SSI is the major complication of surgery and trauma and has been documented for 4000–5000 years.
Definition
surgical site infection (SSI):The infection that required operative intervention, including that complicated from trauma, operation and burns.
Caused by the invasion and proliferation of pathogens, such as bacteria, viruses and fungi.
Physiology
Bacteria prevented from causing infection in tissues by:Intact epithelial surfaces, but once tissues broken down by surgery , truma…….., bacteria contaminate , invade wounds & cause infections.
mechanical barrier, ex. chemical (such as the low gastric pH).
Immunity
Humoral (antibodies, complement )Cellular (phagocytic cells, macrophages, polymorphonuclear cells and killer lymphocytes).
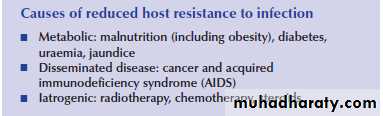
Reduced resistance to infection has several causes:
The wound infection:
The invasion of organisms through tissues following a breakdown of local and systemic host defences, leading to cellulitis, lymphangitis, abscess and bacteraemia.Contamination :
is the presence of M.O in the wound.Infection:
when the M.O invades the tissues and produce ill effects.BACTREMIA: -
Asymptomatic presence of bacteria which are not multiplying in the blood.
it is harmless and follow dental work and instrumentation of urinary tract .
Antibiotic prophylaxis should be given in such cases and to those with prosthetic valves, immunosuppresed patient because these bacteraemia produce harmful effect.Gram +ve bacteraemia less significant than gram –ve .
SEPTICAEMIA:-
Presence of multiplying M.O in the blood stream plus leukocytosis.Sepsis clinically means: significant infection in which bacterial toxins and mediators escape the control of immune system , enter the blood stream and producing chill, fever, pulmonary failure and shock .
Major And Minor SSI
Minor SSI
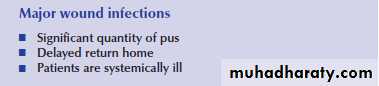
may discharge pus or infected serous fluid but should not be associated with excessive discomfort, systemic signs or delay in return home.Major SSI
The wound discharges significant quantities of pus or needs a secondary procedure to drain it.
The patient may have systemic signs such as tachycardia, pyrexia and a raised white count [systemic inflammatory response syndrome (SIRS).
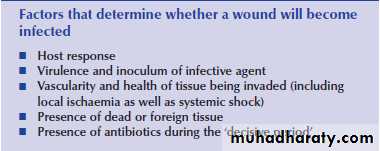
Surgical infection depends on three factors:-
1 – The infectious agent.2 – Host reaction.
3 – Closed space.1 – The infectious agent: -
Either endogenous or exogenous.Endogenous: -
Microflora which are present in the body when the barrier which separate them from sterile area affected.
Example:
skin has staph. and strept. M.O once there is laceration infection occurs.
Gram –ve M.O aerobic and anaerobic present in oropharynx, colorectum, ileum can cause infection if the barrier disrupted.
Exogenous: -
from external environment,eg. hospital, other patients, staff members and improper sterilization.
2 – Host reaction (Immune mechanism) : -
Non specific immunity :-this is done by leukocytes - Phagocytosis and next step killing by lysosomal enzymes. Decrease number of W.B.C as occur in corticosteroid and malnutrition reduces immunity, In D.M. W.B.C kill bacteria poorly than normal .
Specific immunity: -
there is production of antibodiesOn exposure to antigen with subsequent activation of T and B lymphocytes.-Defects in specific immunity as seen in patient with Immunosuppressive therapy, acquired immune deficiency syndrome [A I D S] results in increase susceptibility to Infection.
3 – Closed space: -
infection start in poorly vascularized area such as wound.poor perfusion , hypoxia , acidosis all predispose to infection , special area such as gall bladder , appendix , diverticula are prone to infection once obstructed .
Complications of surgical infections:-
1 – spread of infection occur by: A – Direct spread:- - Necrotizing infections:spread along the anatomical plane like necrotizing fascitis.
- Abscesses:
if not properly drained spread to surrounding tissues.
- Phlegmon:
contain little omount of pus but much edema spread by direct extension.
B- Lymphatic spread:-
strept. And staph. Might spread through lymph vessels producing red streaks in the skin.
C –Blood stream spread:- This result in distant abscess such as appendicitis and inflammatory bowel disease, this called pyaemic abscesses, may cause bacteriaemia and septicemia.
2 – Fistulae and sinus:
like anal fistula, and [pilonidal sinus].3 – Necrosis and gangrene of affected part.
4 – Suppressed wound healing due to infection.5 – Immunsuppression and super infection: -
continuous infection may cause immunosuppression and super infection with normal flora.6 –Gram -ve septicaemias with shock and M.O.F. due to Release of endotoxin .
Diagnosis:-1.Clinical:--Locally the inflamed area is painful, red hot and tender
with loss of function.
-Draining lymph nodes may be enlarged , red , tender
and painful .
-Constitutional symptoms fever, headache, malaise,
tachycardia, Dyspnea, rigor indicate Septicemia or pyaemia.
2. Lab. Studies: -General findings: - There is leukocytosis.In severe sepsis leucopenia or finding of impaired respiratory, renal or hepatic function and DIC.
Bacteriology:-Examine of pus for M.O, culture and sensitivity tests Once culture taken the patient at least 3 days with out antibiotics.Blood culture in serious infections for both aerobic and anaerobic infection.
3. Imaging studies:-plain radiography useful in pulmonary infection, subphrenic abscess and osteomylitis.
Other imaging studies such as US, CT scan and Radioisotopes Study useful in localizing infection.
Principle of Treatment: -
1 – Incision and drainage once pus is formed.2 – Excision: -like appendectomy, amputaion of gangrenous limb and excision of dead tissue.
3 – Antibiotics in addition to the above measures .
4 – General supportive measures like control of DM revascularization in ischemia and nutritional support .
BACTERIA INVOLVED IN SURGICAL INFECTION
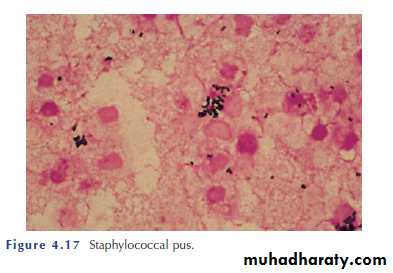
1-Staphylococci:-Commonest gram +ve M.O., 25- 50 % of normal adults found on skin, nostrils , Staphylococci form clumps.Staphylococcus aureus
is the most important pathogen in this group, Strains resistant to antibiotics (e.g. MRSA) can cause epidemics and more severe infection.Infections are usually suppurative and localized.
It cause pustules, boils, paronychia, breast abscess, osteomylitis, infected wound and pneumonia.
Usually sensitive to penicillin but now days there are resistant strains.
2 – Streptococci: -Streptococci form chains & are Gram +ve two types
Hemolytic.
Non Hemolytic.
Hemolytic
The most important is the β-Hemolytic are often present in oropharynx .The group A - β-Hemolytic Streptococcus, also called Streptococcus pyogenes, they can cause spreading infection like cellulites, lymphangitis and erysipelas.
Non hemolytic less virulent, found in the mouth and bowel [entercocci].
3-Clostridia
are Gram-positive, obligate anaerobes, which produce resistant spores.
Clostridium perfringens is the cause of gas gangrene.
C. tetani causes tetanus.
Clostridium difficile cause pseudomembranous colitis.
pseudomembranous colitis
This is HAI, caused by the overuse of antibiotics.The cephalosporins and other anti-staphylococcal antibiotics seem to be the cause.
symptom of bloody diarrhoea can occur.a severe colitis may lead to perforation and the need for emergency colectomy, with high mortality rate.
Treatment
resuscitation and antibiotic therapy with an imidazole or vancomycin.4– Aerobic gram –ve bacilli
Escherichia coli [E. coli]:-found in the intestine of human being, alone or mixed with other are the responsible M.O for suppurative sepsis of abdomen and urinary tract.
Klebsiella: -
gram –ve found in respiratory tract and can cause fulmenant pneumonia in debilitated patients.
Pseudomonas aeroginosa:-
IT causes primary infection or secondary infection in burns and surgical wounds , Present in20% of cases. It is characterized by blue green color pus and bad odor.
Once it is infected the wound it is very difficult to eradicate.
Proteus: -
common causes of urinary tract infection also infected burn and surgical wounds.5– Anaerobic bacteria: - obligatory anaerobes, chiefly peptostreptococci and gram –ve bacilli bacteroids found on skin and mucous membranes.
The M.O are non-spore-bearing, strict anaerobes that colonise the large bowel, vagina and oropharynx can invade the tissue once the barrier is disrupted producing abscesses, including intra-abdominal abscesses, after colorectal or gynaecological surgery. and invade blood stream leading to septicemia.
These abscesses characterized by tissue necrosis, foul smelling discharge and gas formation, usually such M.O fail to grow in aerobic culture.
They are sensitive to metronidazole and some cephalosporins (e.g. cefotaxime).
Classification:
Non-specific infection:suppurative infection presentation:
redness, swelling, hot, soreness
Pathogens: Staphylococus aureus, Streptococci.
Specific infection:
Tetanus, Gas Gangrene,Tuberculosis.
Acute non specific infection:-
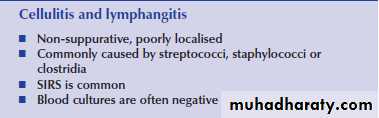
Cellulites :-Caused by gram +ve bacteria mostly streptococci or staph. in to the skin and subcutaneous tissue , mostly M.O enter through prick or scratch .
Pathology : -
Invasive suppurative infection of loose connective tissue ,although there is large amount of polymorph nuclear leukocytes , there is no pus formation.Clinical picture :-
- Skin red or reddish brown , indurated , hot and painful .- Spread rapidly and the edge ill defined.
- There might be skin blisters.
- High or moderate fever.
- Lymphatic spread produce red streaks of lymphangitis and regional lymph nodes .Differential diagnosis:-
- Contact allergy.
- Chemical inflammation at the site of injection.
- Deep vein thrombosis.
Treatment:
- Antibiotics [penicillin group].- Rest and elevation of the affected part.
- Hot packs.
- If no response after 48 hours review the diagnosis or Pus has been formed and need drainage.
Erysipelas:-
Rapidly spreading non suppurative inflammation of the lymphatic of the skin caused by hemolytic strept.,the M.O gain access through scratch or abrasion .Clinical:-- Symptoms of toxemia are present.
Locally the picture is similar to cellulites,
but there are Some Differences:-The skin is rose pink.
The edge is well defined, slightly raised and often shows minute vesicle just below the spreading margins .
- There may be islets of inflammation beyond the spreading margin separated by normal skin .
Complications:-- Facial erysipelas may lead to cavernous sinus thrombosis.- Septicemia.- Recurrent erysipelas may block the lymphatics leading
to elephantiasis .
Treatment:-The patient should be isolated, it is very contagious.- Antibiotic.- Rest in bed.- Hot packs.
Boil [furuncle]:-
Staph. infection of hair follicle or sebaceous gland, it may occur in any hirsute area, but common in face, neck and axilla .Boil common in D.M with lack of personal hygiene.Clinical picture:-Small painful red indurated, swelling, very tender, early treatment boil resolve with out suppuration [blind boil], more often necrosis of the central part occurs and discharged with small bead of pus.
Treatment:-
- Antibiotic effective against staph.
- Painting the surrounding skin with an antiseptic to
prevent infection of surrounding area.
- Always suspect D.M in patient who develop recurrent boils.
Furunculoisis
Carbuncle:-
infective gangrene of the subcutaneous tissues secondary to infection by staph. aureus .It is common in immunocompromised patients as diabetic.The infection occurs mainly in the face, nape of the neck and the back.Pathology :-Infection usually start in the hair follicles and then spread to other hair follicles and to subcutaneous fatty tissue and result in multiple area of necrosis and thrombosis of blood vessels, patch of skin under go sloughing and separate from underlying granulation tissue.
Clinical:-
- Toxemia
- Painful induration of skin and subcutaneous tissue.
- The skin is red.
- As the swelling enlarges its central part become soft, but no fluctuation, multiple areas of skin thin out and separate forming multiple sinuses through which slough come out with little pus.
Complications:-
1- Local spread to lymphatics and cellulites.2- Pyaemia and septicemia.
3- Carbuncles of the face can lead to cavernous sinus thrombosis .
Treatment:-
1 -Antibiotic effective against resistant staph.2 -Culture and sensitivity test of discharge.
3 -Proper control of D.M.
4 -Excision of the sloughs.
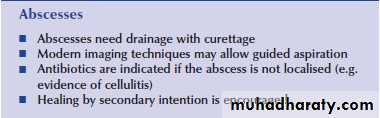
Acute Abcess:-
Localized suppurative inflammation caused by pyogenic M.O mostly staph produce coagulase enzyme which localizes the acute inflammatory process.
Causes:-
1. Direct access of M.O to the affected part throughabrasion or wound .
2. Local extension from adjacent focus osteomylitis of
jaw from infected tooth .
3. Lymphatic spread through lymphatic vessels to lymph
nodes.
4. Blood stream, M.O gaining access to circulation go to
distant organs, liver abscess, lung abscess .
Pathology : -
Grossly :-An abscess consist of three zones :-I.Central zone
of coagulative necrosis , this ultimately separates from surrounding tissue and forms slough which becomes liquefied by the enzymes of dead leukocytes ,an abscess cavity forms contain plasma cells and inflammatory exudates
II.Intermediate zone
of granulation tissue protect other tissue from the effect of bacteria and toxin.III.Peripheral zone
of inflammation fade gradually into surrounding tissue.
Fate: -
1.Resolution if resistance high and early treatment.
2. Pointing and abscess drained rupture out.
3.Spread of infection locally, by lymphatic or blood.
4.Chronic improper treatment hard mass, increase fibrosis ( ANTIBIOMA )
Clinical Features :-
Painful tender mass , skin over it red edematous .Lymph nodes enlarged and tender, there is systemic reaction inform of fever, malaise, headache, tachycardia and anorexia.When pus formed the following changes are noted:-
1. Pain become throbbing.2. Temperature becomes hectic.3. Covering skin pitting edema.4. Inflammation becomes localized.
5.Fluctuation can be elicited in subcutaneous abscess, in deep abscess like gluteal and perinpheric abscess.
Treatment:-
Once pus is formed treatment is drainage.1. Incision and drainage is the standered method , incision done over the pointing area , with skin crease , all loculi should be broken and pus send for culture and sensitivity test , rubber or gauze drain put to allow free drainage and prevent early closure before all pus come out . Antibiotic cover.2. ultrasound or C-T scan guided aspiration drainage for deep seated collection [ intraperitoneal abscess ]
Special infections TETANUS:-
It is specific anaerobic infection caused by clostridium tetani which produce neurotoxin which affect nervous system and muscles.
M.O is gram +ve spore forming bacillus, the spore is in the terminal end of the bacillus forming drum stick appearance.
It is present in the soil, dirt, intestine of horses.
Mode of infection : -
Through contaminated wounds with soil, dirt, penetrating wounds, hypoxic contaminated wounds with foreign bodies and devitalized tissue .or through umbilical stump( tetanus neonatorum).
Pathology: -
M.O produce neurotoxins which reach the C.N.S via blood stream causing severe muscle spasm.pneumonia , exhaustion , and hyperpyrexia .
Death due to heart failure, respiratory failure.Once neurotoxin fixed to CNS no benefit of antitoxin.
Clinical picture: -
Incubation period 1-15 days in non immunized patient,in immunized patient up to several weeks or months .
Tonic stage :-
the first symptom usually limitation of movement of the jaw [ Trismus ] [ lock jaw ] , spasm of facial muscles [ Risus sardonicus ] followed by stiffness of the neck , laryngeospasm , difficulty in swallowing and micturationClonic stage :-Attack of violent muscular contraction , the spasm initiated by stimulus like bright light , tonic and clonic spasm .
Spasms become more and more muscles involved, apnea due to involvement of intercostals muscles and diaphragm.
Temperature high, sweating, tackycardia.
Differential diagnosis :-1. Trismus for arthritis of the jaw, impacted wisdom tooth.
2. Meningitis neck rigidity, CSF.
3. Strychnine poisoning.
4. Tetany hands and feet are more affected low Ca+ level.
5. Rabies history of dog bite and hydrophobia.
Prevention:-
- Immunization program for children .- Injured patient whom receive 1-3 doses for the last 10 years receive booster dose of tetanus toxoid.
- Patient not previously immunized we give them toxiod with tetanus immunoglobulin.
Treatment:-
- Patient should be in intensive care unit .- Give antitoxin preferably in the proximal part of the wound.
- Excision of the contaminated wounds, left open with Hydrogen peroxide and antibiotic.
- Patient given sedation like Valium, phenobarbitone and even put on ventilator .
- Intubation or tracheostomy .
- Penicillin G 10-40 million unite given I.V.
- Nursing isolated room, feeding by nasogastric tube.
Prognosis: -
30-60% mortality rate in established case with respiratory involvement .
GAS GANGRENE [CLOSTRIDIAL MYOSITIS]
Acute spreading gangrene associated with gas formation and profound toxemia due to infection of extensive wounds by the anaerobic spore bearing bacillus clostridium perfringens [ welchii ]It is closely related to grossly contaminated war injuries .Factors predisposing to gas gangrene:-
1. Lacerated wounds involving muscles of the gluteal region and thigh .2. Presence of F.B or devitalized tissue.3. Ischaemia of muscle due to vascular injury, tight bandage or cast or suture under tension.
4. Infection with aerobic bacteria which make the medium suitable for anaerobic infection.
5. Gas gangrene may follow above knee amputation in elderly due to faecal contamination.
Pathology: -
Clostridia produce toxins and cause severe infection with tissue necrosis, the toxins cause:-1. Muscle necrosis.
2. Haemolysis and mild jaundice.
3. Degenerative changes in the liver kidney and adrenal.
Clinical features: -
Incubation period varies from few hours to few days.General:-1. Patient pale, anxious and apprehensive.
2. Increase temp. and pulse rate.
3. The hands cold and clammy.
4. An icteric tinge may be present and there is oliguria.
5. In severe cases patient is shocked.
Locally:-1. Pain, numbness in affected area.
2. Wound is swollen with crepitus with gas bubbles.
3. Dark red, greenish to dark discoloration of muscles.
They don’t contract or bleed on pinching.
4. Skin green or dark, multiple blebs, full of dark fluid with foul smelling .
Differential diagnosis :-
- Non clostridial gas forming infection cause by mixtur of gram-ve bacilli [ E. coli ] and gram +ve cocci ,the infection as virulent as gas gangrene need incision ,Drainage and antibiotics.- Surgical emphysema: - presence of gas under the skin, It is not associated with toxemia.
Prevention:-
1. Wound debridement of all contaminated wounds underGA all dead tissue and muscles removed.
2. Antibiotic therapy Penicillin.
3. Circulatory support to avoid tissue hypoxia.
Treatment:-
1. Wound management: - under G.A .all dead tissue and muscles removed , facial compartment opened , no closure of wounds amputation if necessary .2. When infection or wound near anus and soiling occur,Diverting colostomy should be done.
3. Hyperbaric oxygenation to decrease bacterial growth and production of toxin 3 atom for 1-2 hour repeated every 6-12 hours .
4. Fresh blood also important.
5. Antibiotics 20- 40 million unit/day penicillin given IV if sensitive to penicillin clindamycin or Metronidazole , anti gas gangrene no more given now.
Prognosis: - mortality rate 20%.
TREATMENT OF SURGICAL INFECTION
Suppurative wound infections take 7–10 days to develop, and even cellulitis around wounds caused by invasive organisms (such as the β-haemolytic Streptococcus) takes 3–4 days to develop.Major surgical infections with systemic signs, evidence of spreading infection, cellulitis or bacteraemia need treatment with appropriate antibiotics.
E
N
D