1
RNA NON-ENVELOPED VIRUSES
Picornaviruses
Picornavirusesrepresent a very large virus family with respect to the number of
members but one of the smallest in terms of virion size and genetic complexity.
They include two major groups of human pathogens: enteroviruses and
rhinoviruses.
Enteroviruses are transient inhabitants of the human alimentary tract and may be
isolated from the throat or lower intestine.
Rhinoviruses are isolated chiefly from the nose and throat
Properties Picornaviruses
They are small non-enveloped viruses
Icosahedral nucleocapsid.
Genome: Single-stranded RNA, linear, positive-sense, infectious when
purified
(Single stranded RNA POSITIVE POLARITY.)
Proteins: Four major polypeptides (VP1-4) cleaved from a large precursor
polyprotein
Replicate in the cytoplasm of the cell.
They are not inactivated by lipid solvent, such as ether, because they do not
have envelope.
PICORNAVIRUSE family includes three medically important genera;
enteroviruses, rhinoviruses and Hepatovirus (hepatitis A virus).
ENTEROVIRUSES:
RHINOVIRUS
Major group
Polioviruses types 1–3.
Coxsackieviruses A and B.
Echoviruses.
100 serotype
Infect the enteric tract
Found in the nose and throat
Replicate at 37◦C
Replicate at 33◦C
Stable at acid pH 3-5, so survive at
gastric acid
Acid labile
A. ENTEROVIRUSES
1. Poliovirus
Disease: POLIOMYELITIS

2
Poliomyelitis is an acute infectious disease that in its serious form affects the
central nervous system. The destruction of motor neurons in the spinal cord results
in flaccid paralysis. However, most poliovirus infections are subclinical.
There are three antigenic (serologic) types based on different antigenic
determinants on the outer capsid proteins. Because there is little cross reaction,
protection from disease requires the presence of antibody against each of the three
types.
Pathogenesis & Pathology
The mouth is the portal of entry of the virus, and primary multiplication takes place
in the oropharynx or intestine. The virus is regularly present in the throat and in the
stools before the onset of illness.
One week after infection the virus continues to be excreted in the stools for several
weeks even though high antibody levels are present in the blood.
It is believed that the virus first multiplies in the tonsils, the lymph nodes of the
neck, Peyer's patches, and the small intestine. The central nervous system may then
be invaded by way of the circulating blood.
Poliovirus can spread along axons of peripheral nerves to the central nervous
system, where it continues to progress along the fibers of the lower motor neurons
to increasingly involve the spinal cord or the brain. Poliovirus invades certain types
of nerve cells, and in the process of its intracellular multiplication it may damage
or completely destroy these cells.
Clinical Findings
When an individual susceptible to infection is exposed to the virus, the response
ranges from inapparent infection without symptoms, to a mild febrile illness, to
severe and permanent paralysis. Most infections are subclinical; only about 1% of
infections result in clinical illness.The incubation period is usually 7–14 days
1-Mild Disease
This is the most common form of disease. The patient has only a minor illness,
characterized by fever, malaise, drowsiness, headache, nausea, vomiting, Recovery
occurs in a few days.
2-Nonparalytic Poliomyelitis (Aseptic Meningitis)
In addition to the symptoms and signs listed in the preceding paragraph, the patient
with the nonparalytic form has stiffness and pain in the back and neck. The disease
lasts 2–10 days, and recovery is rapid and complete.
3-Paralytic Poliomyelitis
The predominating complaint is flaccid paralysis resulting from lower motor
neuron damage. Maximal recovery usually occurs within 6 months, with residual
paralysis lasting much longer.
4-Progressive Postpoliomyelitis Muscle Atrophy
Laboratory Diagnosis

3
1. The virus may be recovered from throat swabs taken soon after onset of illness
and from rectal swabs or stool samples collected over long periods.
2. An isolated virus is identified and typed by neutralization with specific
antiserum. Paired serum specimens are required to show a rise in antibody titer
during the course of the disease.
3. Virus can also be identified by polymerase chain reaction (PCR) assays.
2. Coxsackieviruses
Disease: They cause a variety of disease
Group A Coxsackieviruses: acute hemorrhagic conjunctivitis and hand-foot-mouth
disease.
Group B Coxsackieviruses: myocarditis and pericarditis.
Both can cause non-specific upper RT disease, febrile rashes, and aseptic
meningitis.
Transmission & Epidemiology: Coxsackieviruses can be transmitted by fecal-
oral route, but respiratory aerosols also play a role.
Pathogenesis & Pathology: Virus has been recovered from the blood in the early
stages of natural infection in humans. Virus is also found in the throat for a few
days early in the infection and in the stools for up to 5–6 weeks. Virus distribution
is similar to that of the other enteroviruses.
Clinical Findings
A. Group A Specific Diseases:
Herpangina : fever, sore throat, and tender vesicles in oropharynx.
Hand-foot-mouth Disease: vesicular rash on the hands and feet and ulceration in
the mouth.
B. Group B Specific Diseases:
Pleurodynia: fever and severe pleuritic chest pain
Myocarditis and pericarditis
Diabetes: the v suspected to have a role in juvenile diabetes in humans.
C. Diseases Caused by both Group:
Aseptic meningitis.
Upper respiratory tract infections with or without rash
3. ECHOVIRUSES:
Disease: viruses cause variety of diseases such as aseptic meningitis, upper
respiratory infection, febrile illness with or without rash, infantile diarrhea, and
hemorrhagic conjunctivitis.
They are transmitted by fecal-oral route.
They are one of the leading cause of aseptic (viral) meningitis
4
RNA NON-ENVELOPED VIRUSES
Reoviruses, Rotaviruses, & Caliciviruses
Reoviruses
Reoviruses are medium-sized viruses with a double-stranded, segmented RNA
genome. The family includes human rotaviruses, the most important cause of
infantile gastroenteritis around the world
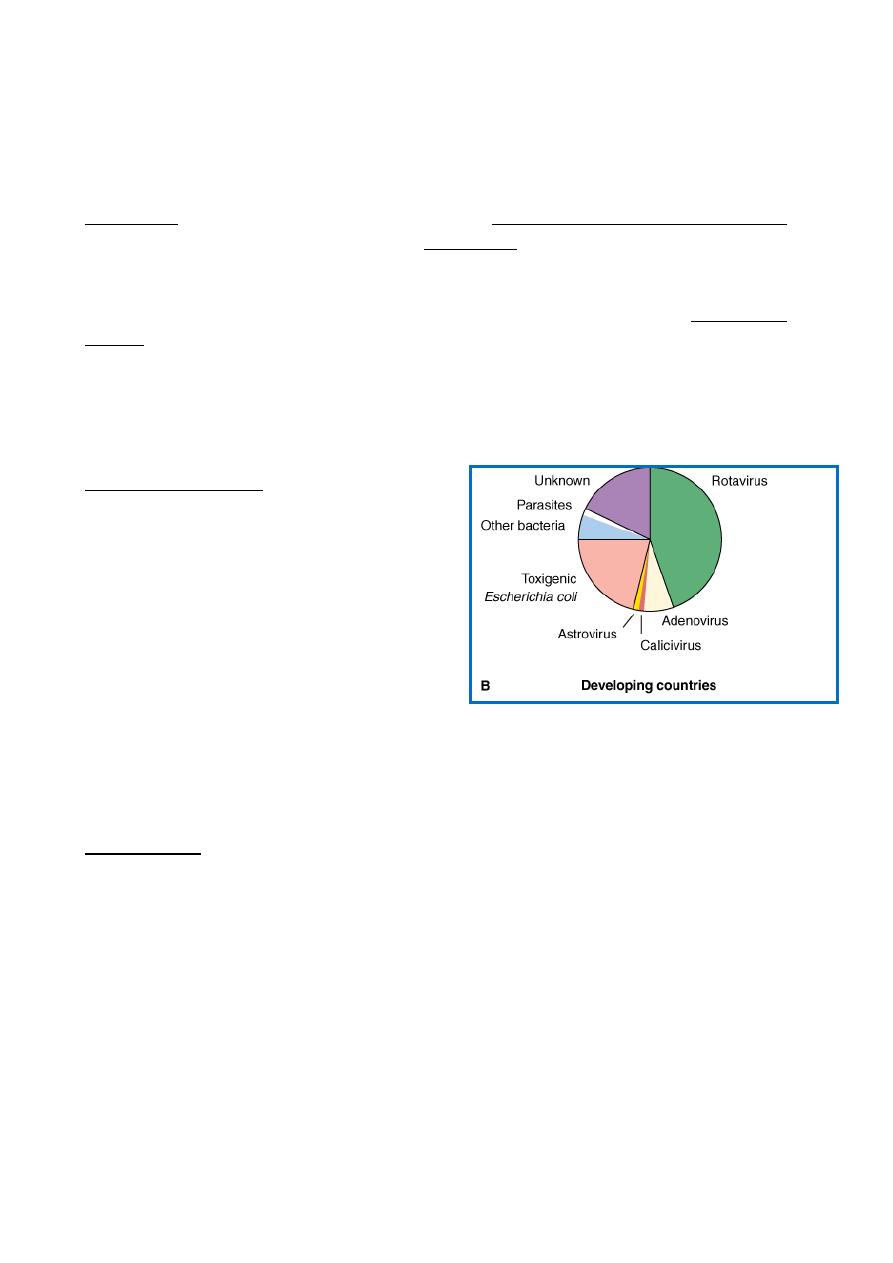
Acute gastroenteritis is a very common disease with significant public health
impact. In developing countries it is estimated to cause as many as 1.5 million
deaths of preschool children annually
An estimate of the role of etiologic agents in severe diarrheal illnesses requiring
hospitalization of infants and young children
Rotavirus
Important properties: They are composed
of:
Segmented double-stranded RNA genome
Double-layered icosahedral capsid without
envelope.
RNA-dependent RNA polymerase.
Rotaviruses have been classified into five
species (A–E). Group A rotaviruses are the
most frequent human pathogens
Outer capsid proteins VP4 and VP7 carry
epitopes important in neutralizing activity, with VP7 glycoprotein being the
predominant antigen.
Five serotypes are responsible for the majority of human disease. Serotype
distributions differ geographically
Transmission and epidemiology: The rotavirus transmitted by the fecal-oral route.
Pathogenesis
Rotaviruses infect cells in the villi of the small intestine (gastric and colonic
mucosa are spared).
They multiply in the cytoplasm of enterocytes and damage their transport
mechanisms.
One of the rotavirus proteins, NSP4, is a viral enterotoxin and induces secretion by
triggering a signal transduction pathway.
Damaged cells may slough into the lumen of the intestine and release large
quantities of virus, which appear in the stool
Viral excretion usually lasts 2–12 days in otherwise healthy patients but may be
prolonged in those with poor nutrition.
5
Diarrhea caused by rotaviruses may be due to impaired sodium and glucose
absorption as damaged cells on villi are replaced by non-absorbing immature crypt
cells. It may take 3–8 weeks for normal function to be restored
Clinical Findings
Rotaviruses cause the major portion of diarrheal illness in infants and children
worldwide but not in adults.
The incubation period is 1–3 days.
Typical symptoms include watery diarrhea, fever, abdominal pain, and vomiting,
leading to dehydration.
In infants and children, severe loss of electrolytes and fluids may be fatal unless
treated
Epidemiology
Rotaviruses are the single most important worldwide cause of gastroenteritis in
young children.
Typically, up to 50% of cases of acute gastroenteritis of hospitalized children
throughout the world are caused by rotaviruses.
Rotavirus infections usually predominate during the winter season. Symptomatic
infections are most common in children between ages 6 months and 2 years, and
transmission appears to be by the fecal–oral route. Nosocomial infections are
frequent
Treatment & Control
Treatment of gastroenteritis is supportive, to correct the loss of water and
electrolytes that may lead to dehydration, acidosis, shock, and death. Management
consists of replacement of fluids and restoration of electrolyte balance either
intravenously or orally, as feasible.
An oral live attenuated rotavirus vaccine was licensed in the United States in 1998
for vaccination of infants. It was withdrawn a year later because of reports of
intussusception (bowel blockages) as an uncommon but serious side effect
associated with the vaccine.
In 2006, an oral pentavalent bovine-based rotavirus vaccine was licensed in the
United States, which is not associated with intussusception.
A safe and effective vaccine remains the best hope for reducing the worldwide
burden of rotavirus disease
