1
L2
Prostate Cancer
Carcinoma of the prostate
Is the second most common cause of cancer related death in men older than 50 years of age
after carcinoma of the lung with peak incidence between the ages of 65-75 years.
Autopsy studies show that 30% to 40% of men over 50, who had no symptoms of prostate
cancer whilst alive, have histological evidence of prostate cancer at the time of death. This
percentage rises to 60% to 70% in men over 80 years of age.
Proposed Risk Factors
ⱴ Family history
ⱴ Diet, fat, obesity, alcohol
ⱴ Hormones
ⱴ Smoking
ⱴ Sexual activity (early, multiple partners, STD)
ⱴ Chemicals, toxins, radiation
ⱴ Viruses (Herpes 2, CMV)
ⱴ Vasectomy
ⱴ BPH
Pathology
70-80% of Ca prostate arise in the outer peripheral glands and hence may be palpable as
irregular hard nodules by rectal digital examination and because of its peripheral location. Ca
prostate less likely to cause urethral obstruction in early stage than nodular hyperplasia.
Grossly
Early lesions appear as ill-defined mass just beneath the capsule of the prostate. On cut
section, foci of CA appear as firm gray white to yellow lesions that infiltrate the adjacent gland
with ill defined margin.
ⱴ Metastases to regional pelvic lymph nodes may occur early. In advance cancers
invasion to seminal vesicles, periurethral zones of the prostate, wall of the bladder may
occur but the rectum is rarely involved by invasion that is because there is a connective
tissue separating the lower genitourinary tract structures from the rectum, which
prevent the growth of the tumor posteriorly.
Pathology of Male Reproductive System
2
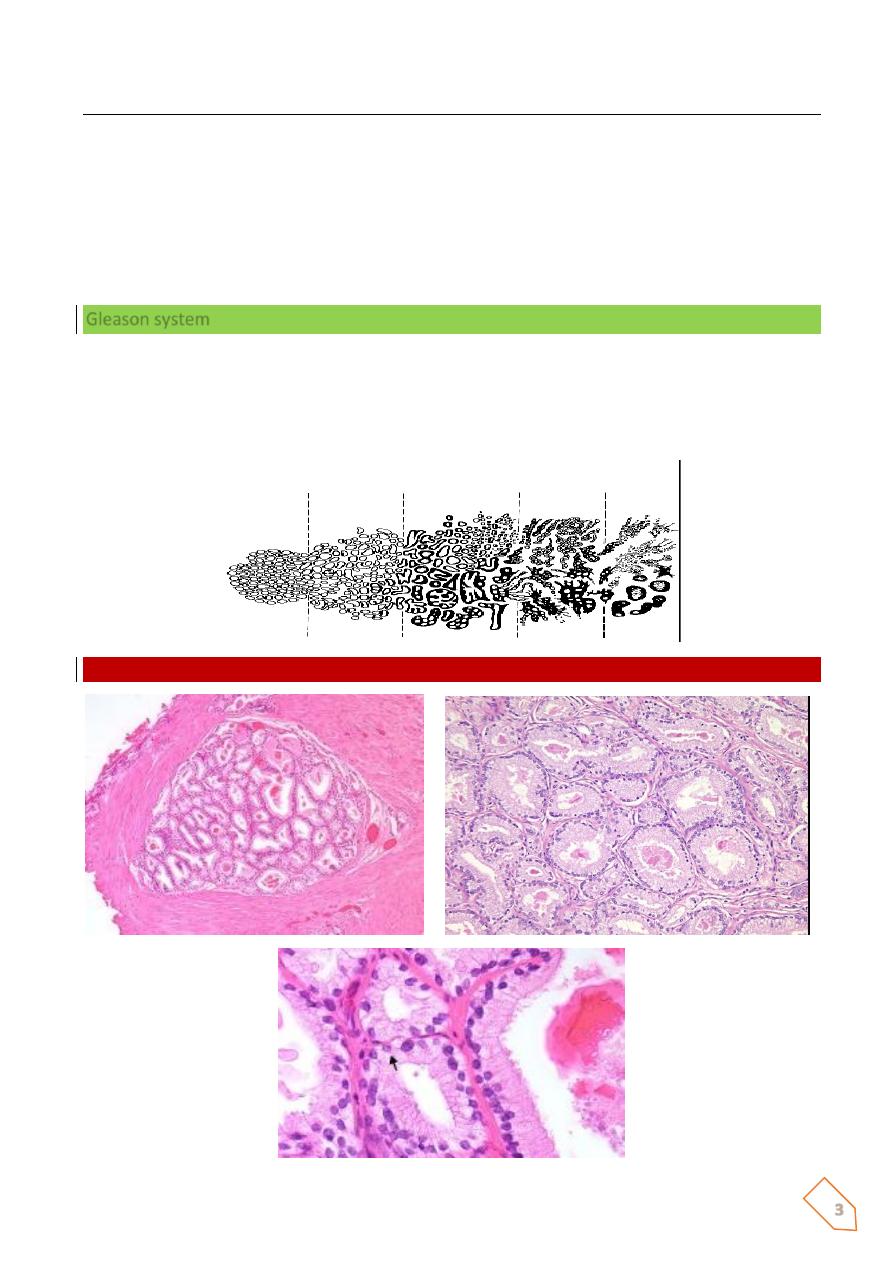
ⱴ Well-differentiated adenocarcinomas are composed of small glands infiltrate the
adjacent stroma in irregular haphazard fashion. In contrast to normal and hyperplastic
prostate
ⱴ The glands in carcinoma doe not encircled by collagen or stromal cells but they appear
to have (back-to-back) appearance.
ⱴ The neoplastic glands are lined by a single layer of cuboidal cells with conspicuous
nucleoli ;( the basal layer seen in normal and hyperplastic glands is absent).
ⱴ The undifferentiated adenocarcinoma characterized by
1) increasing variability of gland size and configuration
2) papillary and cribriform patterns
3) sometimes there is no gland formation but there is a solid cord or sheet of
infiltrating malignant tumor cells within the stroma.
Clinical features:
Ca prostate are often clinically silent especially during early stages, but 20% of localized ca
are discovered accidently during histological examination for biopsy removed for nodular
hyperplasia.
Discovered accidently during routine digital rectal examination as hard firm nodules under
the capsule of peripheral glands.
More extensive Ca may produce signs and symptoms of prostatism due to lower UT
obstruction.
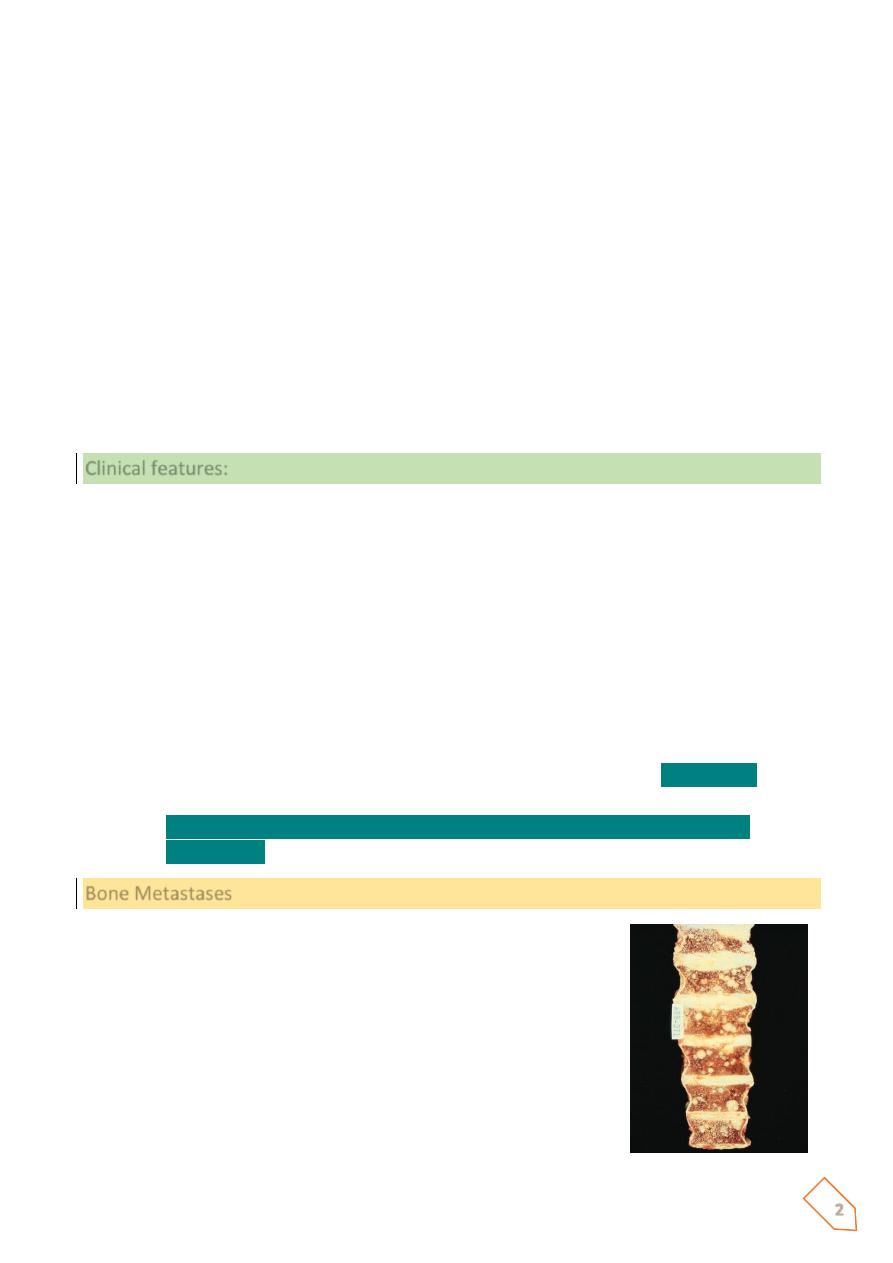
ⱴ More aggressive tumor may give clinical presentation of metastases. Bone
metastases especially to axial skeleton is the most common and prostatic Ca may
cause either osteolytic (destructive lesion) or more commonly
osteoblastic
lesions(bone producing lesions).
ⱴ
The presence of osteoblastic metastases is strongly suggestive of advance
prostatic Ca.
Bone Metastases
ⱴ Spinal mets ->
ⱴ Painful
ⱴ May cause lots of reactive bone growth at the site of the
met
o Osteoblastic
ⱴ May cause bone destruction
o Osteolytic
3
Microscopically
Most Ca prostate are adenocarcinomas with variable degree of differentiation. They originate
from intraductal dysplastic foci termed prostatic intra epithelial neoplasia (PIN) which is a
premalignant state in which the prostatic ducts lined by cytologically a typical luminal cells
and a concomitant diminution in the number of the basal cells.
PIN is of low and high-grade patterns, it precedes the appearance of invasive carcinoma by
two decades, and there severity increases with increasing age.
Gleason system
ⱴ Based on architectural pattern
ⱴ Cytological features not factored in
ⱴ Overall grade is not based on highest grade component
ⱴ Score = Primary pattern (1-5)+ secondary pattern (1-5)
Pattern 1
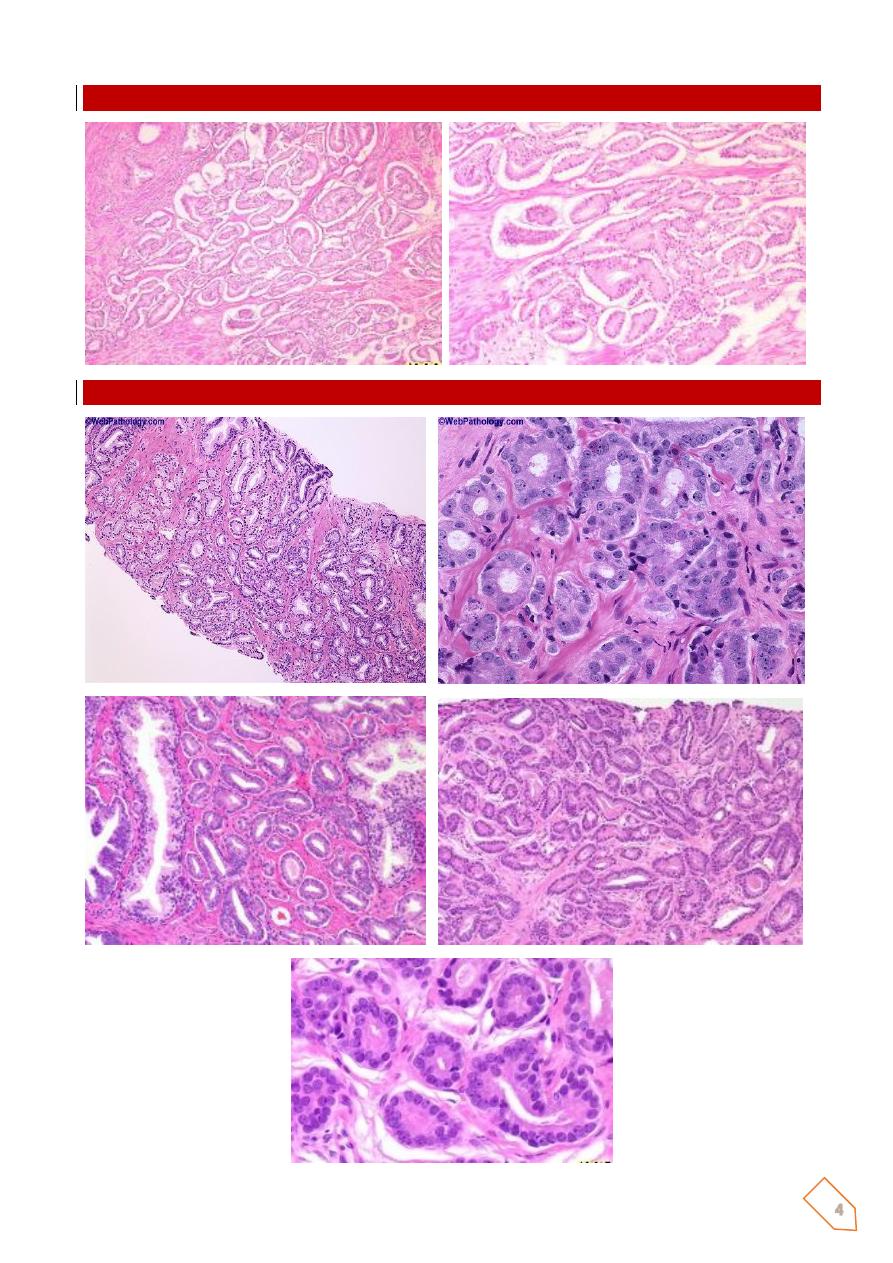
4
Pattern 2
Pattern 3
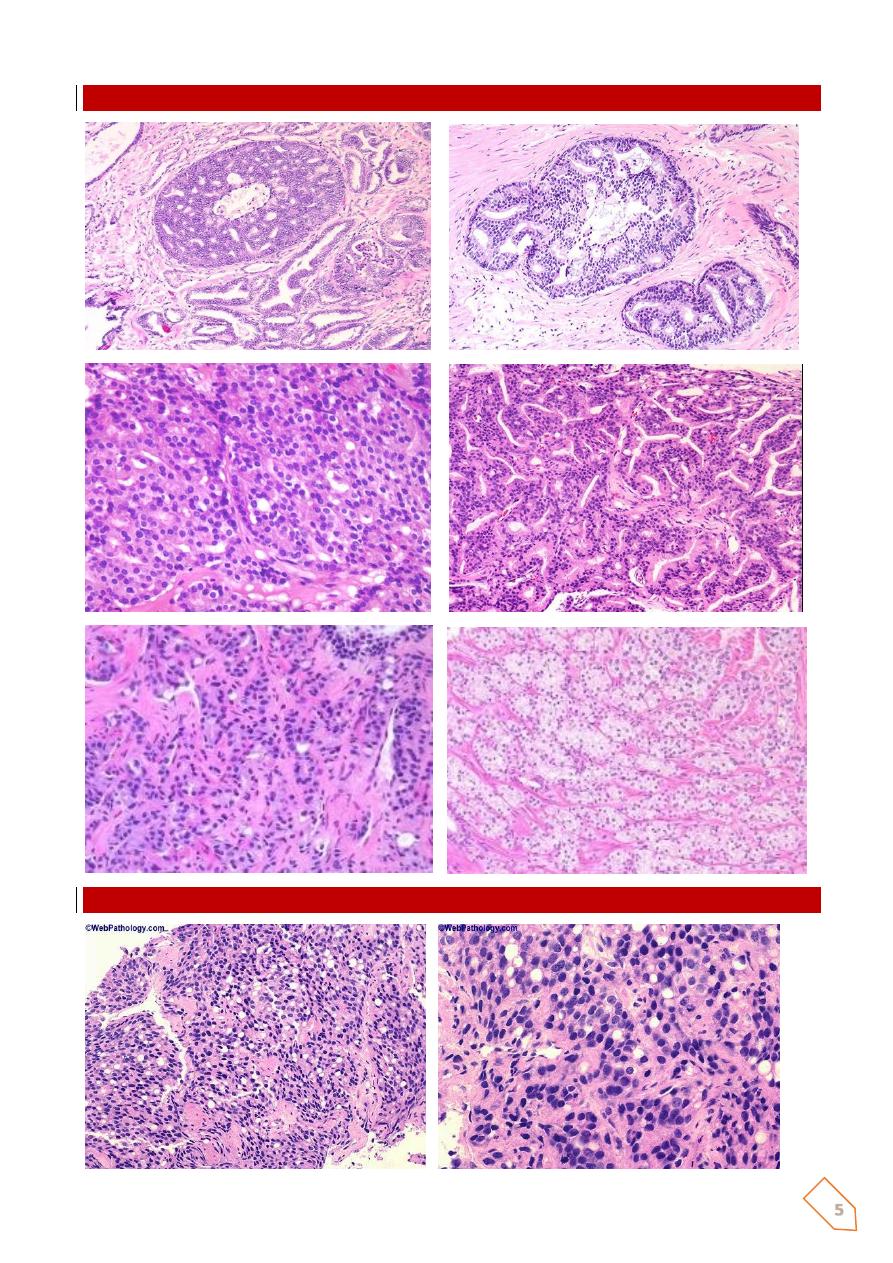
5
Pattern 4
Pattern 5
6
Prostate Cancer
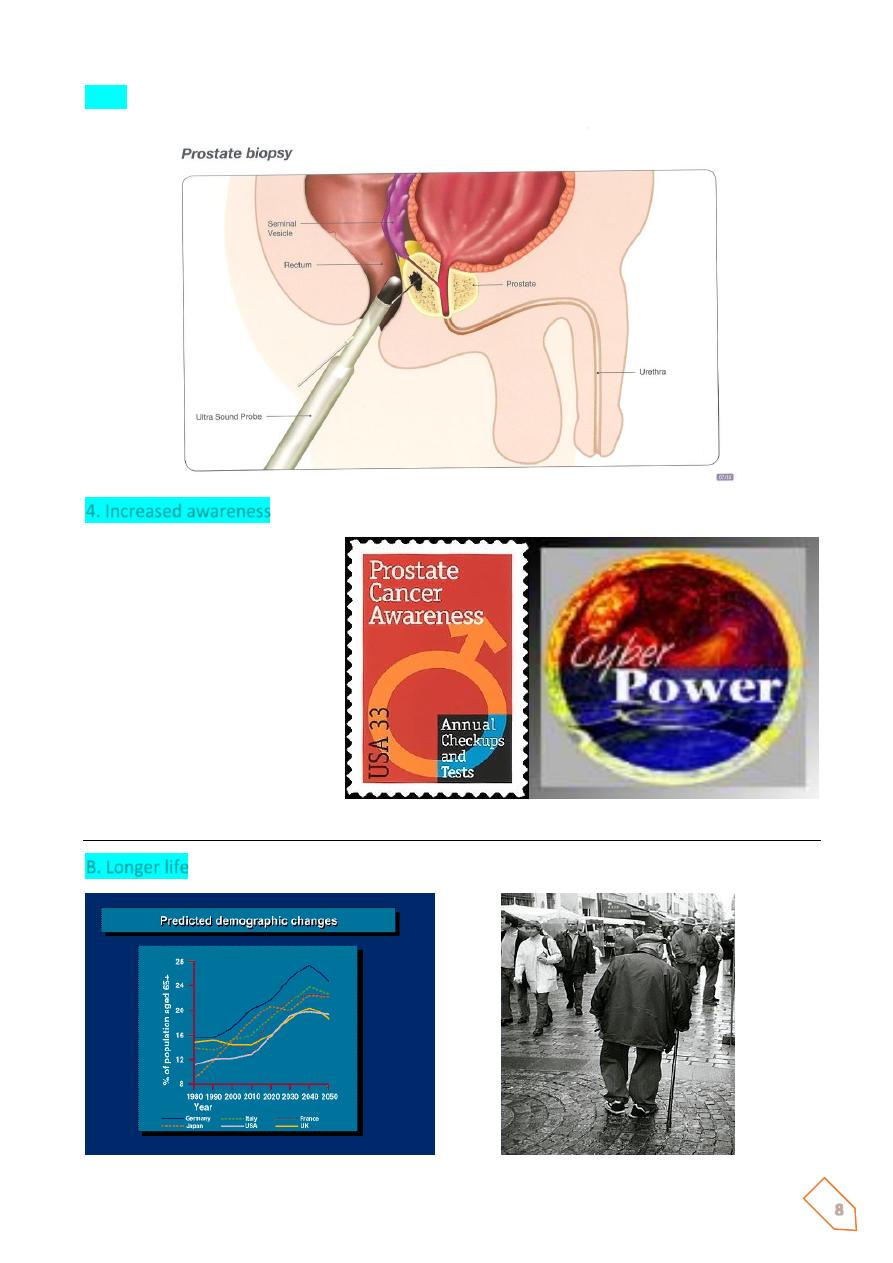
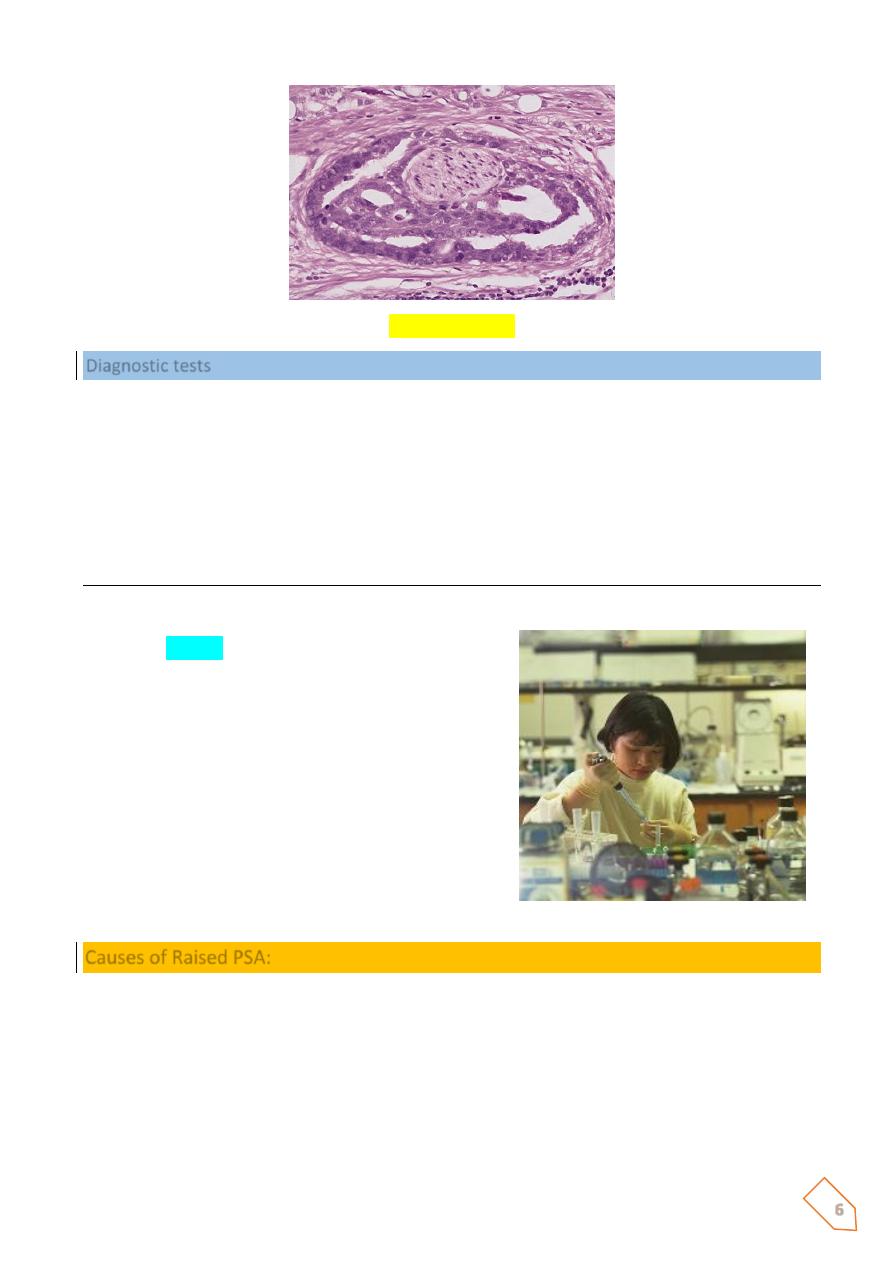
Diagnostic tests
ⱴ DRE
ⱴ PSA
ⱴ TRUS
o To identify lesions of suspected malignancy
o To improve the accuracy of prostate biopsies
ⱴ Prostate biopsies
Causes of increased incidence
A- Early detection:
1. PSA
ⱴ prostatic
–specific
antigen
(PSA)
is
proteolytic enzyme produced by both
normal and neoplastic epithelium. It
secreted into prostatic acini then into the
seminal fluid where it increases the motility
of the sperm by maintaining the seminal
secretion in a liquid state.
ⱴ It s upper normal limit value 4ng/L. it is used
in the diagnosis of early Ca but it is of limited
that due to
Causes of Raised PSA:
ⱴ Prostaitc cancer
ⱴ BPH
ⱴ Prostatic infarction
ⱴ Prostatic manipulation
ⱴ Prostatic biopsy
ⱴ Acute urinary retention
ⱴ Urethral catheterisation
7
Age related reference limits:
<49y
50-59y
60-69y
70-79y
<2.5 g/l
<3.5
<4.5
<6.5
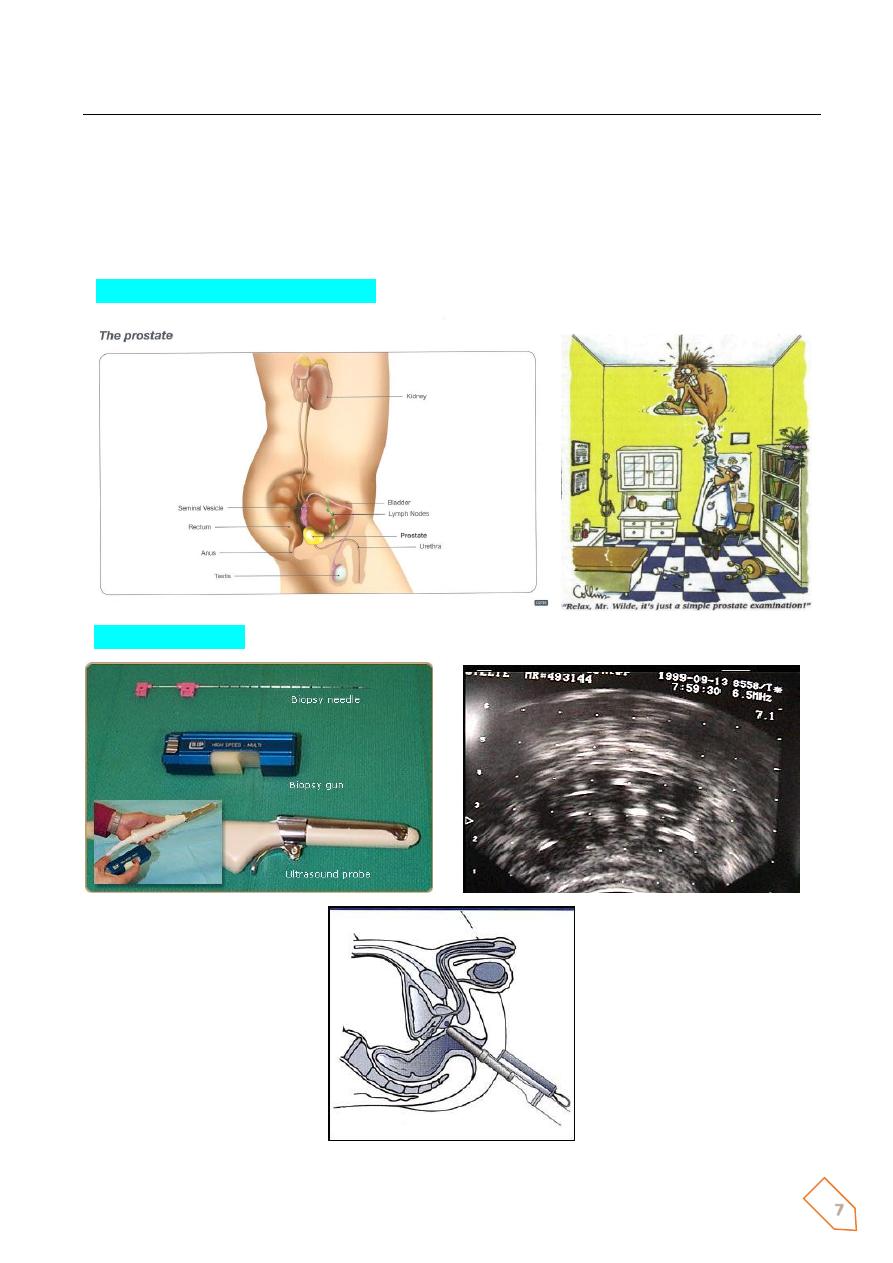
2. Digital Rectal Examination (DRE)
3. TRUS and Biopsy
9
Incidence versus Age
ⱴ Rare < 40
ⱴ latent cancer (at autopsy) =
o 10% at 50 years
o 80% by 80 years
Grading of Prostatic Ca.
Gleason’s System
ⱴ Grades 1-5
ⱴ Scores 2-10
ⱴ Strongest predictor of biologic behaviour
ⱴ Should be included with other prognostic factors in therapeutic decision making
e.g- age, health status, clinical stage, PSA
Transitional cell carcinoma
3 types are identified:
1. Direct extension/invasion from the bladder
2. Spread from the bladder along prostatic ducts
3. Primary TCC of prostatic urethral lining with no lesion in bladder
Mesenchymal Tumours
ⱴ Phyllodes (Benign & Malignant)
ⱴ STUMP
ⱴ Leiomyoma & Leiomyosarcoma
ⱴ Spindle cell nodule (post operative)
ⱴ Pseudosarcomatous fibromyxoid tumour
ⱴ Solitary fibrous tumour
ⱴ Embryonal rhabdomyosarcoma
10
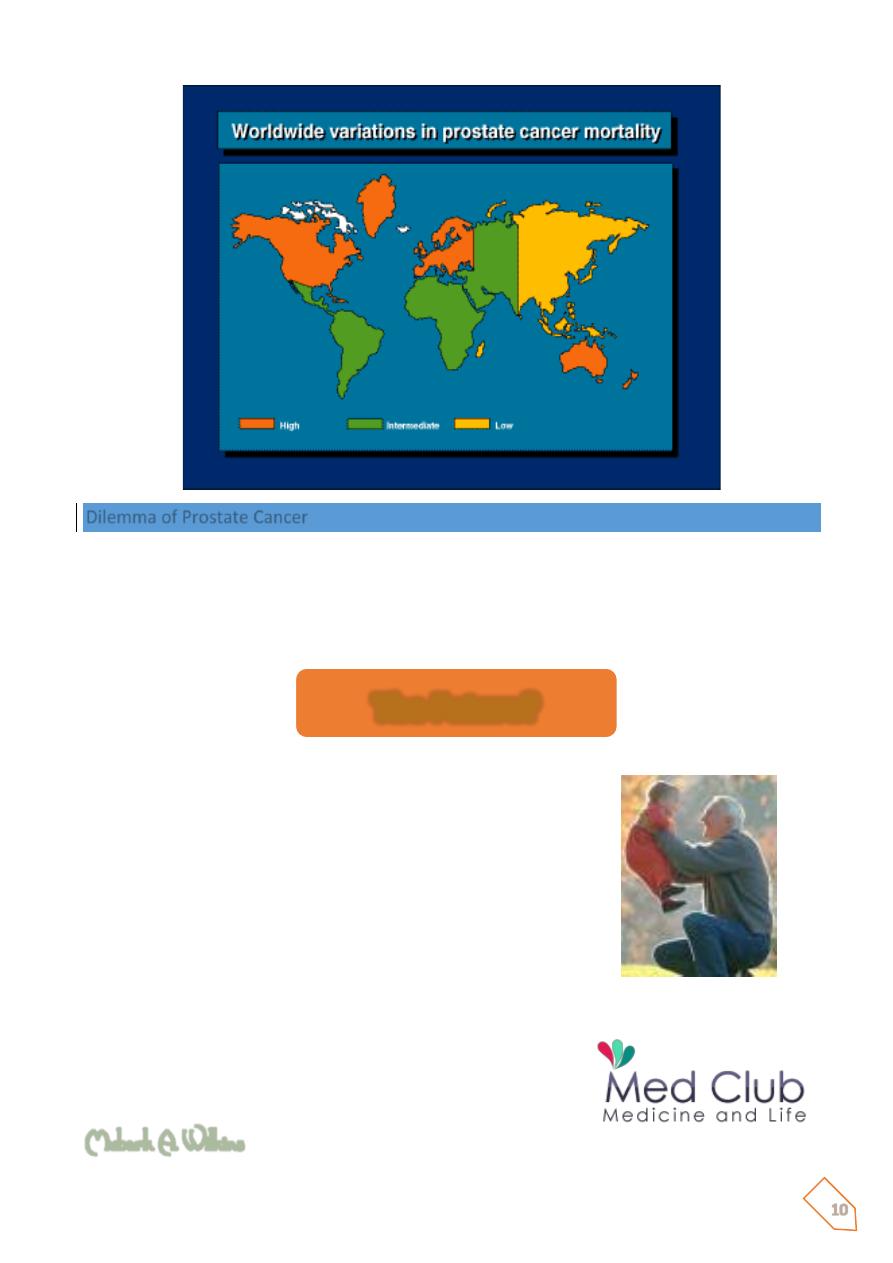
Dilemma of Prostate Cancer
30 - 50% of patients undergoing radical surgery for localised disease have extra capsular
extension at the time of surgery.
Current staging tests are inadequate to accurately identify these patients.
1- PIN versus CANCER
2- To understand the biological behaviour of prostate
cancer
3- To improve staging methods
4- Standardisation of Treatment
To achieve a good quality of life for men with Prostatic
Cancer
Mubark A. Wilkins
The Future?