Adult Respiratory Distress Syndrome
BackgroundAdult respiratory distress syndrome (ARDS) is an acute diffuse alveolar damage (DAD) diffuse pulmonary parenchymal injury associated with noncardiogenic pulmonary edema and resulting in severe respiratory distress and hypoxemic respiratory failure.
Characteristic Features
Acute onsetBilateral infiltrates
Pulmonary artery wedge pressure less than 19 mm Hg (or no clinical signs of congestive heart failure)
PaO2/FIO2 ratio less than 200 (ARDS) or less than 300 (acute lung injury [ALI]): which is a milder clinical expression of the injury of ARDS that may or may not progress to ARDS.
Pathophysiology
:DAD is caused by inflammatory reaction mediated byReactive Oxygen Radicals
Proteolytic Enzymes from Neutrophils.Cytokines
Complement
Loss of the integrity of the alveolar-capillary barrier
Exudation of protein-rich fluid across the barrier,
Pulmonary edema
Hypoxemia from intrapulmonary shunting.
History
ARDS can follow a variety of pulmonary or nonpulmonary insults, and the presence of such factors should alert physicians to the potential for development of ARDS.Onset of symptoms in ARDS can follow the predisposing condition from 4 hours to several days; thus, the timing of symptom onset may vary greatly.
Dyspnea is present in all cases except those in which alteration in sensorium is present.
Other symptoms, if present, typically are related to the predisposing condition.
Physical
: Findings on physical examination are not specific for ARDS and can be found in pulmonary edema of any cause.
Dyspnea and tachypnea
Cyanosis and sweating
Tachycardia
Scattered crackles
Agitation
Lethargy followed by obtundation
Causes
Infection - Pneumonia of any etiology (especially viral) and systemic sepsis (especially gram negative)
Shock - Any type, particularly septic and traumatic shock
Aspiration - Gastric contents, near drowning, and toxic inhalationTrauma - Pulmonary contusion, fat embolization, and multiple trauma
Other - Systemic inflammatory response syndrome, pancreatitis, postcardiopulmonary bypass, massive blood transfusion, drug ingestion (eg, heroin, methadone, barbiturates, salicylates)Differential diagnosis
Cardiogenic pulmonary edemaFulminant pneumonia
Pulmonary embolism
Acute on chronic severe respiratory illnesses
Lab Studies
Arterial blood gases analysis (ABGs)Hypocapnia is a typical finding early in ARDS, but hypercapnia can be seen later as ventilatory failure progresses.
PaO2 less than 50 mm Hg with an FIO2 more than 0.6
Other laboratory studies are nonspecific and are obtained as indicated by the underlying or predisposing
Imaging Studies
The chest radiograph reveals characteristic diffuse bilateral alveolar-interstitial infiltrates.In early cases, the radiographic findings may not be fully developed.
Additional localized pulmonary findings may be present if the predisposing condition involves a pulmonary process.
Chest CT may be helpful in advanced cases but is not necessary for diagnosis.
Echocardiography may be helpful to exclude a cardiogenic etiology for pulmonary edema.
Management
Usually at RCUAirway and ventilation support and oxygenation are the initial priorities of management
Mechanical ventilation with positive end-expiratory pressure (PEEP)
Treatment of the underlying condition
Cautious use of antibiotic and I.V. fluid
Complications
Multiple organ failurePermanent lung disease
Oxygen toxicity
Barotrauma
Superinfection
Prognosis
Mortality rate averages 60%.Nonsurvivors usually die from sepsis or multiple organ failure.
Survivors usually have a good outcome with minimal, if any, persistent pulmonary symptoms.
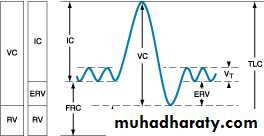
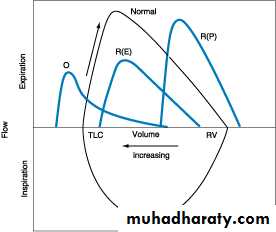
Survivors of severe cases may have some degree of permanent pulmonary fibrosis and symptoms of restrictive lung disease.