
D.Haider L3
1
Bruellosis
: disease of domestic and wild animal(zoonosis) transmittable to
human.
It has different non-specific symptom and signs.
1886 Bruce isolated Brucellae melitensis from spleens of Malta fever victims.
The brucellae are obligate intra-cellular parasites of animals and humans .
Brucella melitensis typically infects goats; Brucella suis, swine; Brucella
abortus, cattle; and Brucella canis, dogs. The disease in humans, brucellosis
(undulant fever, Malta fever), is characterized by an acute bacteremic phase
followed by a chronic stage that may extend over many years and may
involve many tissues.
Source of infection:
Brucellosis is a systemic infectious disease transmitted from certain animals
to humans (zoonotic disease). Brucellosis in humans is predominantly
caused
by
four
different
species
of Brucella bacteria: Brucella
melitensis (goats,
sheep,
camels), Brucella
suis (pigs), Brucella
abortus (cows, buffalo, elk, camels, yaks), and Brucella canis(dogs). Though
all of these species can cause human brucellosis, Brucella melitensis is the
most prevalent worldwide, and it is felt to cause the most severe cases of
brucellosis.
Brucellae
D.Haider L3
2
Morphology & Identification
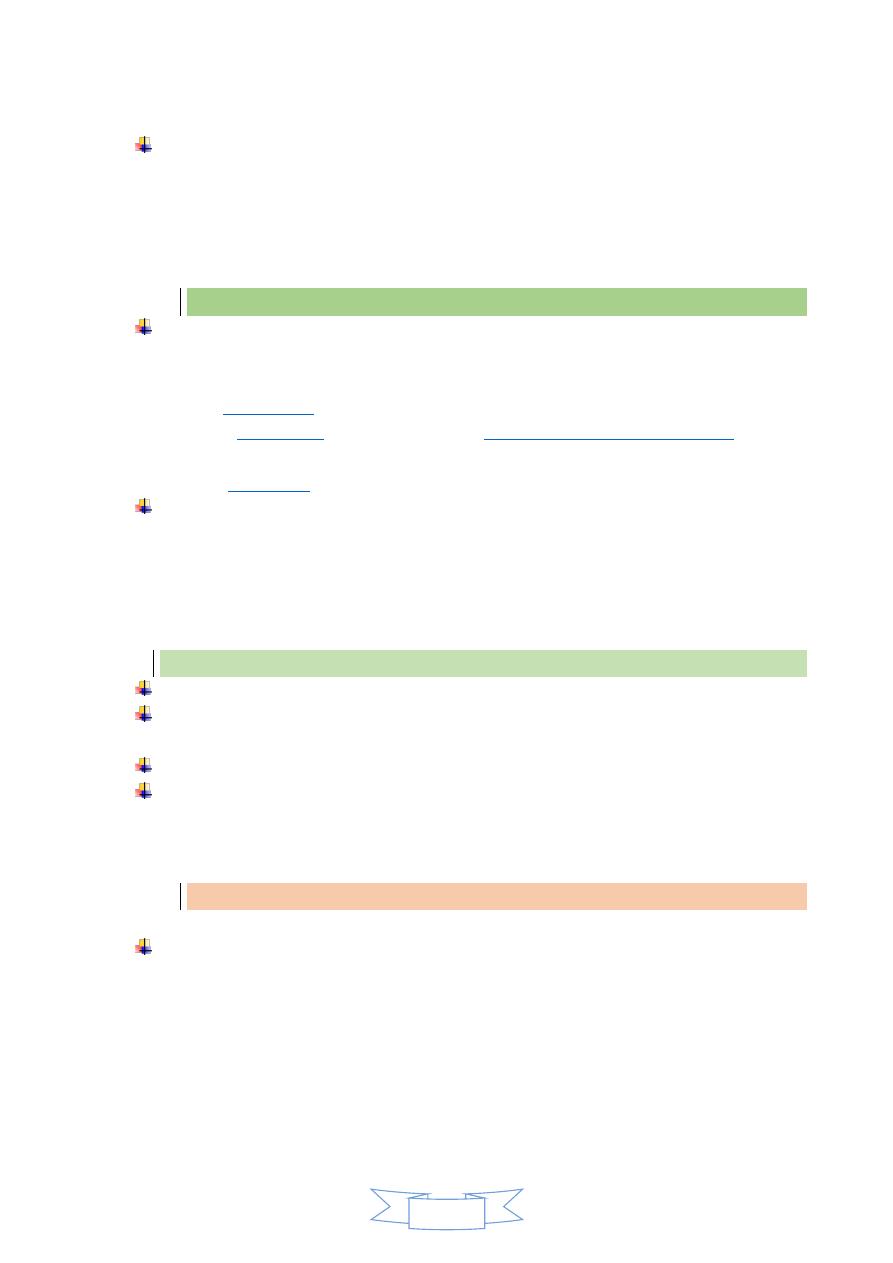
The bacteria varies from cocci to rods with short coccobacillary forms
predominating. They are gram-negative , aerobic, non-motile, Catalase and
oxidase are positive and non-spore-forming . They produce small, convex,
smooth colonies on enriched media in 2–5 days. Hydrogen sulfide is
produced by many strains, and nitrates are reduced to nitrites.
Differentiation among brucella species or biovars is made possible by their
characteristic sensitivity to dyes and their production of H2S.
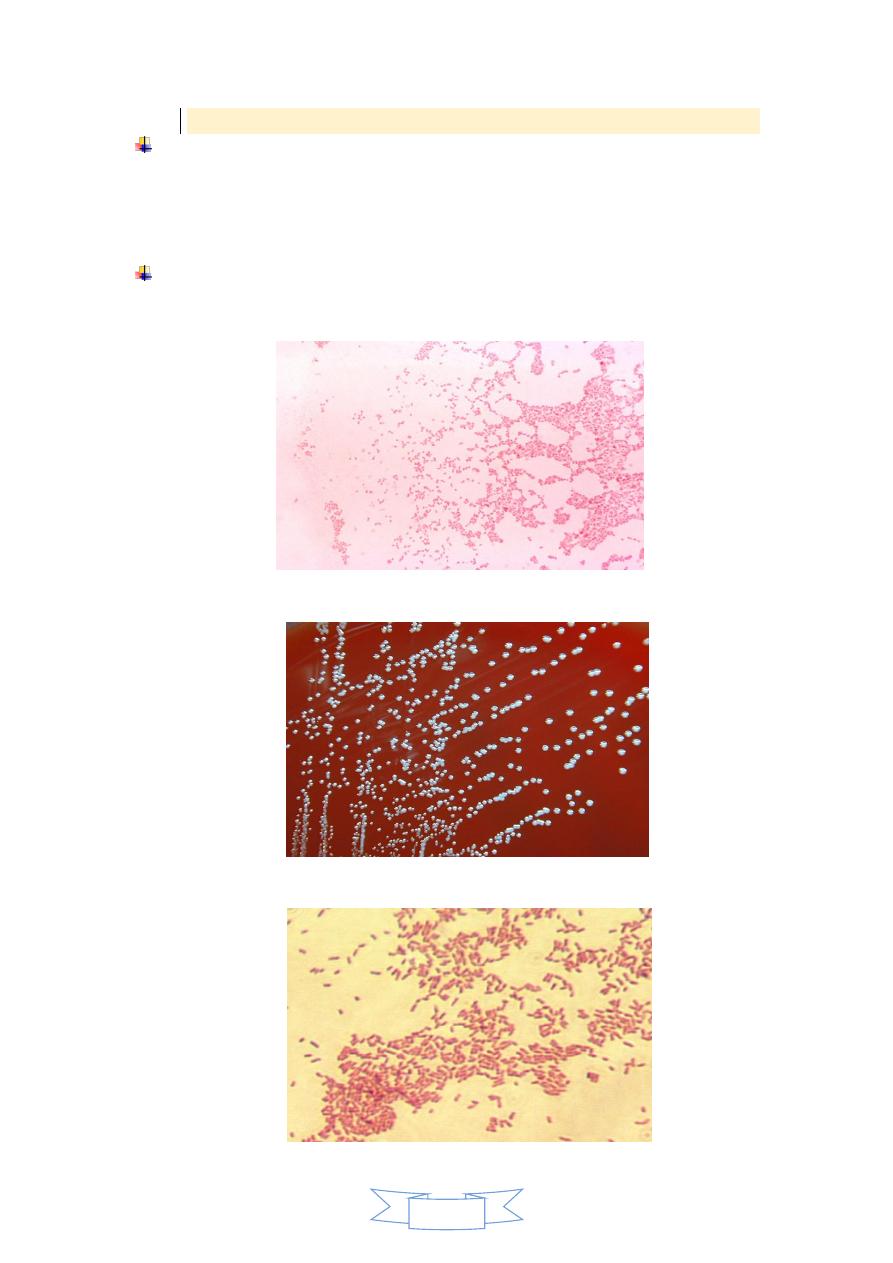
Gram negative of Brucella spp
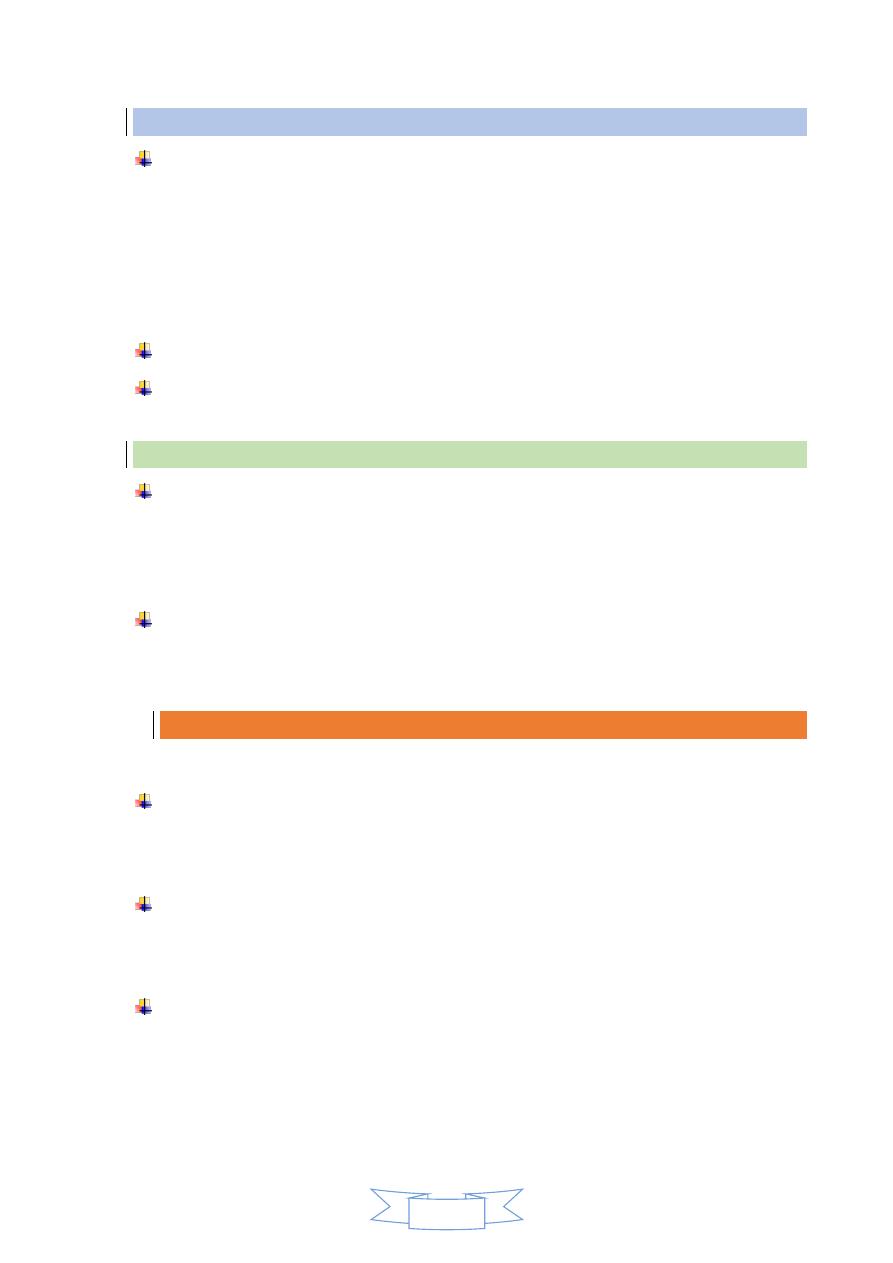
Colonies of brucella on enriched media
Brucella (gram stain) G-ve,
D.Haider L3
3
Pathogenesis & Pathology
The common routes of infection in humans are the intestinal tract (ingestion of
infected milk), mucous membranes (droplets), and skin (contact with infected
tissues of animals). The organisms progress from the portal of entry via lymphatic
channels and regional lymph nodes to the thoracic duct and the bloodstream which
distributes them to the parenchymatous organs. Granulomatous nodules that may
develop into abscesses form in lymphatic tissue, liver, spleen, bone marrow, and
other parts of the reticuloendothelial system.
Survive& Replicate within phagocytes&Monocytes
Infected macrophages localized within reticuloendothelial system(Granuloma
formation in spleen,liver,bone marrow)
Clinical Findings
The incubation period is 1–6 weeks. Early symptoms are malaise, fever, weakness,
aches, and sweats. The fever usually rises in the afternoon. There may be
gastrointestinal and nervous symptoms. Lymph nodes enlarge, and the spleen
becomes palpable. Hepatitis may be accompanied by jaundice. Deep pain and
disturbances of motion, particularly in vertebral bodies, suggest osteomyelitis.
Following the initial infection, a chronic stage may develop, characterized by
weakness, aches and pains, low-grade fever, nervousness, and other nonspecific
manifestations compatible with psychoneurotic symptoms.
Diagnostic Laboratory Tests:
֎ Specimens
Blood should be taken for culture, biopsy material for culture (lymph nodes,
bone, etc), and serum for serologic tests.
֎ Culture
Brucella agar , trypticase soy medium with or without 5% sheep blood, brain
heart infusion medium, and chocolate agar. Blood culture media readily grow
brucella species . All cultures incubate in 8–10% CO2 at 35–37 °C and observed for
3 weeks before being discarded as negative .
After a few days of incubation on agar media, the brucellae form colonies in the
primary streak that are < 1 mm in diameter , nonhemolytic. The observation of tiny
gram-negative coccobacilli that are H2S-production , catalase-positive and oxidase-
positive suggests brucella species. A positive urease test is characteristic of brucella
species.
D.Haider L3
4
֎ Serology
IgM antibody levels rise during the first week of acute illness, peak at 3 months,
and may persist during chronic disease. Even with appropriate antibiotic therapy,
IgG antibody levels rise about 3 weeks after onset of acute disease, peak at 6–8
weeks, and remain high during chronic disease. IgA levels parallel the IgG levels.
The usual serologic tests may fail to detect infection with B canis.
Treatment
The cornerstone of treatment for brucellosis is antibiotics. Because of the high
relapse rate associated with the disease, the use of a multidrug (two or more)
antibiotic regimen is recommended. The antimicrobials most commonly used
include
streptomycin,
rifampin
(Bactrim,
Septra). The combination of antibiotics used will vary based on disease severity,
age and
In general, a full six-week course of antibiotics is recommended, and prompt
treatment can lead to an improvement in symptoms and may also prevent the
complications associated with brucellosis. However, relapse rates of the disease
are still about 5%-10%, even with treatment. Depending on the severity of illness,
the associated complications (if any) and the timing of treatment, recovery may
take from a few weeks to a few months.
Brucell treatmen:
Doxycycline+rifampin
Trimethoprim-sulfamethoxazole for pregnant women and for children younger
than 8 years
6 weeks or longer
Fluoroquinolones, macrolides, penicillins, and cephalosporins either ineffective or
have unpredictable activity.
Epidemiology, Prevention, & Control
Brucellae are animal pathogens transmitted to humans by accidental contact with
infected animal feces, urine, milk, and tissues. The common sources of infection
for humans are unpasteurized milk, milk products and cheese and occupational
contact (eg, farmers, veterinarians, slaughterhouse workers) with infected animals.
Because of occupational contact, brucellae infection is much more frequent in
men.
D.Haider L3
5
Control rests on limitation of spread and possible eradication of animal infection,
pasteurization of milk and milk products, and reduction of occupational hazards
wherever possible.
Previous Exam
Q1: Discuss, Pseudomonas aeruginosa more dangerous
pathogen?
Q2: How can be distinguished between P.aeruginosa from
others Gram –negative bacteria?
Q3: Enumerate, main virulence factors of Pneumococcus, and
explain their functions?
