Pediatric surgery
No. :
Date :
Attendance: Obligatory
Type of lecture: theory
Place : Hall no.4 college of medicine – Al mustansiriyah University .
Date : Sunday 19th of March 2017
Time : 1:30 – 2:30 PM.
Students: 4th year / college of medicine / Al mustansiriyah University
By : Dr. Ali E. Joda M.B.Ch.B. - F.I.C.M.S. - pediatric surgeon
Mobile no. : 009647725465090
E. mail : alieagle677@yahoo.com ali.egab.joda@gmail.com
Topics :-
Cervical lymphadenitis.Branchial cyst.
Thyroglossal cyst.
Cervical dermoid cyst.
Sternomastoid tumor.
Cystic hygroma.
Objectives: -
To know the differential diagnosis of neck mass in children.
The peculiar feature of each mass.
The specific treatment for each one.
Neck mass in children
Classification:Congenital cyst, sinus , fistula.
Infectious , inflammatory ( acute or chronic lymphadenitis).
Neoplastic ( benign or malignant ) , ( primary or secondary).
Traumatic.
Cervical lymphadenitis
Enlarged cervical lymph node is the most common neck mass in children. It commonly associated with systemic viral illness, upper respiratory infection, oropharyngeal infection, nearby skin infection, but malignancy (primary or secondary) must be considered. Enlarged cervical lymph node may be the first clinical manifestation of lymphoma.
Acute suppurative lymphadenitis :-
The most common cause is bacterial infection (staphylococcus aureus , streptococcus hemolyticus). There is Fever , tenderness , hotness . but fluctuation , & thining of the overlying skin indicate abscess formation. Needle aspiration confirms the diagnosis & the material aspirated can be send for culture and sensetivity. Repeated needle aspiration with proper antibiotics can resolve the condition , but surgical incision & drainage with the use of penrose drain or wick drain is the best treatment , the antibiotic therapy should be continued for 10 days.
Chronic lymphadenitis :-
The lymph nodes are not tender & progression to fluctuation is unlikely. The child with this type of lymphadenitis should receive 2 weeks course of oral anti-staphylococcus antibiotics , if no response the child should be evaluated for T.B , atypical mycobacterial infection ,& cat-scratch disease. Any enlarged lymph node present for more than 6 -8 weeks not responding to appropriate antibiotics should be completely excised & send for culture & histopathology to exclude neoplasm. Lymph node present in supraclavicular space or posterior triangle is more suspicious of malignancy than those found in the submandibular or anterior triangle.
Mycobacterial lymphadenitis
Most of the mycobacterial lymphadenitis is caused by MAIS complex ( mycobacterium avium intracellulare scrofulaceum) which are group of 10 -15 mycobacteria produce specific , localized form of lymphadenitis. the port of entry is through the mucous membrane of the pharynx , while lymphadenitis resulting from mycobacterium tuberculosis is thought to be an extension of primary pulmonary T.B , & usually involve supraclavicular L.N .children with tuberculous lymphphadenitis usually are symptomatic with fever , weight loss , sweating , having positive finding of pulmonary T.B on CXR , & the child show positive tuberculine test using PPD (purified protein derivative).While children with atypical mycobacterial lymphadenitis ( MAIS complex) are asymptomatic , having normal CXR , negative tuberculine test . Confirmative diagnosis may depend on culture or histopathology of the excised L.N. the lymph nodes in mycobacterial infection in general are not tender with tendency of spontaneous regression or breakdown of the node to skin surface forming sinus or fistula.
Treatment :-
Anti T.B chemotherapy for tuberculous scrofula , resolution of lymphadenopathy occur within few months. Treatment of MAIS lymphadenitis is mainly by surgical excision of the group of the affected L.N before extensive ulceration of the overlying skin. Children with this type of atypical mycobacterial infection respond well to complete surgical excision without drug therapy.
Cat-scratch disease
The most common cause of non-bacterial chronic lymphadenopathy in developed countries. Caused by gram negative Rickettsial organism Bartonella Henselae. The disease usually transmitted via superficial wound caused by a cat , dog , or monkey. Healthy kitten is the most frequent vector. The disease begin as superficial infection or pustule followed by regional lymphadenopathy in 1 -2 week . Axilla is the most common involved area then head & neck. The treatment is mostly symptomatic as the disease is self-limited & the lymphadenopathy resolves spontaneously over a period of weeks to months , azithromycine may have been used if antibiotic are needed.
Branchial cyst , sinus , fistula
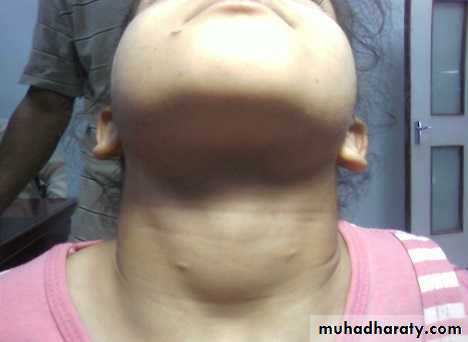
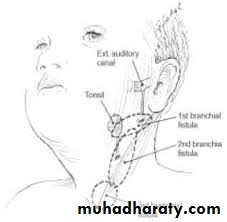
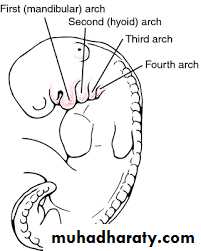
ناسور , جيب , كيس خيشوميThe branchial apparatus consist of 6 branchial arches separated by 5 branchial clefts & pouches. Incomplete obliteration of branchial clefts ( most commonly the second branchial cleft) during embryonic development give rise to such congenital cyst ,sinus ,fistula. Branchial sinus & fistula are more common in infants & children while branchial cyst occur more often in older children & young adult. There is a pin point opening at the anterior border of lower third of sternomastoid muscle which may be unnoticed for sometimes ,the tract penetrates the platysma & cervical fascia to ascend along carotid sheath then pass between the bifurcation of carotid artery to end in the tonsillar fossa as internal opening. with small drops of clear mucoid discharge at the external opening, or infection in the branchial tract associated with upper respiratory tract infection result in palpable mass as a result of inability of the thick mucoid material to drain spontaneously. The infection is more common in the cyst & less common in the sinus & fistula. the tract of the fistula may be palpable as a cord like structure specially during hyper-extension of the child's neck. Compression along the tract may produce mucoid material discharging from the opening. 10% of the branchial fistula is bilateral. Persistent discharge , possibility of infection , & risk of malignancy in the future are the main indications of surgical removal. Colored dye or radio-opaque material can be injected to outline the fistula , or ultrasound may be useful to identify the cystic nature of the mass if it is not apparent by physical examination.
Treatment :-
The aim is complete surgical excision electively when there is no infection , the younger age the better surgical excision , if infection is present; use warm soaks & antibiotics because surgery on infected field result in nerve injury , incomplete resection , & recurrence of the fistula. the surgical procedure can be done as outpatient procedure under general anaesthesia, the child in supine position, hyper-extension of the neck , transverse elliptical incision around the external opening ,catherter or probe can be placed in the tract , use of head light & loupe magnification provide good visualization for dissection. A second more cephalad parallel incision (step-ladder incision) may be necessary for dissection of the most superior part of the tract.
Thyroglossal cyst
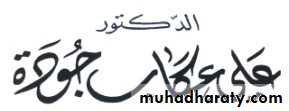
The most common midline cervical swelling in children , mostly noticed in preschool children. the foramen caecum at the base of the tongue is the site of development of thyroid diverticulum called ( thyroglossal duct) which descends in the neck to form the thyroid gland at the pre-tracheal position while maintaining its connection to the foramen caecum , the thyroglossal duct may pass infront or behind the hyoid bone but most commonly it passes through it. Normally the duct disappear when thyroid gland reach its proper position , but if not , it will form thyroglossal duct cyst. It never have primary external opening (no primary fistula, & the thyroglossal fistula noticed result from rupture of the cyst , or incision of inflamed cyst) ) because the embryologic thyroglossal duct never reach the surface of neck. it can be located anywhere in the midline of the neck along the course of the thyroglossal tract from the base of tongue to behind the sternum but the most common site is just inferior to the hyoid bone or adjacent to it. It may be associated with complete failure of migration of thyroid gland result in ectopic thyroid tissue ( lingual thyroid ) at the base of the tongue.Presentation :-
The classic presentation is cystic mass in the midline of the neck at or just below the hyoid bone . suprahyoid cyst is rare & most be differentiated from submental dermoid cyst or submental lymph node. Suprasternal cyst is also rare. On examination the cyst is smooth, soft , non-tender , moves up with protrusion of the tongue because of its attachment to foramen caecum at the base of the tongue. Ectopic thyroid tissue may be mistaken for thyroglossal cyst so ultrasound or thyroid scan before surgery is necessary to detect any ectopic thyroid tissue & avoid doing permanent hypothyroidism, & any evidence of hypothyroidism necessate doing thyroid function test.Treatment :-
Complete surgical excision to avoid complications of infection & small risk of ( less than 1 % ) of cancer developing in the cyst. Sistrunk operation: complete excision of the cyst with its tract upward to the base of tongue with excision of the central part of the hyoid bone to prevent recurrence. Risk of recurrence is 20% if central hyoidectomy not done & it may be as much as 10 years following surgery , while recurrence rate is only 5% with doing central hyoidectomy. recurrence of thyroglossal fistula or infected cyst is higher than that of uncomplicated cyst.
Cervical Dermoid cyst
Typically midline , well circumscribed cyst , lined by squamous epithelium , contain sebaceous debris which can be secondary infected . the overlying skin is often adherent , small cutaneous pit may be visible . yellowish appearance at surgery & sebaceous content of the cyst differentiates it from thyroglossal cyst which often contain clear viscous fluid.Sternomastoid tumor
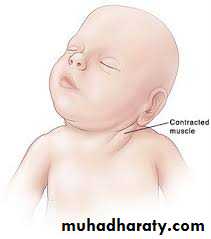
(Congenital torticollis , fibromatosis colli , wry neck)Fibrous replacement of the muscle fibers ( just like Dupuytren contracture or planter fibromatosis) result in shortening of the sternomastoid muscle which tilts the head & neck to the side of the lesion (traction of the mastoid process toward sterno-clavicular joint , face rotated away from the side of the lesion), the resulting mass represent the fibrous tissue is palpable clinically within the muscle or detected by ultrasound. This fibrous tumor may be related to breech presentation or complicated obstetric position , or in-utero positional disorder resulting in injury & fibrosis of the sternomastoid muscle.
Presentation :-
the mass is not found at birth but appear 2 - 3 weeks after birth , as hard , spindle shaped , painless mass ( pseudo-tumor) located within the middle or lower third of the muscle. In 2/3 of the cases there is localized tumor, it is often but not always accompanied by torticollis , there may be diffuse fibrosis of the sternomastoid muscle in 1/3 of the cases, causing postural torticollis without obvious mass. the infant has characteristic posture (facing to opposite side), & with the time if not corrected ; facial & cranial asymmetry will develops . facial hemi-hypolpasia ( flattening & under development of the malar eminence & downward displacement of the ear, eye , mouth on the affected side ) , plagiocephally ( flattening of both the frontal area on the ipsilateral side & the occipital area on the contralateral side ).Treatment :-
80 – 97% of the affected infants do not require operative treatment , the successful treatment is by early recognition & prompt physiotherapy by full range of motion , stretching exercise , & positional changes with the baby in the crib , the parents should be taught to perform these exercise once or twice each day , one parent holds the child's shoulder down against firm surface & the other rotates the head toward the opposite shoulder , re-arranging the baby's room by placing the toys & desirable objects in the crib on the ipsilateral side to encourage the baby looking to that side. operative intervention is not indicated in the neonates , but 100% of children older than 1 -1.5 year with still torticollis & development of facial hemi-hypoplasia will need surgery because they are often refractory to conservative treatment. The muscle divided by transection in the middle third through lateral collar incision.Cystic hygroma
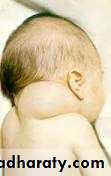
Lymphatic malformation either macrocystic ( cystic hygroma ) or microcystic (lymphangioma), most commoly located in the region of heavy lymphatic channels , 75% in the neck , 20% axilla , or in mediastinum , pelvis , retroperitoneum , groin , buttock.
Presentation :-
Soft , compressible mass most commonly in the posterior triangle of the neck , usually ballotable & trans-illuminate ,contains cholesterol crystals, have risk of infection leading to cellulitis or even systemic illness. infection elsewhere in the body or viral illness can cause increased size & tension of the lymphatics causing disfigurement , significant airway obstruction , intra-lesional hemorrhage , dystocia at the time of delivery so ( EXIT procedure ) = (ex-utero intra-partum treatment) may be indicated to prevent neonatal asphyxia. Ultrasound can differentiate macrocystic from microcystic lesion. MRI is used to define the extent of the lesion & its relation to vital structures.Treatment :-
Surgical resection for well localized lesion.
Sclerotherapy : ablasion of focal , macrocystic lesion.
For cellulitis : antibiotics .
For intra-lesioal bleeding : rest , analgesia , antibiotics.
Tracheostomy may be needed for oropharyngeal lesion & severe airway obstruction.
Intra-lesional sclerotherapy using ethanol , doxycycline , sodium tetradecyl sulfate , OK 432 under fluoroscopic guidance causing scarring & collapse of macrocystic lymphatic malformation with successful result but it is not effective for microcystic lesion. Complete surgical excision may carry potential complication of injury to the surrounding structures , recurrence of residual lesion if not completely resected. Prolong drainage using closed suction drain will be required for weeks after hospital discharge.