
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
1
Plasma membrane: phospholipid bilayer with embedded proteins
Nucleus: chromatin (euchromatin vs heterochromatin).
Mitochondria: oxidative phosphorylation (main source of ATP).
Endoplasmic reticulum (ER), Ribosomes & Golgi Apparatus:
RER & Golgi - synthesis and packaging of proteins for export.
SER - lipid biosynthesis, detoxification of harmful compounds.
Lysosomes: enzymatic (acid hydrolases) digestion of materials in the cell.
Cytoskeleton: structure and movement of cells:
1- Microfilaments: actin in various forms! cell shape.
2- Microtubules: tubulin! organelle movement (flagella/cilia/ mitotic
spindle).
3- Intermediate filaments: cytokeratins, vimentin, desmin (neurofilament
proteins).
Peroxisomes: enzymes (e.g. catalase, oxidases)! metabolism of hydrogen
peroxide & fatty acids.
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
2
Pathology
is the study of disease, the word pathology is derived from two root
words:
Pathos
, which means “suffering” or “disease,” and
Logos
, which means
“the study of”. This study of disease (
Pathology
) may be divided into four main
parts:
1.
The study of the cause
, or
Etiology
of disease, which may be genetic or
acquired. Genetic etiologies arise from changes within genes, whereas
acquired etiologies refer to disease caused by outside sources, such as
bacterial or viral infections or metabolic or nutritional disorders.
2.
The study of mechanisms in the development of disease
, or
Pathogenesis
. This
describes the sequence of events at the cell and tissue level as a disease
expresses itself. Pathogenesis includes factors that influence the development
of a disease which known as
Pathogenicity
.
3.
The study of morphological alterations in tissues that occur with disease
, or
Lesions
. Lesions give rise to functional disturbances. These disturbances
serve to distinguish one disease from another and occasionally may be
diagnostic of an etiological agent. The alteration of tissue is studied by:
(1)
Gross or macroscopic examination (lesion) with naked eye,
(2)
Microscopic (lesion) examination by light microscopy, and
(3)
Ultrastructural examination by electron microscopy.
4.
The study of the functional consequences of lesions that give rise to signs or
symptoms of disease;
known as
Diagnosis
. A diagnosis is achieved when the
precise nature of the lesions causing the symptoms is recognized.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
3
1) Homeostasis:
Cells are able to maintain normal structure and function (e.g. ion
balance, pH, energy metabolism) in response to normal physiologic demands.
2) Cellular Adaptation:
Cells encounter some stresses (e.g. excessive physiologic
demand or some pathologic stimuli) they may make functional or structural
adaptations to maintain homeostasis. Cells may respond to these stimuli by
either
increasing
or
decreasing
their content of specific organelles (
atrophy
,
hypertrophy
,
hyperplasia
and
metaplasia
).
3) Cell Injury:
if the limits of adaptive response are exceeded, or in certain
instances when adaptation is not possible (e.g. with severe injurious stimulus),
a sequence of events called cell injury occurs.
a) Reversible Cell Injury:
Removal of injurious agent results in complete
restoration of structural and functional integrity as in
Degeneration
.
b) Irreversible Cell Injury (Cell Death):
If injurious agent persists (or severe
enough from the start) the cell will suffer irreversible cell injury lead to cell
death. It’s types:
-Necrosis:
Type of cell death characterized by severe membrane injury and
enzymatic degradation which is a pathologic process.
-Apoptosis:
Regulated form of cell death that can be physiologic or
pathologic process.
- Autophagy
: Natural, regulated, destructive mechanism of the cell that
disassembles unnecessary or dysfunctional components allows the
orderly degradation and recycling of cellular components.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
4
1) Atrophy:
Decrease in either the number of cells and/or the size of the cells (results in
decrease in size of the organ / structure). Atrophic cells are not dead or necessarily
badly injured but they have a reduced functional capacity. Given enough time and
removing the reason for cellular atrophy, the cells can return too normal.
- Etiology
1- Decreased workload.
2- Loss of innervation (denervation atrophy), and nerve compression.
3- Loss of hormonal stimulation (trophic).
4- Reduced blood supply / hypoxia, inadequate nutrition.
5- Persistent cell injury,
6- Aging (senile atrophy).
- Gross Appearance: tissue/organ is decreased in size.
- Microscopic Appearance: cells are smaller than normal
2) Hypertrophy:
Increased in size of tissue due to an increase in cell size without cellular
proliferation, mostly seen in tissues which have minimal proliferative capacity
(cardiac and skeletal muscle).
- Etiology
1- Increased work load:
a- Physiologic: Increase in muscles size due to exercise.
b- Pathologic: Heart failure.
2- Hormonal signals:
a- Physiologic: Uterus in pregnancy.
b- Pathological: Myocardial hypertrophy in hyperthyroid cats.
3- Certain drugs or toxins as in phenobarbital.
- Gross Appearance: tissue and organ increased in size and weight.
- Microscopic Appearance: cellular enlargement due to a proportional increase
in the number and size of organelles.
3) Hyperplasia:
Increase in organ size or tissue mass due to increase in the number of cells,
mostly seen in tissue cells that have ability to proliferation.
4) Hypoplasia:
Incomplete development or underdevelopment of an organ or tissue.
5) Aplasia:
Lack of development of an organ or tissue.
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
5
6) Metaplasia:
Adaptive response in which a different but related type replaces one type of
mature differentiated cell. It is usually reversible and is most commonly seen
from more specialized to less specialized but more resistant cell type (e.g.,
columnar or transitional cell type to squamous epithelia). Metaplasia occurs
following prolonged irritation or chronic infection (e.g., stones in urinary ladder),
and in nutritional deficiencies (e.g., Vitamin A deficiency cause squamous cell
metaplasia of prostate gland).
7) Dysplasia:
Literally means "abnormal growth" it is a proliferative response
accompanied by loss of regular differentiation and by cellular atypia and
disorderliness. These changes most frequently are observed in epithelia subjected
to chronic irritation or inflammation. Cellular atypia is characterized by
Pleomorphism
(variation in size and shape) and
Hyperchromicity
(increased
staining). Dysplasia is however reversible if the cause is removed or the dysplasia
may progress to become neoplasms.
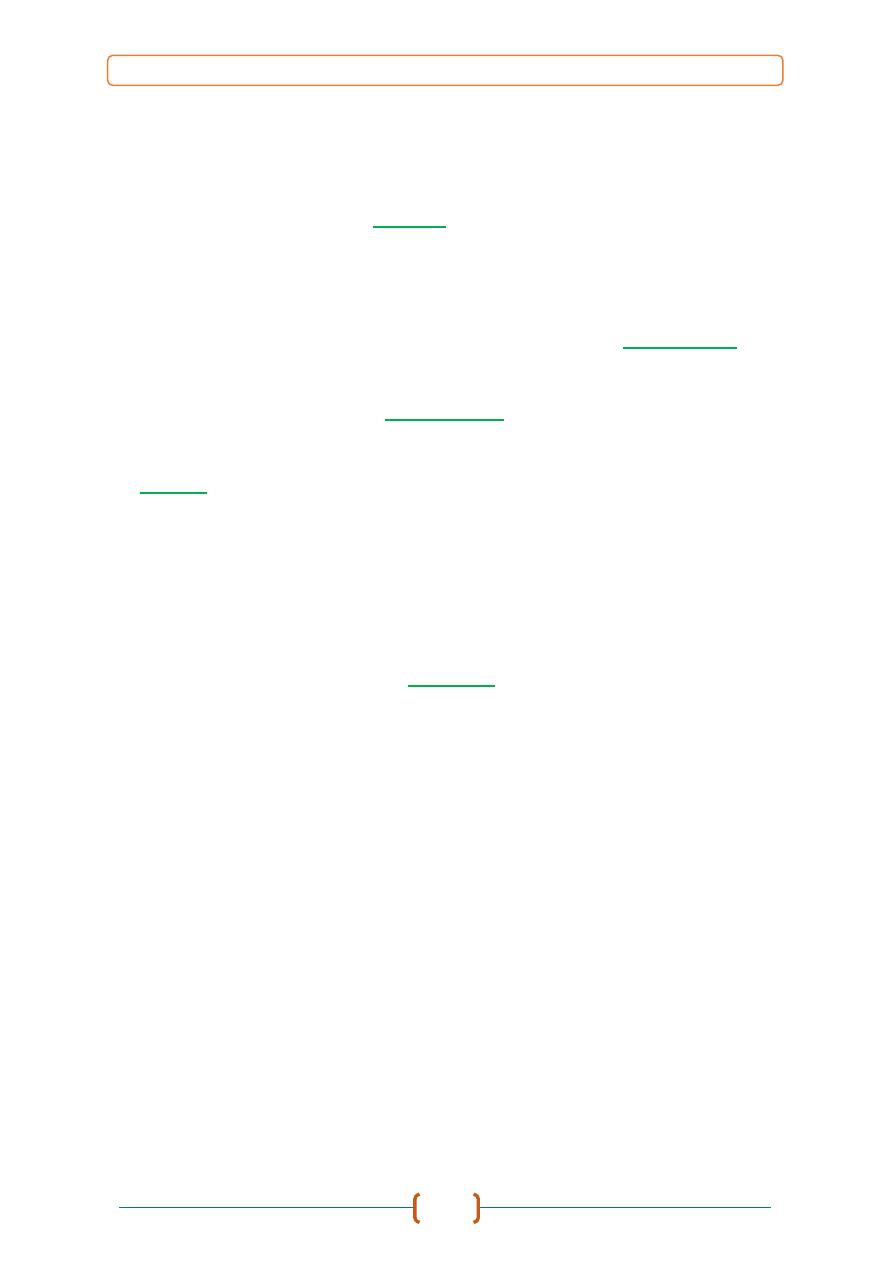
Figure show Type of
Cellular Adaptations

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
6
1) Hypoxia:
One of the most important and common causes of cell injury and cell death
cause impairment of oxidative respiration.
a)
Deficient blood supply.
b)
Reduced oxygen-carrying capacity of the blood.
c)
Interference with respiratory chain / oxidative phosphorylation.
2) Physical agents
a)
Direct mechanical trauma:
lacerations or crush injuries.
b)
Temperature extremes:
heat (thermal burn), cold (frostbite).
c)
Radiation:
radioactive isotope or electromagnetic radiation (UV, x-rays).
d)
Electric Shock.
e)
Sudden changes in atmospheric pressure.
3) Chemicals, Drugs & Toxins
a)
Inorganic poisons:
e.g. lead, copper, arsenic, selenium, mercury, etc.
b)
Organic poisons:
e.g. nitrate/nitrite, oxalate, hydrocyanic acid, etc.
c)
Manufactured chemicals:
e.g. drugs, pesticides, herbicides, rodenticides.
d)
Physiologic compounds:
salt, glucose, oxygen, etc.
e)
Plant toxins:
e.g. ragwort, sweet clover, braken fern, etc.
f)
Animal toxins:
e.g. snake or spider venom, tick toxin, etc.
g)
Bacterial toxins:
e.g. botulinum toxin, aflatoxin, ergot, etc.
4) Infectious agents
a)
Viruses.
b)
Bacteria / rickettsiae / chlamydia.
c)
Fungi.
d)
Protozoa.
e)
Metazoan parasites.
5) Immunologic Reactions
a)
Immune response:
e.g. cells damaged in immune / inflammatory response.
b)
Hypersensitivity (allergic) reactions:
to a foreign protein or drug.
c)
Autoimmune diseases:
reactions to self-antigens.
6) Genetic abnormalities
a)
Cytogenetic disorders.
b)
Mendelian
disorders (mutant genes)
c)
Multifactorial.
7) Nutritional Imbalances
a)
Deficiencies:
deficiencies of protein-calories, vitamins, minerals.
b)
Over nutrition:
e.g. excess lipids and calories (obesity), diabetes,
atherosclerosis, etc.
8) Cell Aging:
The cumulative effects of a life time of cell damage (chemical, infectious,
nutrition, etc.) leads to a diminished in the capacity of aged cells and tissues to
maintain homeostasis and adapt to harmful stimuli.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
7
1- Water Overload:
a- Cell Swelling.
b- Hydropic Degeneration.
c- Vacuolar Degeneration.
d- Ballooning Degeneration.
2- Metabolic Overload:
a- Fat Overload
- Fatty Degeneration.
- Fatty Infiltration.
- Fatty Change.
b- Protein Overload:
- Cloudy Cell Swelling.
- Hyaline Degeneration.
- Fibrinoid Degeneration.
- Amyloid Degeneration (Amyloidosis).
- Mucoid Degeneration (Myxoid Degeneration).
c- Carbohydrate Overload:
- Glycogen Degeneration.
3- Mineral Disorder
a- Calcification:
-Dystrophic Calcification.
-Metastatic Calcification.
b- Gout.
c- Cholesterol Clefts.
4- Pigment Disorder
a- Exogenous pigmentation.
b- Endogenous pigmentation:
-Hemoglobin Derivative.
-Melanin Derivative.
-Lipid Derivative.
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
8
1. WATER OVERLOAD
a- Cell Swelling (acute).
It’s a simple response of cell to injurious agent that
cytoplasm appears as hazy appearance, occur as result of excessive fluid
accumulated inside cell, the cell retrains to its normal size if injuries agent will
be removed.
b- Hydropic Degeneration.
Cells swell due to accumulation of excessive amount
of fluid inside cell within cytoplasm, its mostly occur in epithelial cell in skin and
mucous membranes. Other synonyms used are
Cloudy Swelling
(for gross
appearance of affected organ) and
Vacuolar Degeneration
(due to cytoplasmic
vacuolation).
c- Ballooning degeneration:
extreme type of hydropic degeneration in which
cells are greatly enlarged and cytoplasm is containing clear space is typically seen
in epidermal cells infected by epitheliotropic viruses (pox virus). This lesion
frequently progresses to form vesicles from lysis of epidermal cells, in which
these viral infections cause both degradation of cytoplasmic proteins and net flux
of water into cytoplasm.
Etiology:
1- Marked mitochondrial damage.
2- Cessation of ATP production
3- Failure of sodium pump.
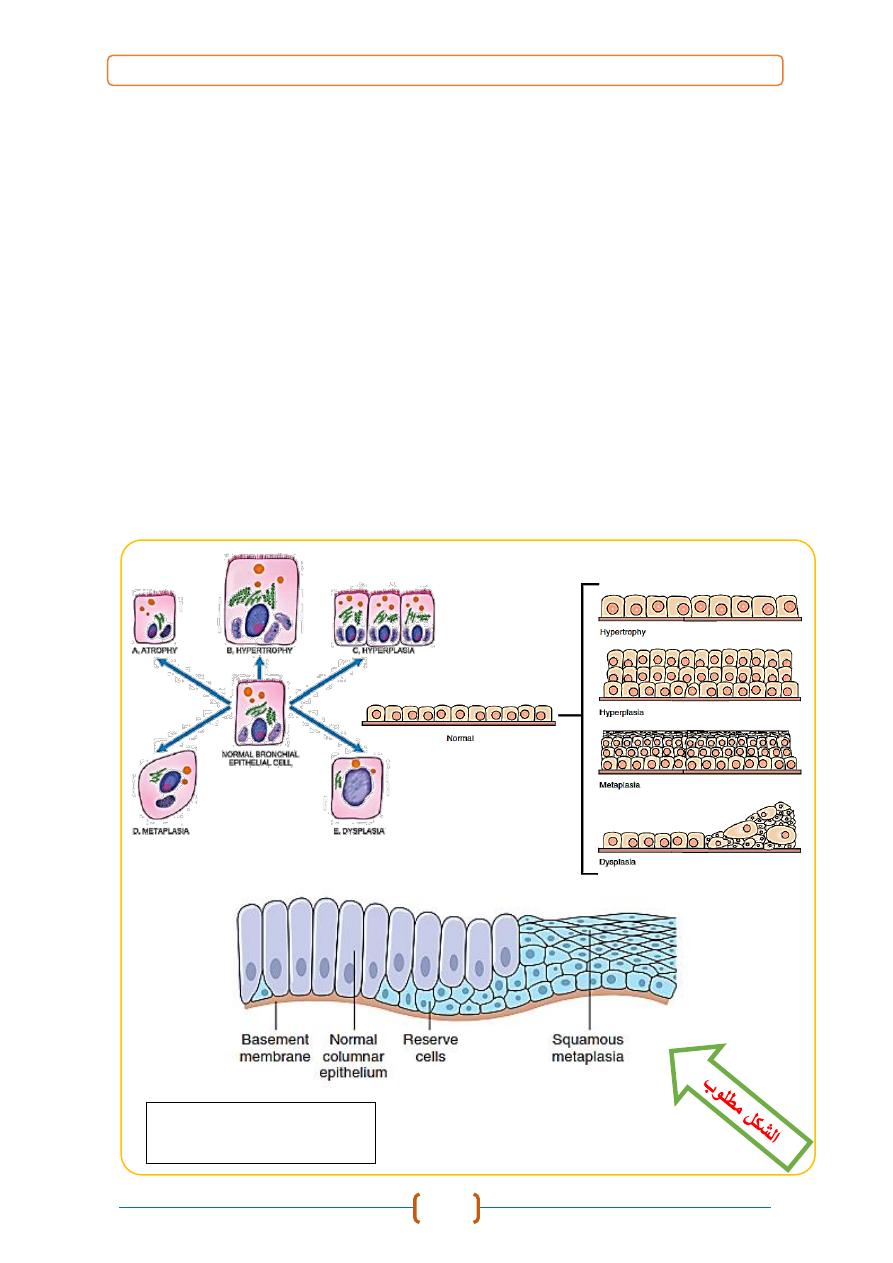
Pathogenesis:
Cell swelling results from impaired regulation of sodium and potassium at
level of cell membrane. This results in intracellular accumulation of sodium and
escape of potassium. This, in turn, leads to rapid flow of water into cell to
maintain iso-osmotic conditions and hence cellular swelling occurs. In addition,
influx of calcium too occurs.
The alteration in selective permeability of cellular membranes leading to
influx of water molecules, these types of degenerations occurs due to failure of
injured cells to maintain electrolyte balance through the "Sodium-Potassium
pump". As this mechanism is energy dependent, a fall in ATP in injured cells
causes efflux of Potassium ions with influx of Sodium ions, increasing osmotic
pressure in cytoplasm attracts water molecules. As a result, swelling of cells
occurs.
Grossly:
The affected organ such as kidney, liver, pancreas, or heart muscle
is
enlarged due to swelling. The cut surface bulges outwards and is slightly opaque.
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
9
Microscopically:
1- The cells are swollen and the microvasculature compressed.
2- Small clear vacuoles are seen in the cells and hence the term vacuolar
degeneration. These vacuoles represent distended cisternae of endoplasmic
reticulum.
3- Small cytoplasmic blebs may be seen.
4- The nucleus and cytoplasm may appear pale.
:مالحظة
.الشكالن مطلوبان في الجزء النظري
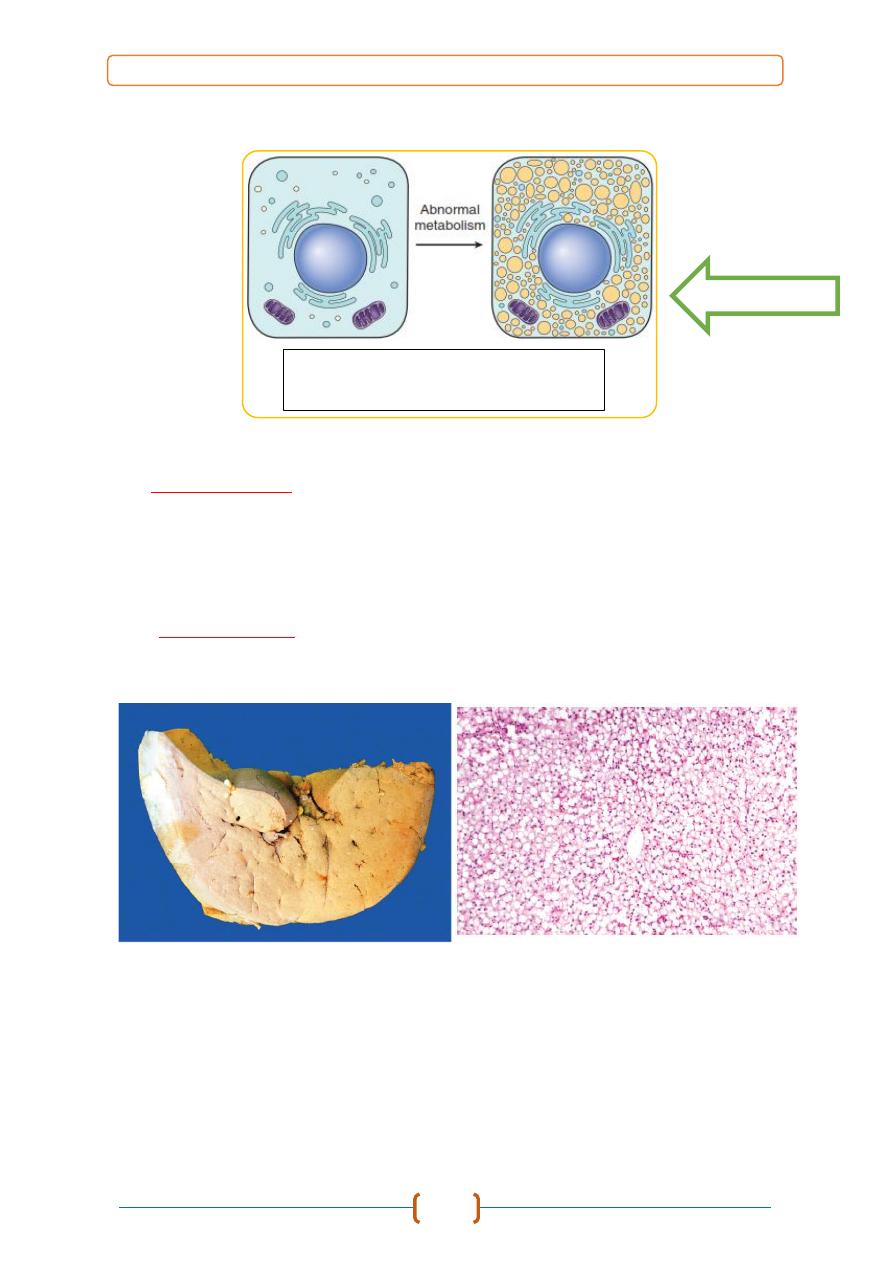
Diagram show
Pathogenesis of
Hydropic Degeneration.
Figure show Pathogenesis of
Vacuolar Degeneration.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
10
2. METABOLITE OVERLOAD
a- Fat Overload:
An overload of fat occurs in parenchymal cells particularly liver cells,
tubular epithelial cells of kidney, and myocardial cells. The etiology is:
1. Conditions with excess fat:
i) Obesity.
ii) Diabetes mellitus.
iii) Congenital hyperlipidaemia.
2. Liver cell damage:
i) Alcoholic liver disease.
ii) Starvation.
iii) Protein malnutrition.
iv) Chronic illnesses (tuberculosis).
v) Hypoxia (anemia, cardiac failure).
vi) Hepatotoxins (CCL
4
, chloroform, ether, aflatoxins).
vii) Drug-induced liver cell injury (methotrexate, steroids).
viii) Reye’s syndrome.
Pathogenesis:
Occurs in conditions that disturb normal metabolism of fat. Normally, fatty
acid is oxidized and combined to proteins to form lipoproteins that are released
into circulation. The following mechanisms result in accumulation of lipids in
cells:
1- Abnormally high levels of fat in diet result in overload in fat metabolism.
2- Interference in protein production.
3- Impairment in the conjugation process.
4- Interference in oxidation of fat.
5- Interference in the release of lipoprotein from cytoplasm of cells.
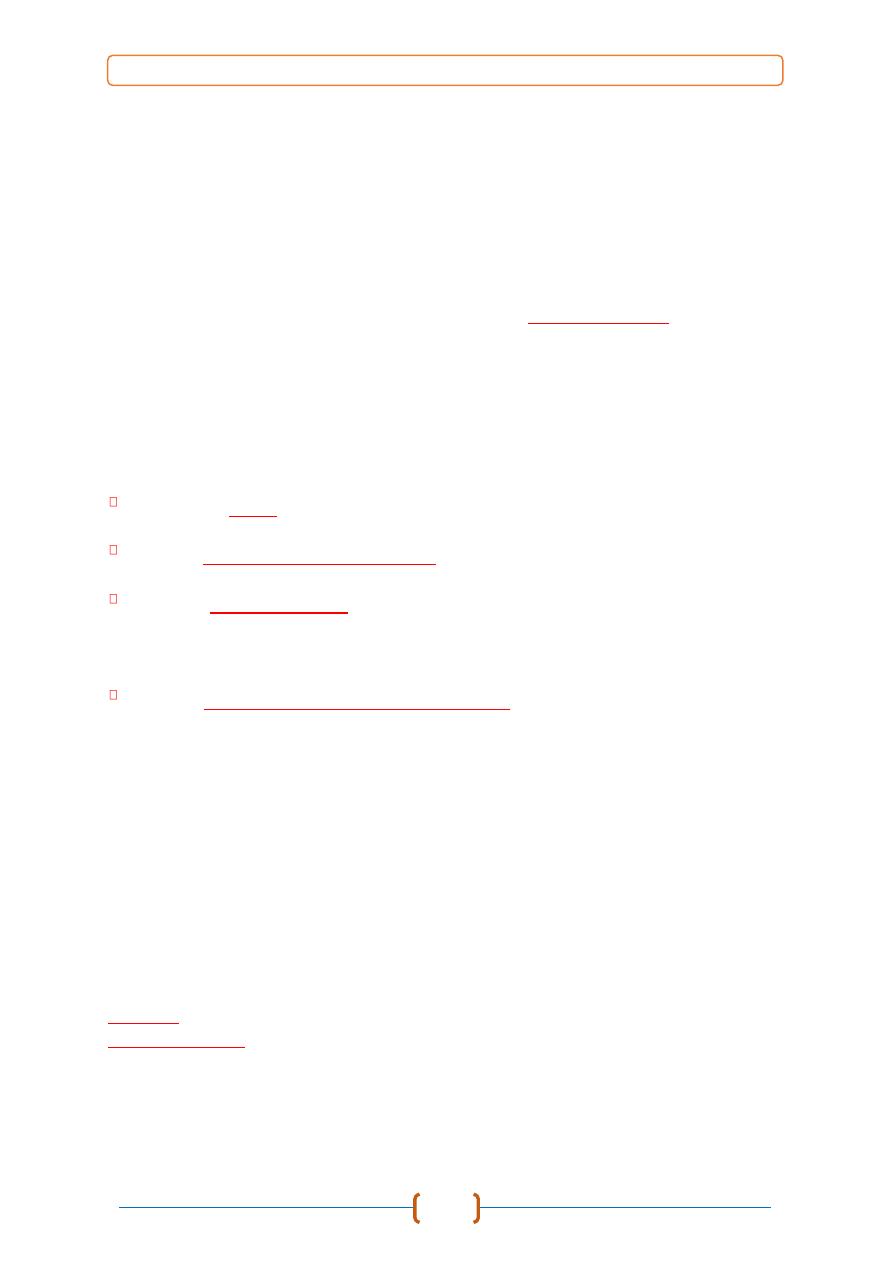
Grossly:
Affected organ (usually liver) shows uniform paleness with a greasy cut
surface and knife contained fat droplets on their edges.
a) Fatty degeneration (Fat phanerosis):
Microscopically,
Presence of multiple small droplets of fat within the
cytoplasm of cells without nuclear displacement. It is considered a primary fat
degenerative change in cells. vacuoles with distinct borders appear in the
cytoplasm of affected cells. These vacuoles make cytoplasm to appear foamy,
and may coalesce to form large globules. In routinely stained preparations these
material is lost because fat is dissolved by alcohol, but they demonstrated using
special stains in frozen sections (
fat type : fatty acids
).
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
11
b) Fatty infiltration (Steatosis):
Microscopically,
characterized by presence of a single globule of fat
displacing the nuclei to one side; which give the cell a ring like appearance and
mostly occur in liver and other parenchymal organs (
fat type : neutral fatty acids
).
c) Fatty change (Lipidosis):
Mean converting one whole type of tissue (special hepatocytes) as fatty
cells.
Microscopically
, the whole section of tissue appears just like fatty tissue
(
fat type : metabolic end products
).
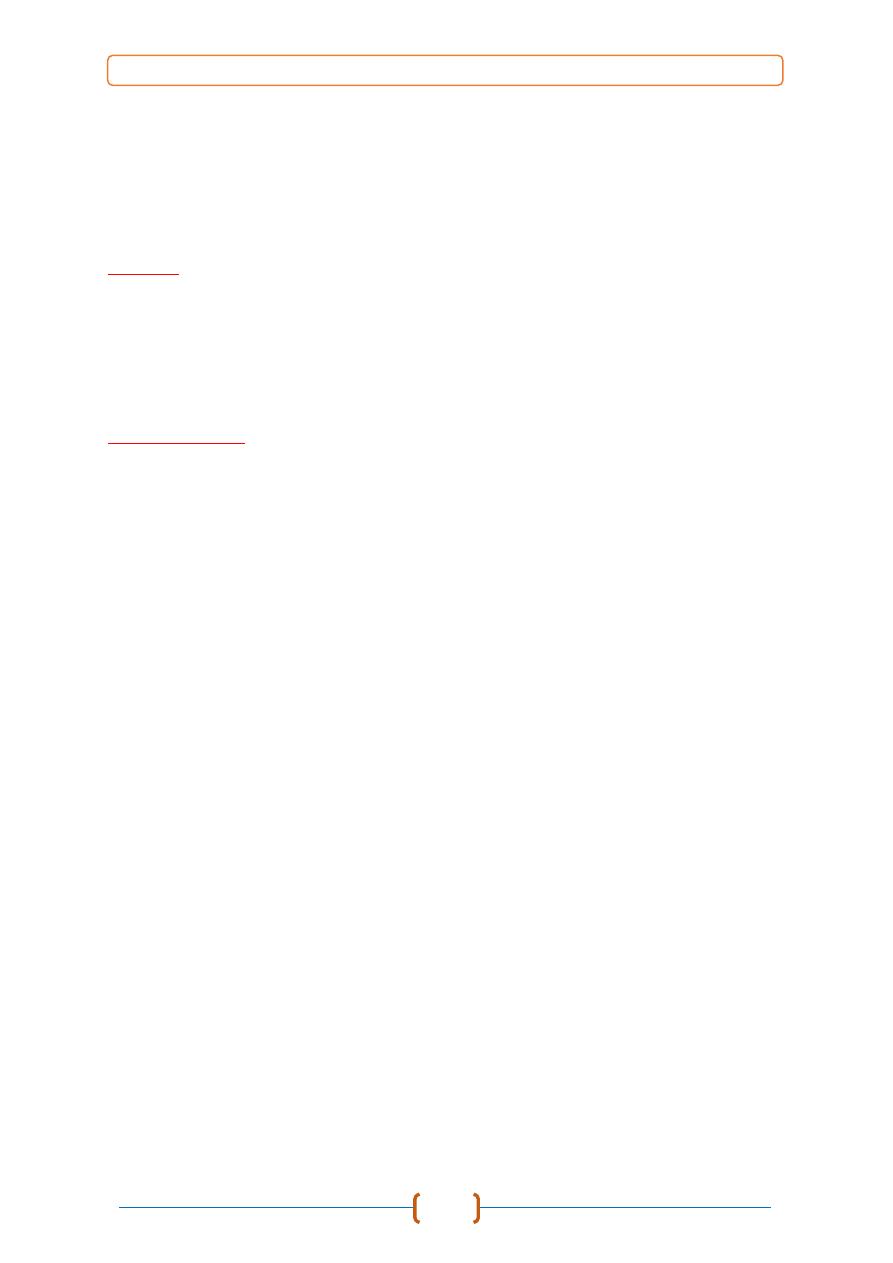
Figure show Pathogenesis of
Fatty Degeneration.
الشكل مطلوب
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
12
b- Protein Overload
a) Cloudy Swelling (Parenchymatous Degeneration)
A type of degenerative changes characterized by intracellular accumulation
of both fluid and protein substance, both glandular and stroma may undergo this
change, they are not equally affected, glandular ones being more liable to injury.
Etiology
1- Slight disturbances of nutrition and metabolism.
2- Inflammation.
3- Infectious.
4- Intoxication.
5- Increased body temperature.
Microscopically
The individual cells will be swollen and larger, more granular, and more
opaque than normal due to presence of minute granules; the nucleus obscured.
b) Hyaline Change (Hyalinization, Hyaline degeneration, Zenker’s degeneration)
Abnormal accumulation of protein droplet inside or outside cell after
abnormal protein metabolism or degeneration of cell protein, its appear as pink-
staining homogenous glassy cytoplasmic material. The hyaline changes either
intracellular or extracellular.
- Intracellular Hyaline:
1-
Hyaline droplets
in the proximal tubular epithelial cells in cases of excessive
reabsorption of plasma proteins.
2-
Hyaline degeneration
of rectus abdominalis muscle called
Zenker’s
degeneration
, muscle loses its fibrillar staining and becomes glassy.
3-
Mallory’s hyaline
aggregates of filaments in hepatocytes in alcoholic injury.
4-
Nuclear or cytoplasmic hyaline inclusions
seen in some viral infections.
5-
Russell’s bodies
excessive Ig in rough endoplasmic reticulum of plasma cells.
- Extracellular Hyaline:
1-
Hyaline degeneration
in leiomyomas of the uterus.
2-
Hyalinized old
scar
of fibro-collagenous tissues.
3-
Arteriolosclerosis
in renal vessels in hypertension and diabetes mellitus.
4.
Hyalinized glomeruli
in chronic glomerulonephritis.
5.
Corpora amylacea
are rounded masses of concentric hyaline laminae seen in
the prostate in elderly, in brain and spinal cord in old age, and in old infarcts
lesions of lung.
General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
13
c) Fibrinoid:
A special type of protein accumulation result due to deposition of coagulated
protein extracellularly found in degenerating blood vessel walls and connective
tissue. It includes fibrin, albumin, and globulin, this condition seen in Arthurs
reaction in hyperimmunized horses.
d) Amyloidosis:
A special form of protein accumulation characterized by deposition of group
of proteinaceous material in basement membrane.
Microscopically,
amyloid is an
extracellular eosinophilic amorphous substance causing compresses adjacent
parenchymal cells, lead to atrophy or death from compression.
This outcome is most evident in hepatic amyloidosis, in which protein is
deposited in space of Disse, here it compresses adjacent hepatocytes and
interferes with hepatocytes access to blood and nutrients in sinusoids. The special
stain used for amyloid is Congo red staining it orange to orange red. Type of
Amyloidosis:
Based on
cause
, into
PRIMARY
(unknown cause) and
SECONDARY
(complication of some known disease).
Based on
extent of amyloid deposition
, into
SYSTEMIC
(generalized) involving
multiple organs and
LOCALIZED
involving one or two organs or sites.
Based on
clinical location
, into
PATTERN I
(involving tongue, heart, bowel,
skeletal and smooth muscle, skin and nerves),
PATTERN II
(involving liver,
spleen, kidney and adrenals) and
PATTERN III
(involving sites of both
pattern I and II).
Based on
tissues in which amyloid is deposited
, into
MESENCHYMAL
(organs
derived from mesoderm) and
PARENCHYMAL
(organs derived from
ectoderm and endoderm).
β-Amyloidosis.
Extracellular accumulation of amyloid-β protein which is
characteristic of Alzheimer’s disease in humans. This type of amyloid has also
been identified in brains of aged dogs, highest concentration being in frontal
cortex in dogs older than 13 years.
e) Mucoid Degeneration (Myxomatous Degeneration):
Mucopolysaccharides are conjugates of protein and carbohydrates normally
found in secretions of epithelial cells. Mucoid degeneration refers to
overproduction of mucinous secretion by cells. Myxomatous degeneration is
described as the transformation of tissues into a jelly-like structure.
Grossly,
affected organ has gelatinous appearance and consistency.
Microscopically
this material is amorphous material that present out or inside the
cells.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
14
c- Carbohydrate Overload
a) Glycogen degeneration
Glycogen degeneration involves the presence of abnormally large amount
of glycogen in the cytoplasm of cells. Glycogen is normally present in cytoplasm
of cells (particularly in liver cells). Excessive accumulation occurs in some
disease processes characterized by prolonged hyperglycemia such as diabetes
mellitus. Best’s carmine and periodic acid-Schiff (PAS) staining may be
employed to confirm the presence of glycogen in the cells.
The
microscopic changes
are presence of clear vacuoles are in affected cells.
This is because in routinely prepared sections, glycogen that is water-soluble is
lost in the preparation. Special stains in frozen sections could show the abnormal
accumulation of this substance in affected cells.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
15
3- Mineral Disorder
a- Calcification
Calcification refers to a pathological deposition of calcium salts in cells and
tissues, it must be differentiated from normal bone formation. Forms include the
following:
(a) Dystrophic calcification:
When calcium salts are deposited in degenerate and
necrotic cells and tissues, without elevation in blood calcium ion level.
(b) Metastatic calcification:
When calcium salt deposited in homeostatic cells and
tissues due to excess ionized calcium in blood. Tissue injury is not required for
calcium to be deposited in tissues, occurs in cases of excessive mobilization of
calcium from skeleton as in hypervitaminosis D and hyperparathyroidism.
Grossly;
the affected areas of tissue are white and when incised have a gritty
feel to them.
Microscopically,
the deposited calcium salts are intensely basophilic
and breaks into fragments, these lesions appear as purple to black brown in color
by routine preparation.
b- Urates Deposition (Gout)
Deposition of sodium urate crystals or urates in tissue in the articular and
periarticular tissues, uric acid and urates are end products of purine metabolism
in birds and reptiles these products are eliminated as semisolid urates, so any
disturbance in their excretion cause this condition, this condition known as Gout.
there are two forms including:
(1) Articular type
(2) Visceral type. characteristically affects the visceral serosae, particularly
parietal pericardium, and the kidneys. Serosa covered with a thin layer of gray
granules. In the renal urate deposits are visible in renal tubules and ureters.
This type occurs mainly due to vitamin A deficiency and high-protein diets.
c- Cholesterol Clefts
A crystal deposition in tissue that suffer from hemorrhage and necrosis,
during preparation of paraffin-embedded both hemorrhage and necrosis dissolved
out of tissue specimen sections, leaving characteristic clefts which resemble
shards of glass. Cholesterol crystals in tissue have no significance except that they
indicate site of an old hemorrhage or tissue necrosis.
Grossly,
the cholesterol appears as firm, crumbly gray nodules in the
cholesteatomas.
Microscopically,
they appear as bright crystals, thin rhomboidal
plates in tissue section.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
16
3) PIGMENTATION
pigments of either exogenous or endogenous origin may accumulate within cells.
They are usually innocuous but provide clues to the existence and nature of
underlying disorder. Two forms of pigmentation occur based on the origin of the
pigment:
(a) Exogenous pigmentation - following injection, inhalation, or absorption from
the gut of some colored foreign materials. Exogenous pigments include the
following groups of materials:
a.1) Metals - silver, bismuth, gold, lead, and iron.
a.2) Coarse Materials - dust, carbon, silica, and asbestos.
a.3) Colored substances - carotene, tetracycline.
a.4) Fungi - monilia, aspergilli
(b) Endogenous pigmentation - due to altered metabolism of breakdown
products of hemoglobin, melanin and fat. Endogenous forms of pigments include
the following:
b.1. Hemoglobin derivatives
(1) Haematins - iron-negative pigments that occur following the action of acids
to hemoglobin (artefacts), parasites in blood (e.g., malaria), or following trauma
to tissues. Their presence in tissues has little significance, except perhaps an
indication of poor techniques and solutions used in tissue fixation.
(2) Hemosiderin - iron-positive pigment chemically known as ferritin (the
storage form of iron), seen in cases of trauma, excessive hemorrhage or
hemolysis. These pigments occur abundantly in the cytoplasm of cells of the
reticulo-endothelial system such as in the spleen, Kupffer cells in the liver, and
bone marrow. The appearance of abnormal amount of this pigment usually
suggests excessive formation because of hemolysis.
(3) Haematoidin or Bilirubin - following excessive hemorrhage or hemolysis,
and failure of the liver to conjugate bilirubin into bile, and/or secrete bile. This
pigment occurs in association with jaundice.
(4) Porphyrins - Porphyrin pigments may accumulate in tissues in rare disease
conditions (example congenital porphyria) characterized by a defect in
hemoglobin formation. Apart from this, it is a normal component in the formation
of hemoglobin. However, it occurs in some disease conditions following
ingestion of toxic plants (for porphyrin is formed following breakdown of the
chlorophyll in plants). This pigment is photoreactive, i.e. it causes activation of
some processes (production of toxic oxygen free radicals) that cause peroxidation
of lipid membranes. The resultant condition is called photosensitization.
b.2 Melanin pigmentation - granular protein containing pigment produced by
melanocytes. Increased production occurs in association with tumors of the
melanocytes (melanoma), excessive irradiation, and effects of sunlight.
b.3 Lipid derived pigment (Lipofuscins) - these pigments represent partially
degraded lysosome-bound indigestible residues of autophagic vacuoles in cells.

General Pathology /
2016 – 2017
/ Dr. Saevan S. Al-Mahmood
17
They are also known in many names as "Wear and Tear Pigment, Pigment of
Brown Atrophy, Ceroid, or Lipochrome".
