
1
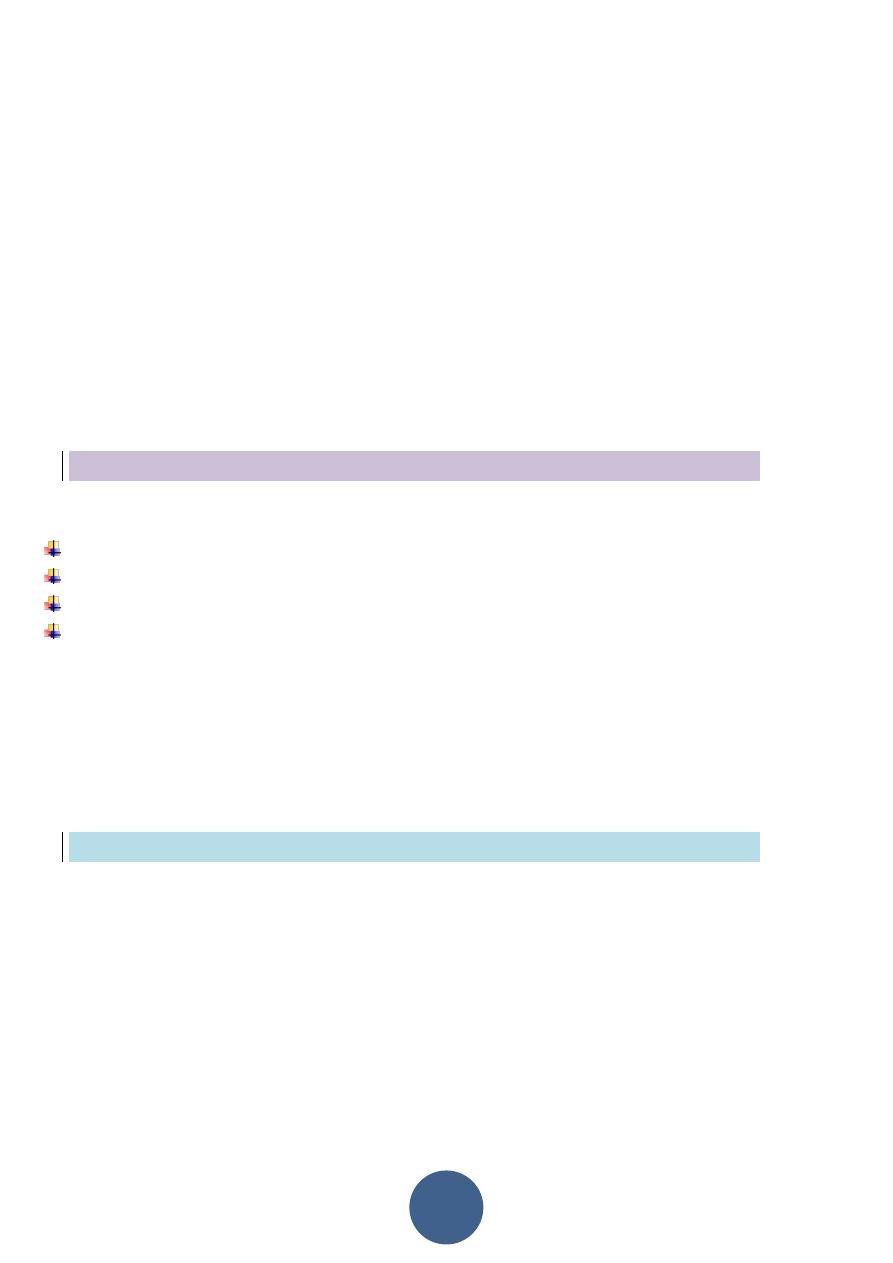
Tumors ovary
The 3 cell types of ovary form potential for large number of tumors and neoplasms
and these types are:-
1- Multipotential surface (coelomic) ovarian epithelium.
2- Germ cells.
3- Sex-cord-stromal cells.
Surface epithelial origin cells are the most common which's constitute over than 90%
of ovarian neoplasms.
The surface epithelial – stromal cells are:
1-
Serous tumor:
which's subdivided into:
a-benign cystadenoma .
b-borderline tumors (serous borderline tumor) .
c-malignant (serous adenocarcinoma).
2-
Mucinous tumor
:
which's subdivided into:
a-benign cystadenoma .
b-borderline tumors (mucinous borderline tumor) .
c-malignant (mucinous adenocarcinoma).
3-
Endometrioid tumor:
which's subdivided into:
a-benign cystadenoma .
b-borderline tumors (endometroid borderline tumor) .
c-malignant (endometroid adenocarcinoma).
4
- Clear cells tumor:
which's subdivided into:
a-benign .
b-borderline tumors .
c-malignant ( clear cell adenocarcinoma)
2
5-
transitional cell tumors:
which's subdivided into:
a-Brenner tumor.
b-Brenner tumor of borderline malignancy.
c-malignant Brenner tumor.
d-transitional cell carcinoma (non-Brenner tumor).
6-epithelial- stromal:
a-adenocarcinoma.
b-carcinosarcoma (formerly mixed mullerian tumor)
Germ cell origin are:
1- Teratoma. which's subdivided into :
immature.
mature.
solid.
cystic (dermoid cyst).
2- Dysgerminoma.
3- monodermal (struma ovarii, carcinoid)
4-yollk sac tumor.
5-mixed germ cell tumors.
Sex cord – stroma :
1- Fibroma.
2- Granulosa – theca cell tumor:- this tumor usually hormonally active and secrete
large amount of estrogen so cause endometrial and breast cancer.
3- Sertoli – Leydig cell tumor.
3
Metastasis carcinoma:-
This occur in older age group and usually come from breast, lungs and GIT.
Serous tumor:-
These are most frequent of the ovarian tumors, it's usually cystic so known as
cystadenoma for benign tumor and cystadenocarcinoma for malignant one and
borderline or recently named as tumor of low malignant potential for borderline
tumor between benign and malignant.
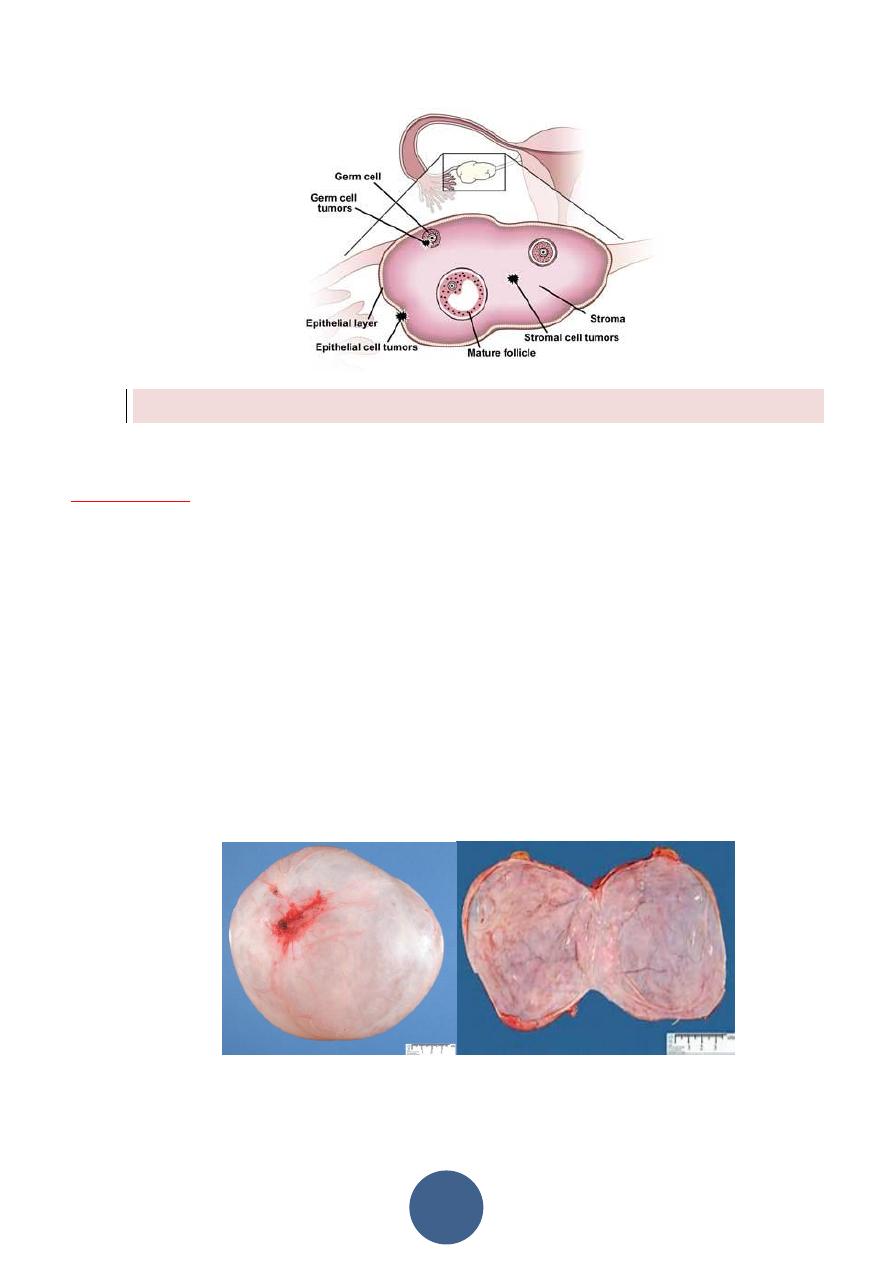
Morphology:-
Grossly:
serous tumor may be small 5 to 10 cm or may reached even 40 cm in
diameter, the surface in benign one is smooth and glistening while in malignant one is
irregular cut section reveal usually unilocular cyst (single cavity) filled by serous fluid
and smooth inner surface in benign one while in malignant tumor the inner surface
usually contain polypoid and papillary growth.
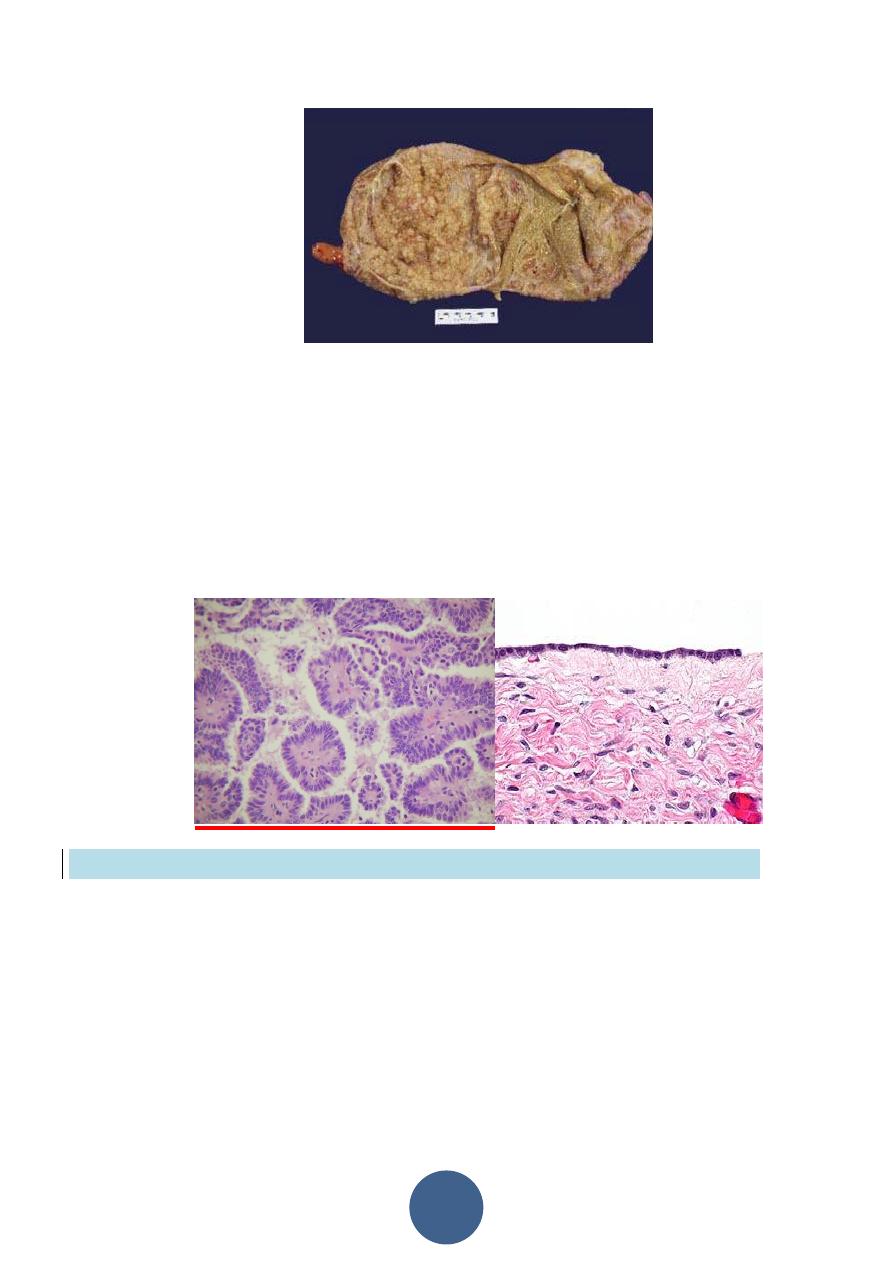
4
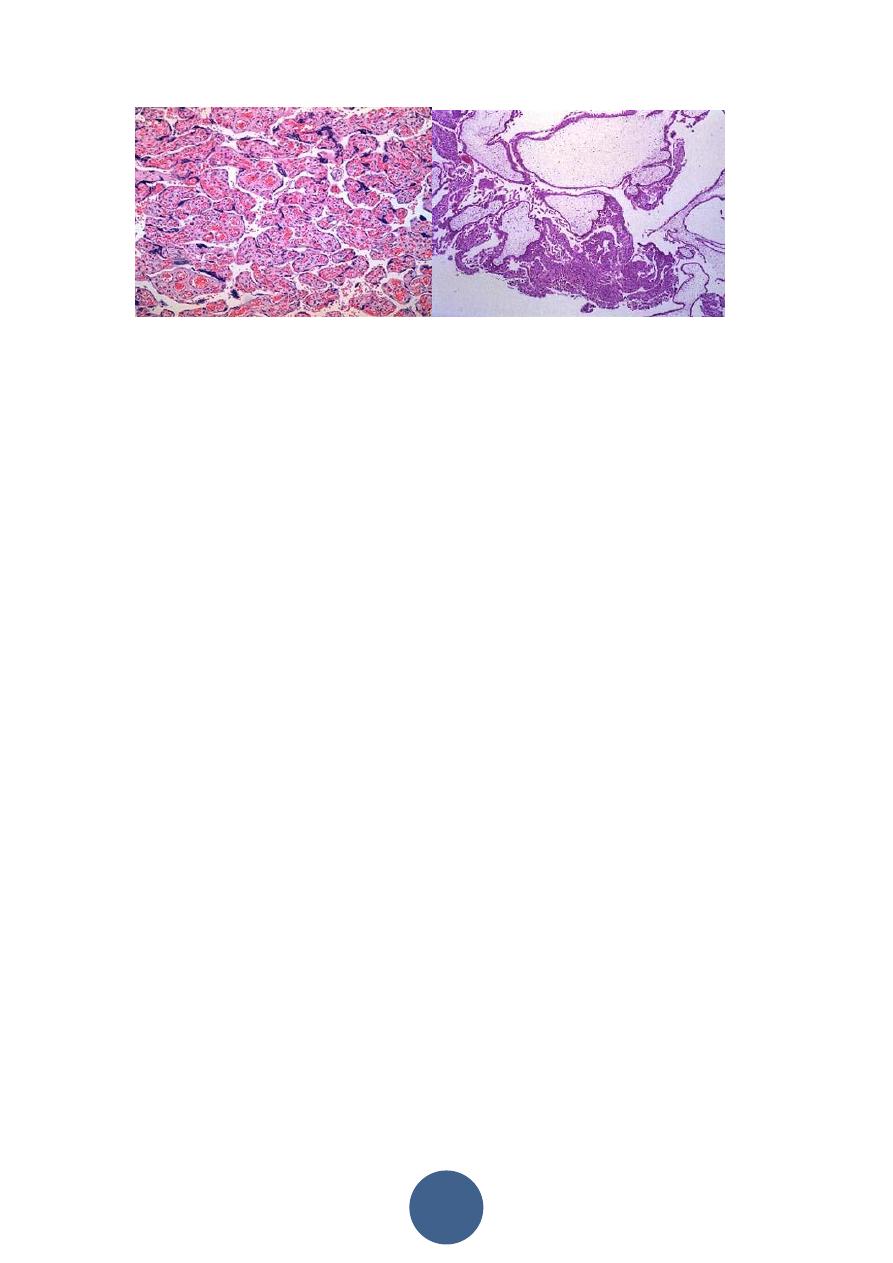
Microscopically:
in benign one usually consist of thin wall lined by single layer of tall
columnar serous epithelial cells.
While in malignant one usually composed of complex papillae lined by multilayring
atypical malignant cells with invasion of stroma, in borderline the atypia of lining
papillae are present but no stromal invasion seen.
The metastasis of this tumor is usually by local invasion of wall and implant itself in
peritoneal cavity so associated with ascitis.
Mucinous tumor
This usually analogous to serous tumor but it's usually larger than serous cyst and
multilocular, it's lined by mucous secreting cells as endocervical cells.
Grossly:
it can't be differentiated from serous cysts but on cut section reveal mucinous
thick material.
Microscopically:
in benign tumor, it consist of thin wall lined by single layer of mucous
secreting cells which consist of apical vacuoles and basal located nuclei, in malignant
one also consist of complex papillae lined by multilayering malignant cells with
stromal invasion which's not seen in borderline tumor.

5
The metastasis or rupture of mucinous cystadenocarcinoma may give rise to
pseudomyxoma peritonii, that the peritoneal cavity becomes filled with mucinous
material with multiple implants on serosal surface so abdominal viscera become
matted together.
Other ovarian tumors:
Teratomas
It's divided into:-
1- Mature (benign teratoma).
2- Immature (malignant teratoma).
Benign (Mature teratoma)
these tumors arise from totipotential germ cells to give
origin of 3 embryonal layers:
1- Ectodermal 2- Mesodermal 3- Endodermal
The more common take the differentiation of ectodermal totipotential germ cells,
which also this teratoma can contain teeth, bone, cartilage, nests of bronchial or
gastrointestinal epithelium even brain tissue.
6
Immature teratoma:-
It usually occur in younger age group than mature, it's bulky and solid.
Micrscopically
consist of different tissues as undifferentiated and immature may be in
one element only especially in neuroepithelial cells.
Diseases of pregnancy:-
Ectopic pregnancy:-
Defined as implantation of fertilized ovum in any site other than normal uterine
location, this condition occur in 1% of pregnancy.
Location:-
1- Over 90% of the implantation occur in oviduct (tubal pregnancy).
2- Other sites are ovaries, abdominal cavity and intrauterine portion of oviducts.
This occur because of retards passage of the ovum along its normal course through
the oviducts to the uterus.
In half cases the delay passage of ovum have no anatomic causes.
But other 50% occur due to:
1- Chronic inflammation.
2- Intrauterine tumor.
3- endometriosis.
Morphology:-
In tubal pregnancy there's usually dilatation of F.T which's may reach 3 to 4 cm in
diameter cut section show blood clot with bits of grey placental tissue and fetal parts.
Microscopically:-
There's decidual reaction of stroma with presence of placental villi and rarely can be
seen fetal parts because the poor attachment of the placenta to the tubal wall result
in death of the embryo and proteolysis.

7
Gestational trophoblastic disease:-
The gestational trophoblastic tumor divided into 3 categories arrange according to
level of aggressiveness:
1- hydatiform mole complete and partial.
2- Invasive mole.
3- Choriocarcinoma.
1- Hydatiform mole:-
It's known aswollen, cystically dilated, chorionic villi appear grossly as a grape like
structures. The complete mole does not perm it embryogenesis and therefore never
contain fetal parts or normal villi and this cause by empty egg fertilized by 2
spermatozoa.
So the epithelial cells carry diploid karyotype (46, xx or 46 xy).
While partial mole contain fetal parts and normal villi with abnormal one, which is
resulting from a normal egg is fertilized by 2 spermatozoa so it carries triploid
karyotype (69 xxy).
Morphology:-
Grossly:
the uterine cavity it's filled by thin- walled translucent cystic structures grape-
like.
Microscopically:
in complete mole all the villi are showing hydropic dilatation with
absence of vascularization and lined by proliferate cyto and syncytial trohoblast.
8
While in partial mole some of villi are normal other are dilated with less proliferation
of trophoblastic cells.
Invasive mole:-
The mole retains the hydropic villi with hyperplastic and atypical changes of
epithelium, the villi invade deeply the muscular layer of uterus and can reach the
vagina or broad ligament by local spread but metastasis do not occur.
Choriocarcinoma:-
This is a very aggressive malignant tumor arise from gestational chorionic epithelium
or less frequently from totipotential cells within the gonads.
This neoplasm occur in female below age of 20 and over age of 40.
Usually occur
50%
after complete mole and less partial mole,
25%
after abortion and
remainder percentage after normal pregnancy.
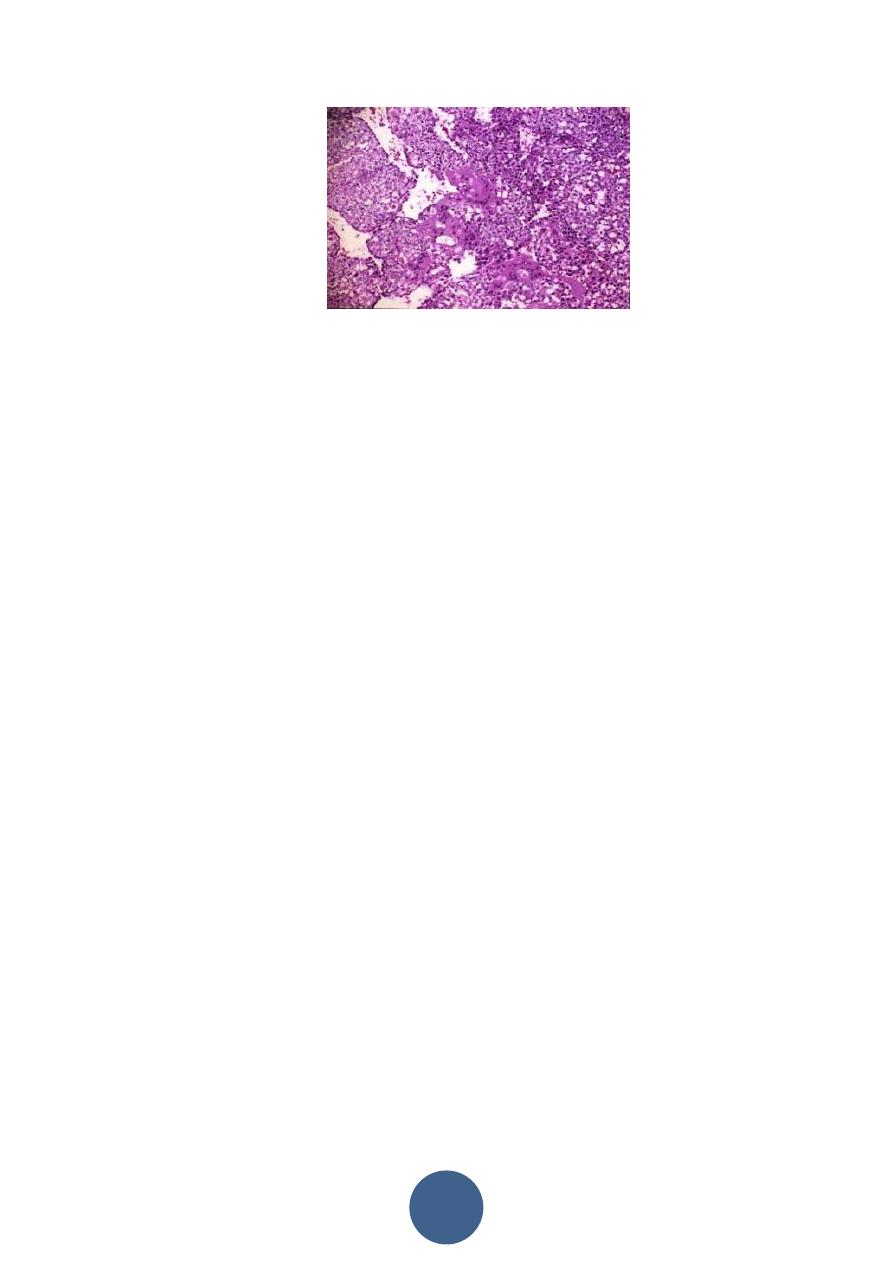
Microscopically:
it's seen as very hemorrhagic necrotic masses within the uterus,
sometimes the necrosis is complete to destruct the primary neoplasm and remain
only the metastasis, in contrast to H.mole chorionic villi are not formed and consist
from only malignant cyto and syncitiotrophoblast and this tumor is wide spread by
blood but lymphatic invasion is not common.
9
This tumor has very good response to chemotherapy. Nearly 100% of cases have been
cured and even healthy infants born to the survivors.
