Pediatric surgery
No. :
Date :
Attendance: Obligatory
Type of lecture: theory
Place : Hall no.4 college of medicine –Al-Mustansiriyah University .
Date : Sunday 5th of March 2017.
Time : 1:30 – 2:30 PM.
Students: 4th year / college of medicine / Al-Mustansiriyah University
By : Dr. Ali E. Joda M.B.Ch.B. - F.I.C.M.S. - pediatric surgeon
Mobile no. : 07725465090
E. mail : ali.egab.joda@uomustansiriyah.edu.iq
Topics:-
Introduction to pediatric surgery.Neonatal intestinal obstruction.
Duodenal atresia.
Jejuno-ileal atresia.
Malrotation of midgut.
Meconium ileus.
Objectives:-
What is the field of pediatric surgery & how it differs from general surgery?
By the end of this lecture, you have to be able to recognize the main features of neonatal intestinal obstruction & how you can approach to infant with this problem.
What is atresia & where it could be occur in gastrointestinal tract? How can you differentiate it from other causes of intestinal obstruction? & what are the main lines of treatment?
Introduction
Pediatric surgery is not just a general surgery performed in smaller people. Children need specialized surgeon to deal with their surgical problems because they differ markedly from that of adults in many aspects, including:-
Unique physiologic demands that vary according to age and development, the neonate's physiologic development is closer to that of a fetus, while adolescents' physiology is similar to that of adults. For example in the Gastro-intestinal tract: Small size stomach (need small frequent feeds), Low level of digestive enzymes due to immature pancreas, underdeveloped gastroesophageal junction (GER is common until 6 months of age), Immature protective mucous layer (High risk of infection), Gastric pH is alkalotic at delivery.
Anatomical difference, Infants and small children have larger body surface area, their occipito-frontal circumference exceeds the chest circumference, they have wide abdomen, broad costal margin and shallow pelvis, the edge of the liver comes below the costal margin and the bladder is largely intra-abdominal, the ribs are more horizontal and are flexible, the umbilicus is relatively low lying. The smaller size organs need gentle surgical skill. Implications: better to calculate drug dosage according to body surface area, Transverse supra-umbilical incisions give greater access than vertical midline ones for open surgery. Trauma (including surgical access) can easily damage the liver or bladder. The geometry of the ribs means that ventilation requires greater diaphragmatic movement, their flexibility means that rib fractures are rare and often a sign of abuse.
Infants and children have pathology unique to their chronologic and developmental age, they may suffer from congenital abnormalities and tumors not seen in adults, and their management requires understanding the relevant embryology and pathogenesis.
Special considerations should be known about venous access, fluid & electrolyte, special drug dosage, thermo-regulation, blood volume & its products, pain control, hyper-alimentation & IV nutrition & minimally invasive surgery.
Therefore, the pediatric surgeon is specially trained surgeon with extensive experience in treating children, infants, neonates & even fetus in utero with surgical problems.
The pediatric surgical procedures need specialized centers with appropriate NICU (neonatal intensive care unit), trained staff, pediatric radiologist, anesthetist, pathologist & pediatrician…etc.
Neonatal intestinal obstruction
Surgical Causes:-Intestinal atresia. ● Pyloric stenosis.
Meconium disease. ● necrotizing enterocolitis.
malrotation of midgut. ● Congenital peritoneal band.
Hirschsprung’s disease. ● Enteric duplication.
Anorectal malformation. ● Mesenteric cyst.
Complicated inguinal hernia. ● Trans mesenteric internal hernia
Main symptoms:-
Vomiting: usually greenish due to bile stained. The higher obstruction the earlier vomiting.Abdominal distention: sever distention is seen in lower intestinal obstruction. While in upper intestinal obstruction the abdomen is flat or with minimal distension.
Delayed or no passage of meconium: normally 50-250 g of meconium should be passed within the 1st 24-48 hr after birth.
Examination:-
Lethargy, hypotonic: due to electrolyte disturbance, sepsis, peritonitis.
Respiratory distress: due to abdominal distention, aspiration pneumonia.
Obvious associated anomalies: like Down syndrome.
Jaundice: due to prematurity, dehydration & associated biliary atresia.
Visible peristalsis: especially in preterm with thin abdominal wall.
On Superficial palpation: distended bowel loops, mass of meconium ileus, mass of necrotic bowel, enteric duplication, mesenteric cyst.
Tenderness: evident by crying, grimace, pulls up the leg.
Infants never exhibit rigidity but edema, redness or echymotic appearance of abdominal wall indicates intestinal ischemia & necrosis.
Inspection of anal orifice & rectal examination with little finger or probe to exclude imperforate anus, Hirschsprung's disease, meconium plug syndrome.
Passing NG tube to exclude esophageal atresia.
Investigation:-
Erect & supine abdominal X-ray (plain film): normally there is no air- fluid level in abdominal X-ray of neonate, the gas shadow is scattered throughout the abdomen, & it is difficult to distinguish between small & large bowel in neonate because the colonic haustration & mucosal folds of small bowel are not evident yet.
X-Ray findings of intestinal obstruction :-
Dilated bowel loops.
Air fluid levels.
Double bubble sign.
Gasless lower abdomen.
Other findings of complication or associated diseases: pneumoperitoneum, meconium pseudocyst, peritoneal calcification, soap bubble appearance, penumatosis intestinalis & others.
Upper GI Contrast study (using barium or gastrografin) for suspicion of partial intestinal obstruction or suspicion of malrotation of midgut.
Lower GI Contrast enema used for low intestinal obstruction, it differentiate between colonic atresia, ileal atresia, Hirschsprung's disease & Meconium ileus.
Intestinal atresia
Atresia = no lumen = رتق
Stenosis = narrowing.
Intestinal atresia & stenosis are one of the most common causes of neonatal intestinal obstruction (mechanical I. O).
Pathological types:-
Type-I: intraluminal web of mucosa & submucosa.
Type-II : blind ends joined by fibrous band. Intact mesentery, normal bowel length.
Type-IIIa: disconnected blind ends with V-shape defect in the mesentery. Subnormal bowel length, associated with cystic fibrosis.
Type-IIIb: (Christmas tree or apple peel deformity). Proximal jejunal atresia near ligament of Treitz, absent superior mesenteric artery, significant loss of bowel length & its mesentery, the distal small bowel lies freely in the abdominal cavity & assumes helix configuration around single perfusing vessel.
Type-IV: multiple segments atresia (string of sausage): grossly shortened bowel length.
type-I type-II type-IIIa type-IIIb type-IV
Duodenal atresia & stenosis
Believed to be caused by failure of recanalization of duodenal lumen between 8th-10th weeks of gestation. Type I atresia constitute 92% of cases, either thick membrane causing complete obstruction or thin membrane with central fenestration causing partial obstruction. The majority (85%) is distal to ampulla of Vatter & 15% proximal to it. Associated anomalies are present in 50% of duodenal atresia like Down syndrome, intestinal malrotation, congenital heart disease, T.E.F(trachea-esophageal fistula), renal anomalies, imperforate anus. the most common associated anomaly is Down syndrome (30% of duodenal atresia), & the most serious one causing death is cardiac anomalies.Other causes of duodenal obstruction in neonates are annular pancreas, preduodenal portal vein, Ladd's band, twisted duodenum in midgut volvulus.
Diagnosis:-
Antenatal ultrasound: maternal polyhydramnios, fetal abdomen (dilated stomach & 1st part of duodenum).
The infant delivered with prematurity in 25%, with growth retardation. Few hours after birth, he develops repeated bile stained vomiting with its sequel (dehydration, electrolyte disturbance, jaundice). Abdominal distension is not evident or mild.
Erect abdominal X- ray: double bubble sign. If there is gas shadow beyond the duodenum, it means partial obstruction so upper GI contrast study is needed.
Partial duodenal obstruction has delayed presentation & may not causing symptoms for many years.
Double bobble sign no abdominal distension
Treatment:-correction of fluid & electrolyte disturbance.
gastric decompression by NG tube.
antibiotic coverage.
premature with respiratory problem may need assisted ventilation.
jaundiced infant need proper IVF & phototherapy.
search for associated anomalies.
Surgery:-
Duodenotomy ( excision of the web & repair of the duodenum).
Duodeno-duodenostomy (bypassing the obstruction): transverse incision in the proximal end & longitudinal incision in the distal end then side-side or diamond shape anastomosis.
Survival rate is 90%. Most of the mortality related to prematurity & associated cardiac & chromosomal anomalies.
jejuno - ileal atresia
The most accepted theory is intrauterine vascular accident in late gestation resulting in ischemic necrosis of sterile segment of bowel & subsequent resorption of the affected segment.
It differ from duodenal atresia by multiple atresias, low incidence of associated anomalies (less than 10%), increased incidence of cystic fibrosis, low incidence of down syndrome.
Diagnosis:-
Mother had Polyhydramnios, +ve family history of similar atresia especially in type- IIIb & type- IV.
Bile stained vomiting.
Abdominal distention.
Delayed or no passage of meconium (or passage of grey plugs of mucus).
Tenderness, edema, erythema of abdominal wall indicate ischemic bowel.
Sometimes altered blood per rectum especially in type-3b due to ischemic distal bowel.
They have increased risk of perforation of the proximal bowel & subsequent peritonitis.
Erect abdominal X- ray:-
Air fluid level.
Gasless lower abdomen.
Ground glass appearance of inspissated mecomium when atresia associated with cystic fibrosis.
Pneumoperitonium when there is proximal bowel perforation.
Peritoneal calcification when there is meconium peritonitis.
Air-fluid levels type -1 atresia Christmas tree atresia
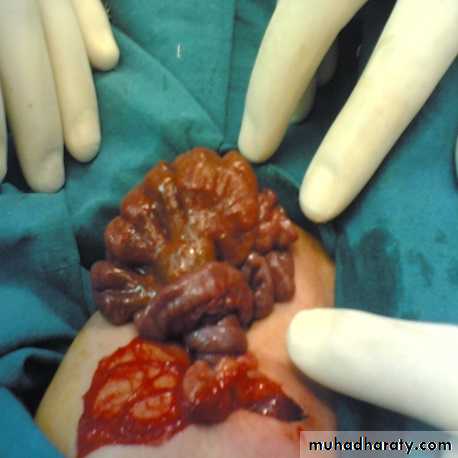
Surgery:-
Supraumbilical transverse abdominal incision , Any perforation should be sutured before further exploration. If there is malrotation : Ladd's procedure. Primary end-end anastomosis. If there is multiple atresia in a localized area we do single resection & end-end anastomosis.
Malrotation of midgut
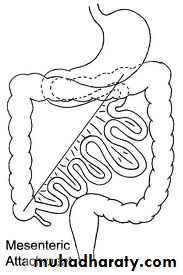
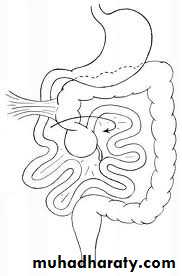
Embryology :-The intestinal tract is first recognized at 4 weeks of gestation & divided into foregut , midgut , & hindgut. During the next few weeks ; growth & development of midgut is faster than that of abdominal cavity , so the midgut normally herniated out of the peritoneal cavity into the umbilical cord then returns to abdominal cavity at 10 weeks of gestation. The return of intestine accompanied by a process of rotation & fixation, the axis of rotation is superior mesenteric artery (SMA). The proximal limb of midgut (duodenojejunal junction) is fixed in the upper left quadrant of the abdomen while the distal limb of midgut (cecocolic ) is fixed in the right lower quadrant of the abdomen. The normal rotation of midgut is critical for the formation of broad base mesentery with its fixation to the posterior body wall. Any error of normal rotation & fixation will lead to formation of narrow midgut mesentery & lack of fixation to the posterior body wall , which allows axial rotation of midgut around SMA resulting in midgut volvulus.
Normal malrotation malrotation with volvulus
Presentation :-
The presentation is age dependent : (1) midgut volvulus (top emergency). (2) partial duodenal obstruction (recurrent intestinal obstruction). (3) chronic non- specific abdominal complaints.(4) asymptomatic: discovered accidentally during investigation or during surgery for other reason. The classic & most common presentation is volvulus of midgut in neonatal period in form of acute onset of bilious vomiting in a previously healthy infant , mild or just upper abdominal distention (secondary to duodenal obstruction) , dehydration , abdominal wall erythema , peritonitis. Hematemesis , malena may result from intestinal mucosal ischemia. partial duodenal obstruction may result from (1)kinking of abnormally positioned duodenum , (2)narrowing of duodenal lumen by torsion of partial volvulus , (3)extrinsic obstruction by Ladd's band ( peritoneal band from cecum to posterior abdominal wall crossing the duodenum) , (4)associated intrinsic duodenal atresia.
Diagnosis :-
Midgut volvulus is true surgical emergency because the delay in diagnosis or operative correction will lead to necrosis of the whole midgut & death.
Plain abdominal X-ray : distended stomach & proximal duodenum with little air in distal small bowel , double bubble sign , or dilated loops of bowel with multiple air-fluid levels.
Upper GI contrast study (barium meal) give us the definitive diagnosis : complete obstruction of second or third part of duodenum , corkscrew (coiled spring ) appearance of duodenum & jejunum , position of DJ is to the right of midline (normally it is to the left of midline).
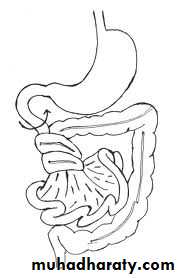
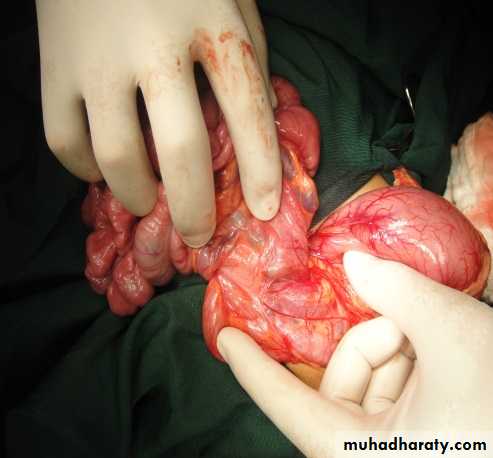
Barium meal volvulus of mid-gut de-torsion of volvulus
Treatment :-
Immediate resuscitation , IVF , NG tube , Foley's catheter , broad spectrum antibiotics , prepare blood , then laparotomy (Ladd's procedure):-Detorsion in counterclockwise direction.
Division of Ladd's band.
widening of the mesenteric base.
Incidental appendicectomy.
Redistribution of bowel ( small in the left side , large in the right side).
Meconium ileus
Meconium ileus is really a wrong name because it is intestinal obstrucrtion due to mechanical obstruction (inspissated meconium) in the terminal ileum due to abnormal composition of fetal meconium due to cystic fibrosis.Pathophysiology :-
Cystic fibrosis is autosomal recessive disease result from mutation (Δ F508 mutation) in the gene responsible for cell membrane protein termed cystic fibrosis transmemebrane regulater (CFTR), which regulate the flow of ions across the epithelial surfaces , so its defect will lead to abnormal electrolyte composition on the epithelial membrane. it affect the respiratory tract , pancreas , & the gastrointestinal tract. The fetal meconium will have less water content, less pancreatic enzyme , sucrase , lipase, more protein & albumin so it will be extremely viscid , thick dehydrated meconium that obstructs the terminal ileum.
Presentation :-
Simple meconium ileus : like any neonatal I.O , failure to pass meconium , progressive abdominal distension , bilious vomiting. Dilated bowel loops which become visible on examination & have doughy character & indents on palpation.
Complicated meconium ileus : volvulus , intestinal atresia , intestinal necrosis , perforation , & meconium peritonitis.
Diagnosis :-
Plain abdominal X-ray : dilated bowel loops , air-fluid levels , soap-bubble appearance (air mixed with tenacious meconium) , peritoneal calcification ,peumoperitonium.
Contrast enema (water soluble - gastrografin) : (it is diagnostic) microcolon of disuse , containing small rabbit pellets of inspissated mucus.
Abdominal ultrasound : ascites , intra-abdominal mass (meconium pseudocyst) , calcification.
Treatment :-
Resuscitation : IVF , NG decompression , antibiotic coverage , vitamin K to correct any coagulopathy.Non-operative management:- (only for uncomplicated meconium ileus)
Using hyperosmolar water soluble enema (gastrografin) under fluoroscopic control through catheter inserted into the rectum , the hyperosmolar gastografin will hydrates & softens the meconium mass result in passage of semiliquid meconium. Sometimes we use 10% N-acetylcysteine solution through NG tube to liquefy upper gastrointestinal secretion.
The success rate of non-operative treatment range from 63-83 % but it has potential risk of : (1) rectal perforation. (2) dehydration & hypovolaemic shock. (3) necrotizing enterocolitis.
Operative management :-
Indications :-
In simple meconium ileus : inadequate evacuation of meconium.
In simple meconium ileus : complication of gastrografin enema.
In complicated meconium ileus.
Surgical options :
Tube enterostomies (T-tube).
Resection & anastomosis .
resection & enterostomy :-
Double parrelled enterostomy (Mikulicz ).
Distal chimney enterostomy (Bishop – koop).
Proximal enterostomy (santulli).