus is active and rapidly progressive.
Microscopically, spongy bone appears in the normally dense enchondral layer of otic capsule. In immature active lesions, there are numerous marrow and vascular spaces with plenty of osteoblasts and osteoclasts and a lot of cement substance which stains blue (blue mantles of Manasse) with haematoxylin-eosin stain. Mature foci show less vascularity and laying of more bone and more of fibrillar substance , and is stained red.
21
Aetiology
The exact cause is not known
Anatomical basis. The fissula ante fenestram lying in front of the oval window-the site of predilection.
Heredity. About 50% of otosclerotics have positive family history; rest are sporadic. it is an autosomal dominant trait with incomplete penetrance and a variable expressivity.
Race. White races are affected more than Negroes.
Sex. Females are affected twice as often as males .
Age of onset. Deafness usually starts between 20 and 30 years of age.
Effect of other factors (HORMONAL). otosclerosis may be initiated or made worse by pregnancy. Similarly, deafness may increase during menopause, after an accident or a major operation.
osteogenesis imperfecta . The triad of symptoms of osteogenesis imperfecta :multiple fractures , otosclerosis and blue sclera, is called van der Hoeve syndrome.
Viral infection. measles virus. It is likely that otosclerosis is a viral disease as has been suggested for Paget's disease
22
23
Symptoms
1. Hearing lossis the presenting symptom and usually starts in twenties (> female). painless and progressive with insidious onset. Often it is bilateral conductive type.
2. Paracusis willisii
patient hears better in noisy than quiet surroundings. This is because a normal person will raise his voice in noisy surroundings.
3. Tinnitus
It is more commonly seen in cochlear otosclerosis and in active lesions.
4. Vertigo
5. Speech
Patient has a monotonous, well-modulated soft speech
Signs
TM is quite normal and mobile. Sometimes, a reddish hue may be seen on the promontory through the TM (Schwartze sign). This is indicative of active focus with increased vascularity.
Eustachian tube function is normal.
Tuning fork tests show negative Rinne (i.e. BC > AC).
Weber test will be lateralised to the ear with greater conductive loss. Absolute bone conduction may be normal.
24
Pure tone audiometry shows loss of air conduction, more for lower frequencies. Bone conduction is normal. In some cases, there is a dip in bone conduction curve, maximum at 2000 Hz and is called the Carhart's notch. Carhart's notch disappears after successful stapedectomy.
Speech audiometry reveals normal discrimination score except in those with cochlear involvement.
Tympanometry shows a curve of ossicular stiffness( As).
Stapedial reflex becomes absent when stapes is fixed
Differential Diagnosis
Otosclerosis should be differentiated from serous otitis media, adhesive otitis media, tympanosclerosis, fixation of head of malleus, ossicular discontinuity, Paget's disease or congenital stapes fixation.
25
Treatment
Medical
no medical treatment that cures otosclerosis. Sodium fluoride has been tried to hasten the maturity of active focus and arrest further cochlear loss.
Surgical
Stapedectomy with placement of prosthesis is the treatment of choice. the otosclerotic stapes is removed and a prosthesis inserted between the incus and oval window . Prosthesis may be a teflon , stainless steel , platinum or titanium teflon piston . In 90% of patients, there is good improvement in hearing after stapedectomy.
Hearing aid
Patients who refuse surgery or are unfit for surgery can use hearing aid.
26
SENSORINEURAL HEARING LOSS AND ITS MANAGEMENT
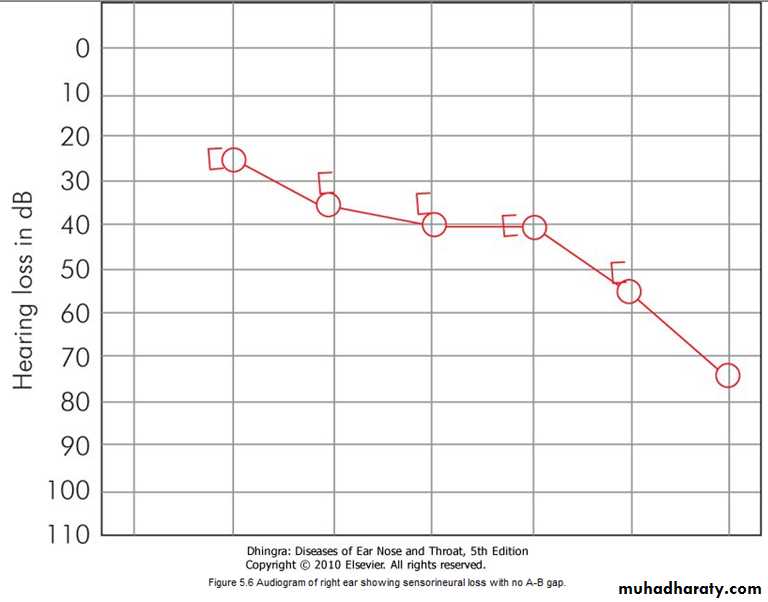
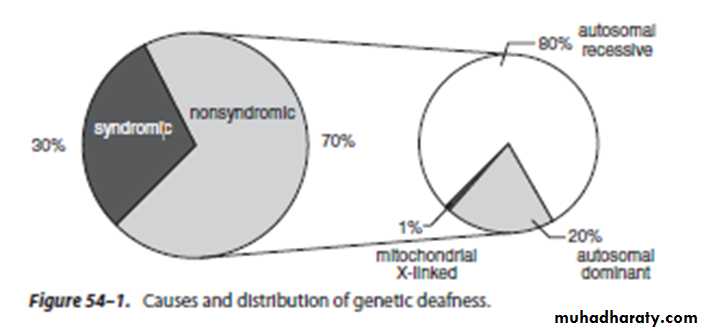
SNHL results from lesions of the cochlea, VIIIth nerve or central auditory pathways. In may be present at birth (congenital) or start later in life (acquired).The characteristics of sensorineural hearing loss are:
1. A positive Rinne test, i.e. AC > BC.
2. Weber lateralised to better ear.
3. BC reduced on Schwabach and absolute bone conduction tests.
4. More often involving high frequencies.
5. No gap between air and bone conduction curve on audiometry.
6. Loss may exceed 60 dB.
7. Speech discrimination is poor.
8. There is difficulty in hearing in the presence of noise.
27
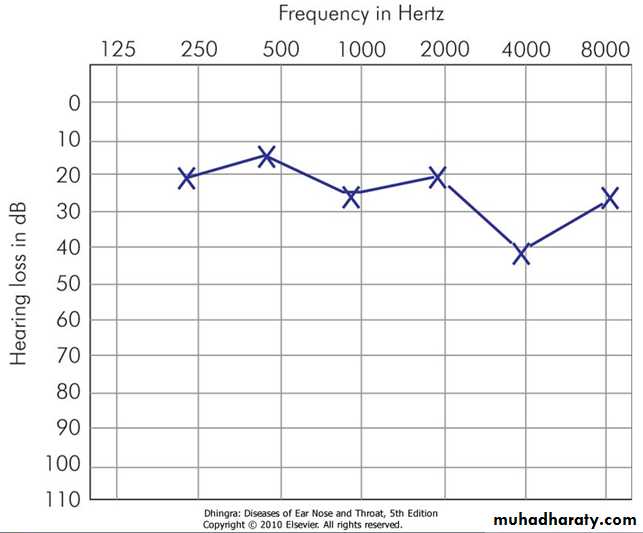
Audiogram of right ear showing sensorineural loss with no A-B gap
28
Acquired
1. Infections of labyrinth-viral, bacterial or spirochaetal,2. Trauma to labyrinth or VIIIth nerve, e.g. fractures of temporal bone or concussion of labyrinth or ear surgery,
3. Noise-induced hearing loss,
4. Ototoxic drugs,
5.Presbycusis,
6. Meniere's disease,
7. Acoustic neuroma,
8. Sudden hearing loss
9. Familial progressive SNHL,
10. Systemic disorders, e.g. diabetes, hypothyroidism, kidney disease, autoimmune disorders, multiple sclerosis, blood dyscrasias
Aetiology of SNHL
CongenitalIt is present at birth and is the result of anomalies of the inner ear or damage to the hearing apparatus by prenatal or perinatal factors
29
Diagnosis
1. History
congenital or acquired, stationary or progressive, associated with other syndromes or not, involvement of other members of the family and possible aetiologic factors.
2. Severity of deafness
(mild, moderate, moderately severe, severe, profound or total) This can be found out on audiometry.
3. Type of audiogram
whether high frequency, low frequency, mid-frequency or flat type.
4. Site of lesion
i.e. cochlear, retrocochlear or central.
5. Other tests
depend on the aetiology suspected, e.g. X-rays or CT scan of temporal bone for evidence of bone destruction (congenital cholesteatoma, glomus tumour or acoustic neuroma), blood counts (leukaemia), blood sugar (diabetes), serology for syphilis, thyroid functions (hypothyroidism), kidney function tests, etc
30
Management
Early detection of SNHL is important as measures can be taken to stop its progress, reverse it or to start an early rehabilitation programme, so essential for communication.
Syphilis is treatable with high doses of penicillin and steroids with improvement in hearing.
Hearing loss of hypothyroidism can be reversed with replacement therapy.
Serous labyrinthitis can be reversed by attention to middle ear infection.
perilymph fistula can be corrected surgically by sealing the fistula in the oval or round window with fat.
Ototoxic drugs should be used with care and discontinued if causing hearing loss.
Noise induced hearing loss can be prevented from further deterioration if the person is removed from the noisy surroundings
31
SPECIFIC FORMS OF HEARING LOSS
A. Inflammations of Labyrinth1. Viral labyrinthitis
Viruses usually reach the inner ear by blood stream
Measles, mumps and cytomegaloviruses .
Several other viruses, e.g. rubella, herpes zoster, herpes simplex, influenza and Epstein-Barr .
2. Bacterial
Bacterial infections reach labyrinth through the middle ear (tympanogenic) or through CSF (meningogenic).
SNHL following meningitis is a well-known clinical entity (H.influenzae & S.pneumoniae) . Membranous labyrinth is totally destroyed.
3. Syphilitic
SNHL is caused both by congenital and acquired syphilis. Congenital syphilis is of two types: the early form or the late form
Diagnosis of otosyphilis can be made by other clinical evidence of late acquired or congenital syphilis (interstitial keratitis, Hutchinson's teeth, saddle nose, nasal septal perforation and frontal bossing) and the laboratory tests. FTA-ABS and VDRL or RPR tests from CSF are useful to establish the diagnosis.
Treatment of otosyphilis includes i.v. penicillin and steroids
32
B. Familial Progressive Sensorineural Hearing Loss
It is a genetic disorder(autosomal dominant) starting in late childhood or early adult life.C. Ototoxicity
1. Aminoglycoside antibiotics
Streptomycin, gentamicin and tobramycin are primarily vestibulotoxic.
Neomycin, kanamycin and amikacin are cochleotoxic. destruction of outer hair cells, starting at the basal coil and progressing onto the apex of cochlea.
2. Diuretics Furosemide and ethacrynic acid , reversible.
3. Salicylates reversible
4. Quinine & Chloroquin reversible.
5. Cytotoxic drugs Nitrogen mustard, cisplatin and carboplatin .
6. Deferoxamine (Desferrioxamine)
It is an iron-chelating substance used in the treatment of thalassaemic patients.
7. Miscellaneous
reported with erythromycin, ampicillin and chloramphenicol, indomethacin, phenylbutazone, ibuprofen, tetanus antitoxin, propranolol and propylthiouracil.
Alcohol, tobacco and marijuana also cause damage to the inner ear.
8. Topical ear drops
by absorption through oval and round windows .e.g chlorhexidine or ear drops containing amino-glycoside antibiotics, e.g. neomycin and gentamicin.
33
D. Noise Trauma
well-known in boiler makers, iron-and coppersmiths and artillery men. Occupational hazard; the compensations and the responsibilities thrust upon the employer and the employee to conserve hearing.
It can be divided into two groups:
1. Acoustic traumaPermanent damage caused by a single brief exposure to very intense sound, e.g. an explosion, gunfire or a powerful cracker. Noise level in rifle or a gun fire may reach 140-170 dB SPL. Sudden loud sound may damage outer hair cells, the organ of Corti and rupture the Reissner's membrane.
2. Noise-induced hearing loss (NIHL)
follows chronic exposure to less intense sounds than seen in acoustic trauma and is mainly a hazard of noisy occupations.
(a) Temporary threshold shift recovers after an interval of minutes to hours.
(b) Permanent threshold shift does not recover at all.
34
NIHL causes damage to hair cells, starting in the basal turn of cochlea.
Outer hair cells are affected before the inner hair cells.
Noise-induced hearing loss is preventable.
pre-employment and then annual audiograms for early detection.Ear protectors (ear plugs or ear muffs) should be used where noise levels exceed 85 dB (A). They provide protection up to 35 dB.
rehabilitation is similar to that employed for other sensorineural hearing losses
Early case of noise-induced hearing loss. Note dip at 4000 Hz.
35
E. Sudden Hearing Loss
SNHL that has developed over a period of hours or a few days (30 decibel (dB) loss over three contiguous frequencies occurring within 3 days). Mostly it is unilateral. It may be accompanied by tinnitus or temporary spell of vertigo.
Aetiology
1.Infections: Mumps, herpes zoster, meningitis, syphilis, OM. 2. Trauma: Head injury, ear operations, noise trauma, barotrauma, spontaneous rupture of cochlear membranes.3. Vascular: Haemorrhage (leukaemia), embolism or thrombosis of labyrinthine or cochlear artery or vasospasm. They may be associated with diabetes, hypertension, polycythaemia, macroglobinaemia or sickle cell trait. 4. Ear (otologic) : Meniere's disease, Cogan's syndrome( AUTOIMMUNE DISEASE), large vestibular aqueduct. 5. Toxic: Ototoxic drugs, insecticides.
6. Neoplastic: Acoustic neuroma. Metastases in cerebellopontine angle, carcinomatous neuropathy.
7. Miscellaneous :Multiple sclerosis, hypothyroidism, sarcoidosis.
8. Psychogenic.
36
Management
Detailed history, physical examination and laboratory investigations may include audiometry, vestibular tests, imaging studies of temporal bones, sedimentation rate, tests for syphilis, diabetes, hypothyroidism, blood disorders and lipid profiles.
Where the cause still remains obscure(IDIOPATHIC) , treatment is consists of:
1. Bed rest.2. Steroid therapy Prednisolone 40-60 mg in a single dose for one week then tailed off in a period of 3 weeks. Steroids are anti-inflammatory and relieve oedema.
3. Inhalation of carbogen (5% CO2 + 95% O2) It increases cochlear blood flow and improves oxygenation.
4. Vasodilator drugs.
5. Low molecular weight dextran It decreases blood viscosity.
6. Hyperbaric oxygen therapy
Prognosis
about half the patients of idiopathic sensorineural hearing loss recover spontaneously within 15 days.
Chances of recovery are poor after 1 month. Severe hearing loss and that associated with vertigo have poor prognosis. Younger patients below 40 and those with moderate losses have better prognosis
37
F. Presbycusis
SNHL associated with aging process in the ear is called presbycusis.
It usually manifests at the age of 65 years .
Patients of presbycusis have great difficulty in hearing in the presence of background noise though they may hear well in quiet surroundings.
They may complain of speech being heard but not understood. Recruitment phenomenon is positive and all the sounds suddenly become intolerable when volume is raised.
Tinnitus bothersome problem sometimes the only complaint.
Patients of presbycusis can be helped by a hearing aid. They should also have lessons in speech reading through visual cues. Curtailment of smoking and stimulants like tea and coffee may help to decrease tinnitus.
38
39
Rehabilitation of the Hearing-Impaired
I. Instrumental devices
A. Hearing aids
(i) Conventional hearing aids
(ii) Bone anchored hearing aids (BAHA)
(iii) Implantable hearing aids
B. Implants
(i) Cochlear implants
(ii) Auditory brainstem implants
C. Assistive devices for the deaf
II. Training
A. Speech (lip) reading
B. Auditory training
C. Speech conservation
40
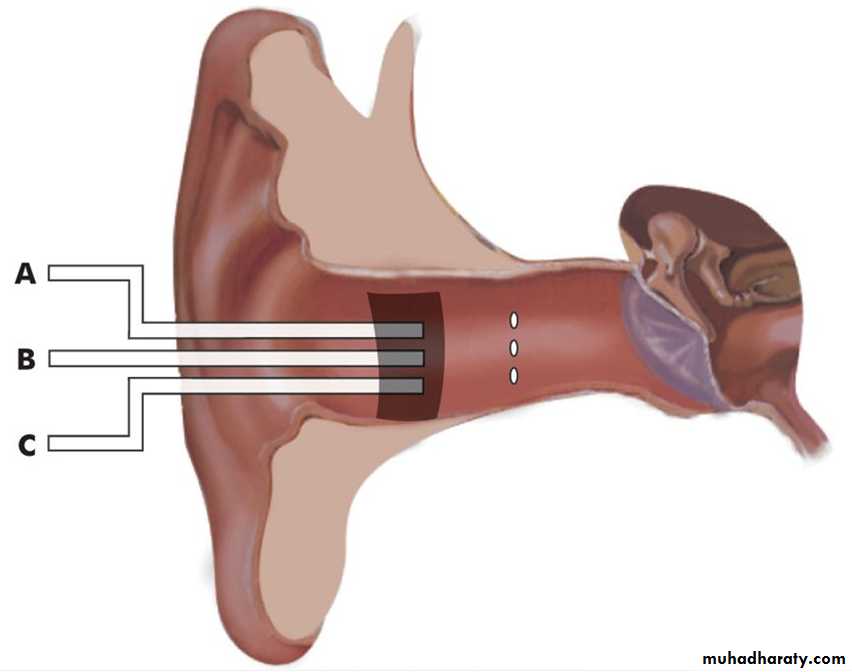
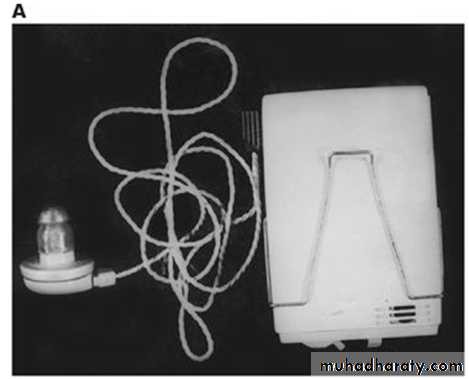
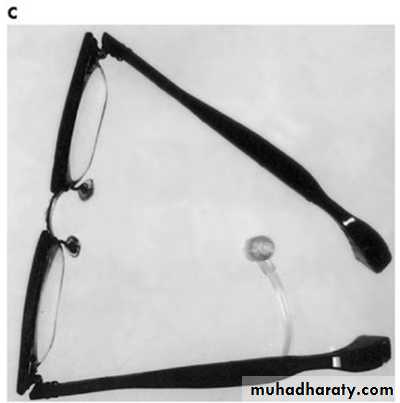
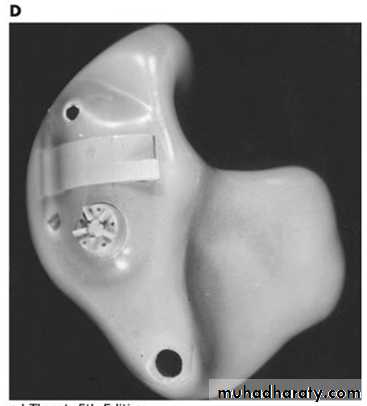
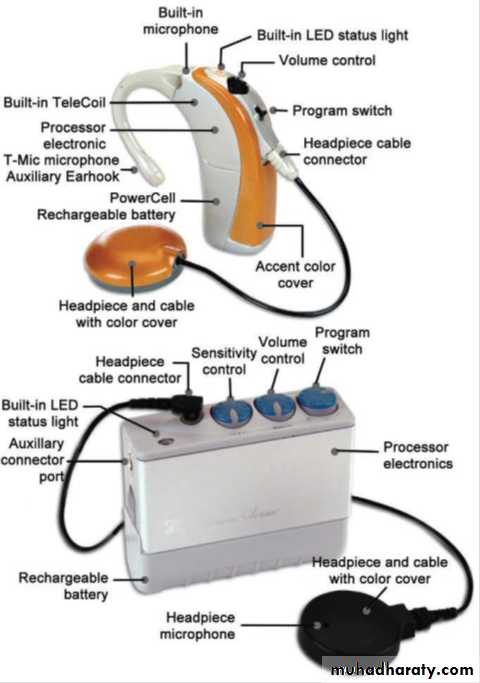
Various types of hearing aids.
(A) Body-worn. (B) Behind-the-ear type.(C) Spectacle type. (D) In-the-ear type.
41
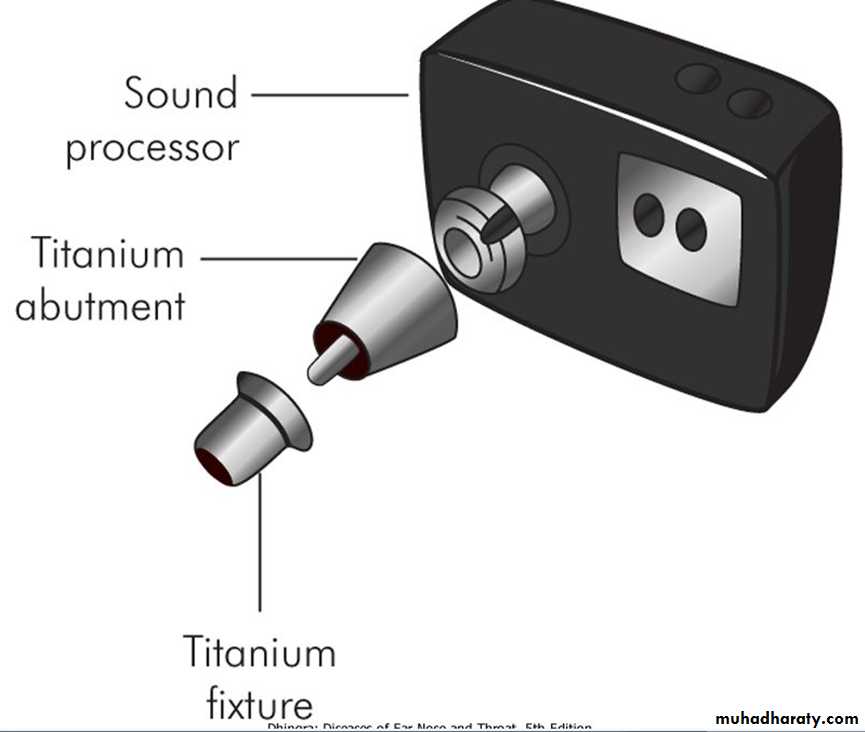
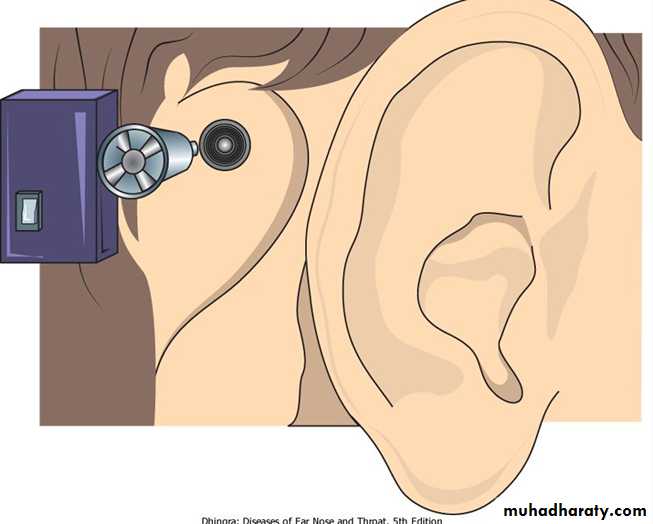
Bone-anchored hearing aid (BAHA).
42
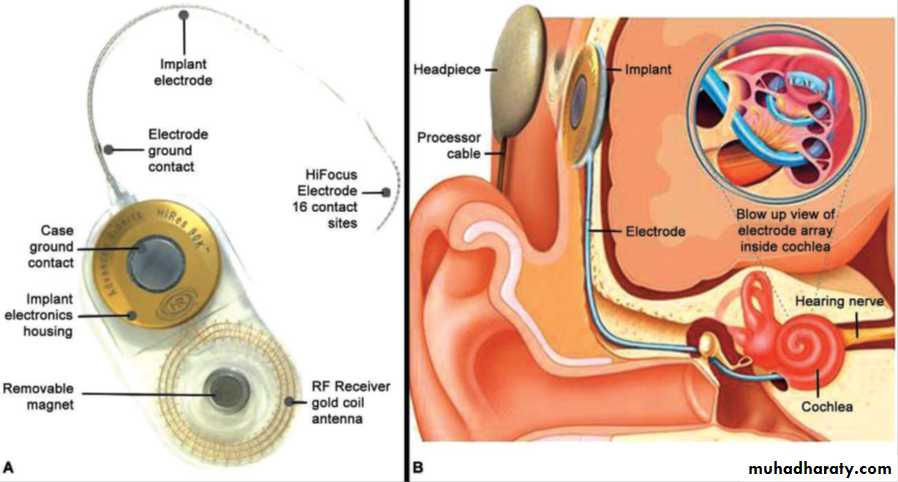
Cochlear implant( A&B internal parts, C external part BHE , D body-worn
4344