clinical Images
Dr. Hussein Mohammed Jumaah
CABM
Mosul Medical College
Mosul-Iraq
2016

Nail Exam
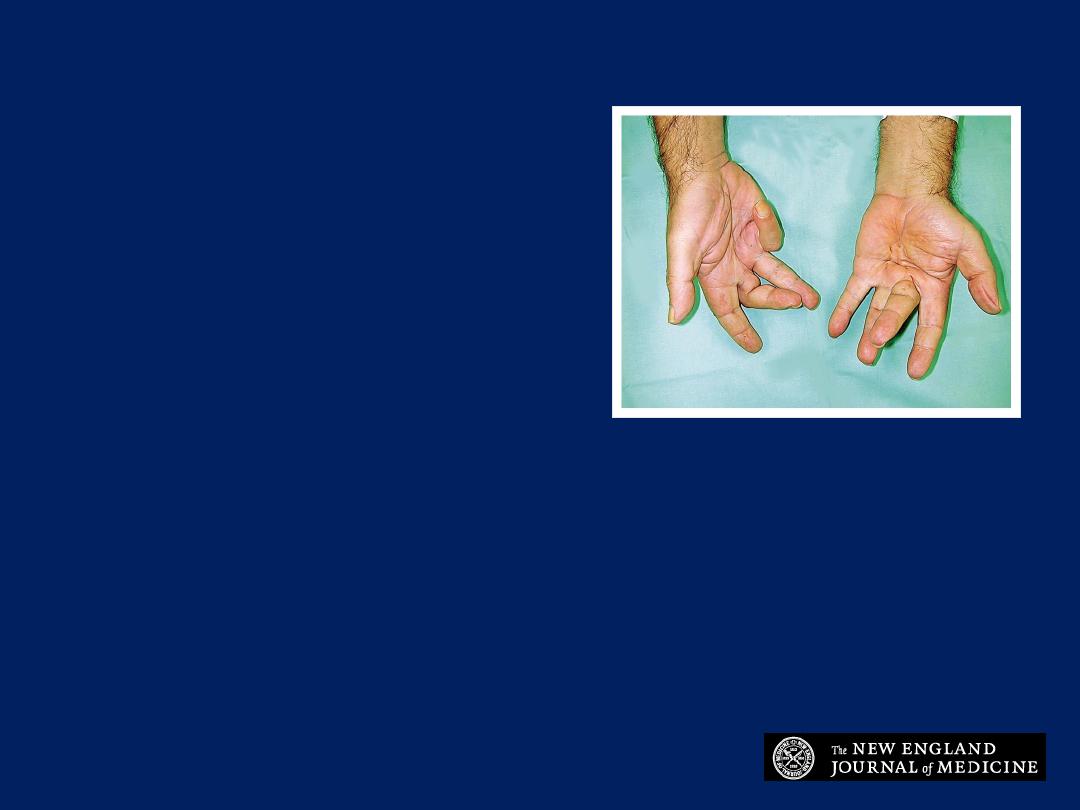
Clubbing
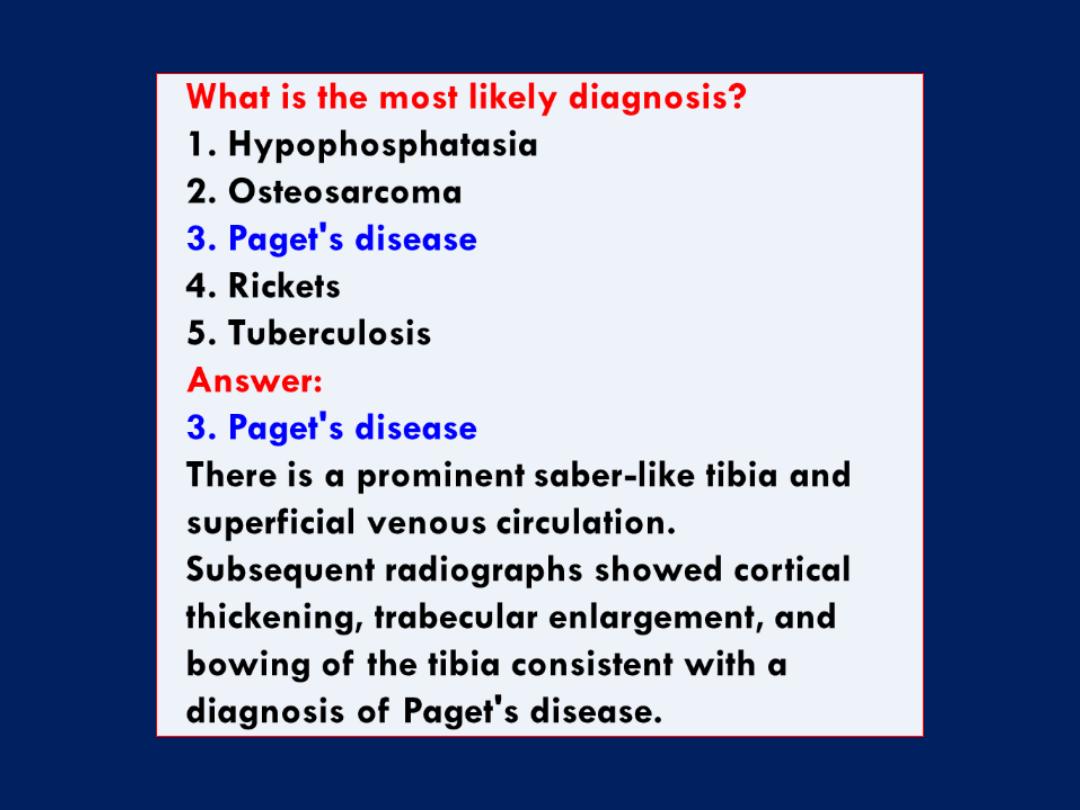
What is the most likely
diagnosis?
1. Acromegaly
2. Cystic fibrosis
3. Eisenmenger's syndrome
4. Squamous-cell lung
cancer
5. Ulcerative colitis
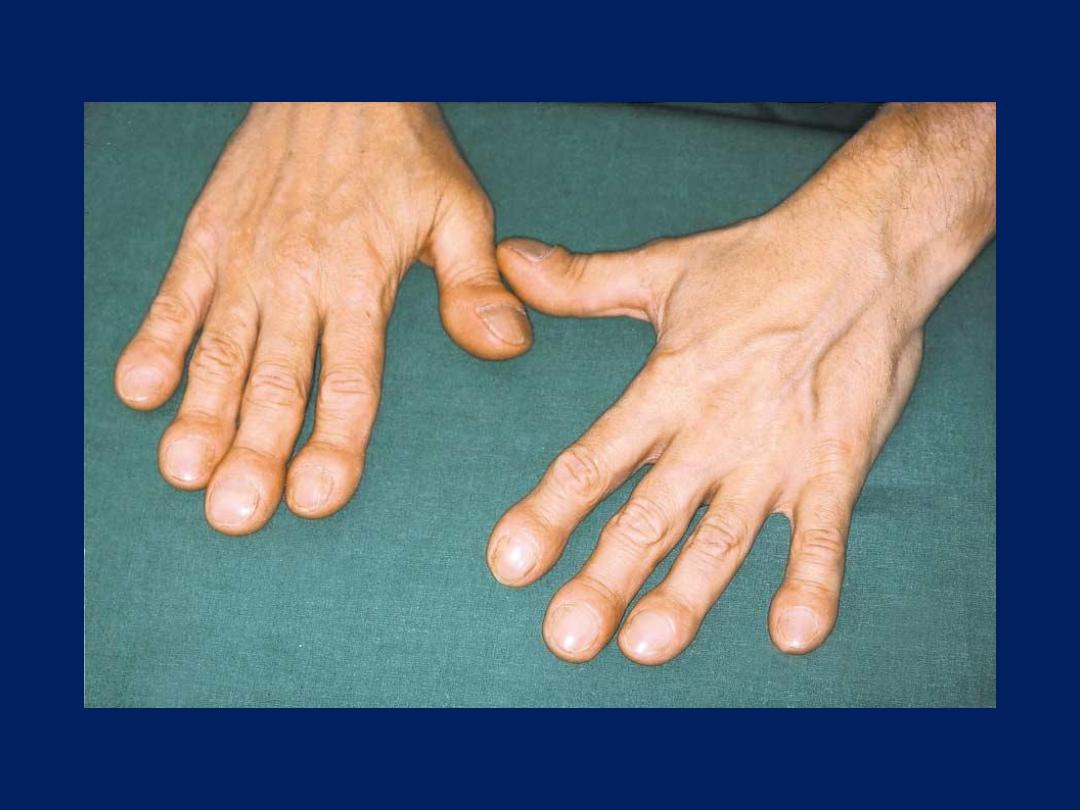
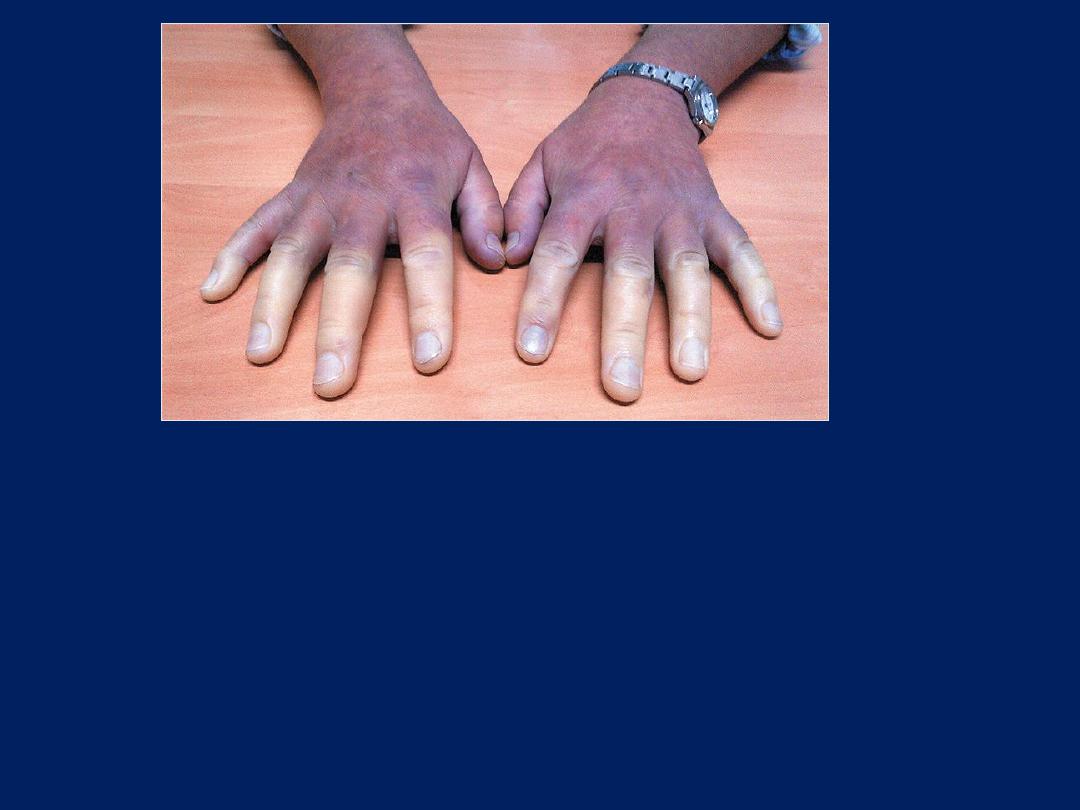
Eisenmenger's syndrome
When
Eisenmenger syndrome
occurs in
concert with a patent ductus
arteriosus, deoxygenated blood from
the right ventricle is delivered to the
aorta distal to the left subclavian
artery. The upper extremities are thus
spared the effects of the shunt,
whereas the lower extremities are
not, resulting in differential clubbing
and cyanosis.
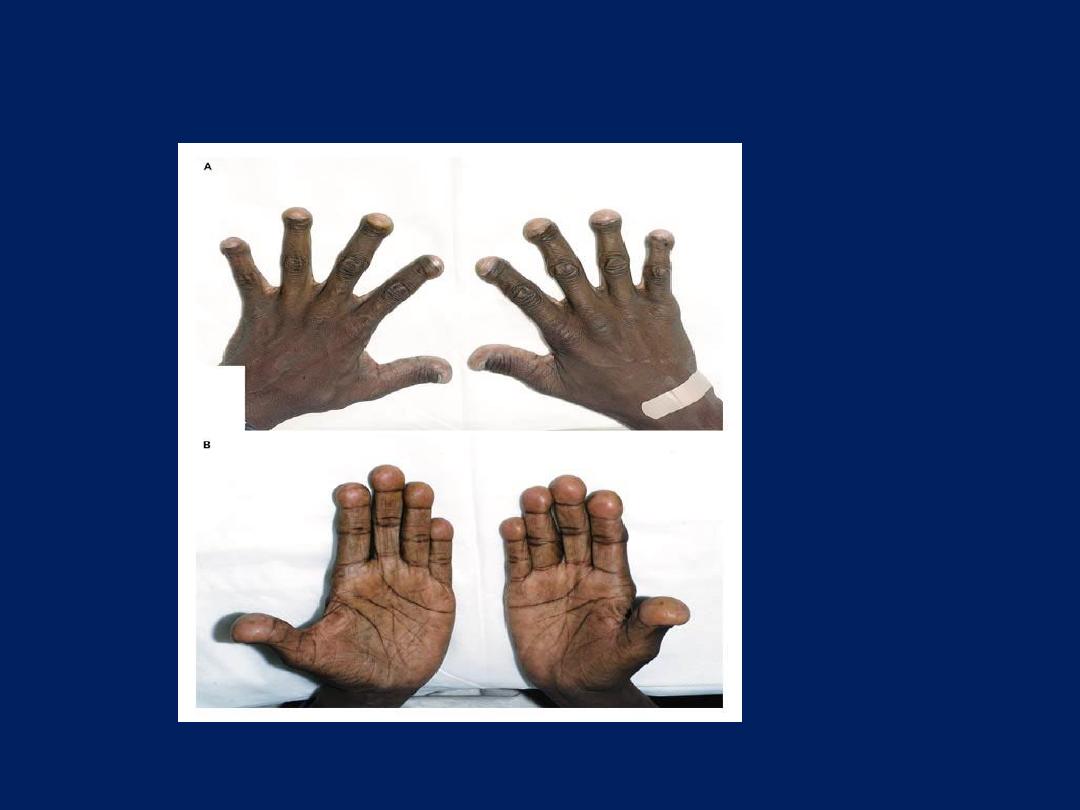
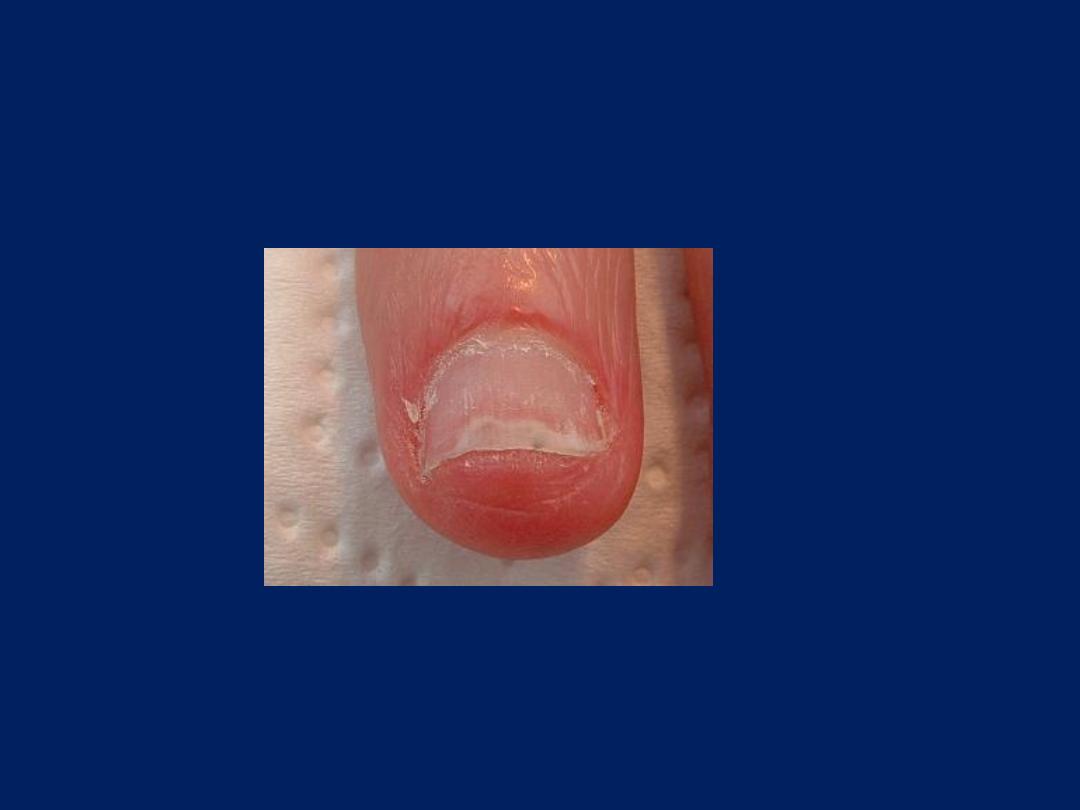
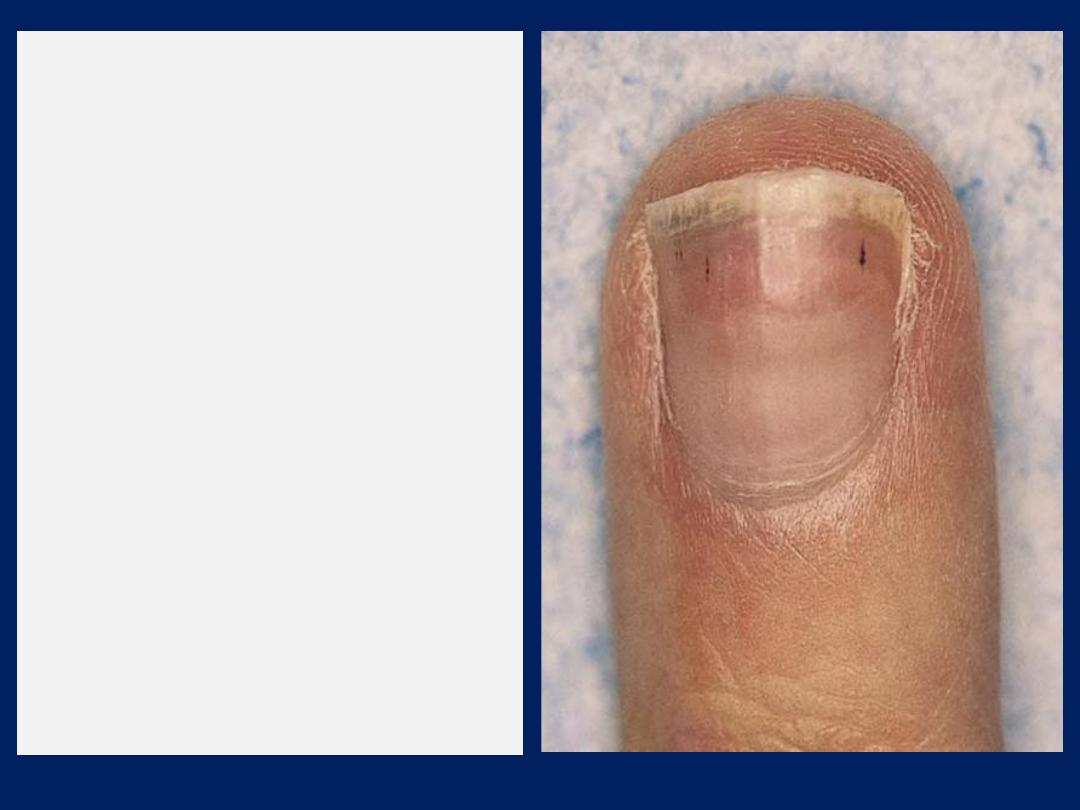
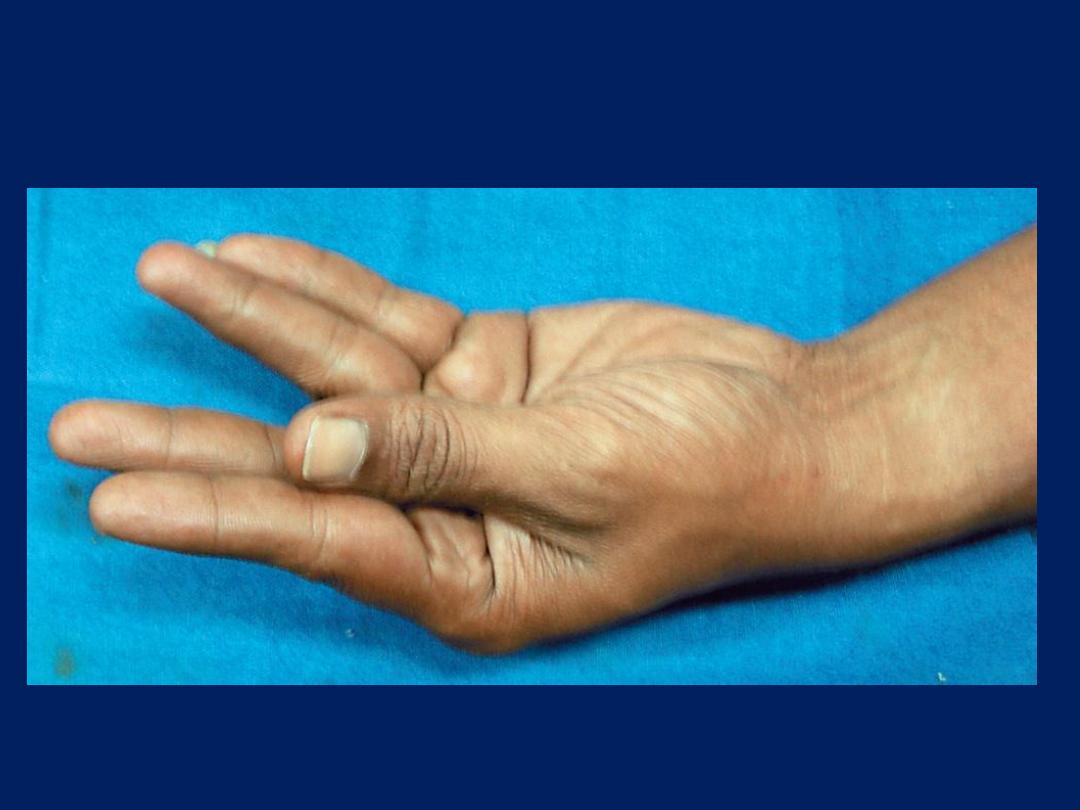
Pseudoclubbing
A 36-year-old man was referred for further evaluation after having
changes in his fingers that were initially thought to be due to clubbing
(Panels A and B). He had a history of obstructive nephropathy
necessitating hemodialysis and renal transplantation. His course had
been complicated by severe secondary hyperparathyroidism requiring
parathyroidectomy. The digital changes had first been noted several
years earlier, while he was undergoing dialysis, and progressed until
he underwent parathyroidectomy. Close examination revealed that the
nail-fold angle, or
Lovibond’s angle,
was well preserved, and a
diagnosis of pseudoclubbing from previous hyperparathyroidism was
made. The changes in this patient’s fingers are the result of soft-tissue
collapse owing to severe bone erosions of the terminal phalanges.
Pseudoclubbing may be distinguished clinically from clubbing by the
preservation of the nail-fold angle and bony erosion of the terminal
phalanges on radiography.
Copyright © 2006 Massachusetts Medical Society.

Nail Exam
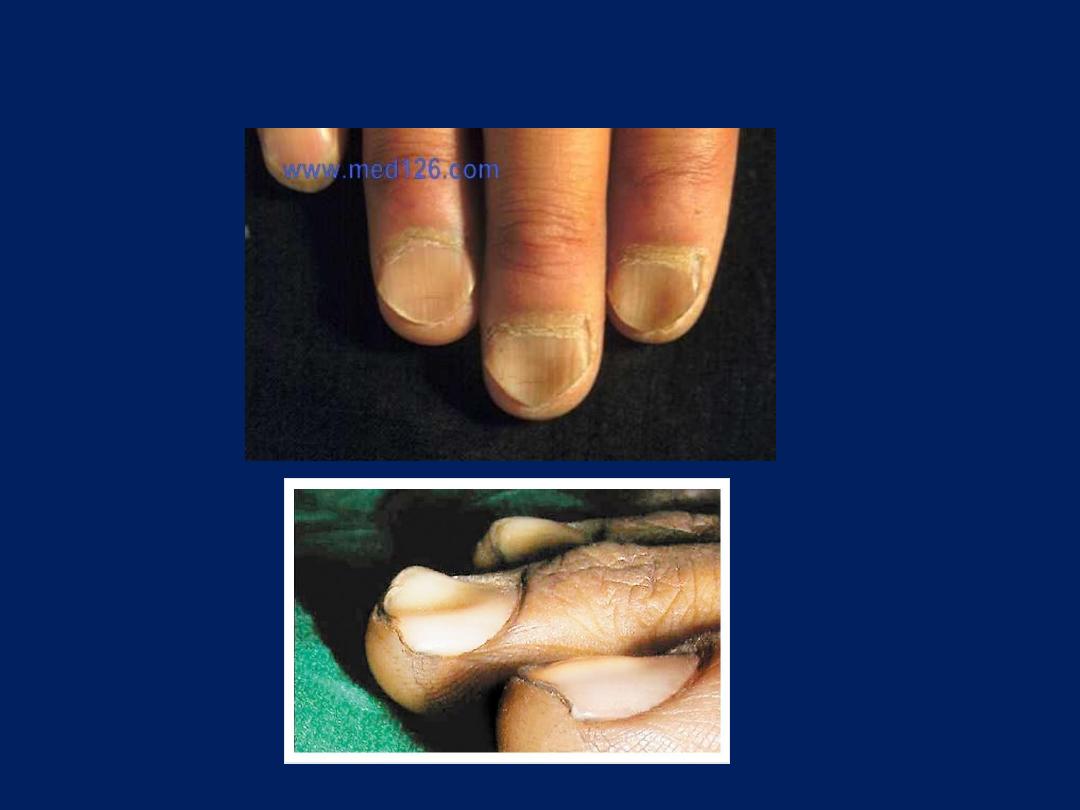
Leukonychia
Nail Exam
Onycholysis
Nail Exam
Koilonychia
Causes of Koilonychia
Iron deficiency anemia
Thyroid dysfunction
Musculoskeletal conditions
SLE
Renal disease
Hemochromatosis
Nail Patella Syndrome
Raynaud’s disease
Contact dermatitis to petroleum-based solvents
Direct trauma
Excessive use of soaps or oils
congenital.
Splinter hemorrhages
are
tiny blood clots that tend to
run vertically under the nails
and can be associated with
trauma,
systemic
vasculitis,
or due to a fragment of
cholesterol
lodged in the
capillaries and seen in
haemato
logical malignancy,
SLE , sclerod
erma,
rheumatoid
arthritis,
subacute
infective
endo
carditis,
trichin
osis and
antiphosph
olipid syndrome.

Hand Exam
Caynosis

Hand Exam
Anemia

Hand Exam
Petechiae

Palmar erythema

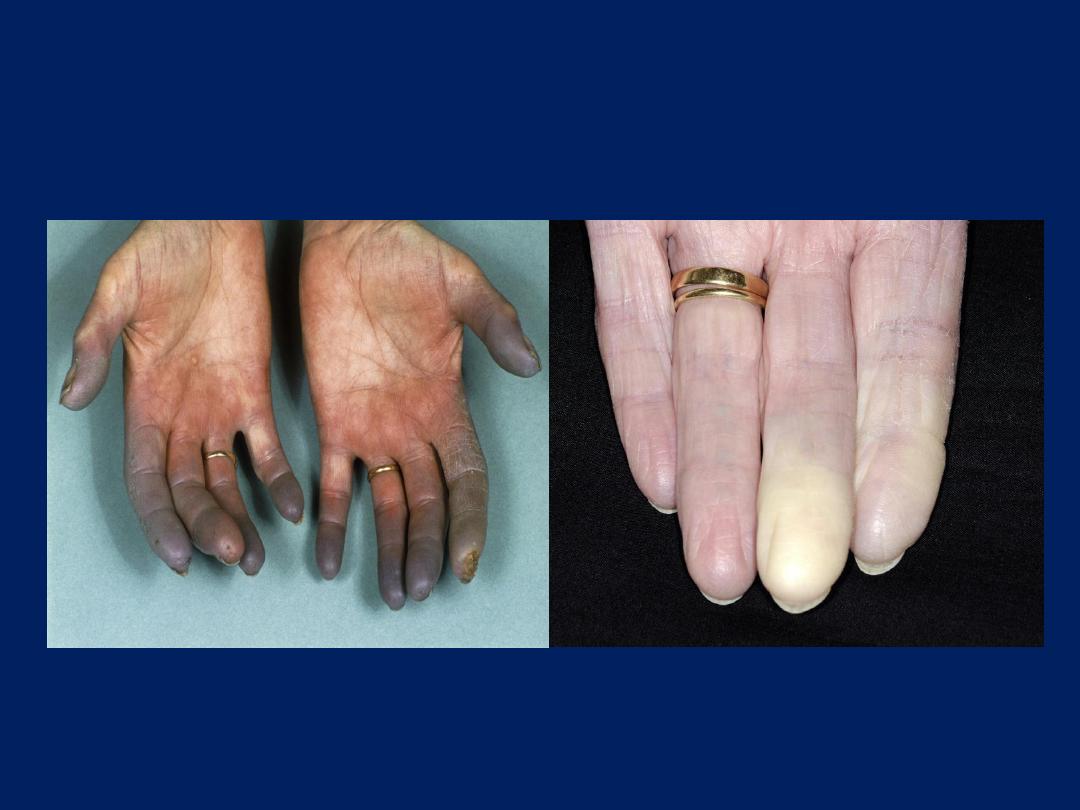
Raynaud's phenomenon
What serologic test is most likely to be positive in this patient?
1. Anticentromere antibody
2. Anti-double stranded DNA
3. Anti- ribonucleoprotein antibody
4. Anti-Ro antibody
5. Anti-Smith antibody

Answer
Anticentromere antibody
Systemic sclerosis is the most frequent
condition associated with
secondary
Raynaud's
phenomenon and is typically
associated with anticentromere antibody.
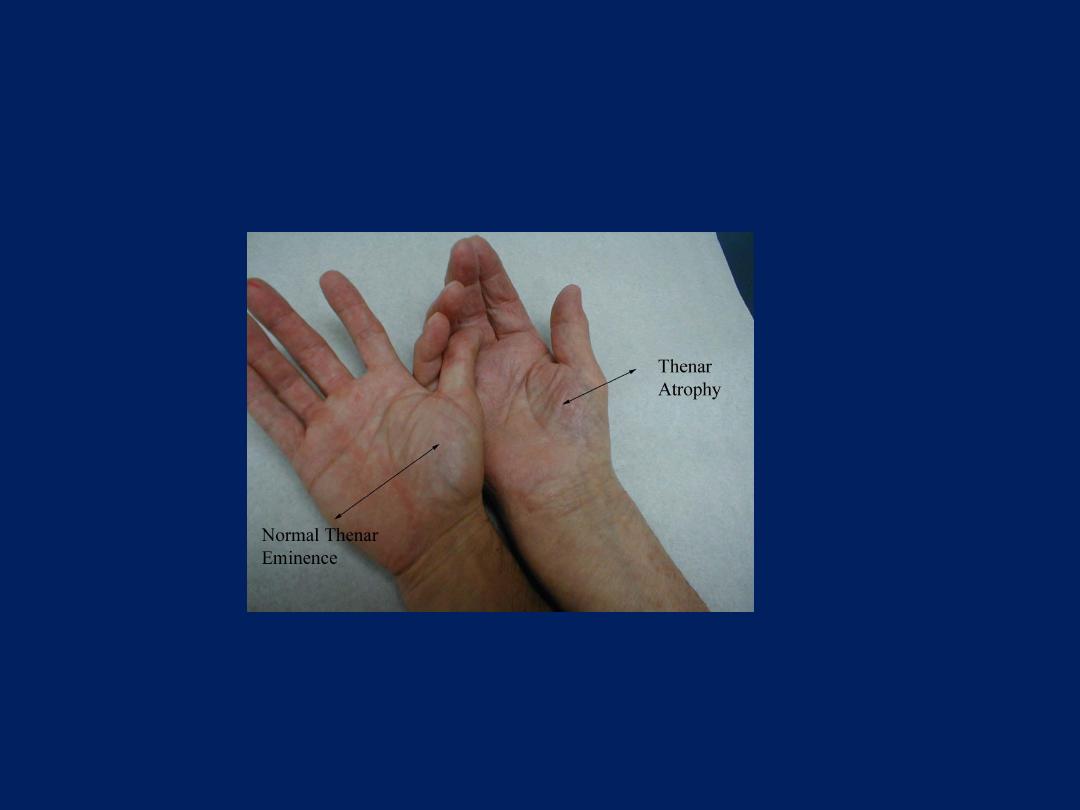
Small Muscle Exam Atrophy

Small Muscle Exam Atrophy
Carpal tunnel syndrome

Small Muscle Exam
Claw hand

Acute lymphangitis
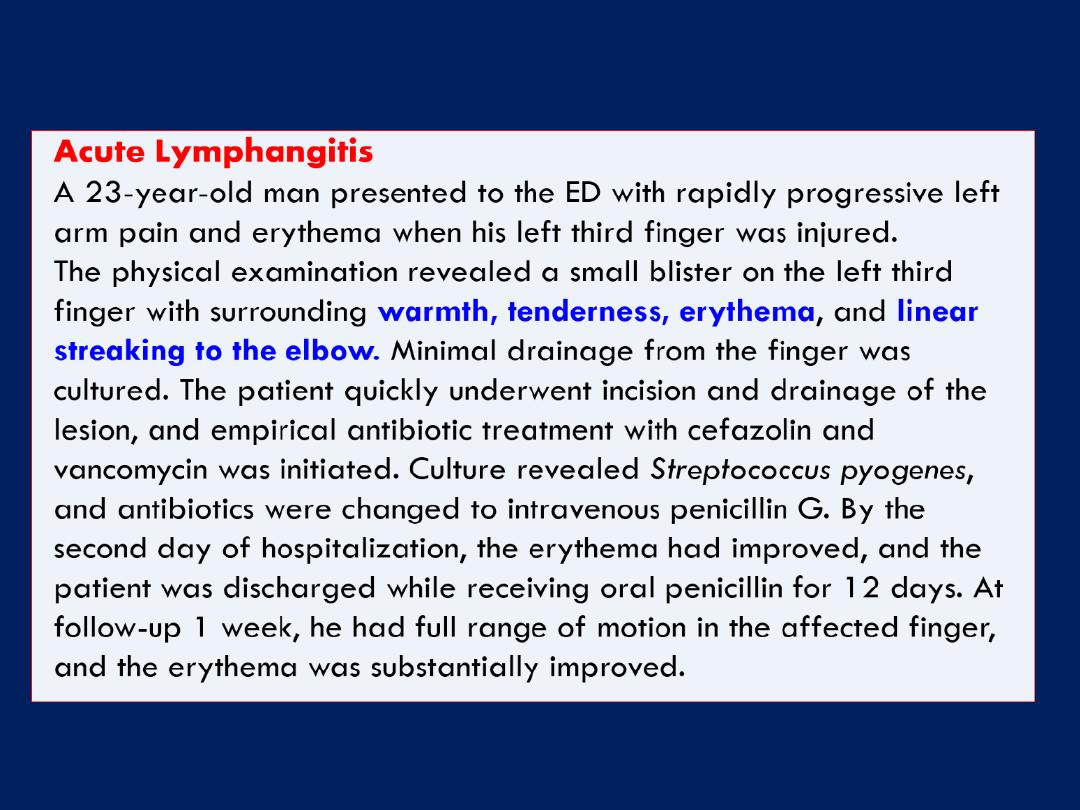

What is the diagnosis?
1. Gout
2. Rheumatoid arthritis
3. Gonococcal arthritis
4. Leprosy
5. Psoriasis
Gout
The image illustrates severe deforming gout.
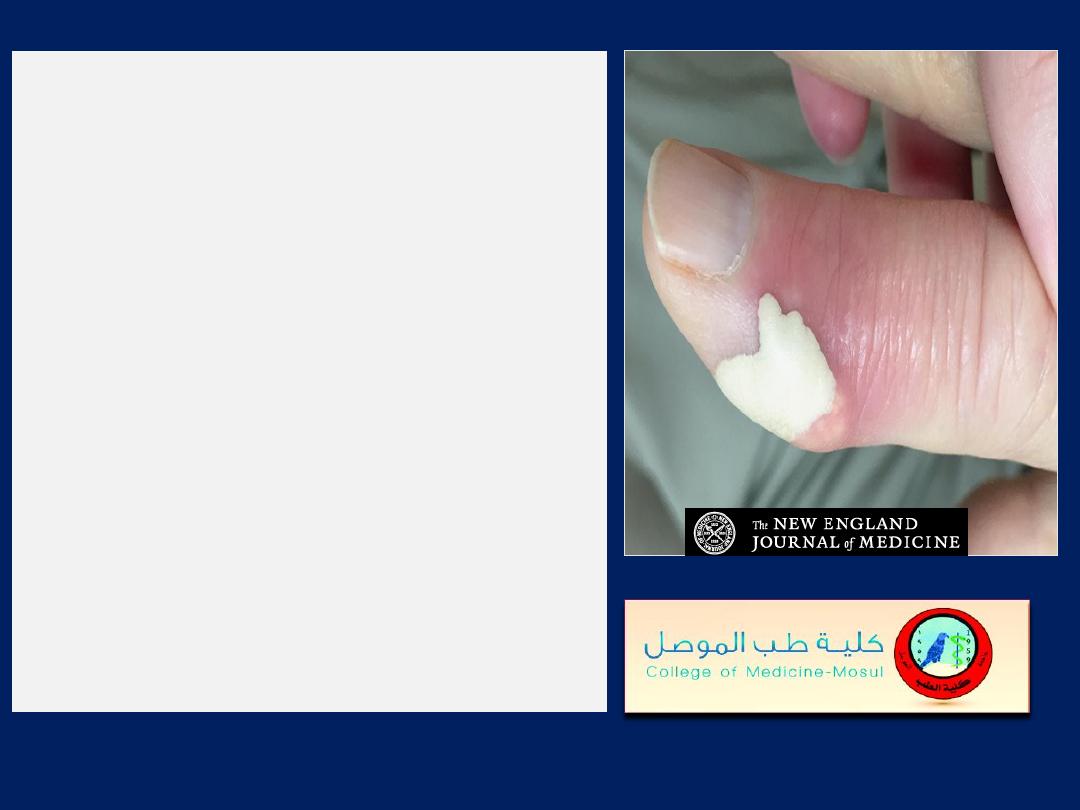
Image Challenge
Q :
In a patient with a history of renal
transplantation, now on
cyclosporine, this finding is most
likely associated with which
underlying diagnosis?
1. Rheumatoid Arthritis
2. Mycobacterial Infection
3. Gout
4. Calciphylaxis
5. Calcium Pyrophosphate
Deposition Disease
Image Challenge
Answer: Gout
The correct answer is gout. This patient had a history of
gout with a pre-existing tophus on his right hand, and
presented with this new blister. Examination of the fluid
aspirated from this blister under polarized light microscopy
revealed sheets of negatively birefringent monosodium
urate crystals. Gout is a common disorder that has an
increased incidence after renal transplantation,
especially in those treated with cyclosporine.
The most common presentations
of gout include acute
gouty arthritis and formation of tophi, though in rare cases
bullae filled with milk of urate can develop.

Henoch–Sch
ِ nlein purpura
20-year-old man was admitted to the hospital with a one-day history
of fever and acute, painful symmetric polyarthritis that involved the
wrists, elbows, and ankles. During the next two days, edema and
palpable purpura developed over the dorsal aspect of the hands and
feet (Panels A and B), as well as on the buttocks and legs. Severe
abdominal pain with hematemesis developed, along with an increase
in liver aminotransferase levels.
Henoch– Sch
ِ nlein purpura
was
suspected.
Computed tomographic scanning of the abdomen revealed edema of
the small intestine, a finding consistent with the presence of intestinal
vasculitis. Examination of a biopsy specimen of a skin lesion revealed
leukocytoclastic vasculitis without IgA deposition.
The serum IgA level was normal. The serum creatinine level and the
results of urinalysis were also normal. Blood cultures were sterile, and
multiple immunologic studies were negative. The patient remained
febrile for approximately five days without further progression of his
skin lesions. His condition improved with supportive care, and he was
doing well at follow-up two months after the onset of his illness.

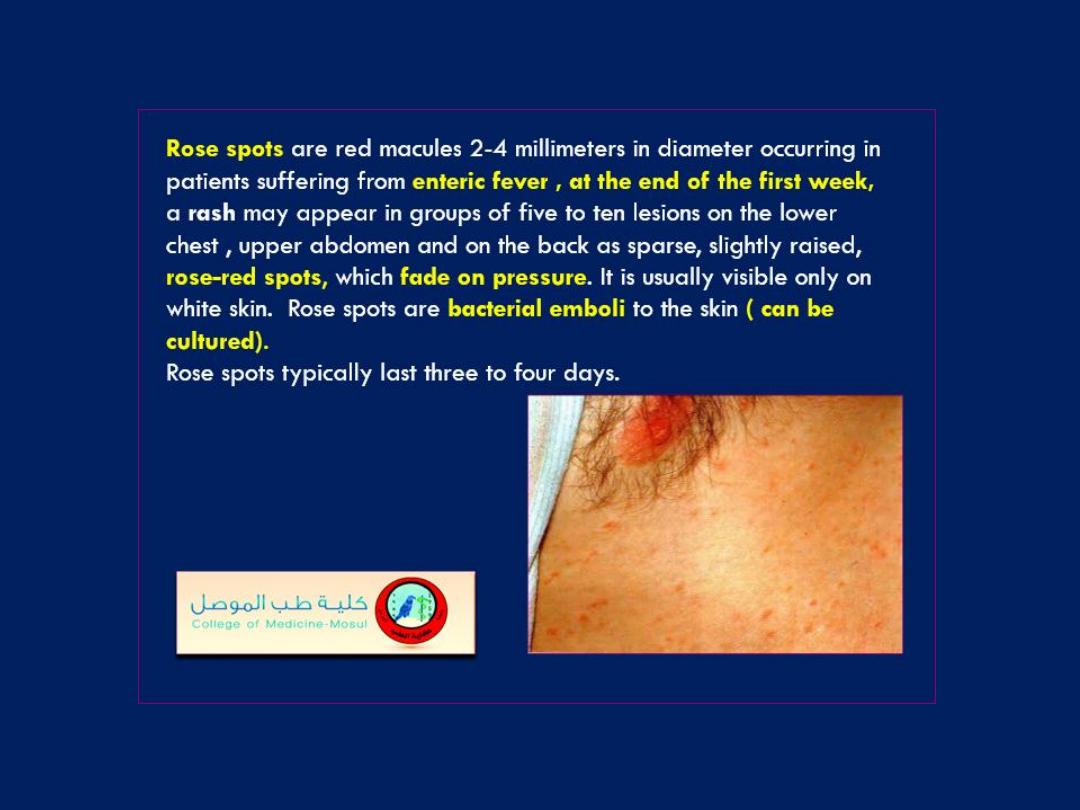
Skin lesion
Purpura

Skin lesion
Ecchymosis

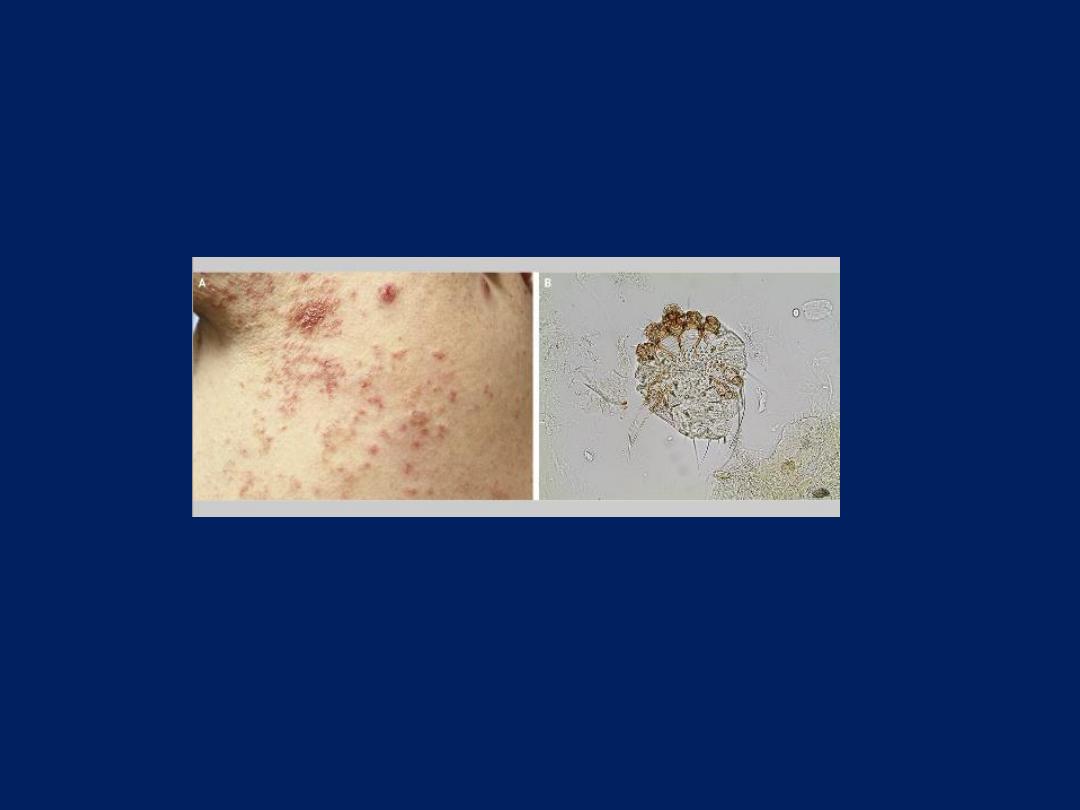
Scabies
N Engl J Med 2016
A 61-year-old woman presented with severe pruritic rash, which had been
present for 6 months. Excoriated papules with honey-colored crusting were
present on the abdomen, back (Panel A), arms, and legs. Treatment with
fluocinonide cream and doxycycline for suppurative folliculitis and prurigo
nodularis for a period of 4 weeks produced no resolution of the rash. A
biopsy of the rash revealed mixed inflammatory infiltrate with eosinophils,
which was suggestive of a drug-related rash. Discontinuation of all
medications resulted in no change. Finally, skin scrapings from several web
spaces on the hands
(scabies preparation)
showed a mite under light
microscopy (Panel B). Topical permethrin cream that was applied overnight to
the entire body and repeated in 1 week cleared the rash within 2 weeks
after the first application. Scabies is a mite-borne disease characterized by
pruritus that is classically worse at night. Untreated disease can be associated
with extensive eczematization of the skin owing to constant scratching.
Secondary infections such as impetigo, ecthyma, paronychia, or furunculosis
can also occur. Clinically, burrows are difficult to visualize and may be
disguised by excoriations and impetigo. Biopsy specimens often show
nonspecific changes without burrows or mites, since patients may have only 6
to 10 mites on their entire cutaneous surface.

Skin lesion
Spider nevi

Decreased fluid intake
Dehydration
Diarrhea
Diabetes
Extreme weight loss
Heat stroke
Vomiting
Skin lesion
Reduced skin turgor
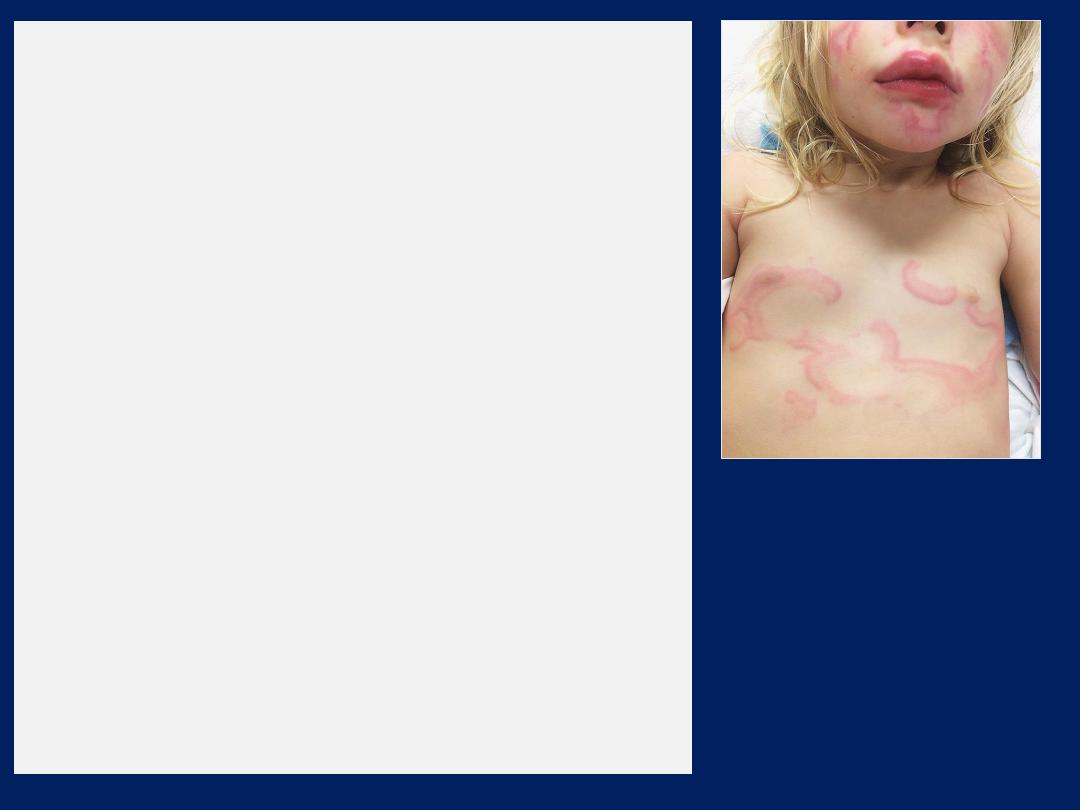
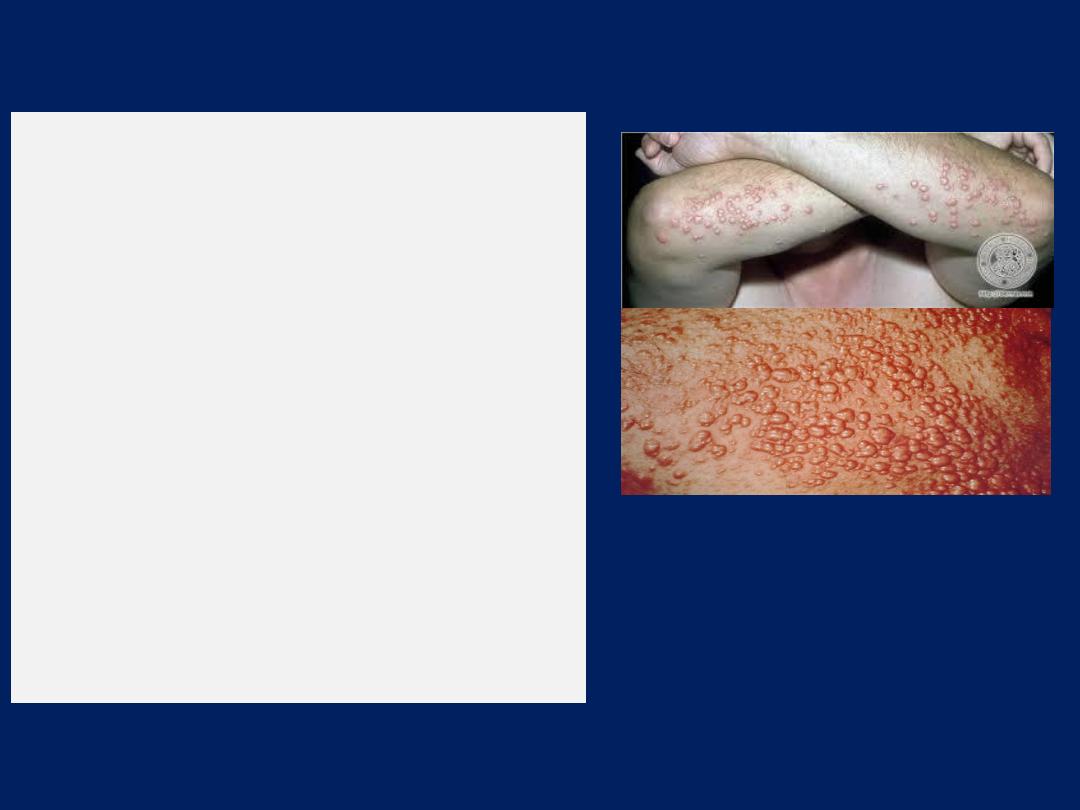
Urticaria multiforme
This patient had a recent viral respiratory
illness and no history of exposure to new
medications or allergens. One week after her
illness, she developed fever, along with a
generalized polycyclic annular rash with
wheals and ecchymotic centers; she then
developed acral edema and the blanching
arcuate urticarial rash seen here. On
examination she was found to have
dermatographism, characterized by the onset
of welts and hives at the site of pressure or
scratching. These clinical features together
are most consistent with a diagnosis of
urticaria multiforme. The patient was treated
with diphenhydramine and the lesions
resolved with no further sequelae.

Varicella
This polymorphic rash
with vesicles, pustules,
and crusty lesions is
most consistent with
varicella infection.
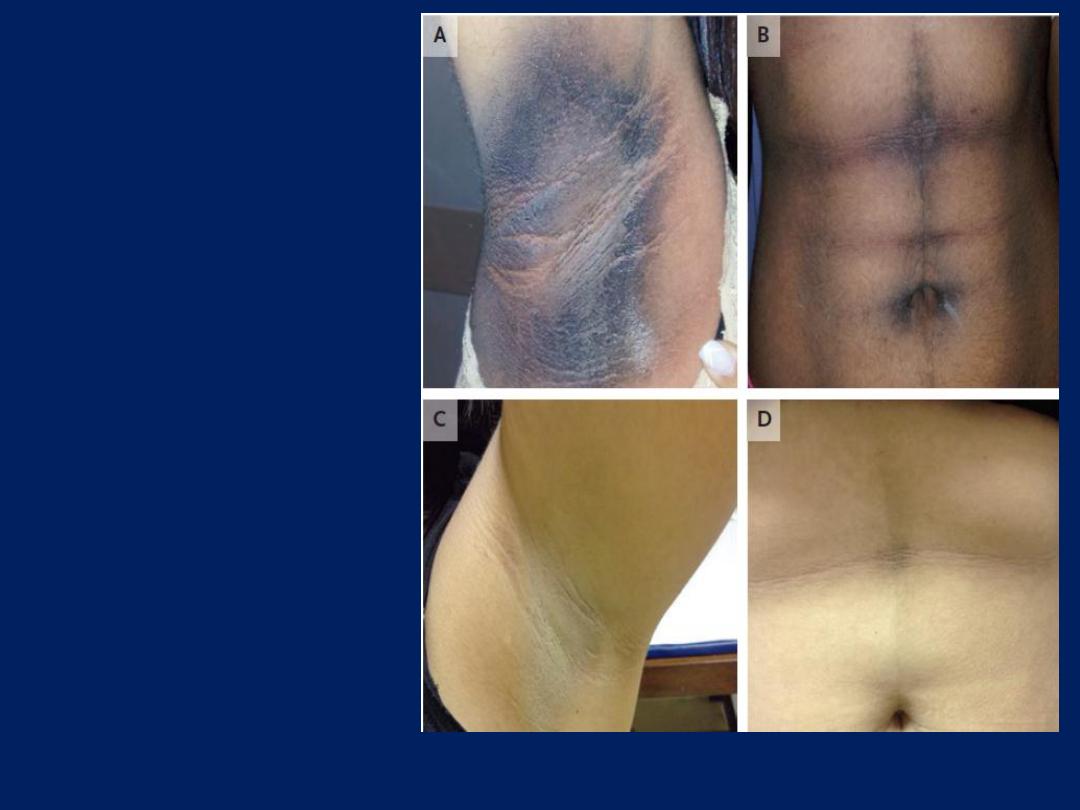
Acanthosis
Nigricans and
Insulin Resistance
NEJM 2016
27-year-old woman presented
with a 2-year history of acanthosis
nigricans (Panels A and B), hirsutism, and amenorrhea. Laboratory
tests revealed elevated levels of insulin
(>200 μU per milliliter) (normal range, 2
to 13
μU per milliliter)
and testosterone
(649 ng per deciliter) (normal range, 9 to 63
ng per deciliter)
, the presence of thyroperoxidase antibodies, and an
antinuclear antibody titer of 1:64
(normal titer, <1:32).
Blood glucose and
glycated hemoglobin levels were normal, and screening for cancer
was negative. On follow-up at 6 months, the patient had weight loss
and hyperglycemia (fasting glucose level, 174 mg per deciliter , and
glycated hemoglobin level, 11.2%) . C-peptide levels were elevated
at
7.3 ng per milliliter (normal range, 1.1 to 5.0),
but tests for anti–glutamic acid
decarboxylase, anti–tyrosine phosphatase-related insulinoma-
associated–2 (IA-2), and anti-insulin antibodies were negative.
NEJM 2016
The administration of metformin was initiated, and 6 months later
hypoglycemic episodes developed. Titers of anti-insulin–receptor
antibodies were elevated (1:1280), and
type B insulin resistance
syndrome was diagnosed.
Treatment with prednisone and azathioprine was initiated, and
after 6 weeks there was normalization of blood glucose,
testosterone, and insulin levels and clinical improvement of
acanthosis nigricans (Panels C and D).
Acanthosis nigricans
can be caused by endocrine, metabolic,
genetic, and paraneoplastic conditions.
Type B insulin resistance syndrome
is an autoimmune disorder
characterized by the production of antibodies against the insulin
receptor, which leads to disorders in glucose metabolism (from
hyperglycemia to hypoglycemia), extreme insulin resistance,
acanthosis nigricans, and hyperandrogenism.
NEJM 2016
What is the diagnosis?
1. Carpal tunnel syndrome
2. Rheumatoid Arthritis
3. Scleroderma
4. Diabetic peripheral
neuropathy
5. Dupuyten's contracture
Dupuytren's contracture
The pictured flexion contractures involving bilateral third digits and
the right fifth digit are most consistent with Dupuytren's contracture.
Dupuytren's contracture
is a fixed flexion contracture of the hand
due to a palmar fibromatosis, where the fingers bend towards the
palm and cannot be fully extended .It is an inherited proliferative
connective tissue disorder that involves the hand's palmar fascia. It is
named after Baron Guillaume Dupuytren, the surgeon who described
an operation to correct the affliction in the Lancet in 1831.The ring
finger and little finger are the fingers most commonly affected. The
middle finger may be affected in advanced cases, but the index
finger and the thumb are not affected as frequently. Suspected, but
unproven, causes of Dupuytren's contracture include
trauma
(manual
labor or over-exertion of the hands), ,
diabetes, epilepsy
and
therapy with
phenytoin.
Smoking,
alcohol,
diabetes , seizures, make dupuytren's contracture.
more likely to develop. There seems to be a genetic factor as it has a
tendency to run in some
families
Carpopedal spasm
35-year-old man presented with a 2-day history of cramps and paresthesias
in the arms, predominantly involving the fingers. This presentation
was preceded by a bout of viral gastroenteritis 1 week earlier. The patient
reported receiving no medications and specifically reported not using thiazide
diuretics. He had a blood pressure of 100/60 mm Hg, a respiratory rate of 24
breaths per minute, and carpopedal spasm, which was reproducible by inflating a
blood-pressure cuff placed on the patient’s arm. Chvostek’s sign, twitching of the
circumoral muscles with tapping lightly over the facial nerve. Laboratory
investigation revealed a serum calcium level of 1.9 mmol per liter (7.6 mg per
deciliter) (normal range, 2.2 to 2.6 [9.0 to 10.5]), a potassium level of 2.8 mmol per
liter (10.9 mg per deciliter) (normal range, 3.5 to 5.0 [13.7 to 19.5]), and a
magnesium level of 0.5 mmol per liter (normal range, 0.8 to 1.2). Analysis of
arterial blood gas showed a pH of 7.53, a bicarbonate level of 34 mmol per liter,
and a partial pressure of carbon dioxide of 30 mm Hg. A diagnosis of
hypocalcemia
was made, and the patient was treated with calcium gluconate.
Urinary calcium excretion was subnormal, with increased urinary loss of potassium,
magnesium, and chloride, which supported the diagnosis of Gitelman’s syndrome, an
inherited renal salt-wasting disorder. The patient had a good response to therapy
with oral magnesium and potassium supplements.
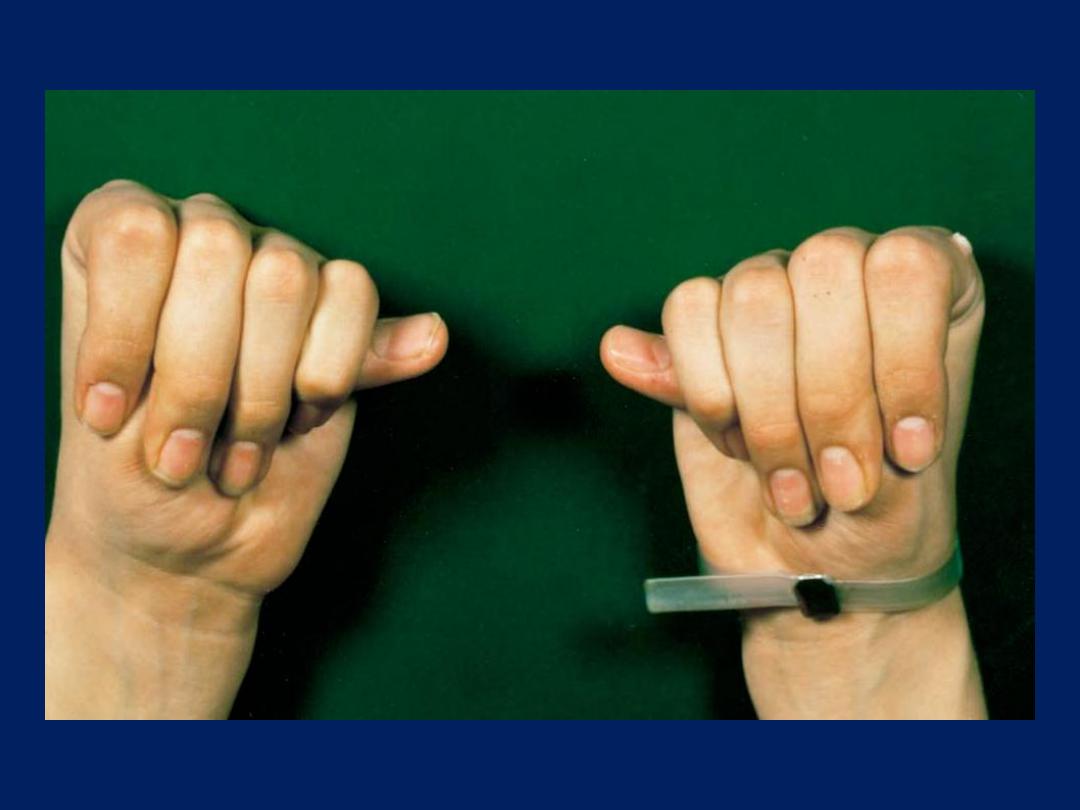
The “Thumb Sign” in Marfan’s Syndrome
The thumbs protrude from the clenched fists of a 24-
year-old man who presented with congestive heart
failure due to severe chronic aortic regurgitation and
left ventricular dysfunction.
Arachnodactyly (“spider finger”) and loose joints
account for the ability to position the fingers in this
way.
The patient also had other skeletal features of
Marfan’s syndrome, including pets excavatum and a
higharched palate.
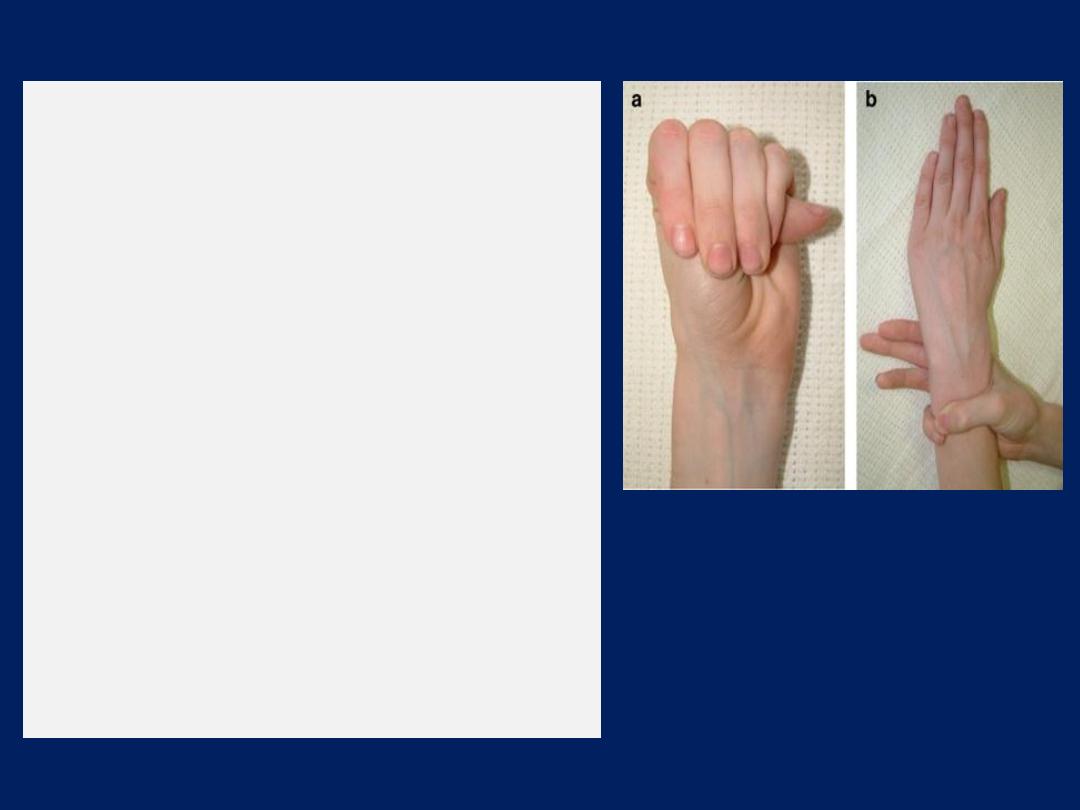
THE STEINBERG SIGN (a):
Instruct the patient to fold his thumb
into the closed fist. This test is
positive if the thumb tip extends
from palm of hand (see figure a).
THE WALKER-MURDOCH SIGN (b):
This test is used for the evaluation of
patients with Marfan syndrome.
Procedure:
Instruct the patient to grip his wrist
with his opposite hand. If thumb and
fifth finger of the hand overlap with
each other, this represents a positive
Walker-Murdoch sign (see figure b).
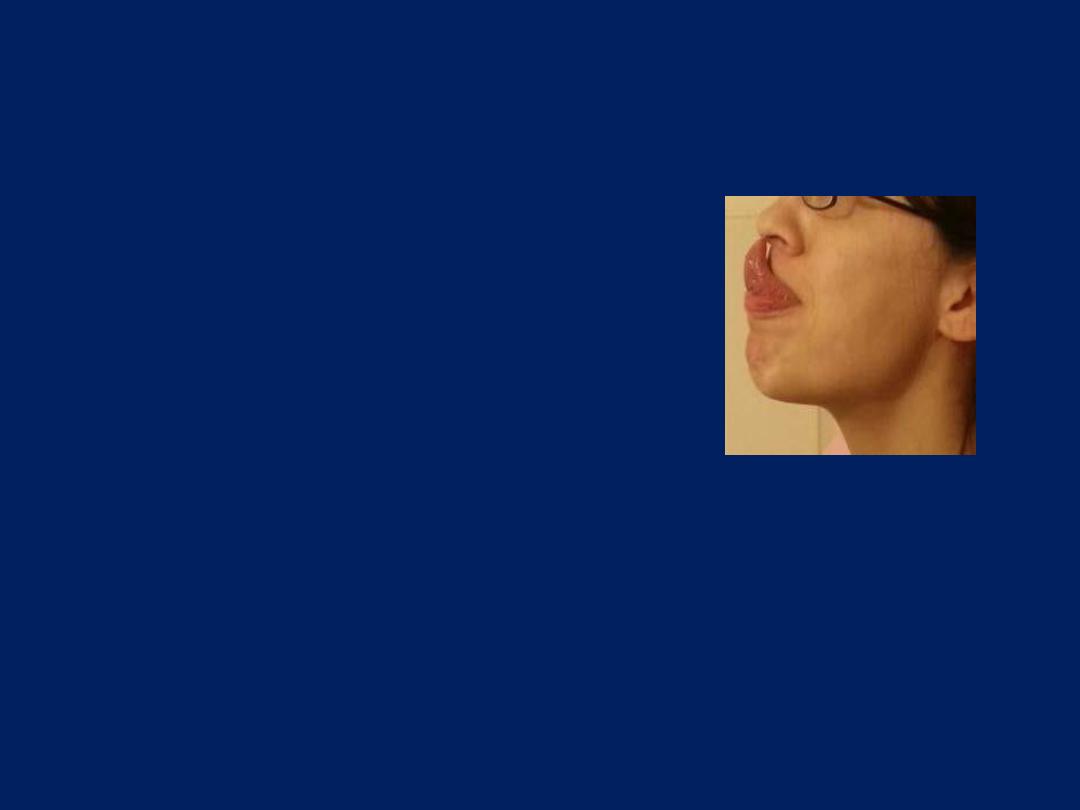
Gorlin’s sign
(the ability to touch
the nose with the tip of the tongue)
is seen in
half of
patients with
Ehlers- Danlos
syndrome and
systemic hypermobility.
Only
8-10%
of the
“normal”
population can perform this
manoeuvre.
Eruptive xanthomas in a
patient with diabetes and
poor glycemic control.
Eruptive Xanthomas
painless, yellowish papules on
an erythematous base that
present as grouped lesions on
the torso, especially the elbows
,chest, and buttock regions.
Triglyceride levels are very
high, often exceeding 2,000
mg/ dL. They may appear in a
patient with diabetes who has
poor glycemic control.
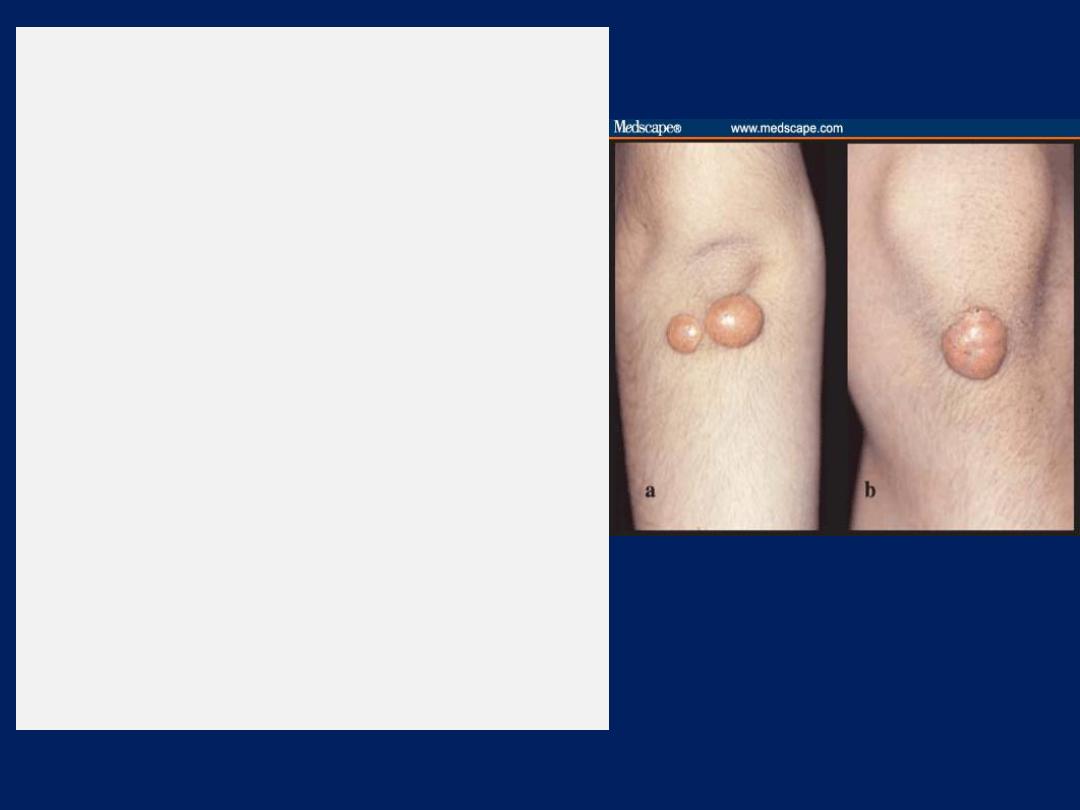
Tuberous and Tuberoeruptive
Xanthomas
firm and nontender cutaneous and
subcutaneous nodules that may be
confused with gouty tophi. They occur
on extensor surfaces of the large
joints or hand ,knees, buttocks, and
elbow ,heels . as well as in areas of
prior trauma. pressure areas
Tuberous xanthomas are circular,
raised lesions that display a
yellowish-orange hue,associated with
hypertriglyceridemia, but they are
also seen in patients with
hypercholesterolemia .
Examples of tuberous xanthomas
on the (a) back of the elbow and (b)
front of the knee.

Tendinous xanthoma
characterized by papules and nodules ,associated with
Type II hyperlipidaemia . Most commonly found in the
tendons of the hands, feet, and Achilles tendon

Edema Exam

Pallor
Cyanosis
Ulcerations
Gangrene
Loss of pulses
Hairless shiny skin
Ischemia Exam

Diabetic foot

Erythema multiforme
Erythema multiforme
It means a redness (erythema) that is of many (multi-)
shapes . The rash can be recognised by the presence of
spots that look like small
targets
(
bull’s eye shaped ‘target
lesions’).
These have a dusky red centre, a paler area
around this, and then a dark red ring round the edge. It is
usually
mild
(erythema multiforme minor)
– with only a
few spots, causing little trouble and clearing up quickly –
but there is also a
rare severe
type
(erythema multiforme
major/bullous erythema multiforme)
that can be life
threatening with involvement of the mucus membranes of
the mouth, in the genital area, and on the conjunctiva of the
eyes occurs most commonly between the ages of 10 - 40.


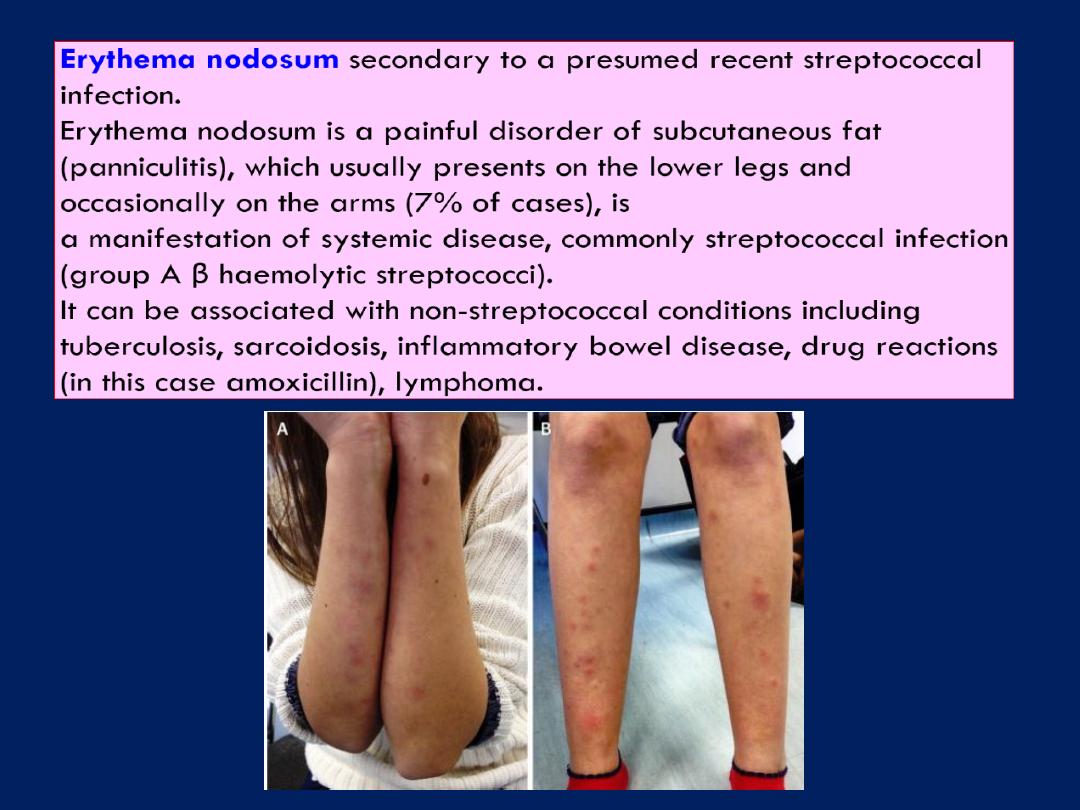
What is the diagnosis?
1. Erythema induratum
2. Erythema nodosum
3. Granuloma annulare
4. Necrobiosis lipoidica
5. Pretibial myxedema
Necrobiosis lipoidica
Necrobiosis lipoidica is a chronic granulomatous dermatitis of unknown cause that is
most often associated with diabetes mellitus. However, in about 25% of patients
with this condition, lesions develop before the onset of diabetes. The lesions appear
as yellow-brown, telangiectatic plaques with central atrophy and raised violaceous
borders. They occur most frequently on the shins or the dorsa of the feet. Ulcers,
which exist in about 30% of lesions, are often induced by trauma.

Erythema ab igne
healthy 69-year-old man with osteoarthritis of the knees presented
with a 2-week history of mottled darkening of the skin on the left
thigh. On examination, there was a reticular, reddish-brown, pruritic,
nontender,macular, nonblanching discoloration around the medial
aspect of his left knee,with a few superficial erosions. He had no fever,
chills, or other constitutional symptoms.For several weeks before this
event, the patient had applied a heating pad repeatedly to his left
knee to relieve the discomfort from the osteoarthritis. The
reticular,hyperpigmented erythema is a typical presentation of
erythema ab igne,
a phenomenon caused by chronic exposure to heat
or infrared radiation. The few superficial erosions were thought to be
due to a mild burn. Erythema ab igne is reported most frequently in
temperate countries where people use a variety of heat sources during
the cold weather. In physical medicine and rehabilitation, erythema ab
igne develops in some patients after they have received heat therapy
for pain and inflammation.
This patient stopped using the heating pad, and the discoloration
gradually lightened over several months without any other treatment.

lipedema
There are several features about lipedema that
distinguish it from lymphedema
One of the most notable differences is the fact that
the feet are generally not involved in lipedema. The
excess accumulation of subcutaneous fat can involve the
entire leg but will generally stop at the ankle, leaving
a characteristic ring at the base of the ankle where
the lipedema stops.
Another difference is the fact that the excess fat is
generally symmetric so that both legs are involved
equally. In many patients, only the lower extremities
and the buttocks are involved, with no excess
accumulation of fat in the arms, chest or abdomen.


Erysipelas
is a superficial
cellulitis characterized by
shiny, raised, indurated, and
tender plaque-like lesions
with distinct margins. It is
almost always caused by
group A β-hemolytic
streptococci.
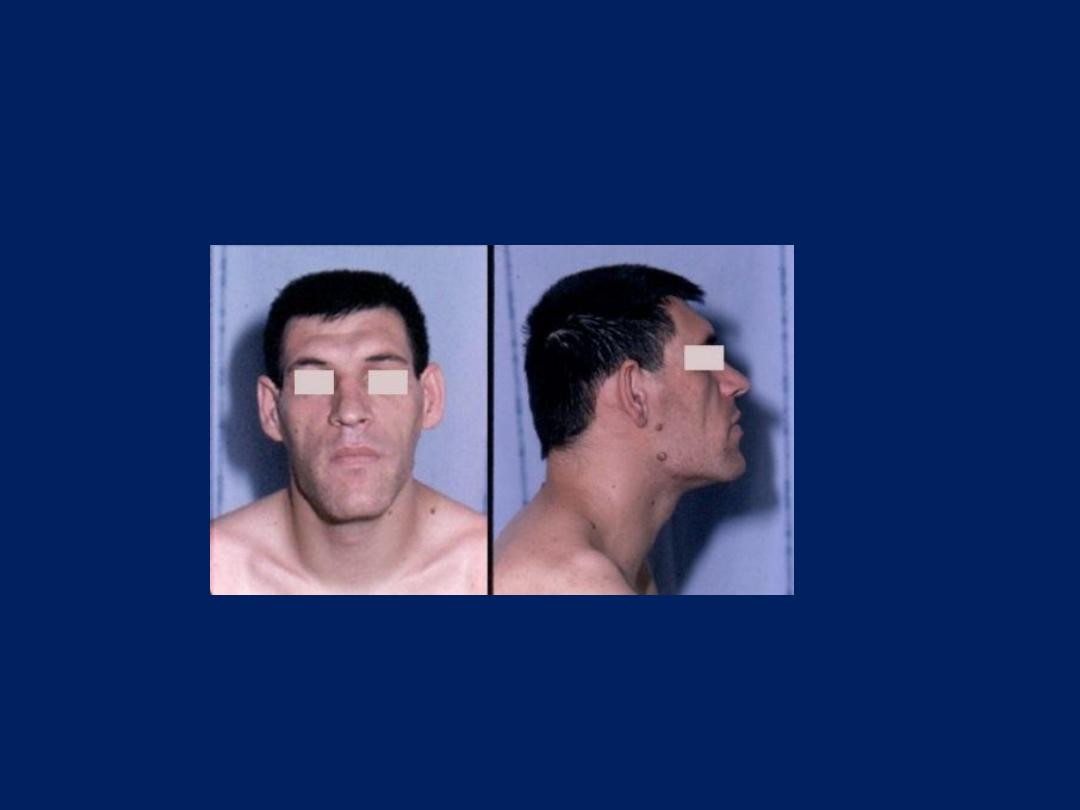
Special facies
Acromegaly
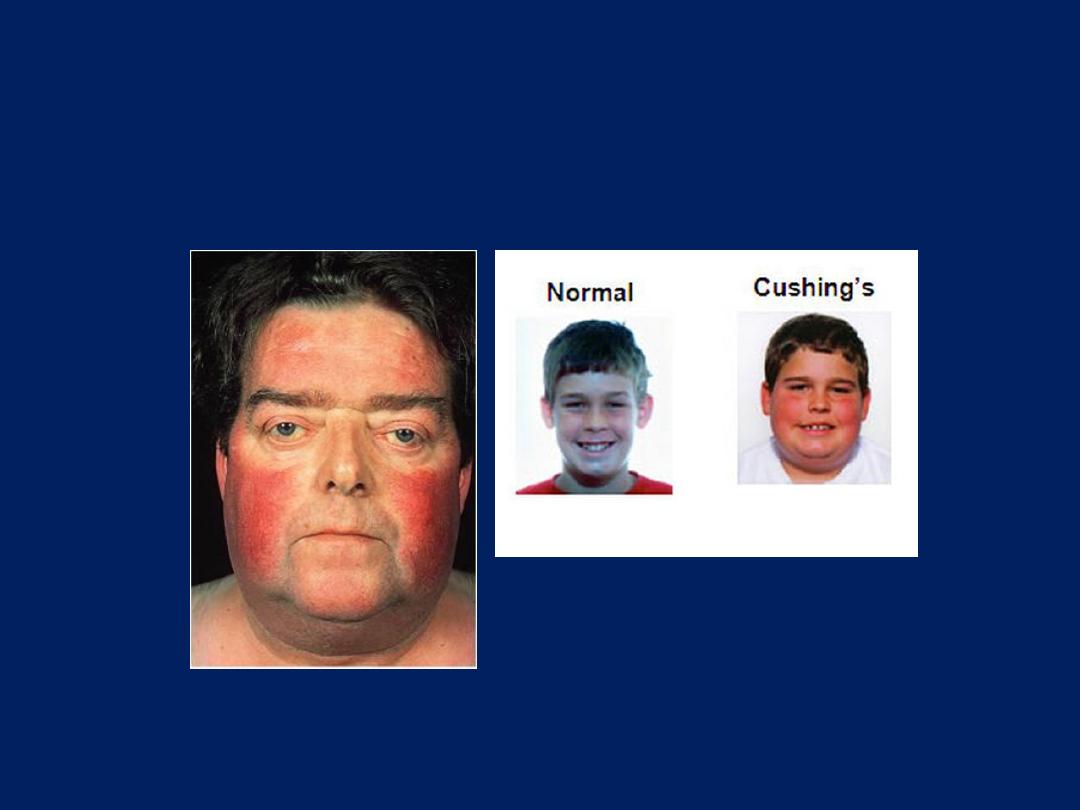
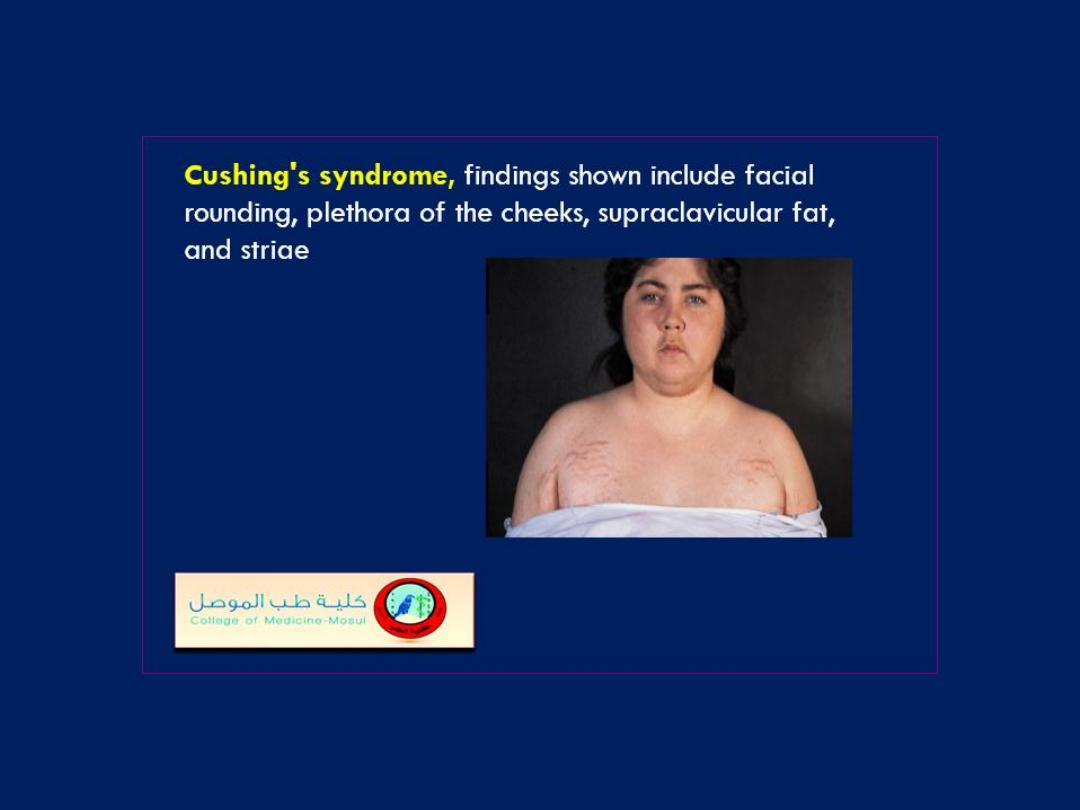
Special facies
Cushing
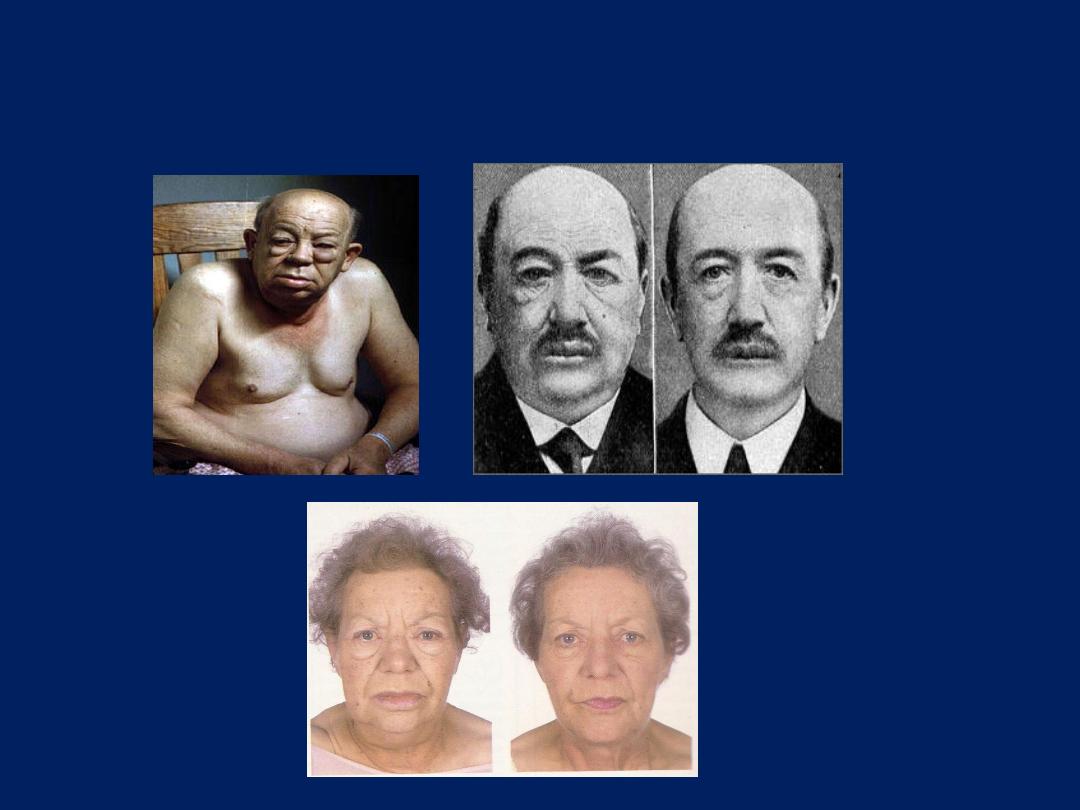
Special facies
Myxedema

Pretibial myxedema
results from the
accumulation in the dermis of
glycosaminoglycans , especially
hyaluronic acid, secreted by fibroblasts
under the stimulation of cytokines. The
cytokines arise from the lymphocytic
infiltration. The resulting characteristic
pathologic changes are mucinous edema
and the fragmentation of collagen fibers.
Clinically, one sees
nonpitting edema
of
the dermis, due both to the hydrophilic
nature of these substances and
compression of dermal lymphatics and
fragmentation of dermal collagen fibers.
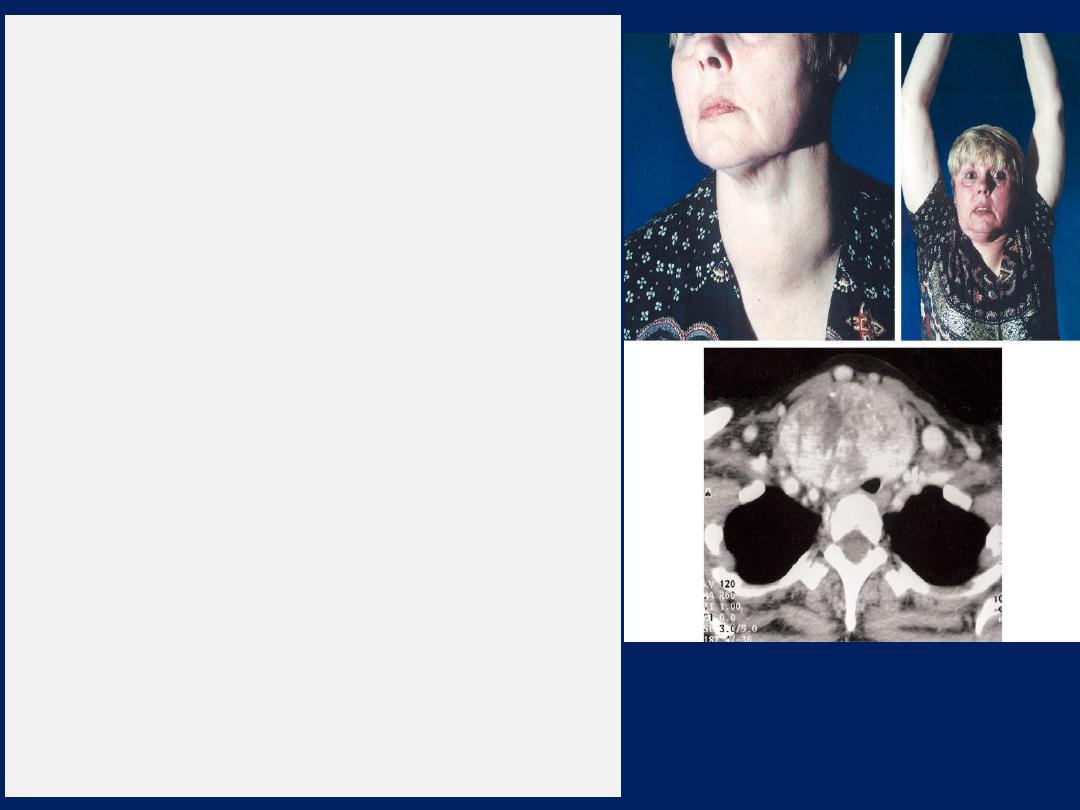
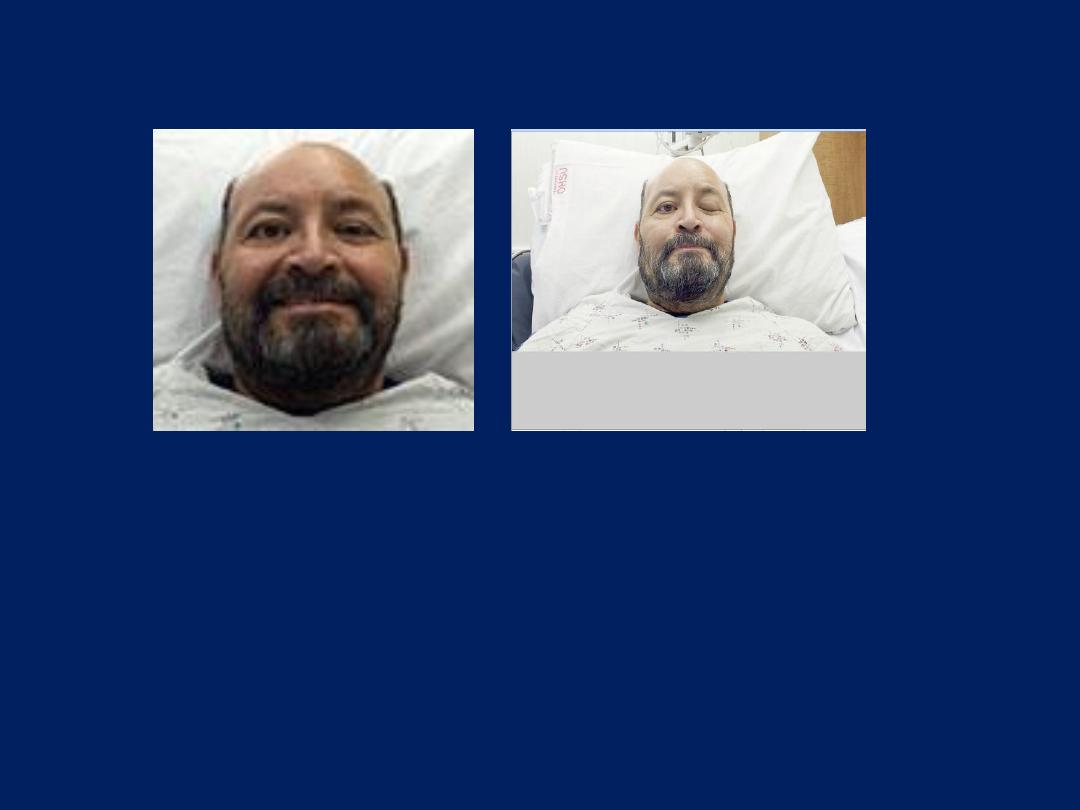
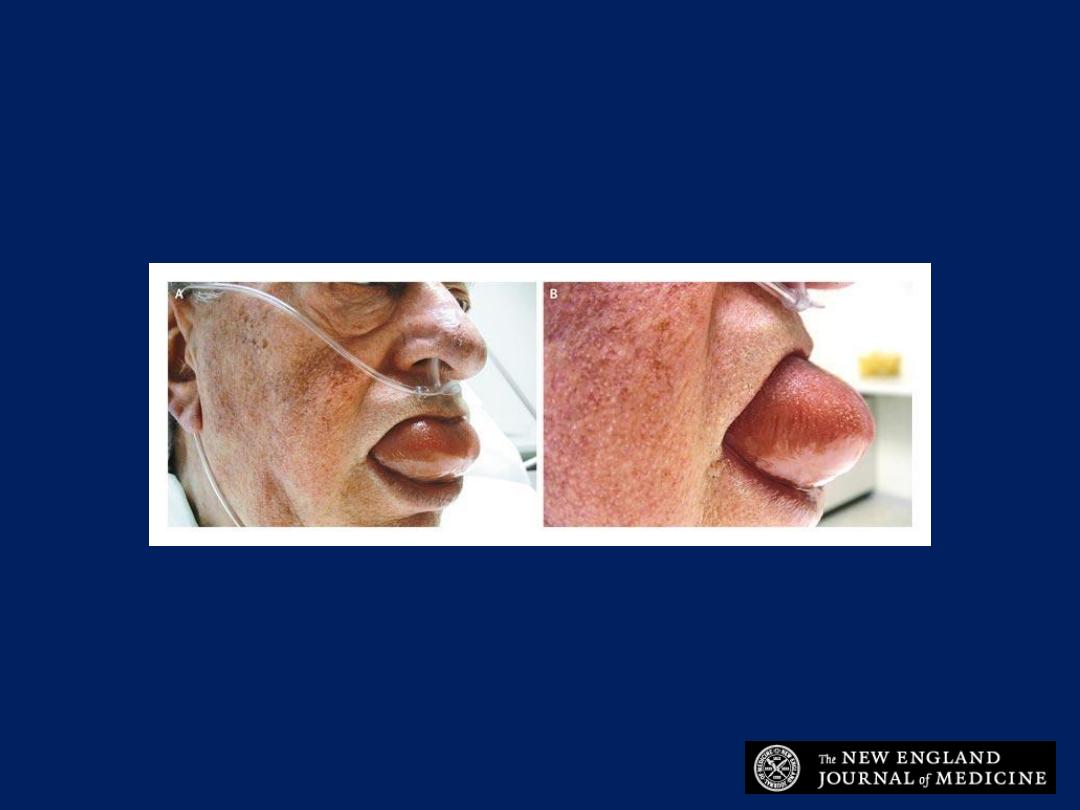
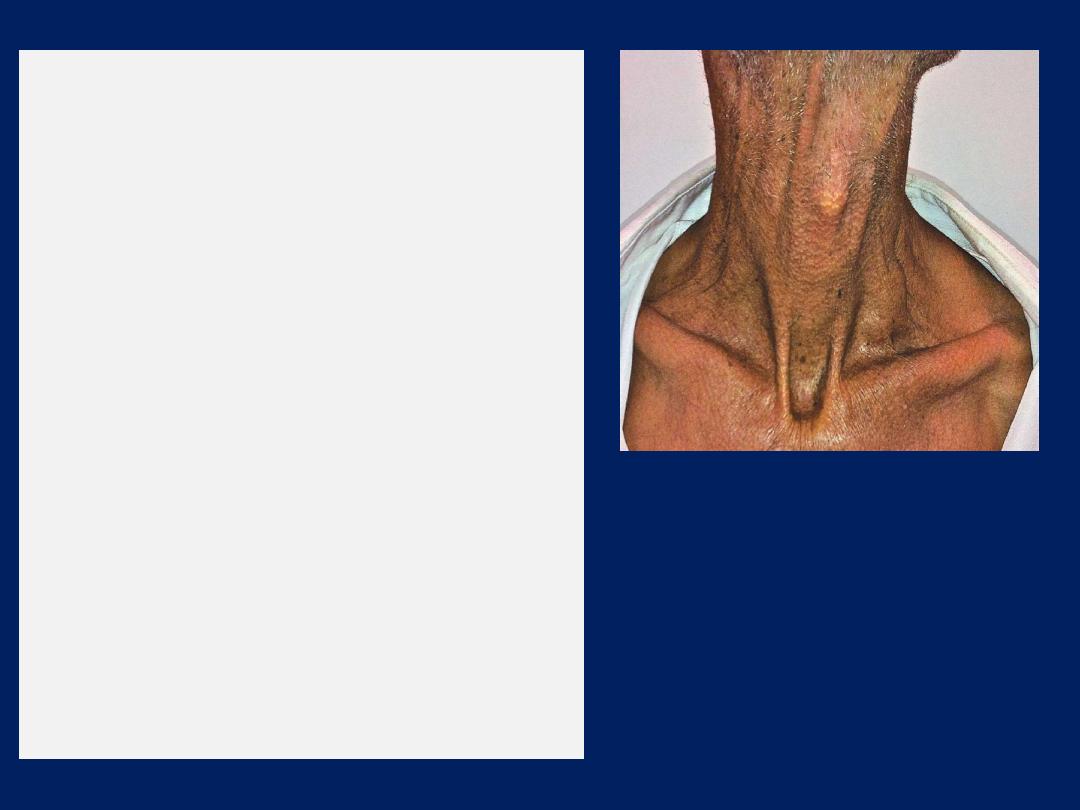
Pemberton's sign
A 58-year-old woman with a 20-
year history of goiter presented with a two-month
history of progressive dyspnea on exertion,
occasional stridor, and a choking sensation while
supine. She had previously been asymptomatic.
Physical examination revealed a diffusely enlarged
thyroid with no palpable nodules (Panel A), but the
lower poles of the thyroid were not palpable. Within
30 seconds after she raised both arms
simultaneously (Pemberton's maneuver), marked
facial plethora (Pemberton's sign)
developed,
indicating compression of the jugular veins (Panel B).
The patient's serum thyrotropin and free thyroxine
concentrations were normal. Computed tomography
of the neck revealed a large goiter extending into the
anterior superior mediastinum and causing compression
and deviation of the trachea (Panel C). The patient
underwent thyroidectomy, and her symptoms resolved.
Pathological examination revealed a multinodular
goiter. Pemberton's sign is observed when the
thoracic inlet rises so that it becomes filled (“plugged”)
by a large goiter that extends retrosternally. This
phenomenon is also known as
“thyroid cork.”
A
B
C
Pemberton's sign
was named after Dr. Hugh Pemberton, who
characterized it in 1946. The Pemberton maneuver is a physical
examination tool used to
demonstrate the presence of latent
pressure in the thoracic inlet.
The maneuver is achieved by
having the patient elevate both arms until they touch the sides
of the face. A positive Pemberton's sign is marked by the
presence of facial congestion and cyanosis, as well as respiratory
distress after approximately one minute. A positive Pemberton's
sign is indicative of superior vena cava syndrome
(SVC),
commonly the result of a mass in the mediastinum.
Although the
sign is most commonly described in
patients with substernal
goiters where the goiter “corks off” the thoracic inlet, the
maneuver is potentially useful in any patient
with adenopathy,
tumor, or fibrosis involving the mediastinum

Thyroid Exam (goiter)
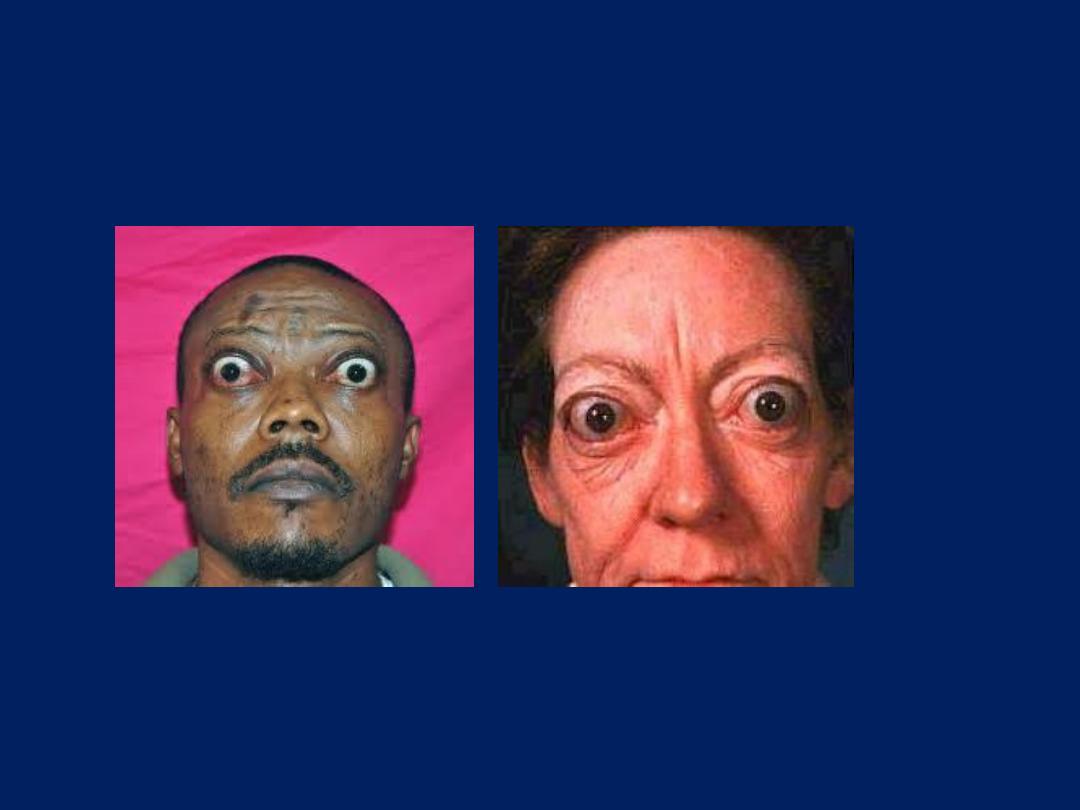
Special facies :Throtoxicosis
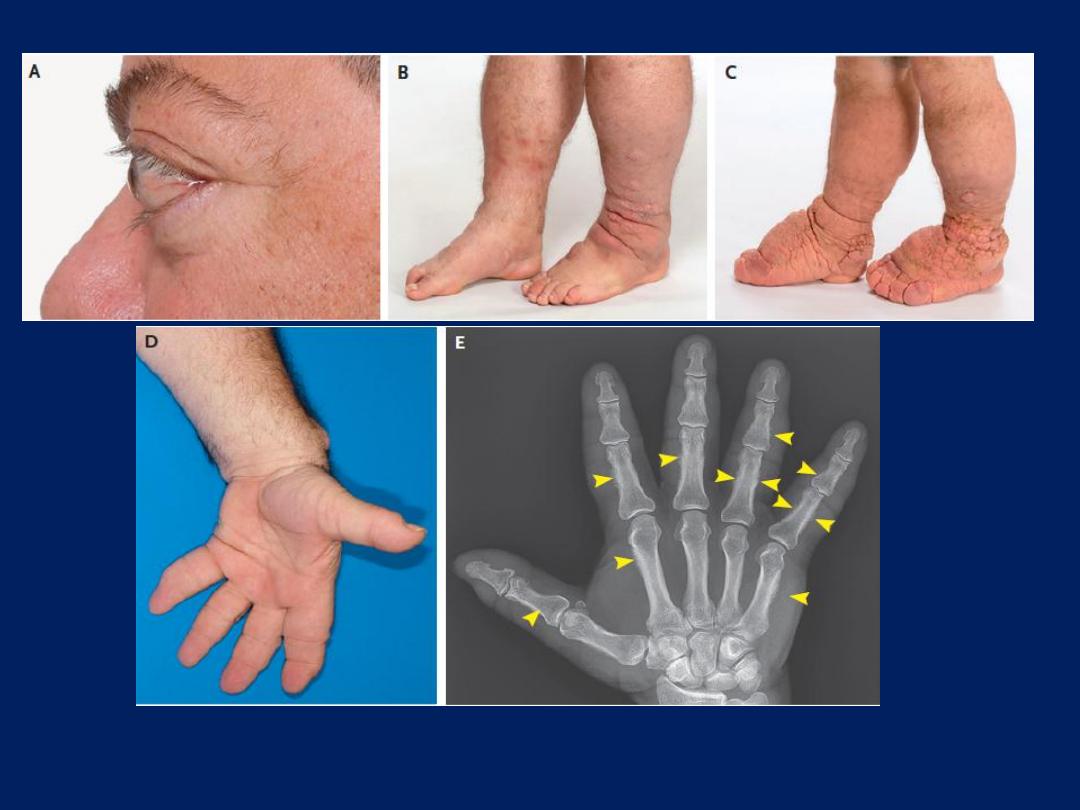
Nejm.org July 21, 2016
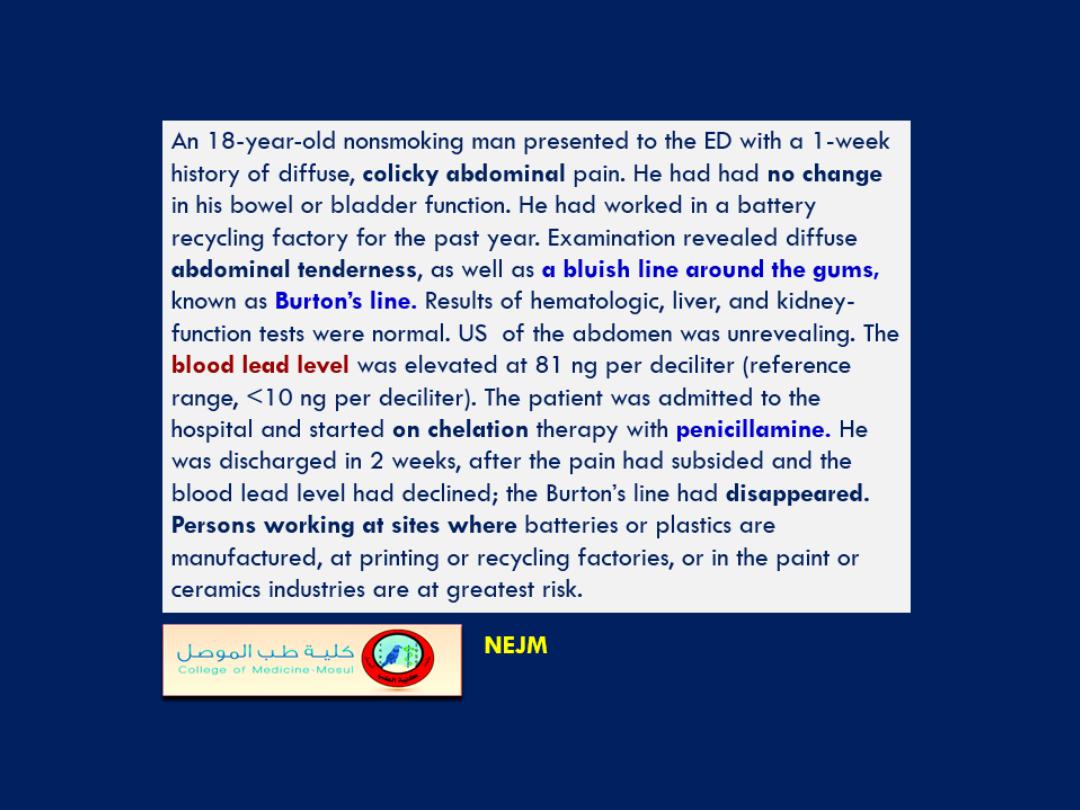
A 56-year-old man was referred to a dermatologist for assessment of the
progression of his
thyroid dermopathy.
Three years earlier he had received a
diagnosis of Graves’ disease with thyroid-associated ophthalmopathy and
dermopathy. He was treated with radioactive iodine ablation. Photographs taken
1 year after treatment showed
proptosis (Panel A)
and
pretibial myxedema
(Panel B).
Shortly thereafter he underwent orbital decompression in both eyes. At
the time of the current presentation, his physical examination showed progression
of the dermopathy, which was functionally limiting and
resembled elephantiasis
(Panel C).
In addition, his hands were enlarged and coarsened, and his fingers
had a
clublike shape (Panel D).
Radiography of the hand showed
periostitis of
multiple
phalangeal and metacarpal
bones (Panel E, arrowheads), with diffuse
swelling of the soft tissue, changes that were consistent with thyroid acropachy, a
rare manifestation of Graves’ disease. Laboratory results showed that levels of
thyrotropin-receptor antibodies were in excess of 40 IU per liter (normal range,
1.75 IU per liter); the test did not allow for more precise measurement. The patient
was started on a combination treatment with intravenous immune globulin and
rituximab. which appeared to halt the progression of his condition. At follow up
several months later there was no disease progression.
Nejm.org July 21, 2016
This 12-year-old boy
presented with abdominal
pain. What is the diagnosis?
1. Cowden syndrome
2. Cronkhite-Canada syndrome
3. Osler-Weber- Rendu
syndrome
4. Peutz-Jeghers syndrome
5. VonWillebrand syndrome
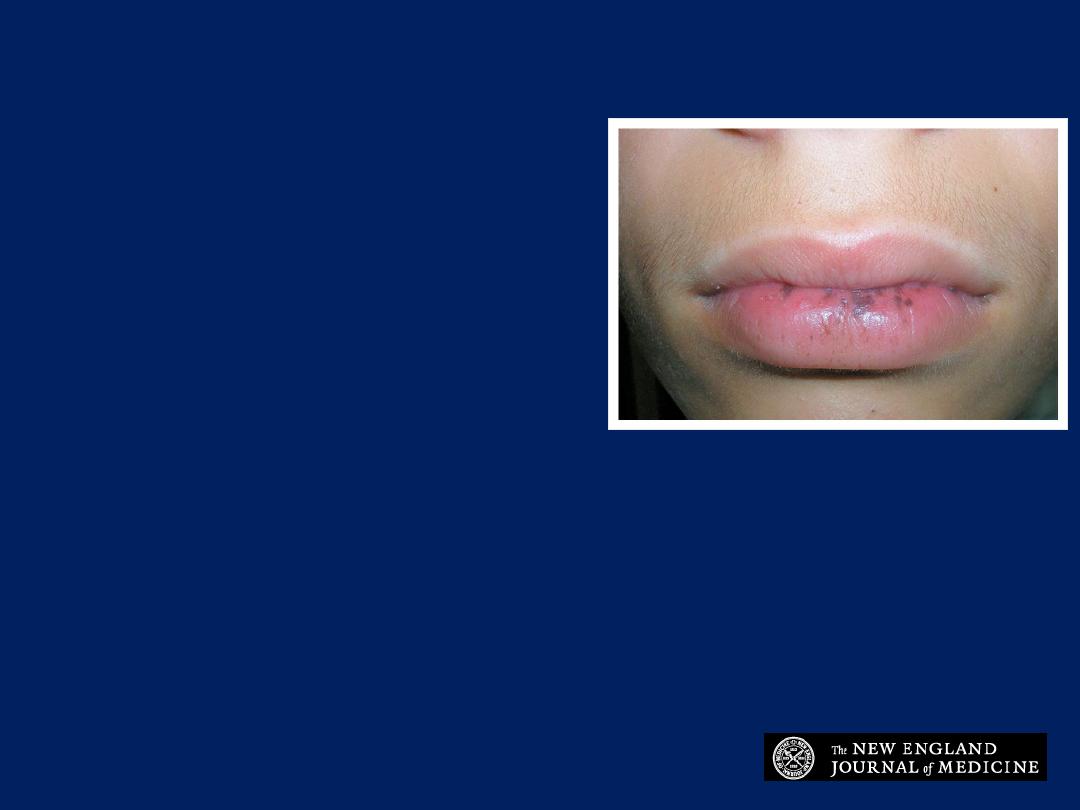
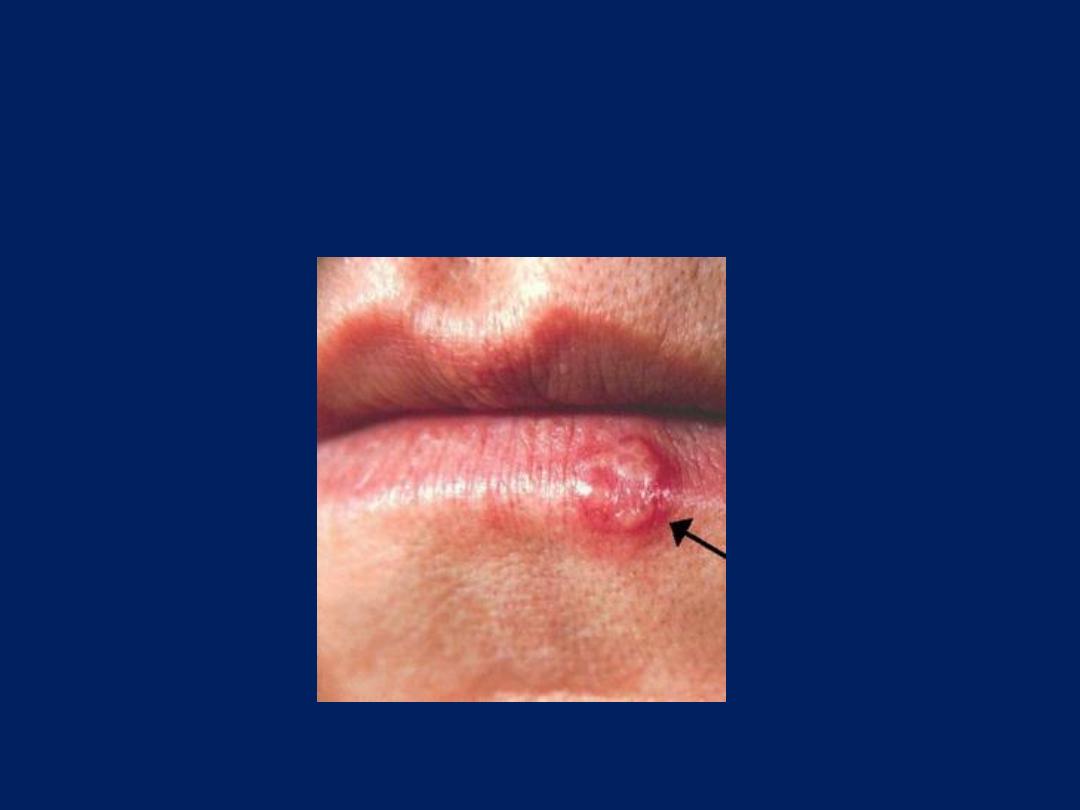
Peutz-Jeghers syndrome
The presence of mucocutaneous pigmented lip
lesions suggests the diagnosis of Peutz-Jeghers
syndrome, an autosomal dominant disorder
characterized by development of multiple
hamartomatous gastrointestinal polyps.

Special facies
Lower motor neuron left fascial palsy
NEJM 2016
The Marin- Amat syndrome
Synkinesis
describes the
involuntary movement
of a
muscle that
occurs with the voluntary
movement of a
different muscle. Cranial-nerve examination revealed
involuntary unilateral ptosis that coincided with voluntary
contraction of the lower facial muscles .
The Marin- Amat syndrome
, a specific form of intrafacial
synkinesis, describes the contraction of the orbicularis oculi
muscle with the movement of the lower facial muscles. It is
thought to develop primarily as a result of aberrant
regeneration of nerve fibers after traumatic injury and
can be a sequela of Bell’s palsy.
Treatment options for synkinesis
include facial
neuromuscular retraining and injection of botulinum toxin.
NEJM 2016
Special facies
Parotid swelling
Facial skin color
plethoric face



Facial skin color
Earthy color

Facial skin color
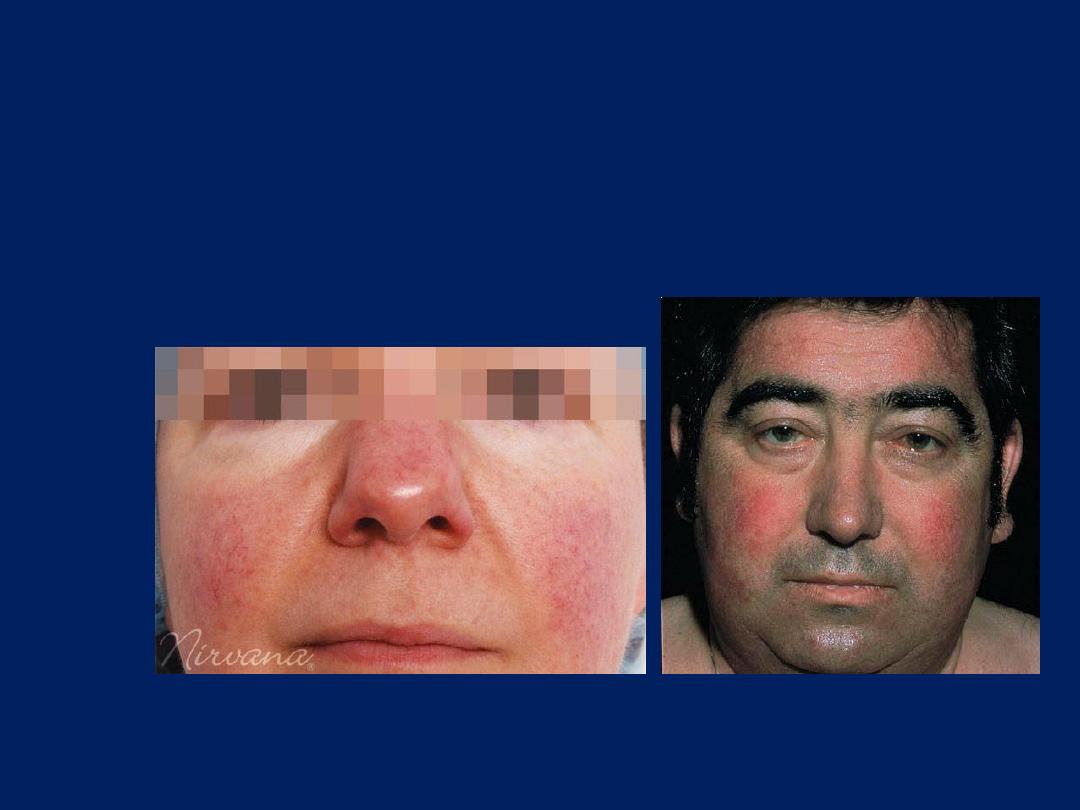
Malar flush
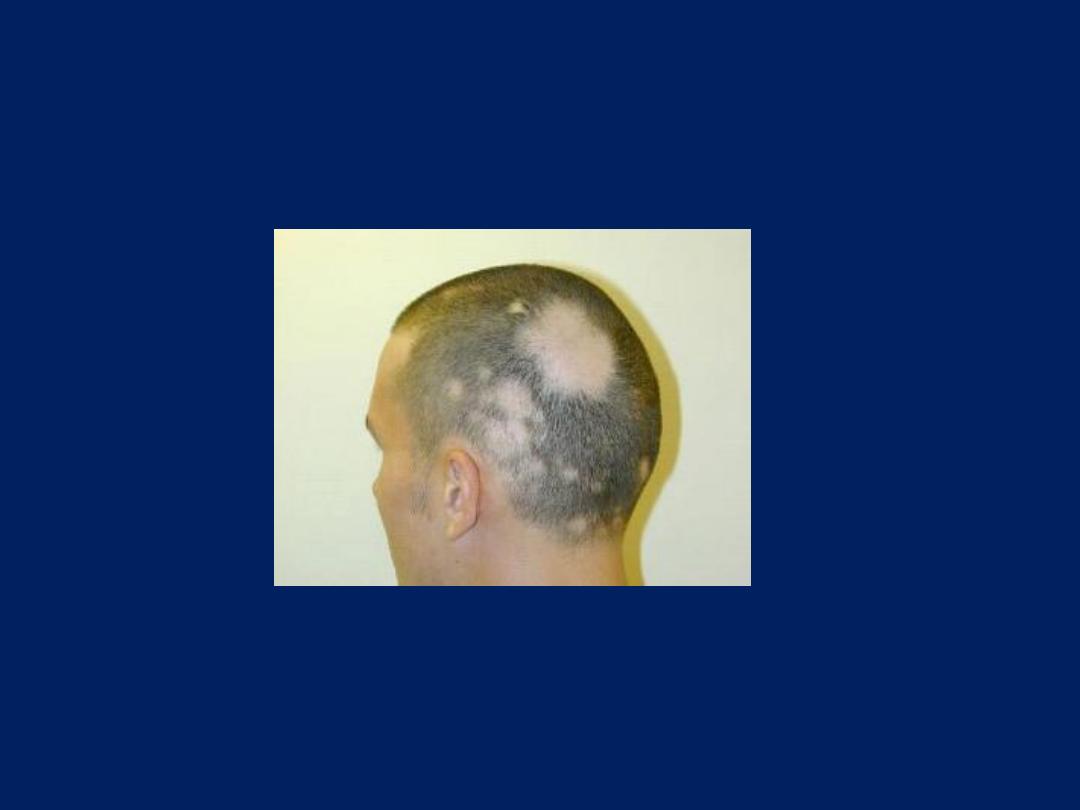
Hair Exam
Alopecia

Lip Exam
Cyanosis
Lip Exam
Herpes labialis

Lip Exam
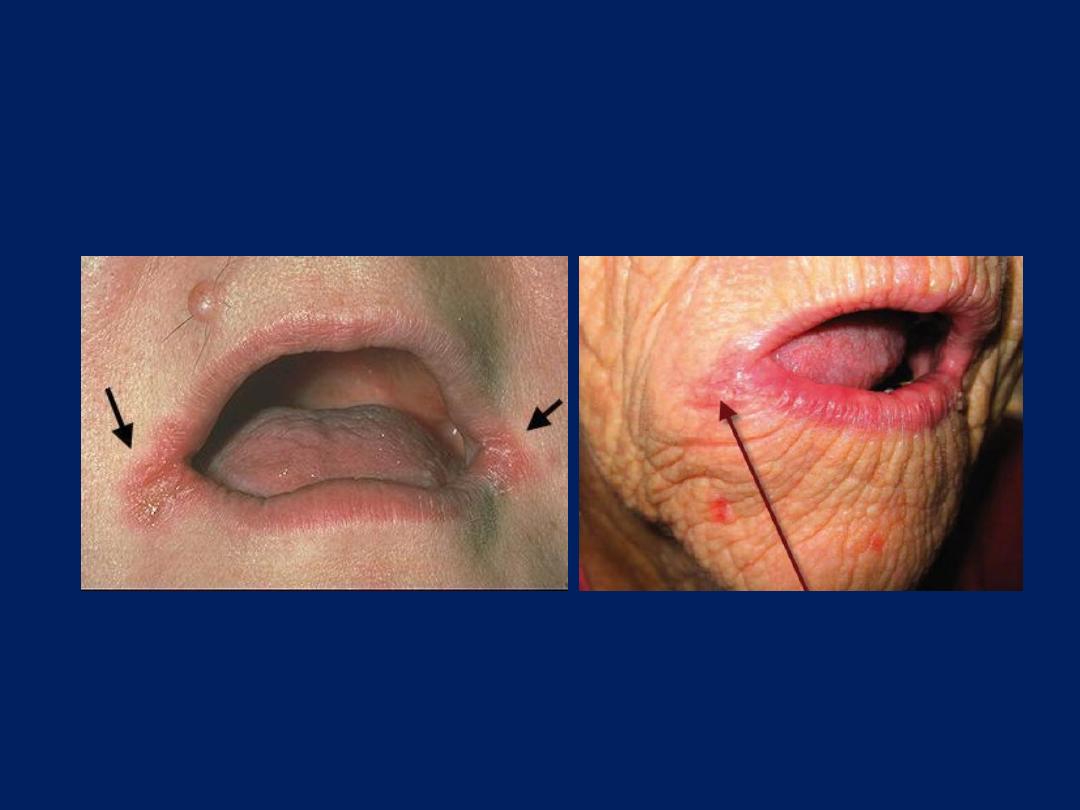
Angular stomatitis

Lip Exam
Ulcer

Herpes Zoster
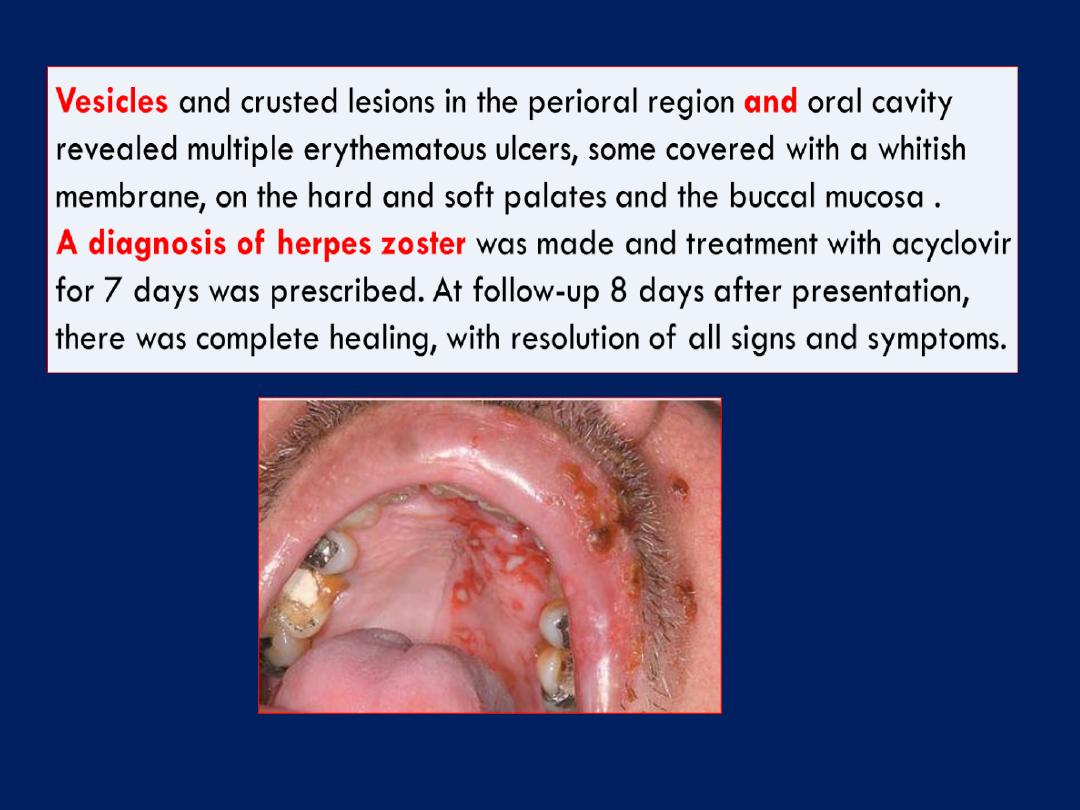
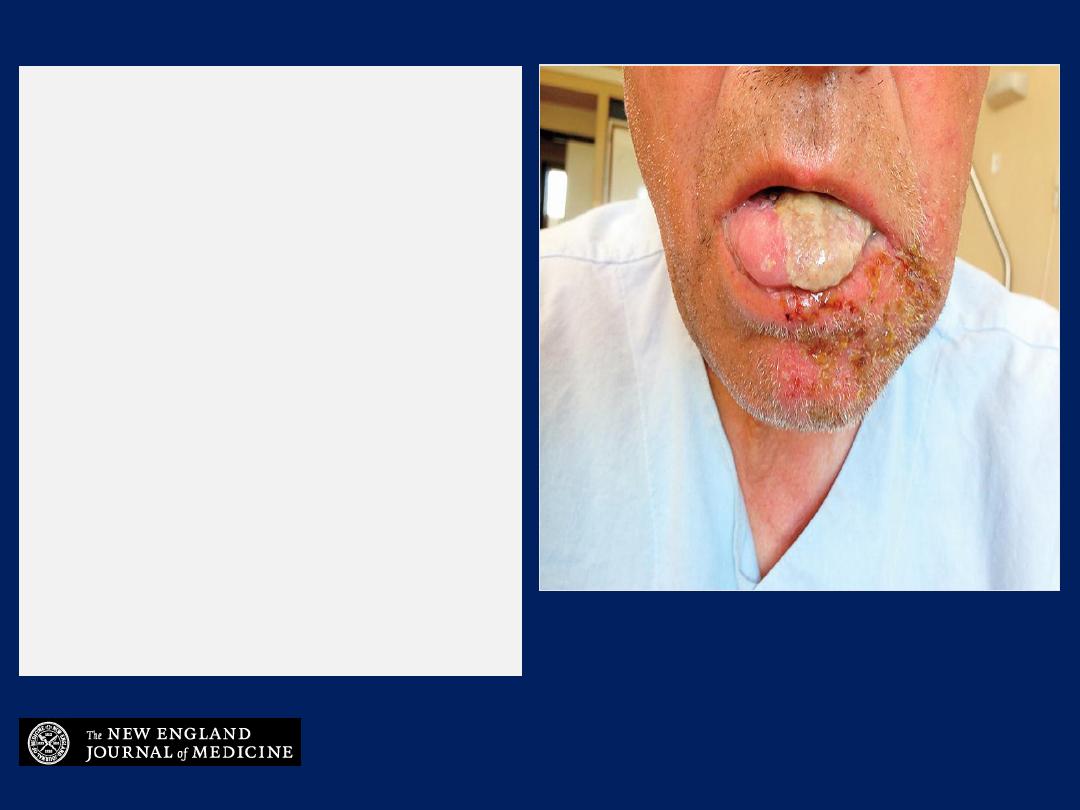
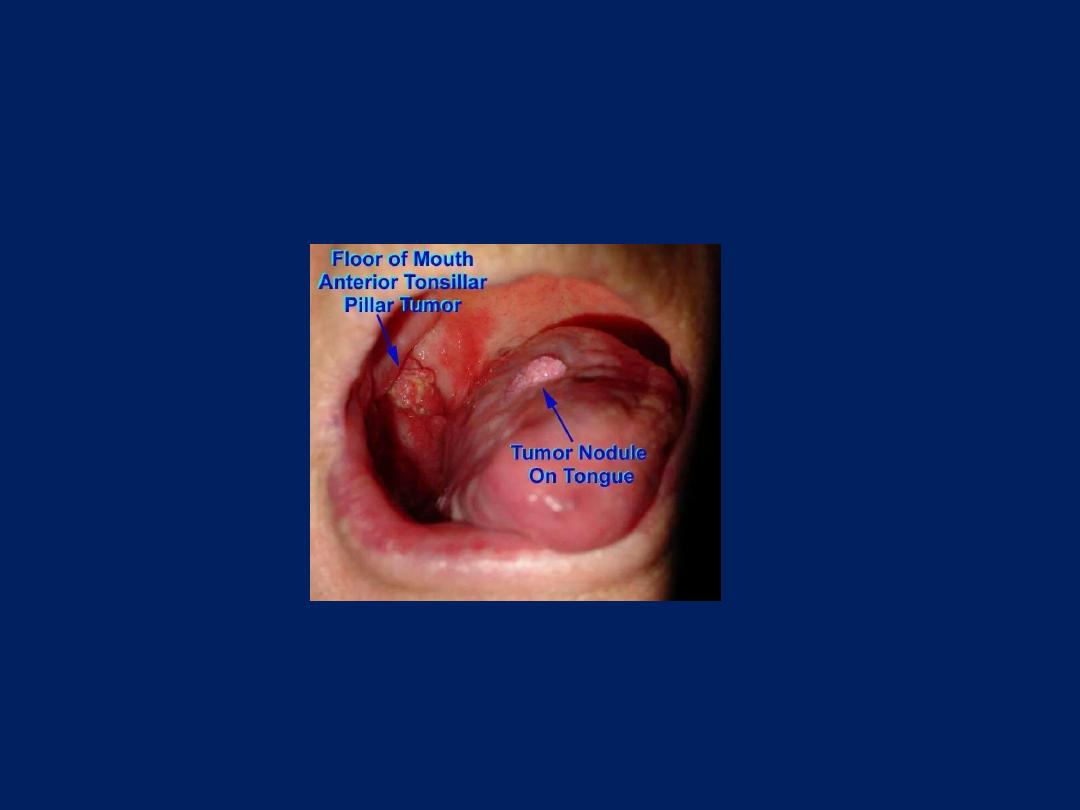
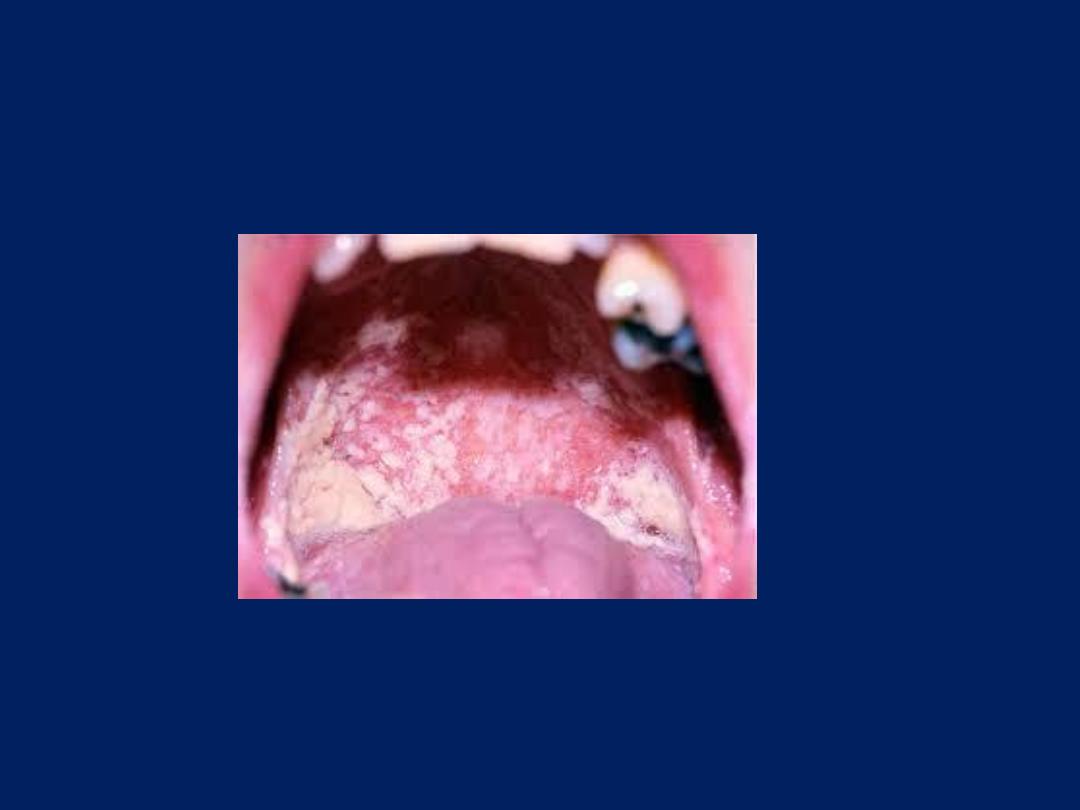
Image Challenge
What is the most likely
cause of this patient’s
presentation with rash and
pain on the left side of his
face, and plaque over the
anterior two-thirds of his
tongue?
1. Herpes simplex virus
2. Enterovirus
3. Contact dermatitis
4. Bullous pemphigoid
5. Varicella-zoster virus
Image Challenge
Answer: Varicella-zoster virus
The answer is varicella-zoster virus. This patient presented
with 3 days of pain on the lower half of the left side of
his face, otalgia, and glossodynia prior to the
development of facial edema and a vesicular rash. The
dermatomal distribution of the symptoms with respect to
the midline led to a diagnosis of varicella-zoster virus
(VZV) reactivation in the mandibular (V3) distribution of
the trigeminal nerve (cranial nerve V). When zoster
affects the trigeminal nerve, it most often affects the
ophthalmic (V1) division. This patient’s mandibular zoster is
seen much less commonly.
A 70-year-old man presented with a 2-day history of facial edema, rash with
vesicles, pustules, and crusts along the left lower jaw, and plaque that had covered
the anterior two thirds of the left half of his tongue. He reported that he had had
pain in the lower half of the left side of his face, otalgia, and glossodynia for 3
days before the outbreak of the rash. On examination, there were no neurologic
deficits, meningeal signs, or lymphadenopathy. The lesions were scattered along
the area that is innervated by the third division of the trigeminal nerve.
A presumptive diagnosis of
herpes zoster mandibularis
was made. Given the
particular distribution of the rash, herpes simplex virus or enterovirus infection was
considered to be less likely. The patient underwent empirical treatment with
acyclovir, analgesic agents (including gabapentin), nystatin, and an antibiotic
agent for bacterial superinfection.
One month after the resolution of the facial rash, postherpetic neuralgia
developed along the involved dermatome. The patient had moderately intense
pain for approximately 4 months after resolution of the rash, after which time the
pain subsided. At a follow-up visit 6 months after the resolution of the rash, he was
asymptomatic and had stopped taking gabapentin.

Gum Exam
Gingivitis

Gum Exam
Gingival hypertrophy
Gingival enlargement (hyperplasia)
has been classified
according to etiology into 5 general groups:
1. Inflammatory
enlargement, the accumulation and retention of
plaque is the chief cause of inflammatory gingival
enlargement. Risk factors include poor oral hygiene, HIV
infection.
2. Drug
induced enlargement
3. Enlargement associated with
systemic diseases
4. Neoplastic
enlargement
5. False
enlargement , when there is an underlying bony or
dental tissue lesion
6. Hormonal
changes: Pregnancy , puberty
False gingival enlargements:
due to underlying teeth or bone lesion.
Gingival enlargement
Drug-induced overgrowth
Three different classes of drugs, all producing a similar response
anticonvulsants (phenytoin, phenobarbital, lamotrigine, topiramate
and primidone NOT common for valproate).
calcium channel blockers, such as nifedipine, amlodipine, and
verapamil. The dihydropyridine derivative isradipidine can replace
nifedipine and does not induce gingival overgrowth.
immunosuppresant ,cyclosporine.
Drug-induced enlargement has been associated with a patient's
genetic predisposition and its association with inflammation is
debated. Some investigator s assert that underlying inflammation is
necessary for the development of drug-induced enlargement.
Many systemic diseases
leukemia , granulolomatous diseases ,wegener granulomatosis,
sarcoidosis, Crohn disease, primary amyloidosis, and acromegaly ,
fibromas, papillomas and malignant melanoma . V C deficiency .

Teeth Exam
Dental caries



Tongue Exam
Glossitis

Tongue Exam
pallor
Tongue Exam
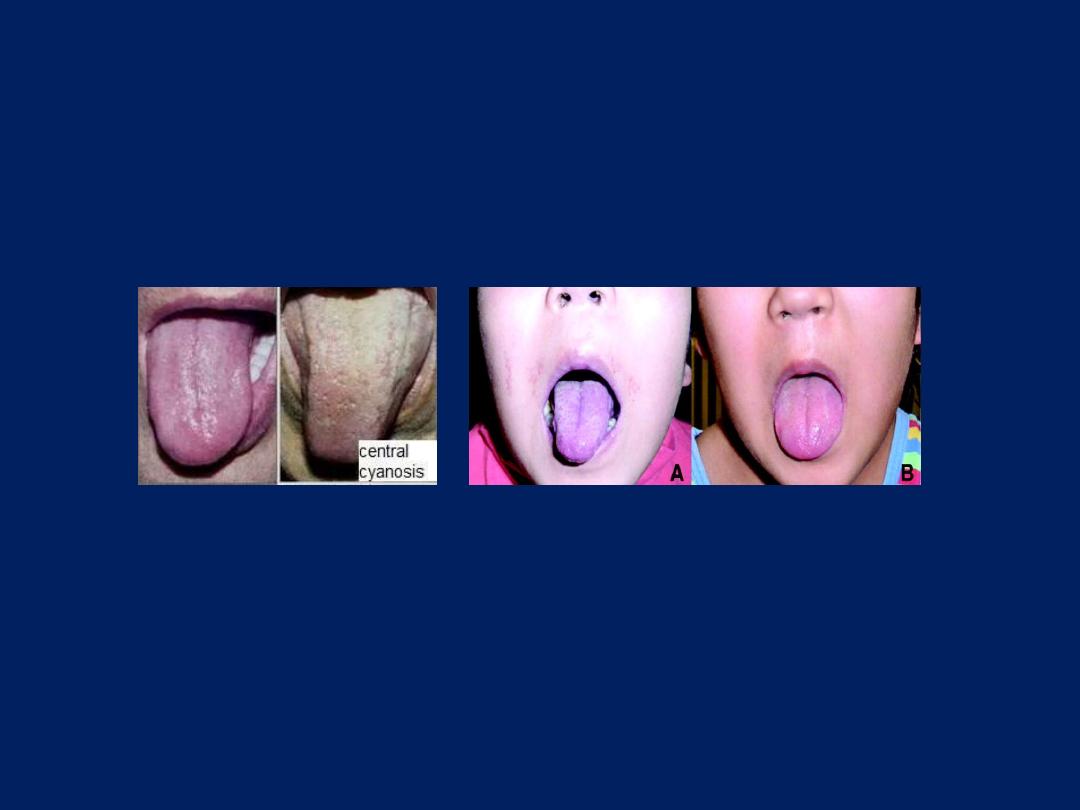
Central cyanosis

Tongue Exam
Dry tongue
Tongue Exam
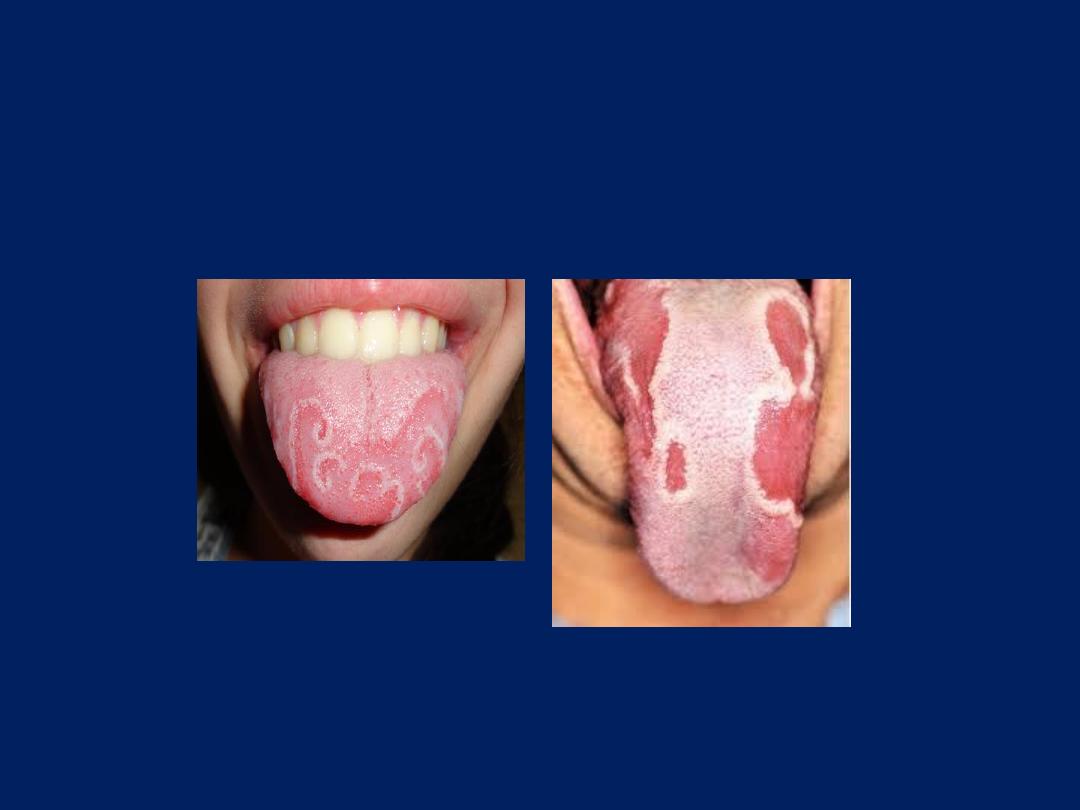
Geographical tongue
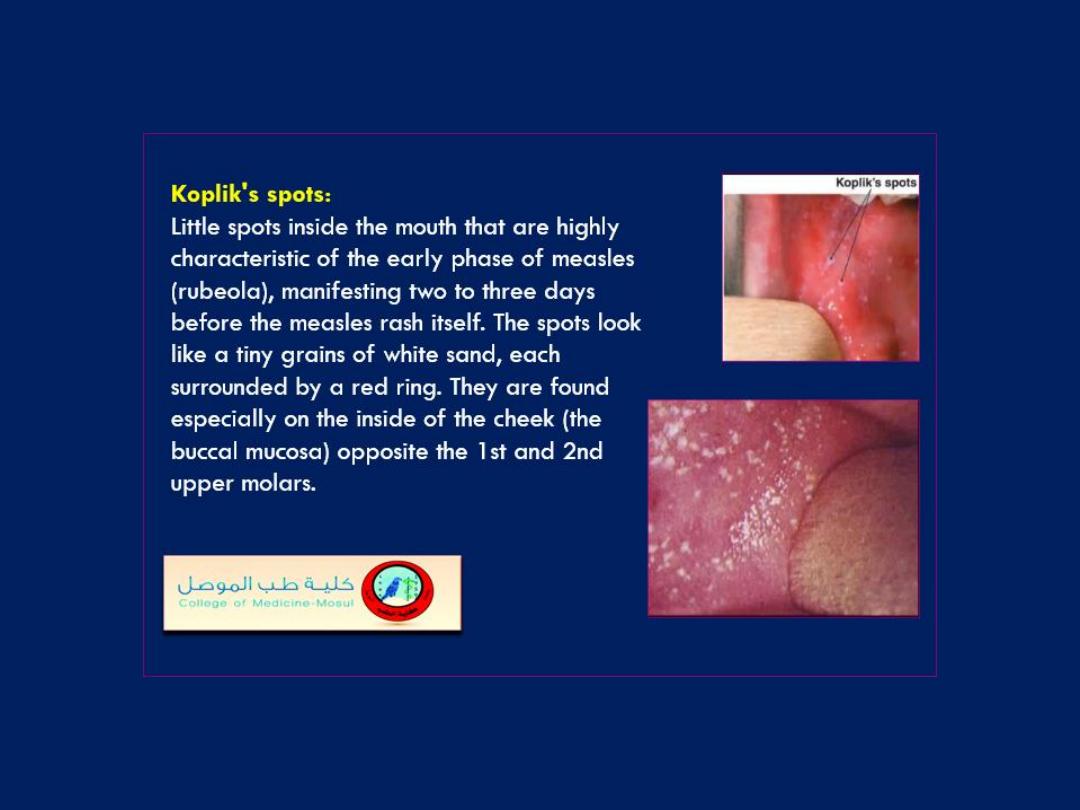
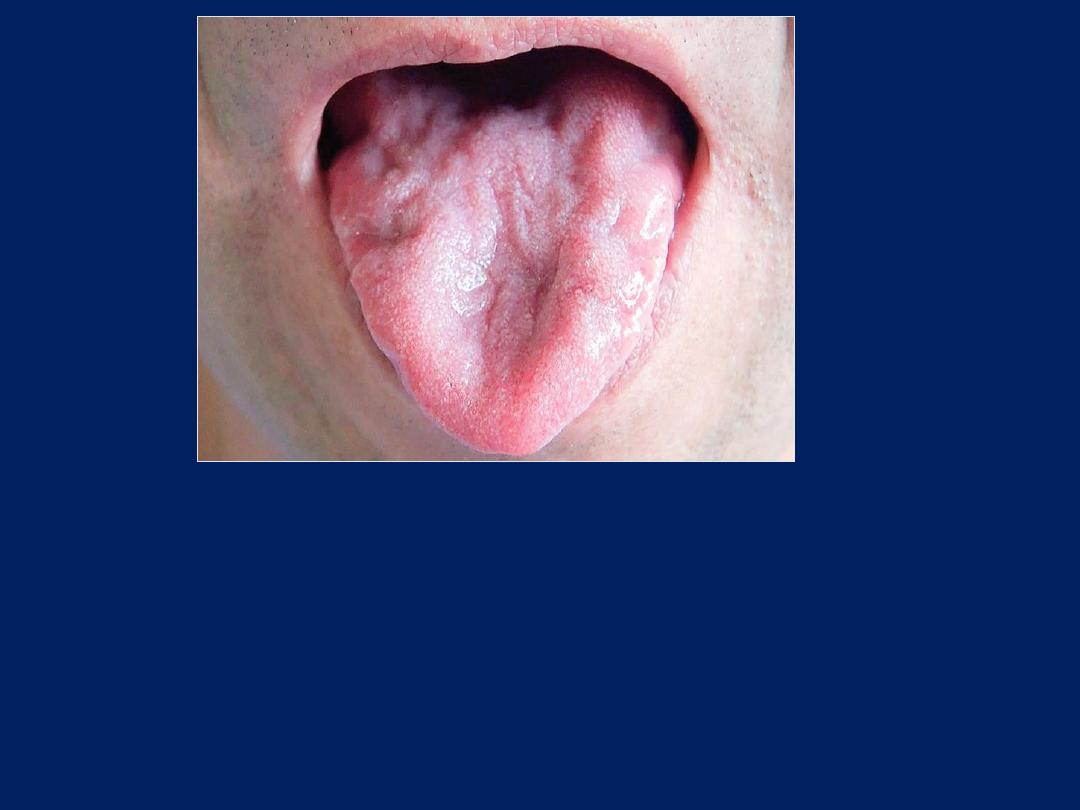
61-year-old man was referred for treatment of painless white lesions
on his tongue that had appeared 1 month earlier. He had been
treated with topical antifungal drugs for presumed oral candidiasis,but
the lesions remained unchanged. The patient reported that a similar
episode 1 year earlier had resolved spontaneously. Lingual
examination revealed multiple erythematous patches with an
annular, welldemarcated white border. A diagnosis of geographic
tongue was made.
Geographic tongue
(benign migratory glossitis) is
a benign inflammatory condition that affects approximately 2% of the
world’s population. The classic manifestation is a maplike distribution
of erythema caused by atrophy of the filiform papillae of the tongue,
surrounded by a white hyperkeratotic rim. The lesions typically
resolve spontaneously without sequelae but can develop quickly in
other areas of the tongue.
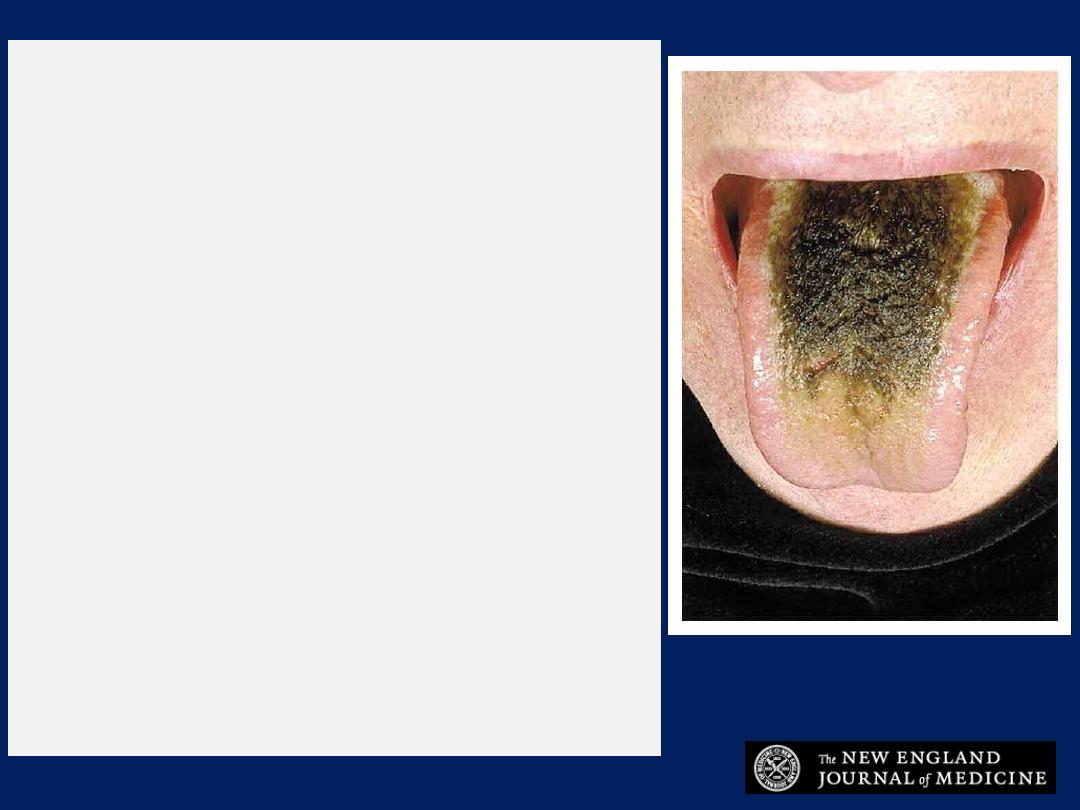
Black hairy tongue,
also known as lingua villosa
nigra, is a painless, benign disorder caused by
defective desquamation and reactive hypertrophy
of the filiform papillae of the tongue. It is
characterized clinically by an abnormal brownish-
black coating of the dorsal surface of the tongue.
The exact pathogenesis is unclear. A number of
relevant etiologic factors have been assumed,
including the use of topical or systemic antibiotics as
well as psychotropic agents, dehydration,
hyposalivation, trigeminal neuralgia, poor oral
hygiene, smoking, ingestion of alcohol, and infections.
Symptoms may include nausea, halitosis, dysgeusia,
and unattractive appearance of the tongue.
Therapeutic options of modest benefit include
increasing hydration and salivation, discontinuing
smoking, brushing the tongue with a soft toothbrush
enhanced by previous application of 40 percent
urea, applying topical retinoids or salicylic acid, or
undergoing surgical excision.
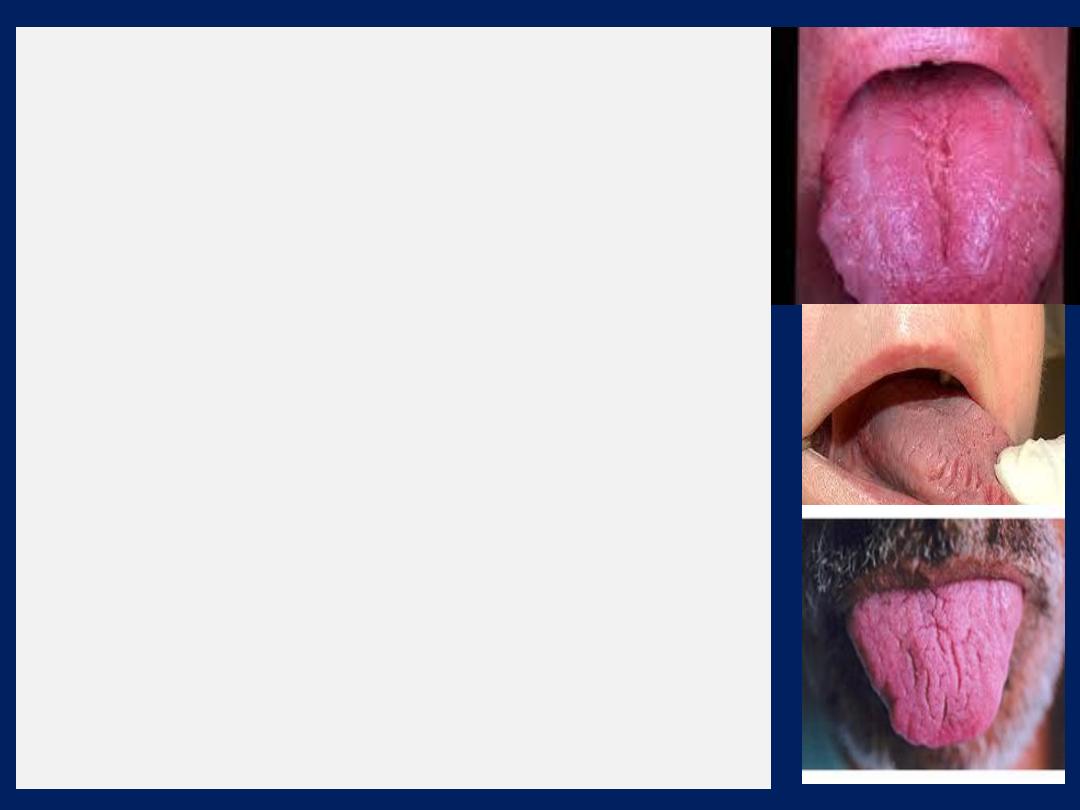
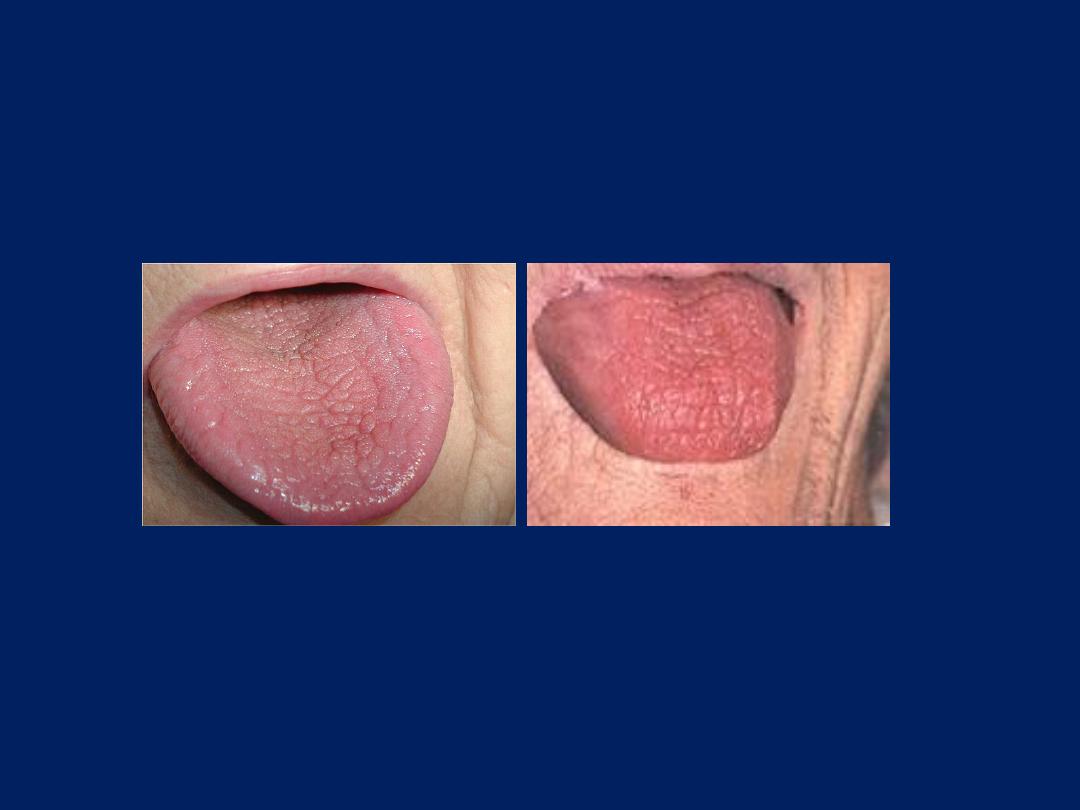
Fissured Tongue
In fact, certain types of grooves or cracks are
considered simply a variation of a normal tongue.
Sometimes called a plicated or scrotal tongue, this
condition is often harmless. Because a fissured tongue
can cluster in families, it may be genetically inherited, it
may appear along with other conditions such as
Geographic tongue, also known as benign migratory
glossitis(BMG). This benign condition often shows up
along with fissured tongue. It may cause no symptoms
other than sensitivity to hot and spicy foods.
A fissured tongue may be an indication of a yeast
infection. Other medical conditions, such as anemia and
vitamin or mineral deficiencies, or local irritants, such
as uneven or broken teeth, cigarette smoking, alcohol,
and strong mouthwashes, may also cause fissured
tongue. Does not require any specific treatment. You
can brush the top surface to remove any remainder that
may cause irritation.
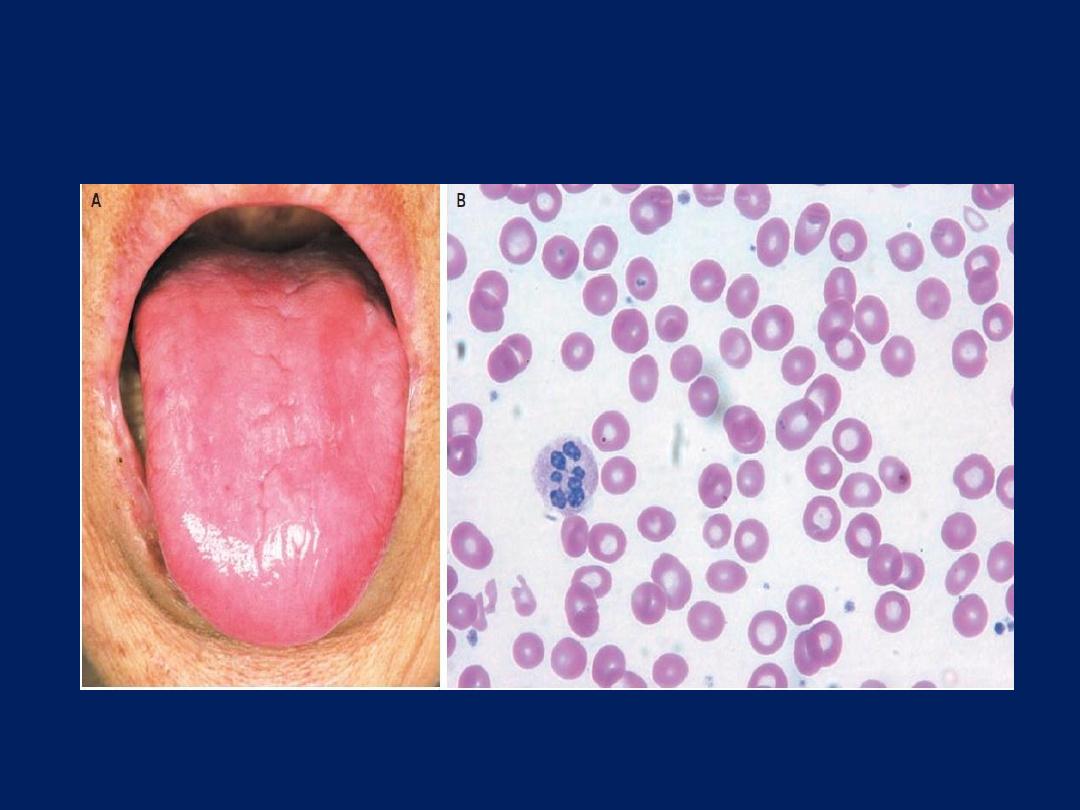
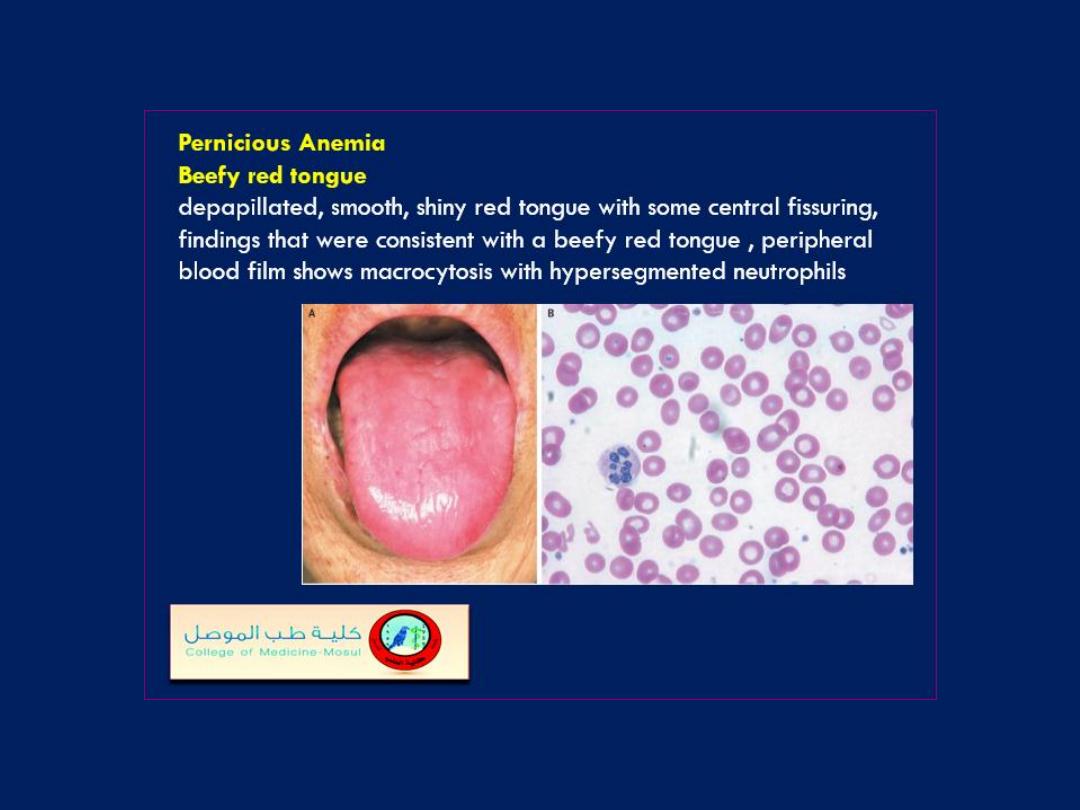
Beefy red tongue
77-year-old woman presented with an insidious onset of fatigue and a burning
sensation of the tongue on swallowing food. Six years earlier, she had undergone
a total gastrectomy for early gastric cancer, which was curative.
On physical examination, she was pale and had a depapillated, smooth, shiny
red tongue with some central fissuring, findings that were consistent with a
beefy red tongue (Panel A). Laboratory testing revealed cytopenia (white-cell
count, 3400 per cubic millimeter; hemoglobin level, 6.4 g per deciliter; and
platelet count, 154,000 per cubic millimeter) with macrocytosis (mean corpuscular
volume, 132 fl [normal range,80 to 100]; red-cell distribution width, 18.6%; and
reticulocyte count, 2.8%) and hypersegmented neutrophils (Panel B, Wright’s
stain). The serum vitamin B12 level was 75 pmol per liter (55 pg per milliliter)
(normal range, 160 to 970 [118 to 716]), and the serum folate level was normal.
The patient received a diagnosis of
megaloblastic anemia
due to vitamin B12
deficiency. She was treated with intramuscular vitamin B12 and had a complete
recovery after approximately 5 months.
A smooth, thickened, depapillated tongue may be associated with a variety of
systemic disorders, including nutritional deficiency.
What is the diagnosis?
1. Herpetic glossitis
2. Aphthous ulceration
3. Pemphigoid
4. Scurvy
5. Oral candidiasis
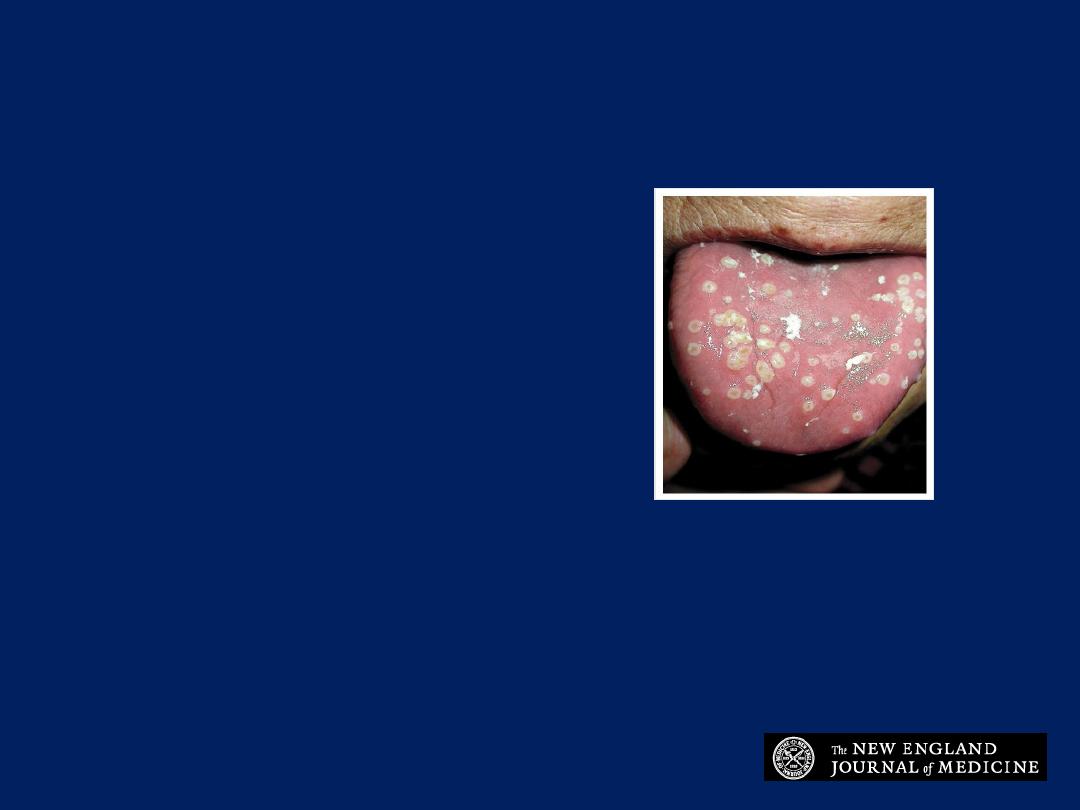
Herpetic glossitis
These multiple well-defined white
papules with a central punctum are
most consistent with herpetic glossitis.
Westra S and de Jager C. N Engl J Med 2006;355:295
diffuse swelling of The tongue
Angioedema
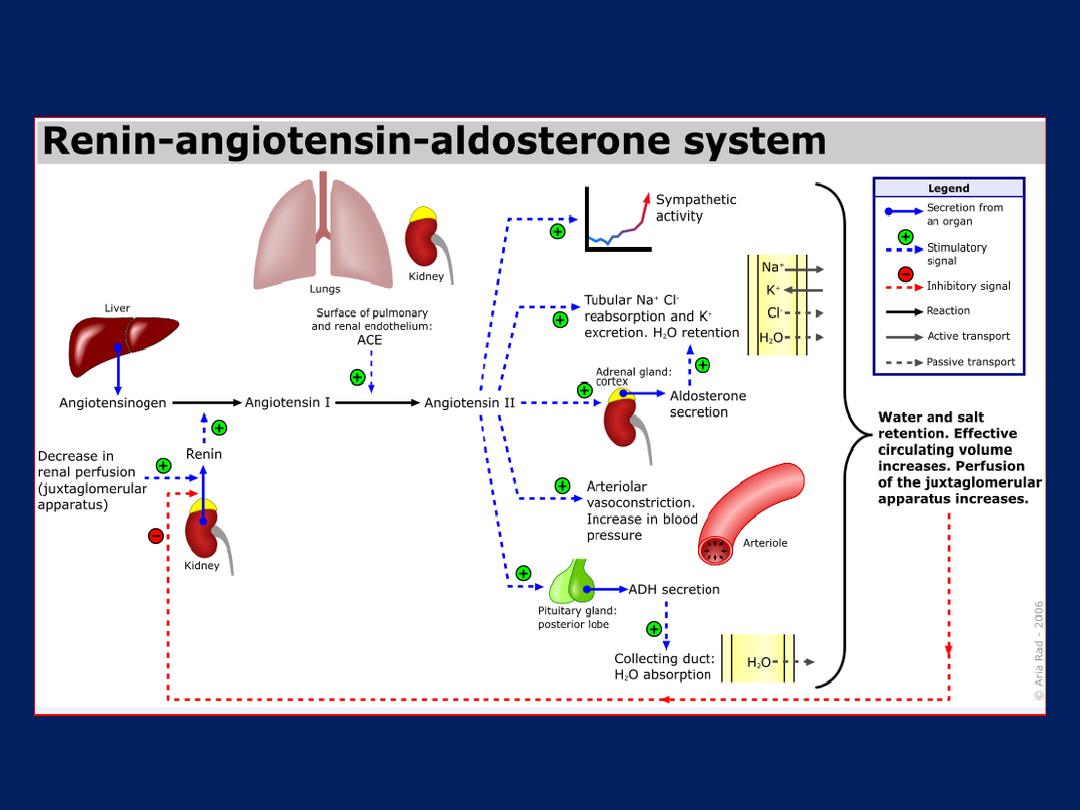
A 71-year-old man presented to the emergency department with rapidly
progressive tongue swelling during the previous 5 hours.
Physical
examination revealed a swollen tongue and no hypotension, rash, bronchospasm,
urticaria, or flushing. There was no personal or family history of similar episodes,
and the patient had no recent exposure to known food allergens, new
medications, or insect stings. His usual outpatient medications included aspirin,
simvastatin, diltiazem, and enalapril. A provisional diagnosis of angioedema
associated with the use of an angiotensin-converting–enzyme (ACE) inhibitor was
made. Inhibition of ACE may prompt a decrease in the production of angiotensin
II and an increase in the
bradykinin level,
resulting in the regional vasodilatation
and increased vascular permeability that are characteristic of angioedema. The
onset of angioedema can occur even after long-term use of ACE inhibitors. In this
patient, no improvement was noted after the parenteral administration of
diphenhydramine, methylprednisolone, and epinephrine. With the patient awake,
a nasotracheal intubation was performed to prevent impending respiratory
compromise. Treatment with enalapril was discontinued. The edema resolved, the
tongue returned to normal size, and the patient was extubated the next day.
There has been no return of symptoms after discontinuation of the ACE inhibitor.
What is the most likely diagnosis in this patient who was having
difficulty swallowing?
1. Amyloidosis
2. Amyotrophic lateral sclerosis
3. Pellagra
4. Pernicious anemia
5. Sjogrens syndrome

Answer
Amyotrophic lateral sclerosis
With his difficulty swallowing, the patient's tongue
atrophy represents a bulbar symptom, and is most
consistent with a diagnosis of amyotrophic lateral
sclerosis (ALS). ALS is associated with dysarthria,
hypophonia, dysphagia, and sialorrhea in addition to
relentlessly progressive disability.
Tongue Exam
tumor

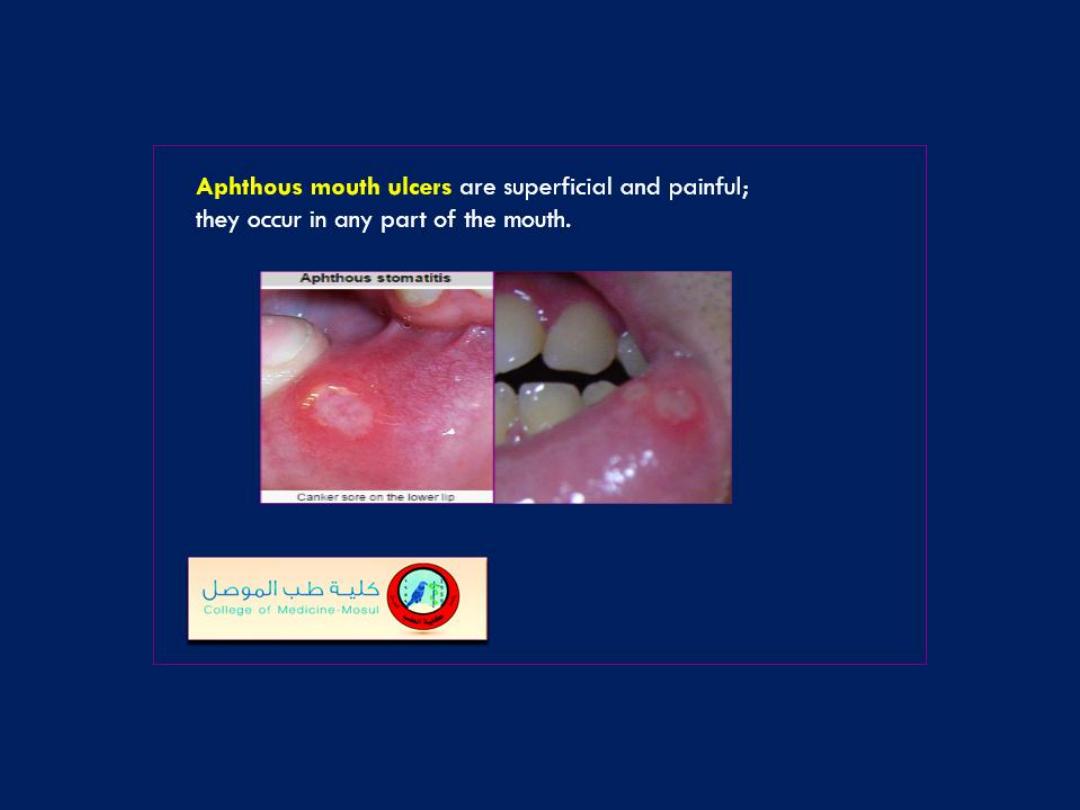
Buccal mucosa
Aphthus ulcer
Buccal mucosa
Thrush
Buccal mucosa
Petechial hemorrhage

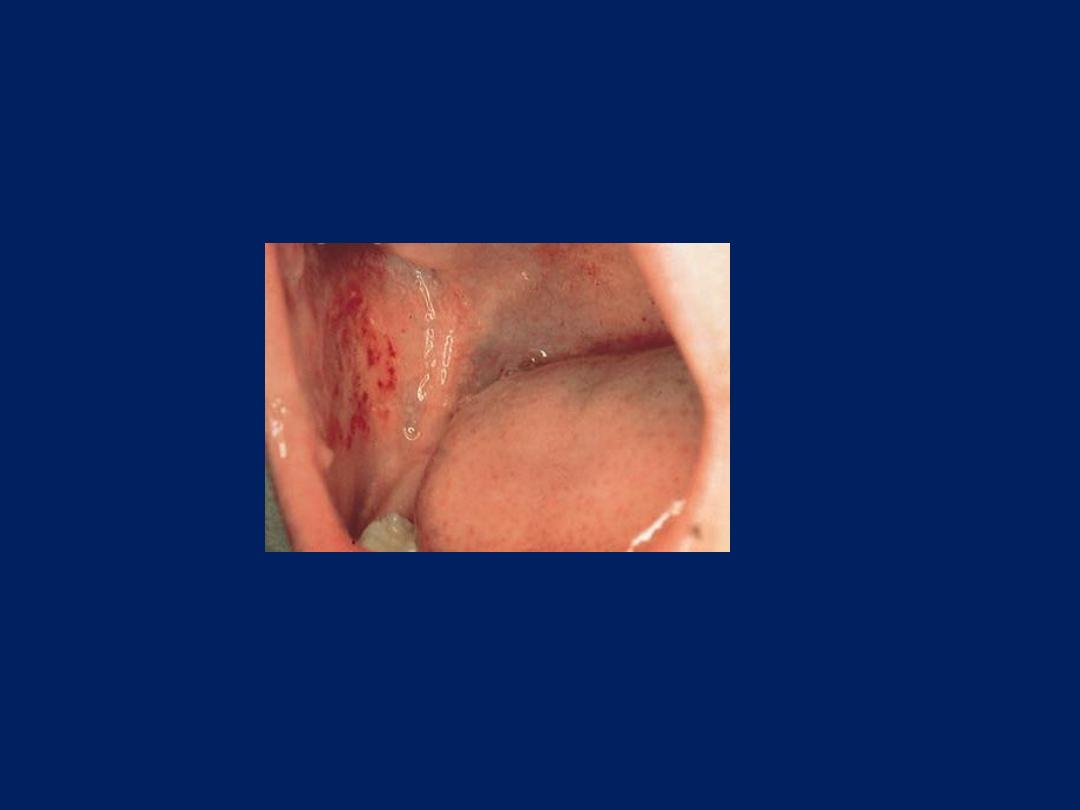
26-year-old man presented to the emergency department with a two-
day history of a sore throat. He was unable to eat solids because of
pain and swelling but was tolerating liquids. He was afebrile but had
taken 800 mg of ibuprofen one hour before arrival. On physical
examination, a white exudate was seen on the tonsils (arrows). The
patient was treated with 1.2 million units of penicillin
G benzathine intramuscularly and given a benzocaine spray for
topical analgesia. The results of a throat culture confirmed the
diagnosis of
streptococcal pharyngitis.
Streptococcal pharyngitis is
caused by group A b -hemolytic streptococci and most often affects
persons situated in close quarters. Common symptoms include sore
throat, pain on swallowing, and fever. The classic finding on physical
examination is the presence of white exudates on swollen tonsils, as
seen in the image. It is important to treat this self-limited illness in order
to prevent rheumatic fever.

Tonsil –Pharynx
Post nasal disharge
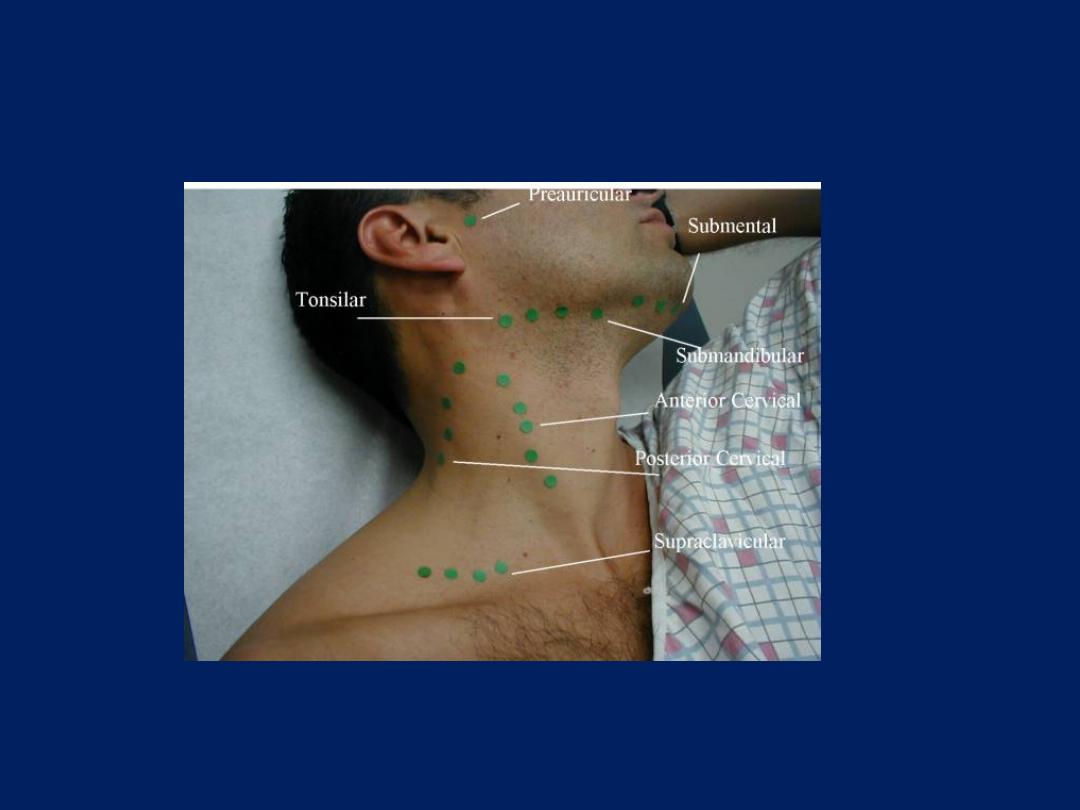
Lymph node
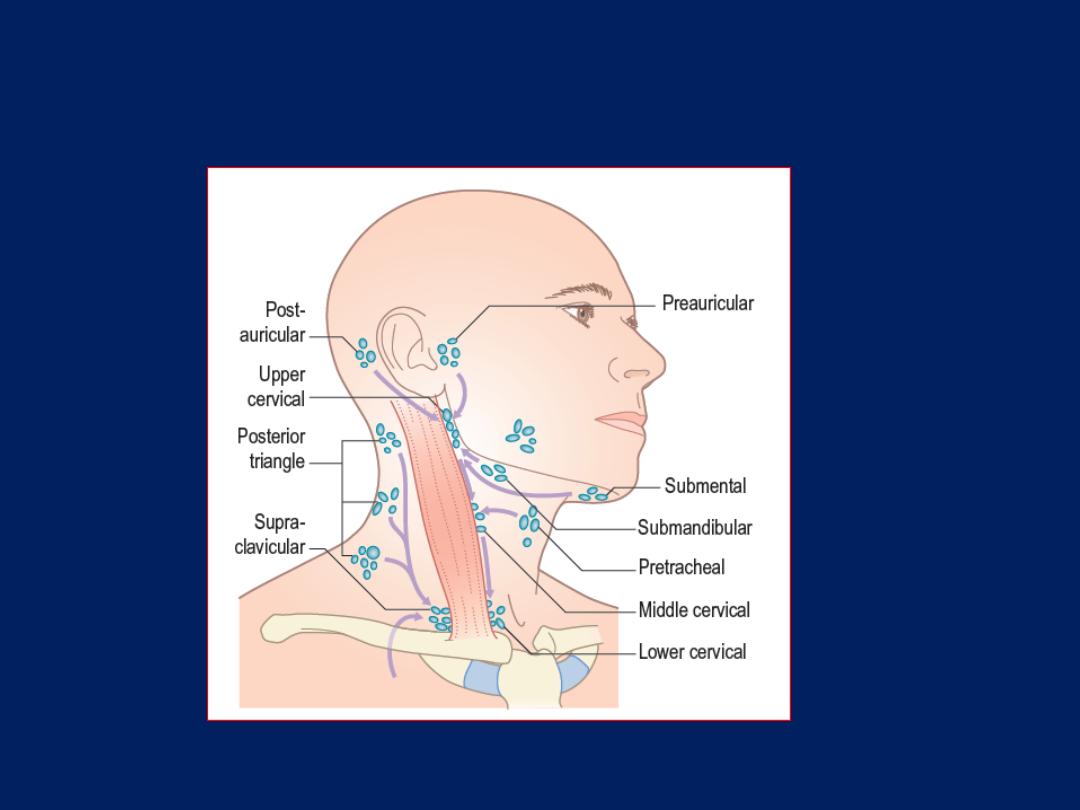
The cervical lymph node groups.
Virchow’s node, or Troisier’s node,
refers to carcinomatous involvement
of the supraclavicular nodes at the
junction of the thoracic duct and the
left subclavian vein. Usually, nodal
enlargement is caused by metastatic
gastric carcinoma, although
supraclavicular nodal involvement can
also be seen in other gastrointestinal,
thoracic, and pelvic cancers. Gastric
cancers tend to metastasize to this
region by means of migration of
tumor emboli through the thoracic
duct, where subdiaphragmatic
lymphatic drainage enters the venous
circulation in the left subclavian vein.

A 56-year-old woman presented with jaundice and a
painless mass in her left supraclavicular fossa that had
become progressively enlarged during the preceding 8 weeks
A 56-year-old woman presented with jaundice
and a
painless mass in her left supraclavicular fossa that had
become progressively enlarged during the preceding 8
weeks. Physical examination revealed a hard lymph node
measuring 6 cm by 6 cm in the left supraclavicular fossa
(Panel A) and hepatomegaly. Plain radiography of the
chest showed multiple nodular opacities in both lungs (Panel
B, arrows). Computed tomography of the abdomen
revealed multiple lesions in the liver (Panel C, arrows).
Endoscopy of the upper gastrointestinal tract showed a
fungating mass around the ampulla of Vater. Biopsy
specimens from the mass and the supraclavicular lymph
nodes showed a periampullary adenocarcinoma with
metastases. The patient was treated with chemotherapy
and palliative care. Abdominal cancers may metastasize to
the left supraclavicular lymph nodes via the thoracic duct.
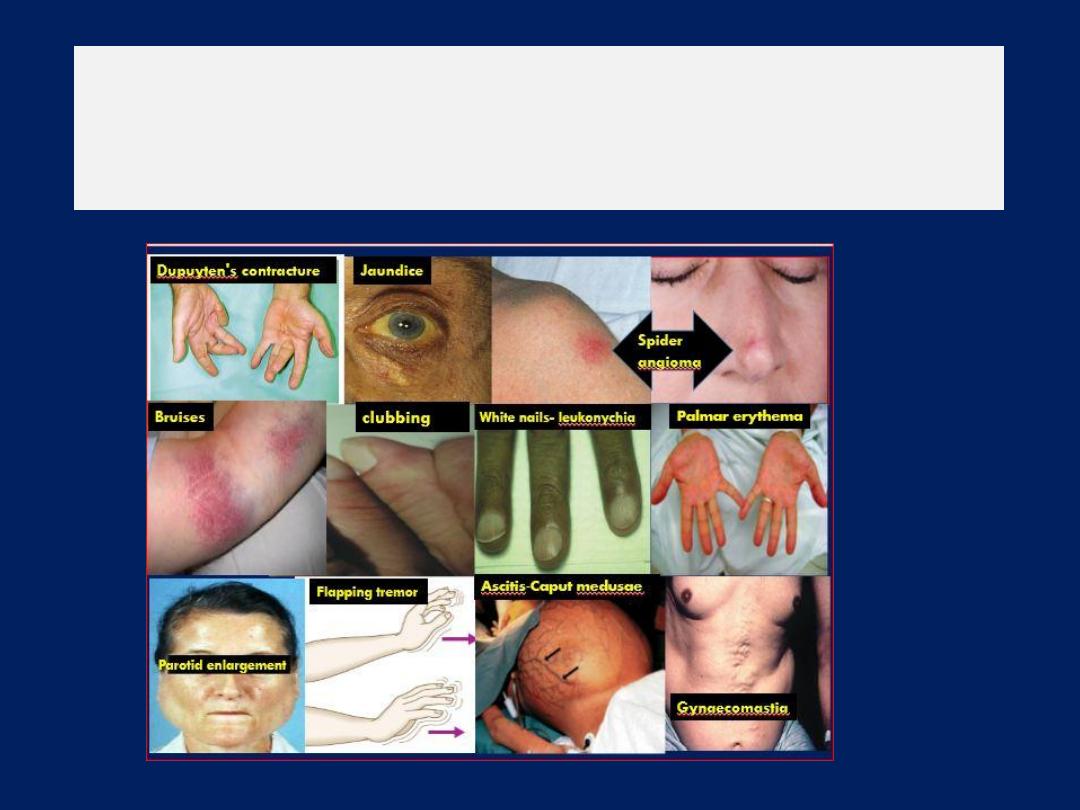
Clinical signs or stigmata of chronic liver disease
are signs that can be visualized by simple
observation of the patient
Bilateral Asterixis(flapping tremor)
Metabolic enceph alopathies, especially hepatic encephalopathy,
damage to brain cells presumably due to the inability of the liver
to metabolize ammonia to urea, “liver (hepatic) flap” and renal
failure, are the most common causes of bilateral asterixis. Those
caused specifically by hepatic failure are known as
Other causes of asterixis include severe congestive heart and
respiratory failure (CO
2
toxicity), electrolyte abnormalities include
hypoglycaemia, hypokalaemia and hypomagnesaemia.
Drug intoxications include barbiturate intoxication, alcoholism,
Asterixis can be prominent after primidone , IV phenytoin
intoxication (“phenytoin flap”), and also if the patient is on
narcotics.
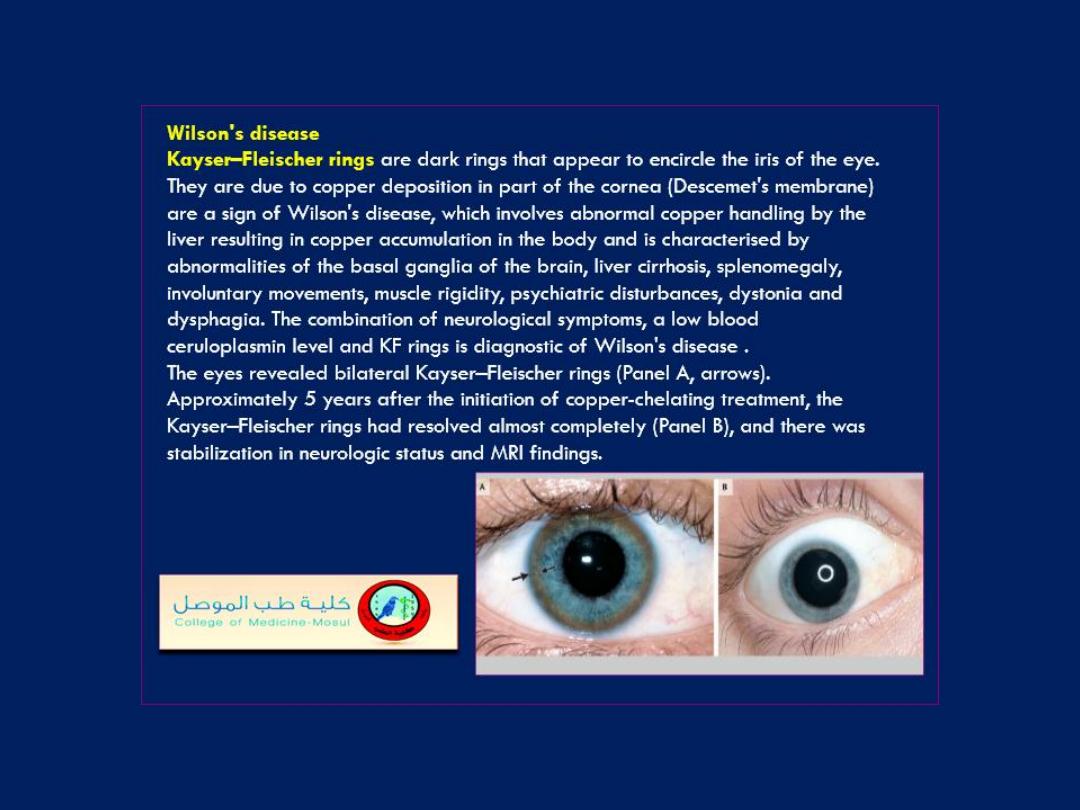
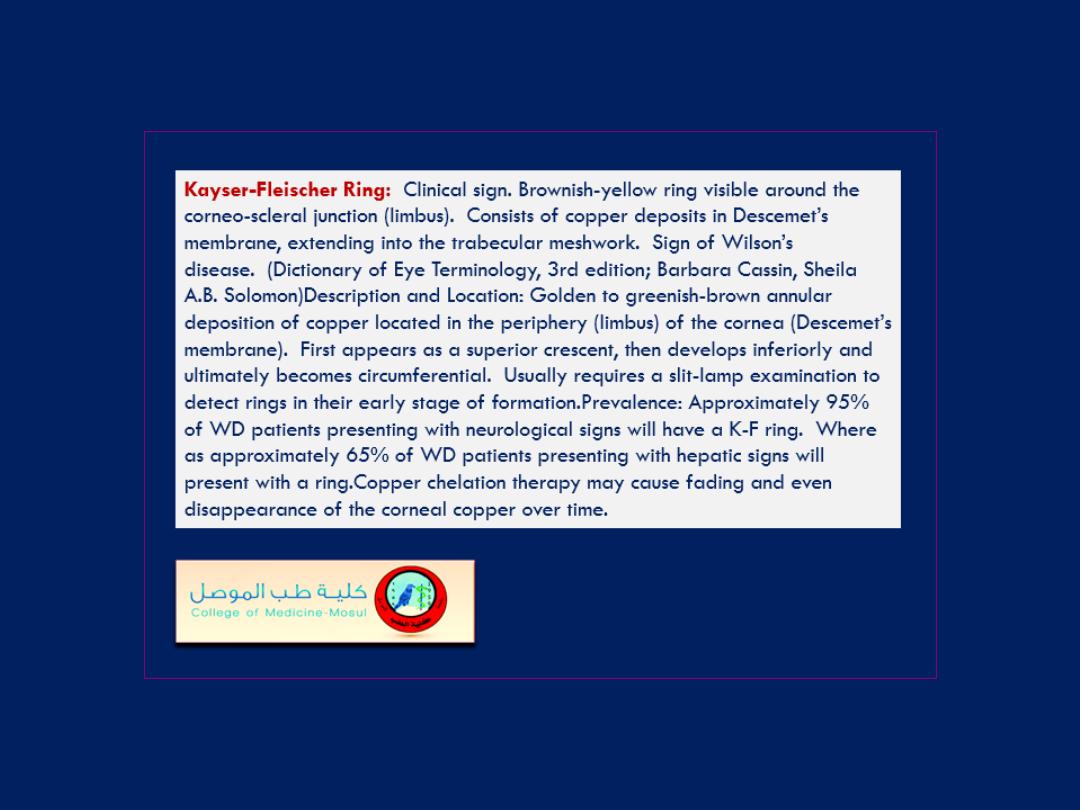
Wilson’s disease and focal brain lesions in the rostral midbrain
tegmentum may also cause asterixis.

An alternate method of testing for asterixis
involves
having the patient relax his legs
while he lies supine with his knees bent. The
feet should be kept flat on the table and as
the legs fall to the sides, watch for flapping
of the legs at the hip joint. This repetitively
brings the knees back together.

Esophageal varices grade II and III
Esophageal varices grade II (right) und grade III (left). Cherry red
spots are signs of imminent hemorrhage (right). They correspond to
areas of especially thin and altered variceal wall.
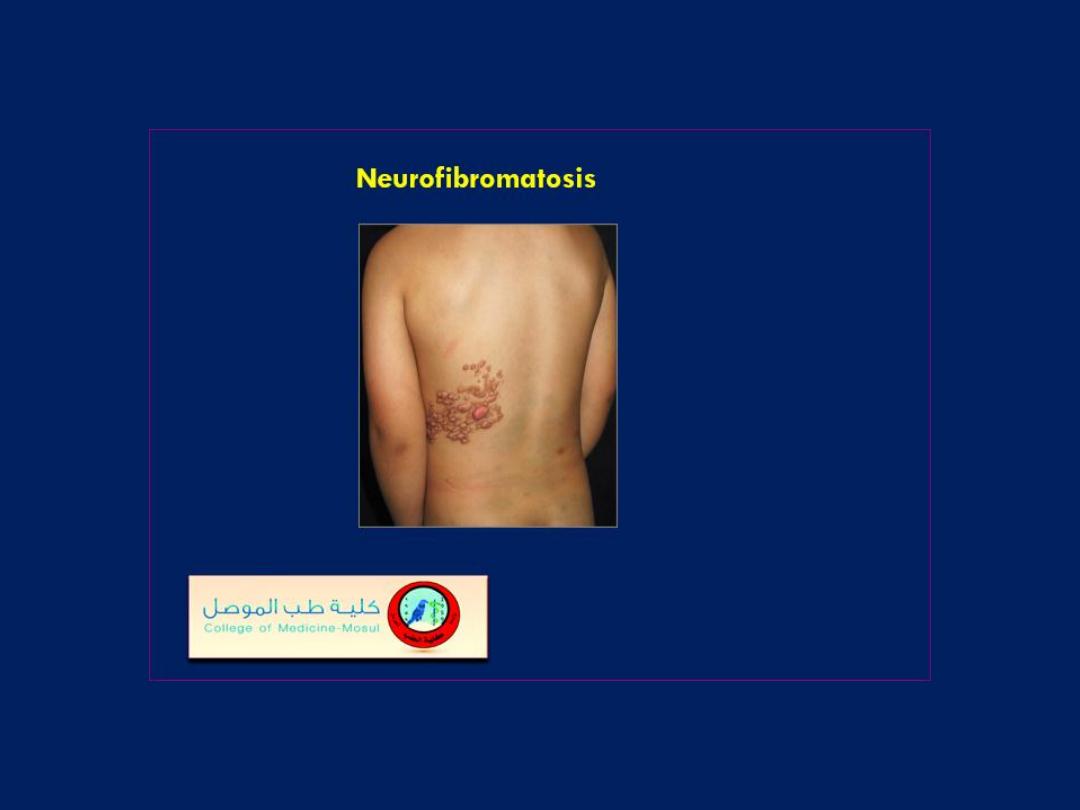
What is the diagnosis?
1. Subcutaneous metastases
2. Filariasis
3. Caput Medusae
4. Neurofibromatosis
5. Hepatocellular
carcinoma
Answer
Caput Medusae
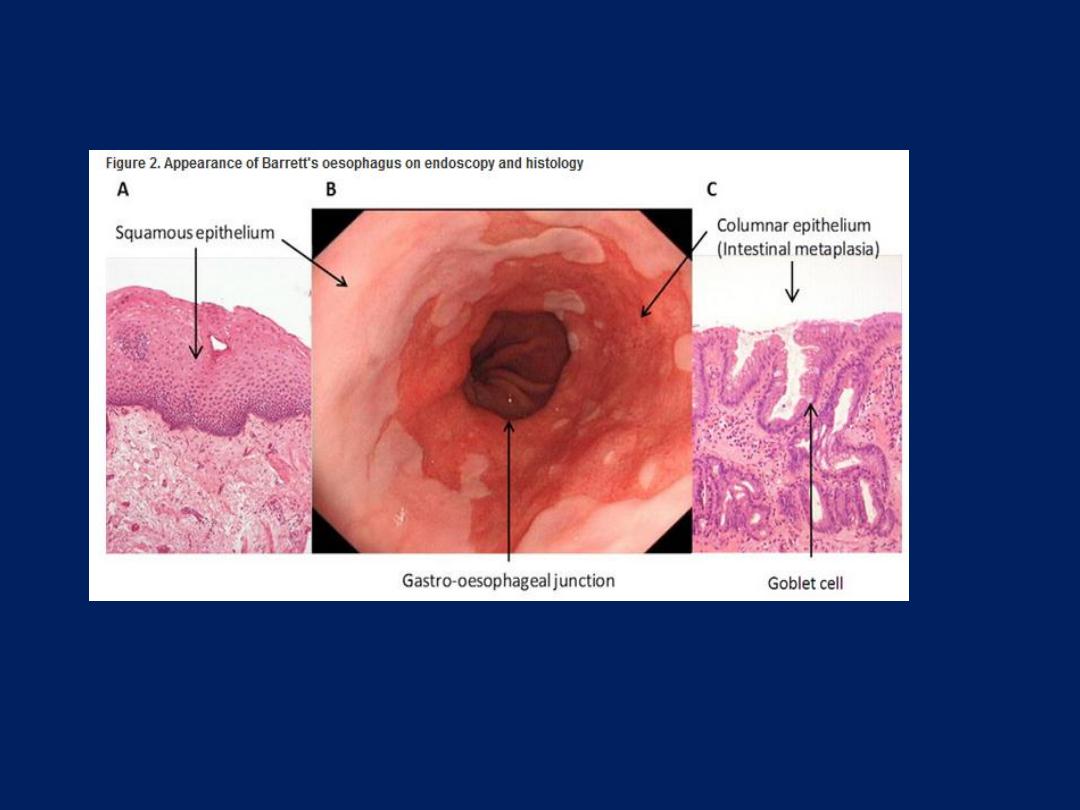
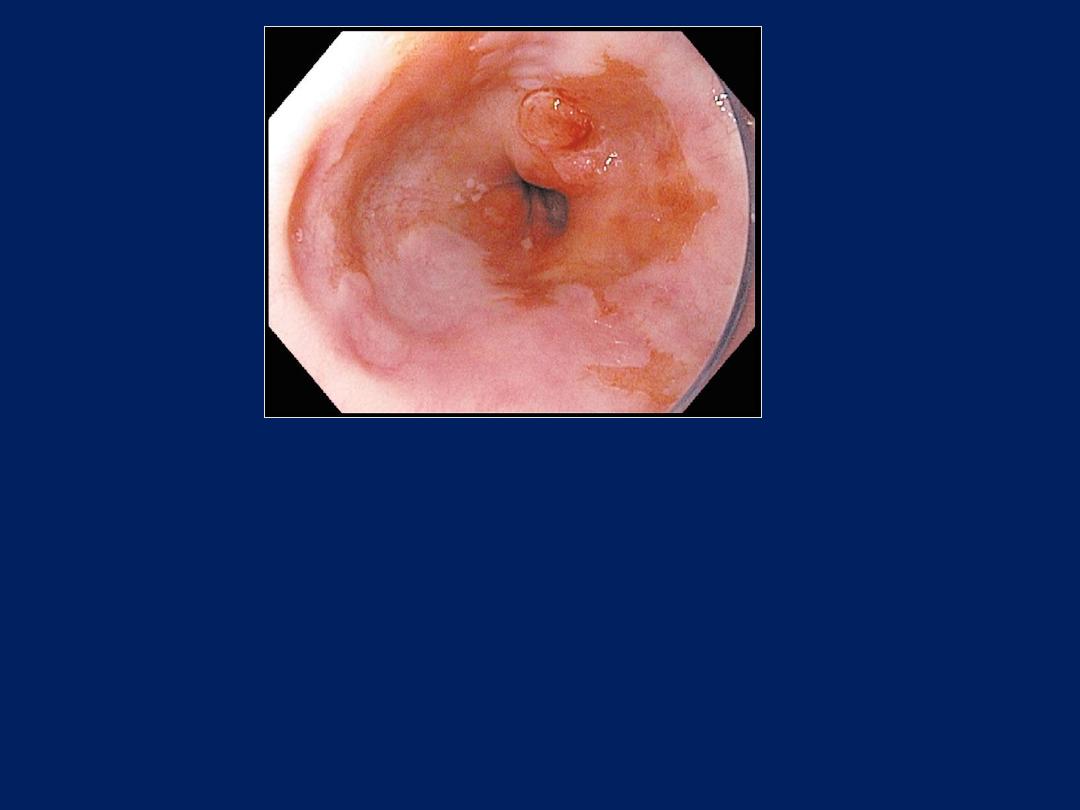
What is the most likely diagnosis for this finding detected
during esophageal endoscopy?
1. Adenocarcinoma
2. Candidiasis
3. Dieulafoy's lesion
4. Schatzki ring
5. Systemic sclerosis

Answer
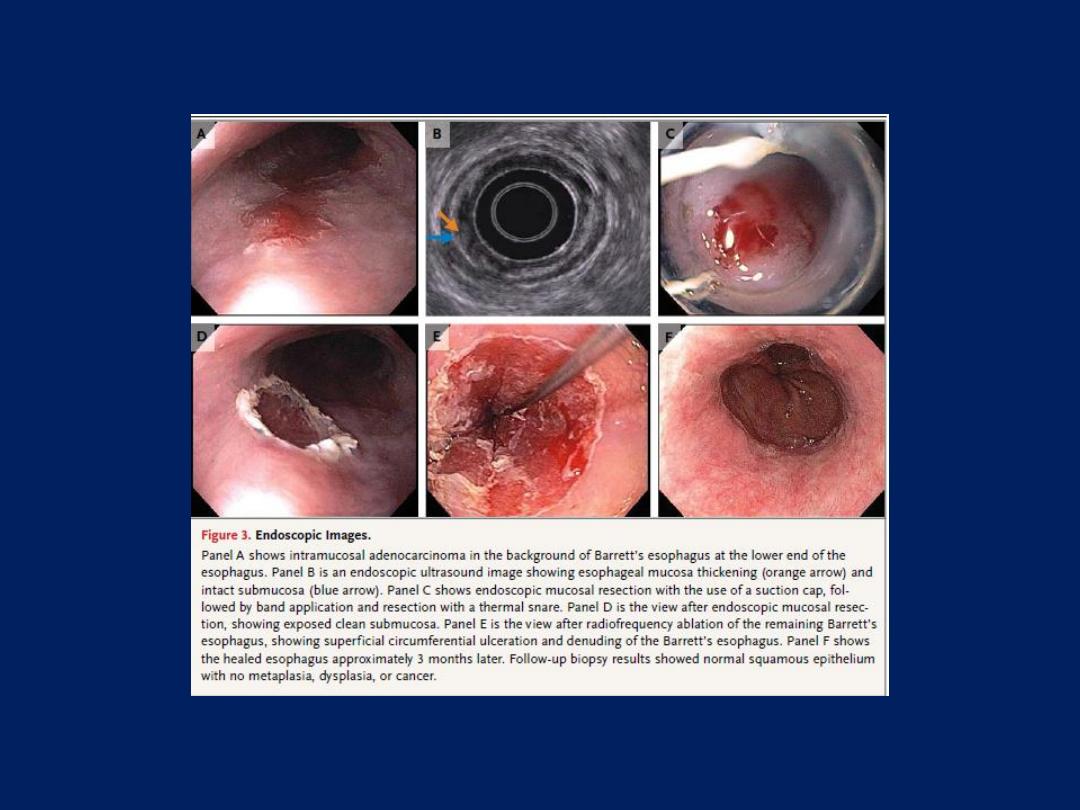
Adenocarcinoma
This nodular abnormality was found to be an
early adenocarcinoma in a patient with
Barrett's esophagus.

Esophageal candidiasis

Eye Exam
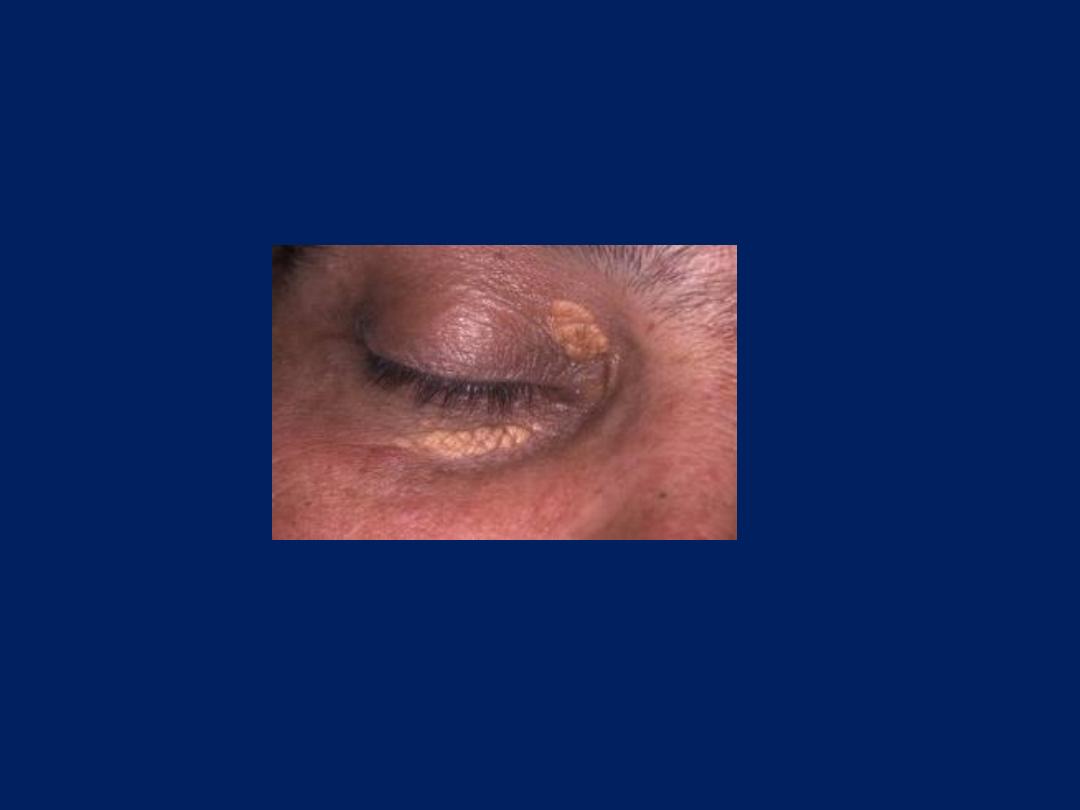
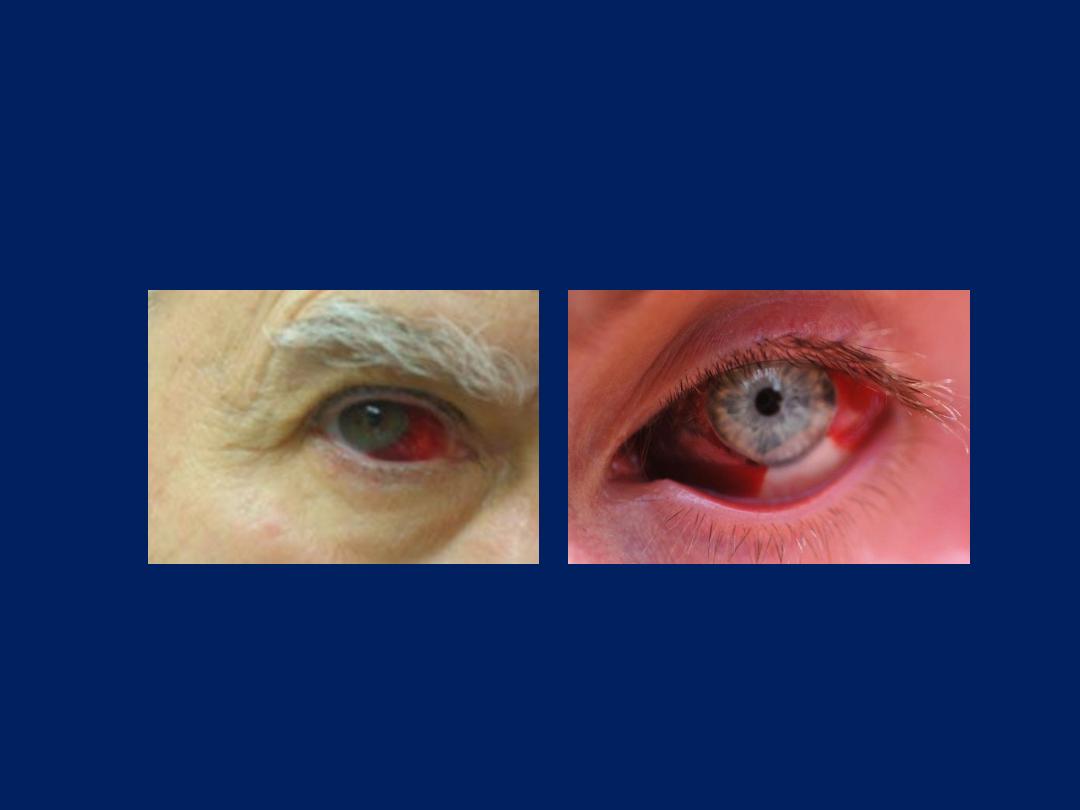
Polycythemia
Eye Exam
Puffiness
Eye Exam
Jaundice
Eye Exam
Xanthelasma

Eye Exam
Anemia

Eye Exam
Corneal arcus
Eye Exam
Subconjuctival hemorrhage

Eye Exam
Periorbital edema

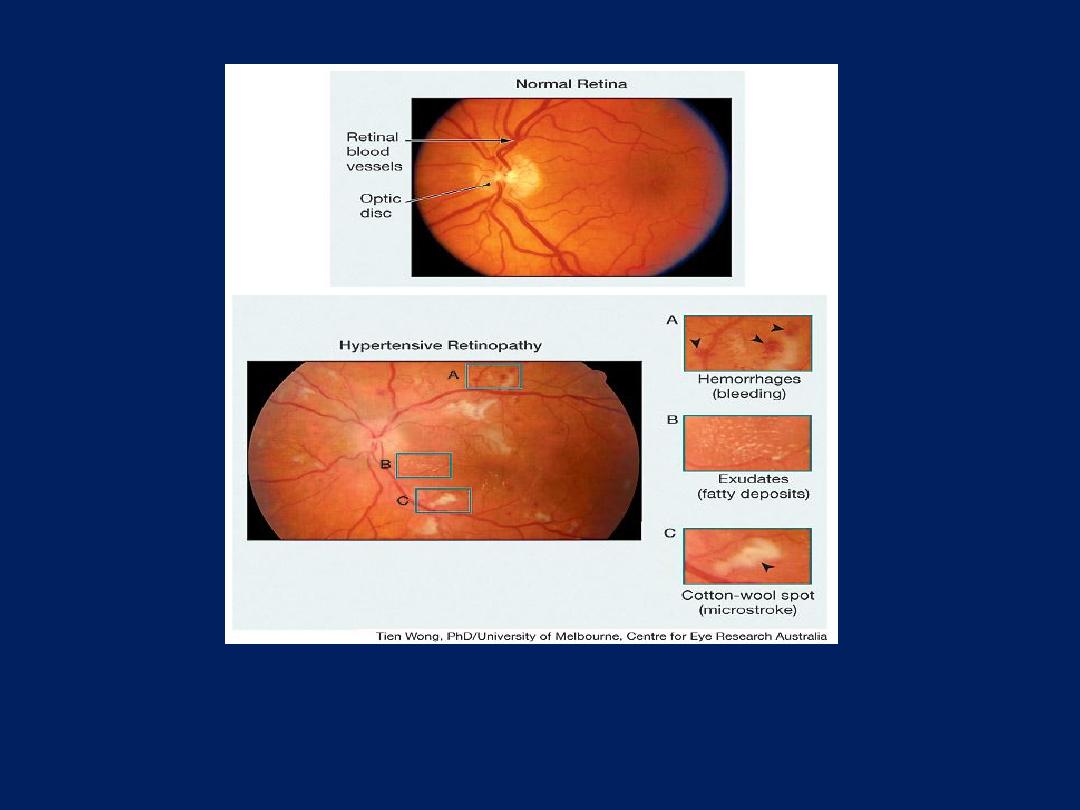
What is the diagnosis?
1. Cytomegalovirus retinitis
2. Roth spots
3. Central retinal vein
occlusion
4. Hypertensive retinopathy
5. Papilledema
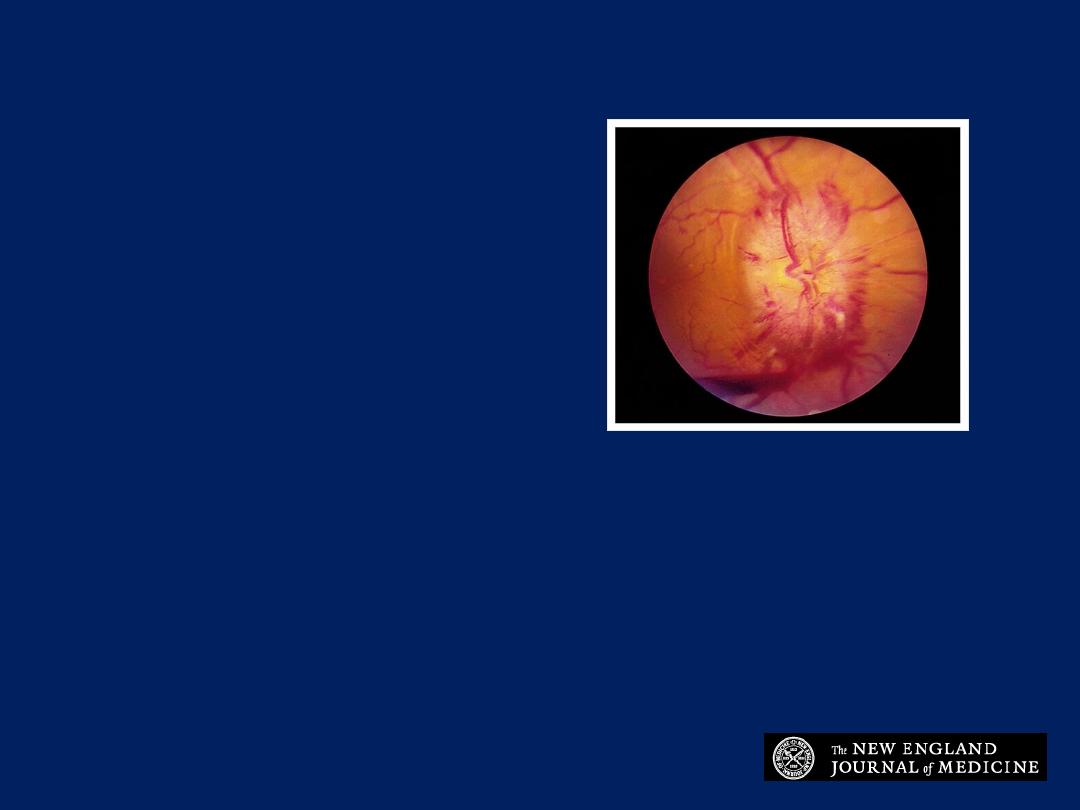
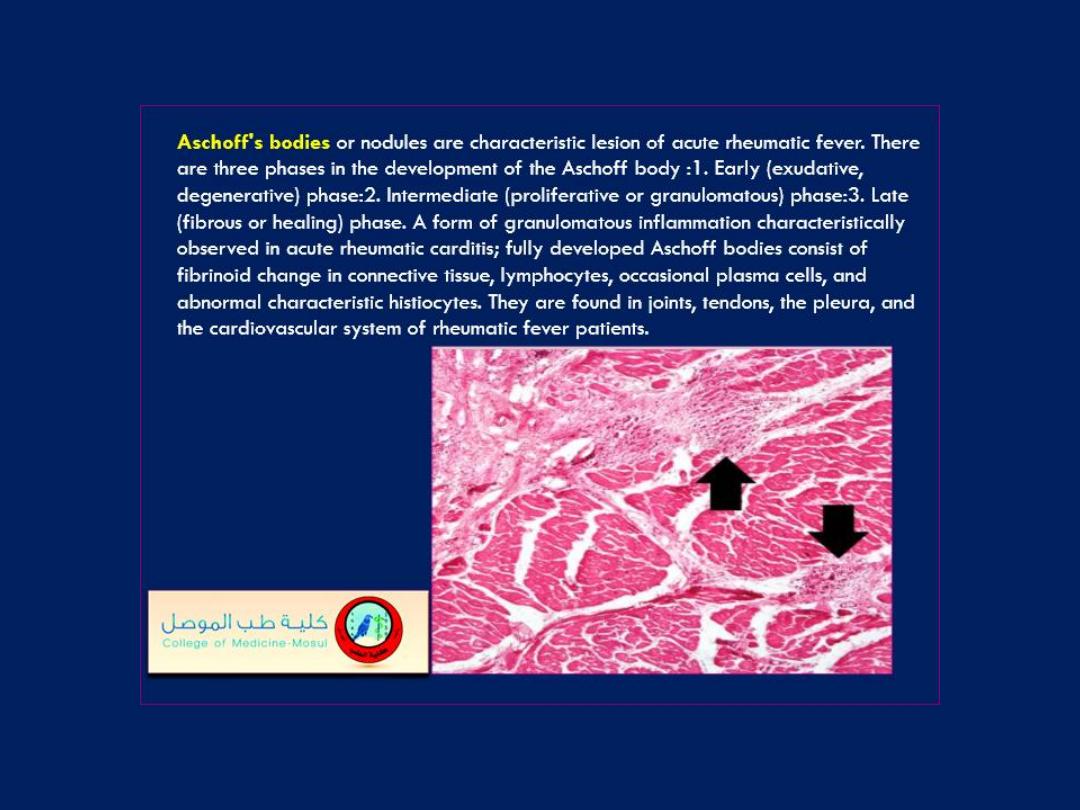
Papilledema
The fundoscopic image suggests florid papilledema.
What is the diagnosis?
1. Central retinal vein
occlusion
2. Profilerative diabetic
retinopathy
3. Hypertensive retinopathy
4. Chorioretinitis
5. Papilledema
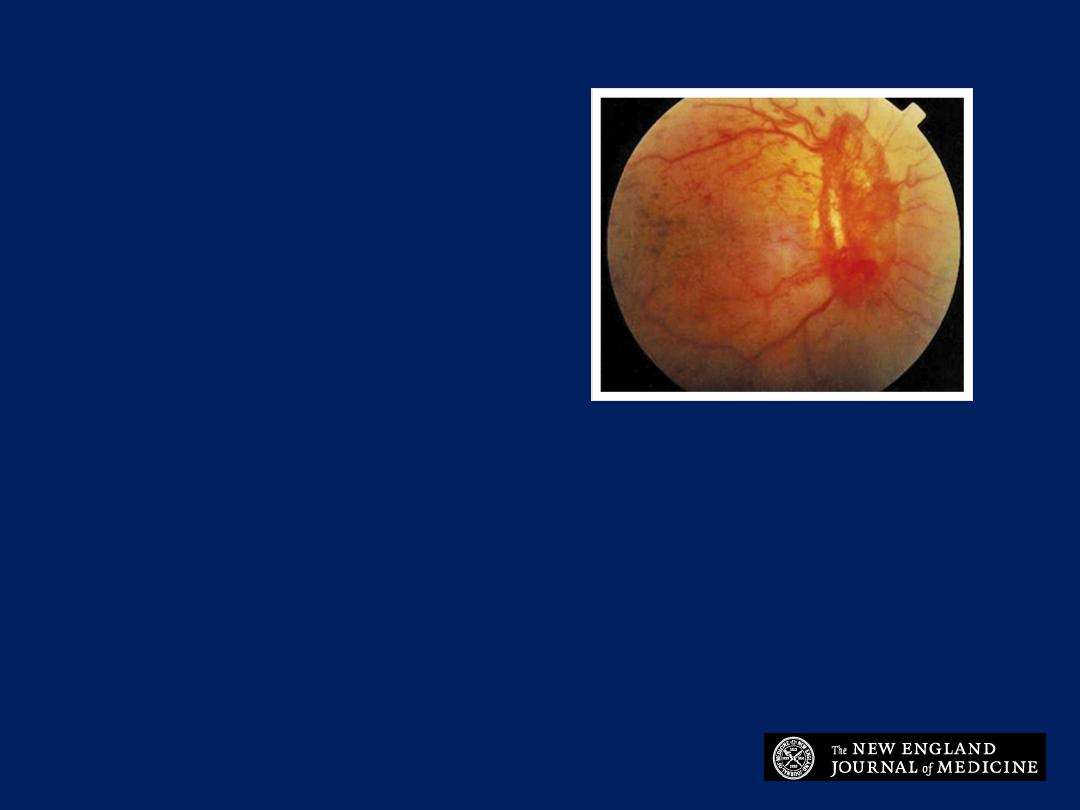
Profilerative diabetic retinopathy
Severe bilateral proliferative diabetic retinopathy with significant
optic-disk neovascularization is visible.

What is the diagnosis?
1. Central retinal artery occlusion
2. Diabetic papillopathy
3. Ocular toxoplasmosis
4. Optic neuritis
5. Malignant hypertension
This patient presented with
loss of vision. What is the
diagnosis?
1. Central retinal artery
occlusion
2. Diabetic retinopathy
3. Tay- Sach's disease
4. Hypertensive retinopathy
5. Papilledema
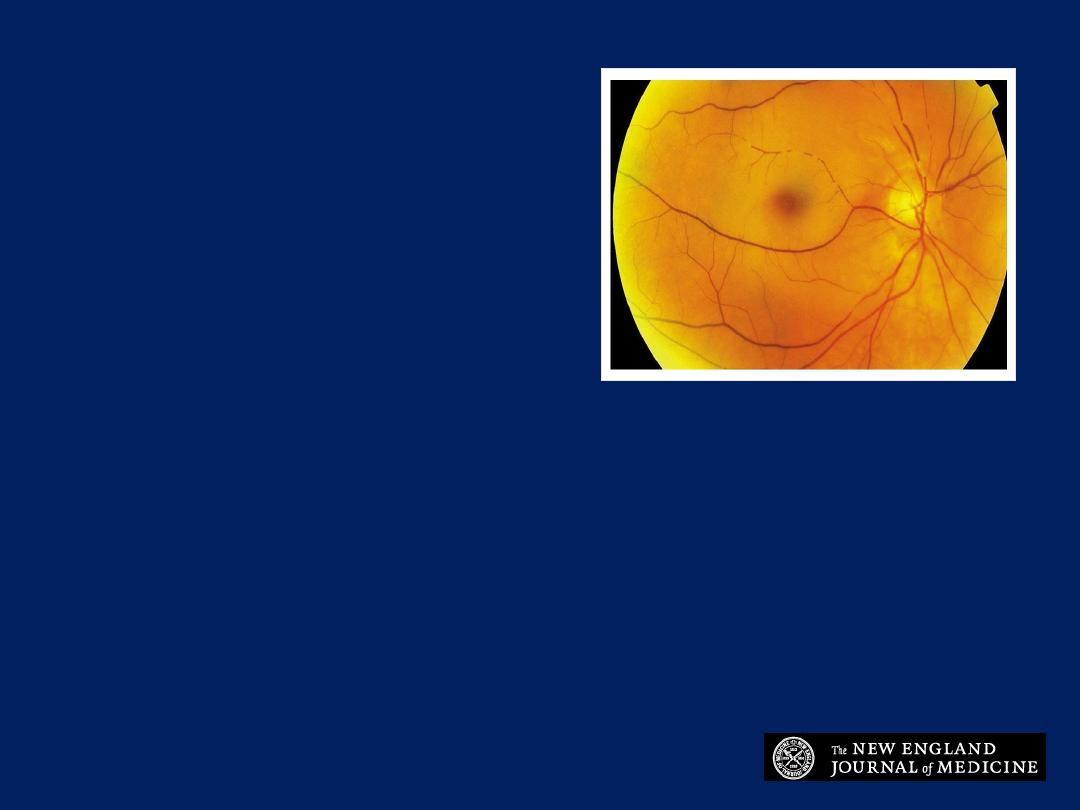
Central retinal artery occlusion
Diffuse retinal whitening, constriction of the arteriole and venule
with segmentation and a
cherry red spot
in the macula are most
consistent with central retinal artery occlusion.
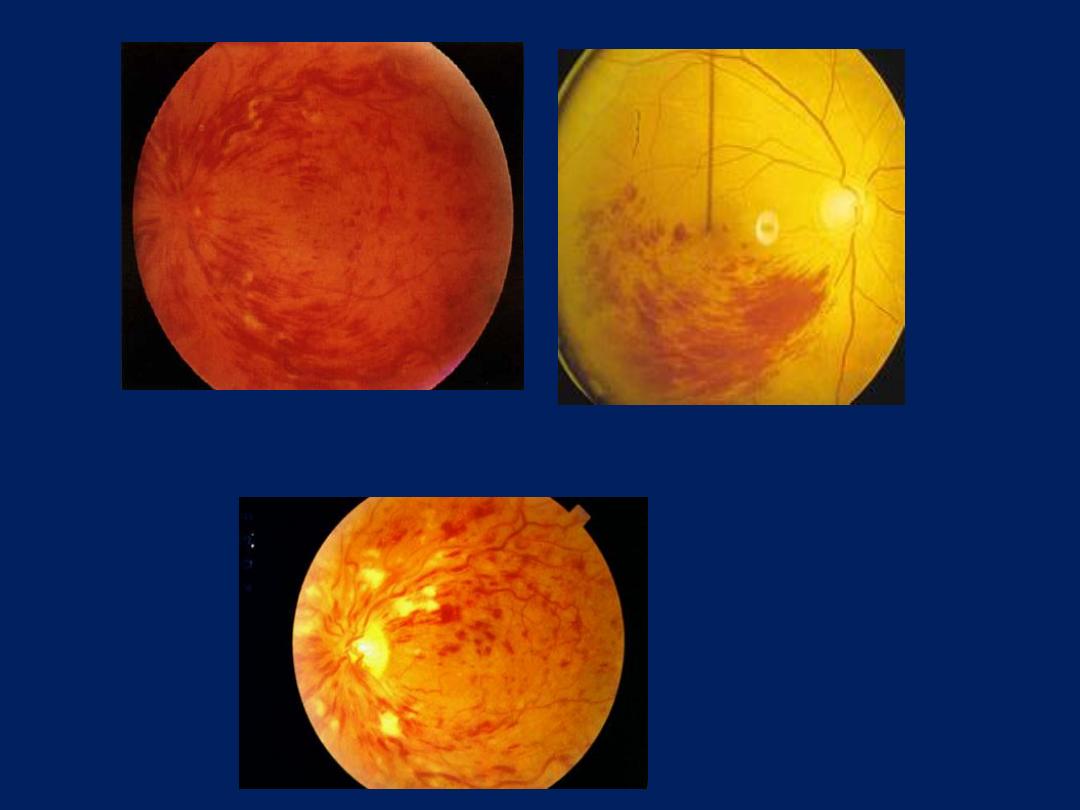
Central retinal vein occlusion
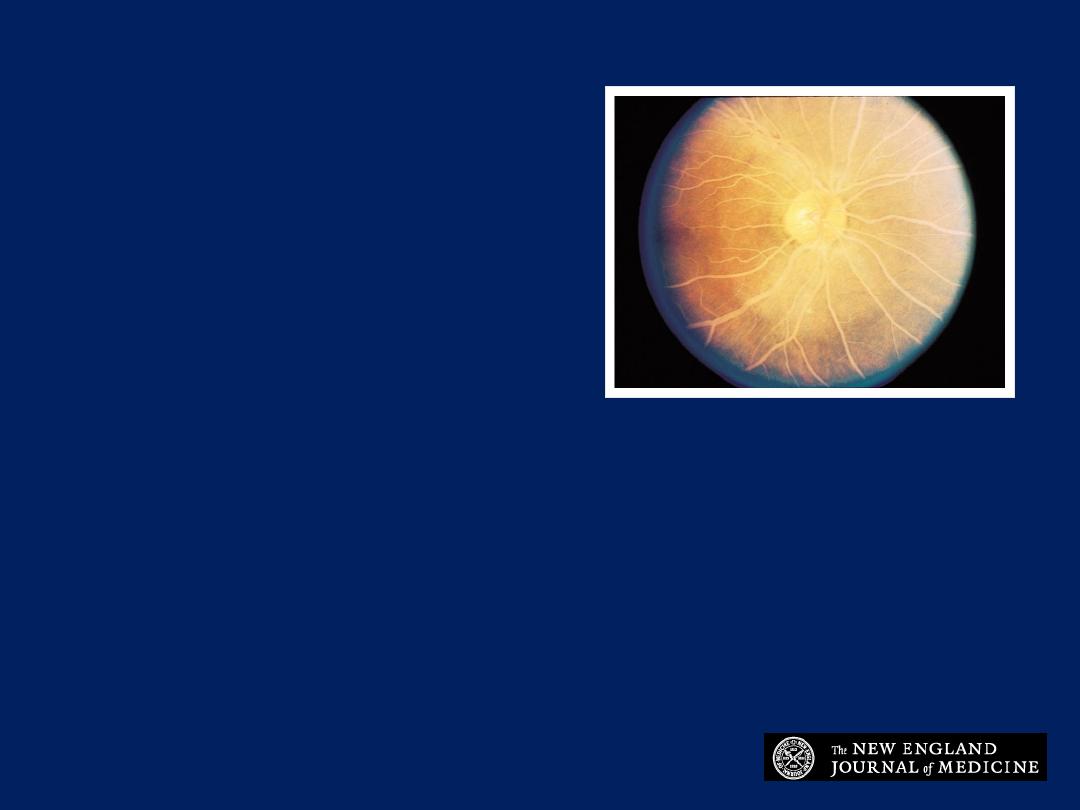
What is the diagnosis?
1. Hypertriglyceridemia
2. Hypertensive
retinopathy
3. Optic atrophy
4. Central retinal artery
occlusion
5. Cytomegalovirus retinitis
Hypertriglyceridemia
The creamy white vessels in the fundus resulted from
extreme hypertriglyceridemia.
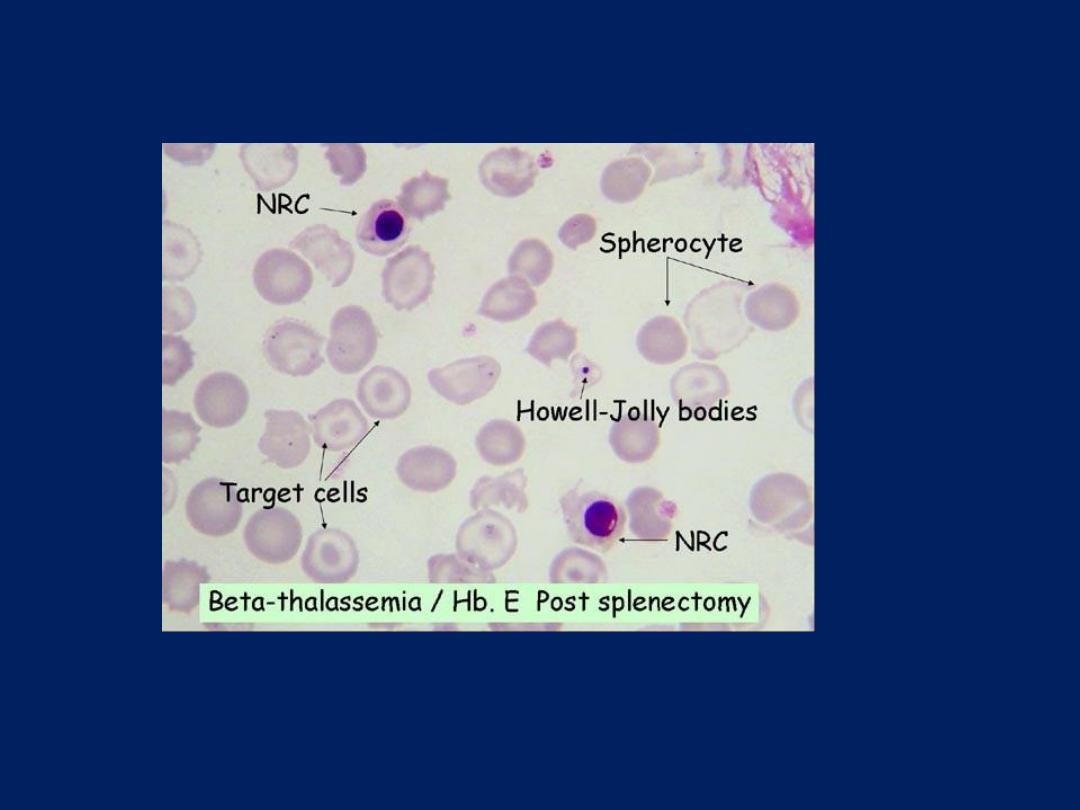
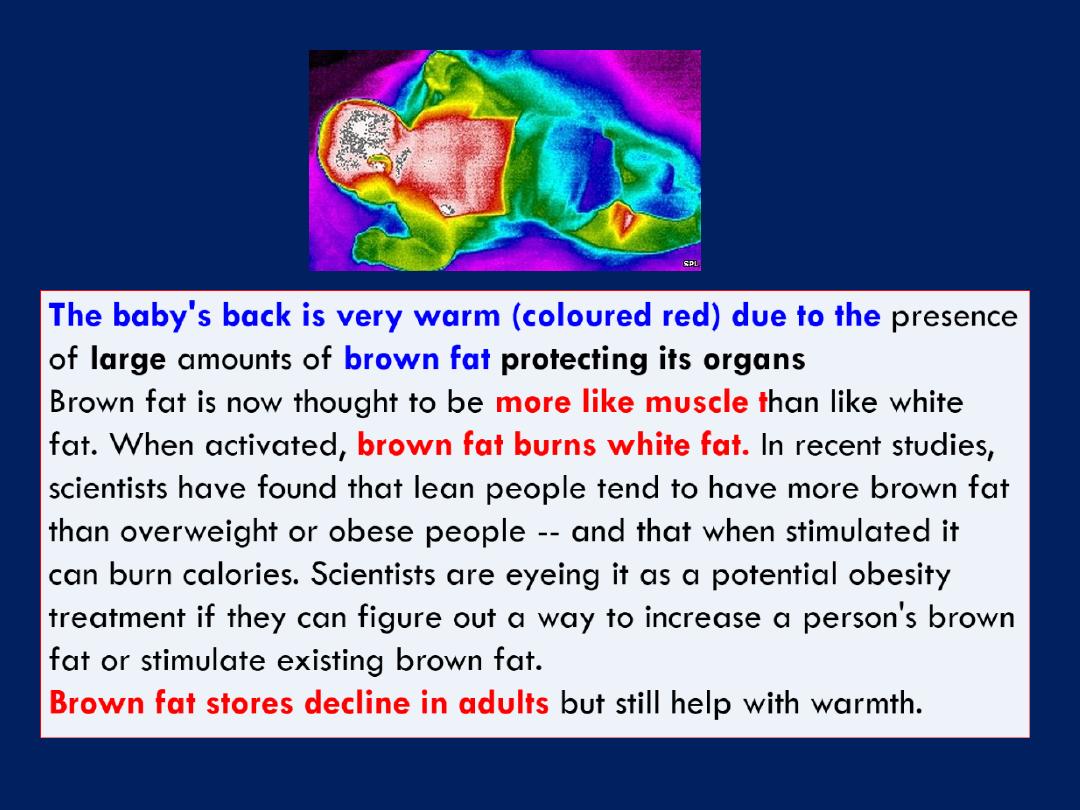
Howell-Jolly bodies
are little fragments of the red cell
nucleus, seen most commonly in patients with splenectomies,
hyposplenism or asplenia (normally, the spleen just bites
them out)and can be seen without a special stain - they
look like dark, round dots.
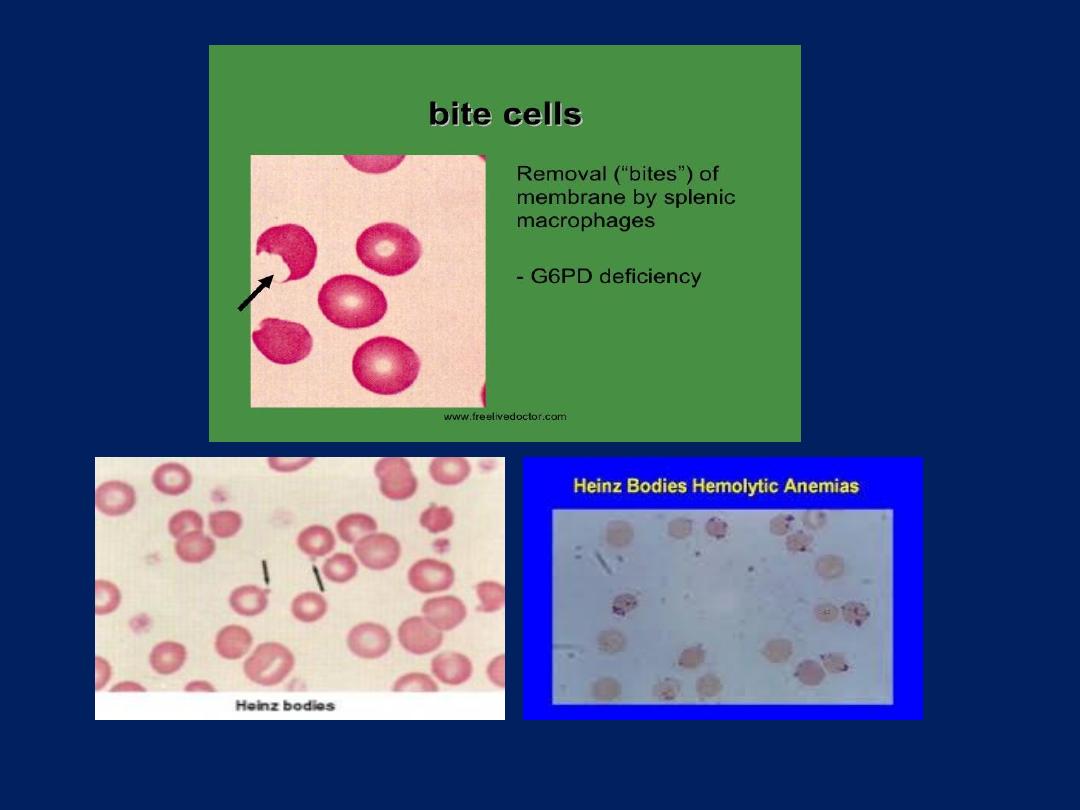
Heinz bodies seen in G6PD deficiency and Alpha
thalassemia chronic liver disease , hyposplenism or
asplenia.
They represent denatured globin chains, forming a little
ball that sticks to the inside of the red cell membrane. You
can't see it unless you do a special stain (like the supravital
stain). Macrophages in the spleen bite Heinz bodies out
(the resulting red cells are actually called bite cells!).
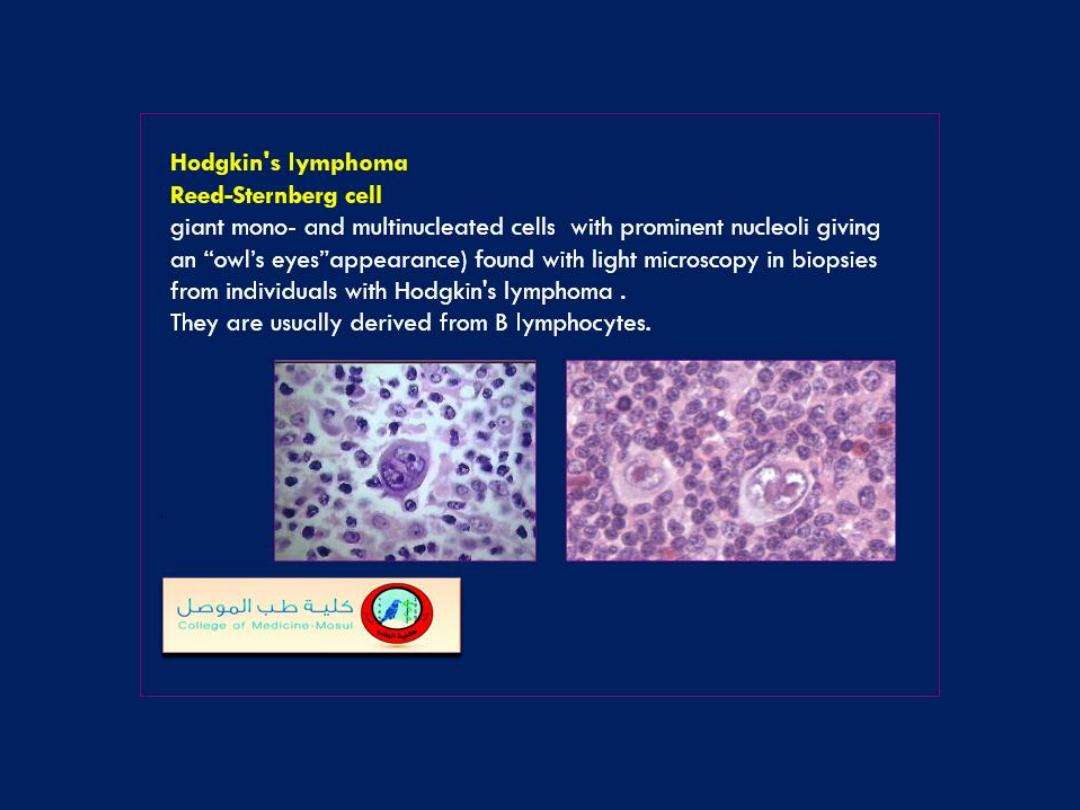
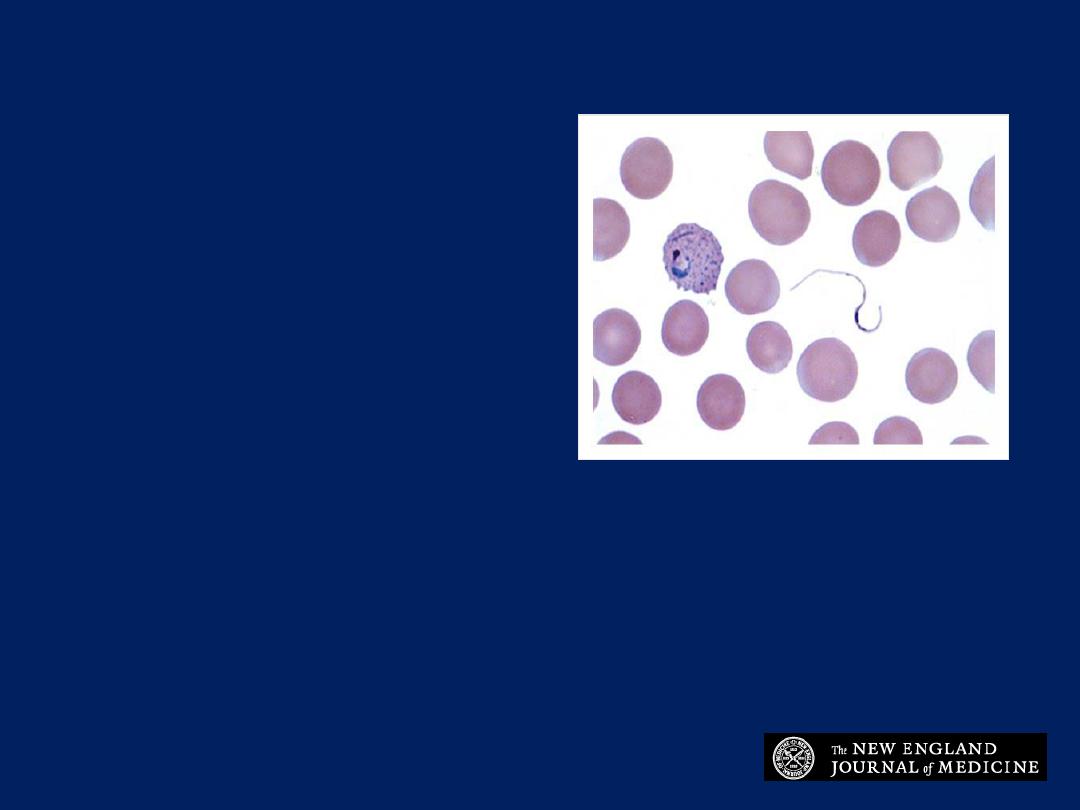
A 31-year-old woman
presented with fever
following a trip to Brazil.
What diagnosis is
suggested by the findings
on her blood smear?
1. Paracoccidioides
brasiliensis
2. Trypanozoma cruzi
3. Rickettsia typhi
4. Plasmodium vivax
5. Leishmania donovani
Plasmodium vivax
The presence of a ring form and basophilic
stippling within the red cell accompanied by
serpentine forms suggest Plasmodium vivax as
the responsible organism.

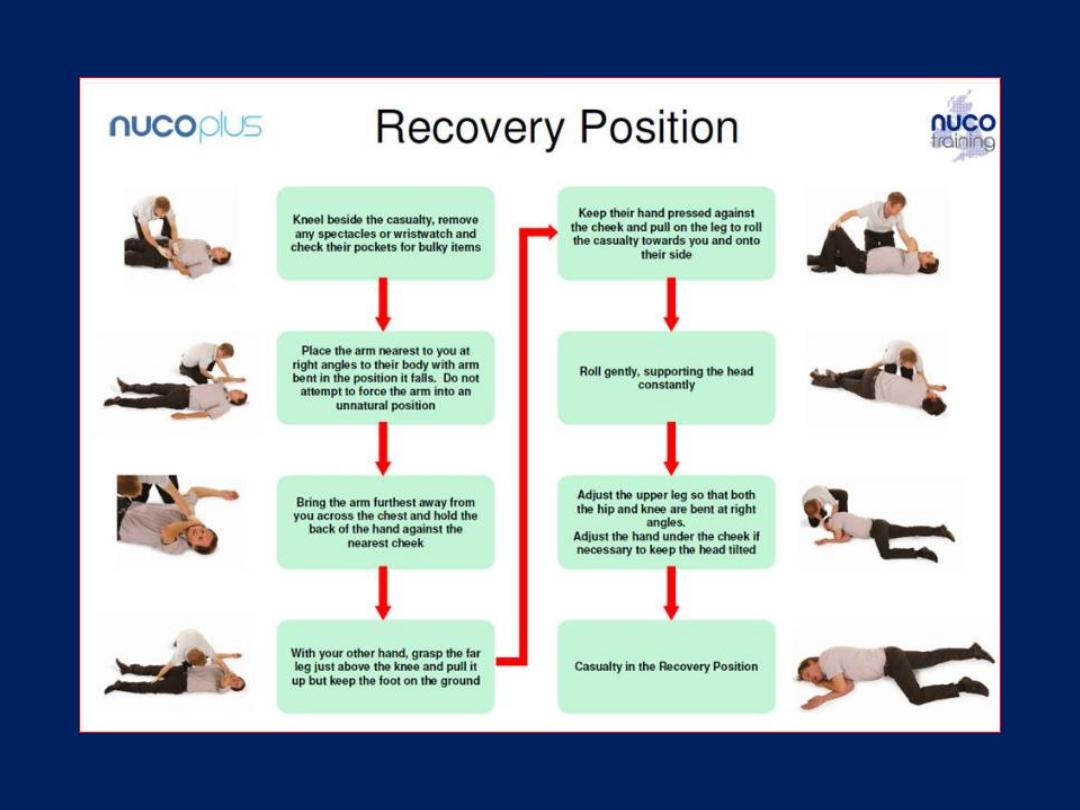
An unconscious casualty in the
recovery position
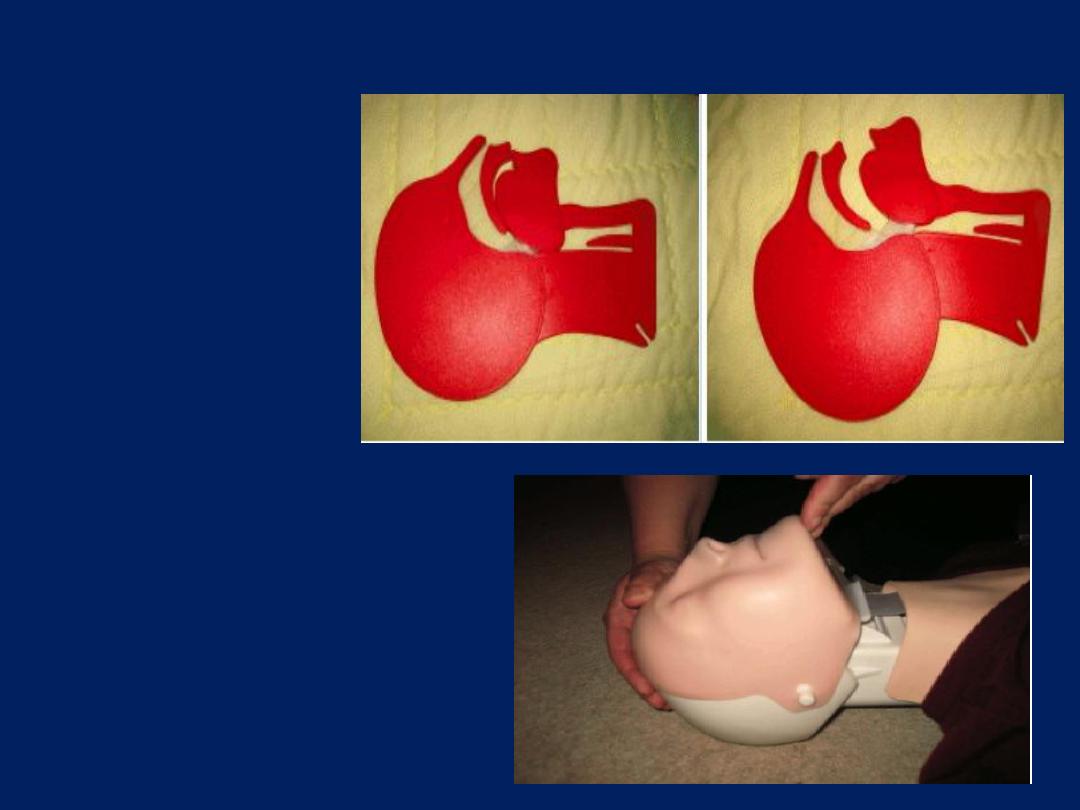
Figure a: Model
showing airway
obstruction in
unconscious
casualty
Figure b: Model
showing effect of
head tilt/chin lift on
casualty's airway
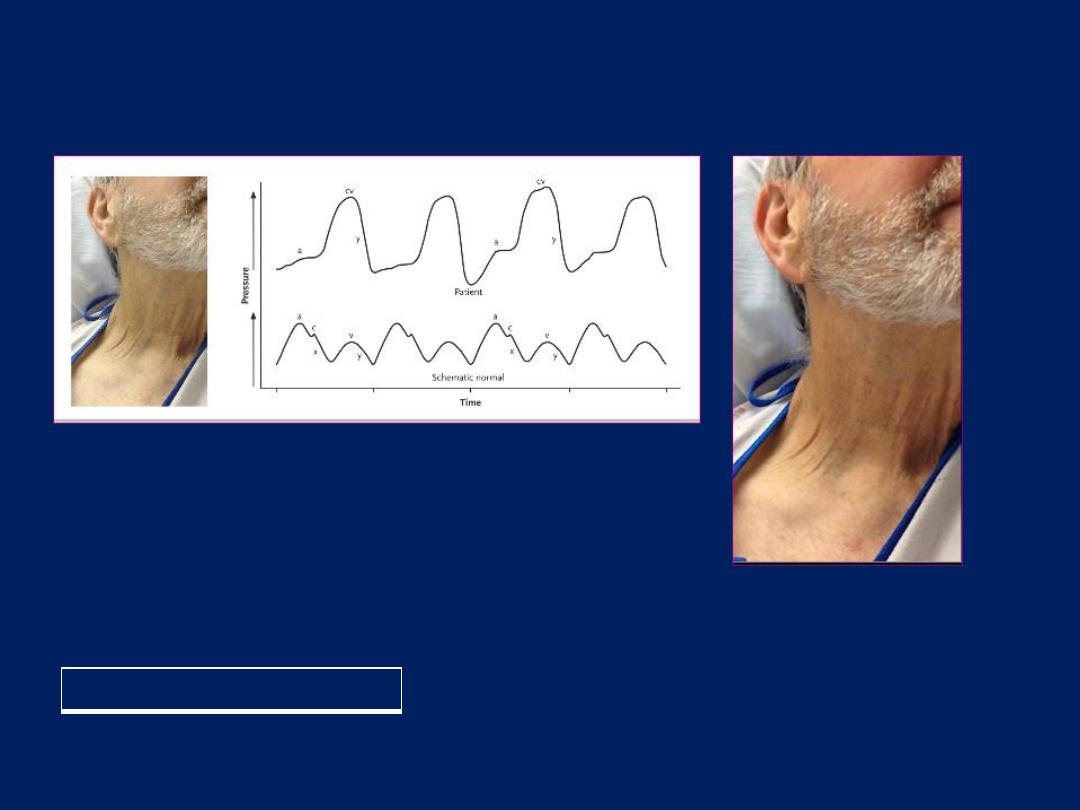
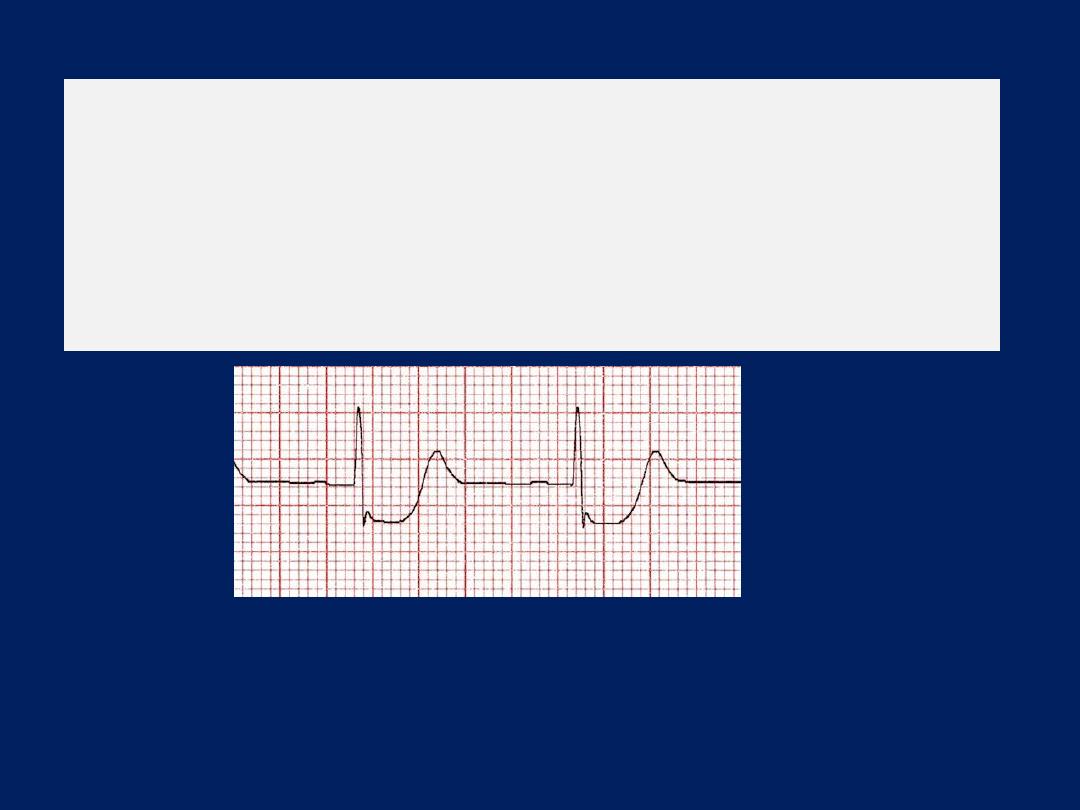
NEJM January , 2016
Lancisi’s sign
A 60-year-old man with nonischemic cardiomyopathy presented with progressive dyspnea
and weight gain of approximately 9 kg that had developed over a period of 2 to 3
weeks. On examination, a grade 2/6 holosystolic murmur that augmented with inspiration
was noted at the left lower sternal border. Examination of the neck revealed a palpable,
monomorphic venous pulsation, known as Lancisi’s sign (see video). Transthoracic
echocardiography revealed malcoaptation of the tricuspid-valve leaflets as a result of
annular dilatation, with resultant severe regurgitation.
Lancisi’s sign is a physical finding
of severe tricuspid regurgitation.
Normally, three peaks and two troughs characterize the
venous waveform (the lower strip is a generic representation of normal findings, for
comparison). The first peak, called the a wave, results from atrial contraction during late
diastole. Next, during early systole, isovolumetric ventricular contraction triggers closure of
the tricuspid valve, producing the c wave. In mid-systole, given a competent tricuspid valve,
a combination of atrial relaxation and descent of the atrial floor during ventricular
contraction results in the x descent. The third peak, the v wave, occurs as a result of atrial
filling during late systole. Finally, passive ventricular filling in early diastole produces the y
descent. In the context of tricuspid regurgitation, retrograde blood flow into the right
atrium during ventricular systole results in loss of the x descent (the upper strip shows the
right atrial pressure tracing from this patient), creating a fused cv wave that appears as a
large pulsation within the internal jugular vein that is often palpable. This wave is typically
followed by an augmented y descent, which is the consequence of an increased pressure
gradient between the right atrium and right ventricle. In this patient, diuretic agents were
used to normalize the volume status, and the symptoms abated.
N Engl J Med 2016
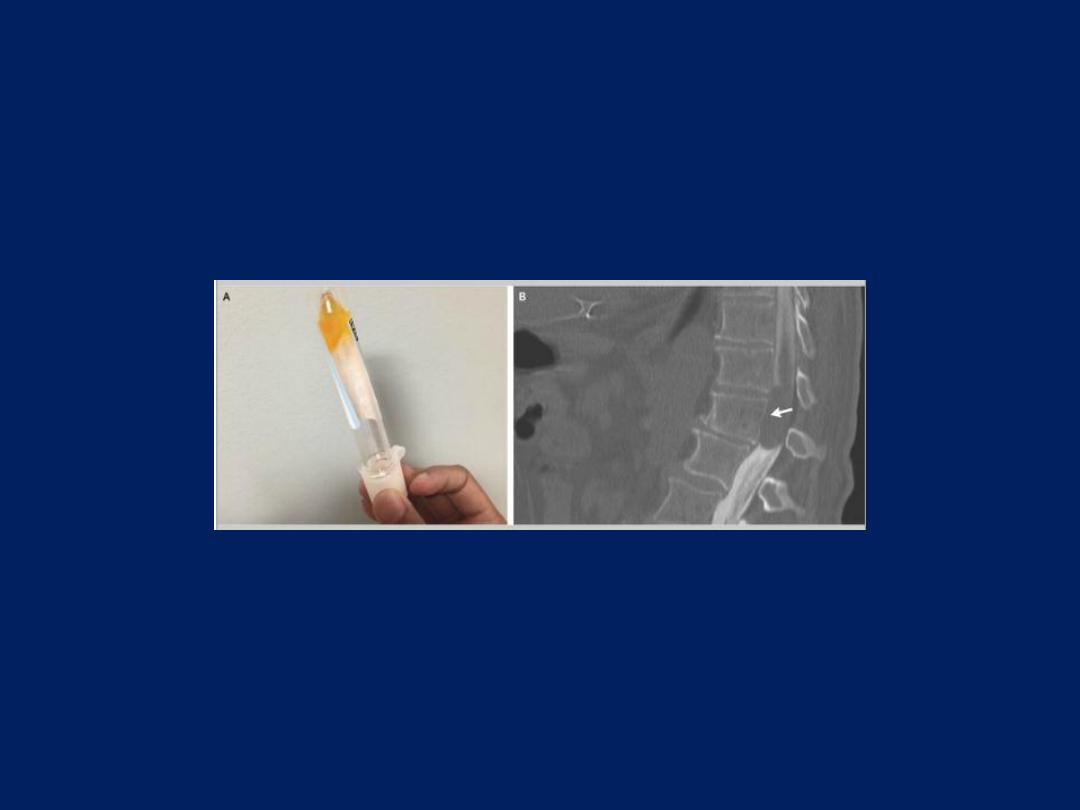
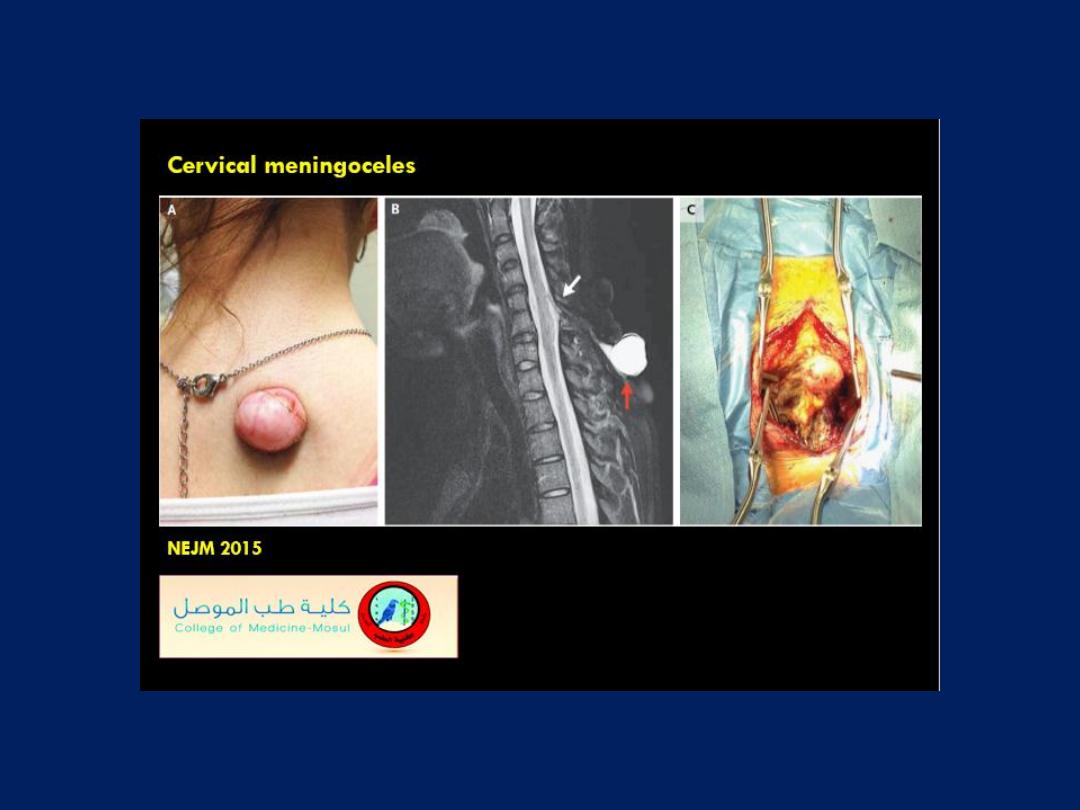
Froin’s Syndrome
A 64-year-old man presented with a 1-week history of progressive bilateral
weakness in the legs. The neurologic examination showed paralysis of the legs
and decreased sensation starting at the L1–L2 level. Magnetic resonance
imaging could not be performed owing to the presence of a pacemaker. Since
the patient had atrial fibrillation and an elevated prothrombin time, there was
concern about a possible spinal hematoma. Computed tomography (CT) of the
spine showed only degenerative disk disease. On lumbar puncture, the
cerebrospinal fluid (CSF) was xanthochromic, viscous, and coagulated in the tube
(Panel A). The protein level in the CSF was more than 1500 mg per deciliter, and
the glucose level was 45 mg per deciliter (2.5 mmol per liter). The CSF
contained less than one nucleated cell per cubic millimeter, and the results of
Gram’s staining and cultures were negative. The combination of elevated
protein, xanthochromia, and hypercoagulation of CSF is pathognomonic for
Froin’s syndrome,
which can occur with blockage of CSF flow by a spinal cord
mass or with meningeal irritation from meningitis. CT myelography showed a
large intradural, extramedullary lesion at T11–T12 (Panel B, arrow), which was
compressing the spinal cord. The patient underwent total laminectomy of T11
and T12 and partial laminectomy of L1 with tumor resection; a benign nerve-
sheath tumor (schwannoma) was diagnosed on pathological analysis. No
radiotherapy or chemotherapy was performed. After 1 month of rehabilitation,
the patient had improved sensation but continued having leg paralysis.
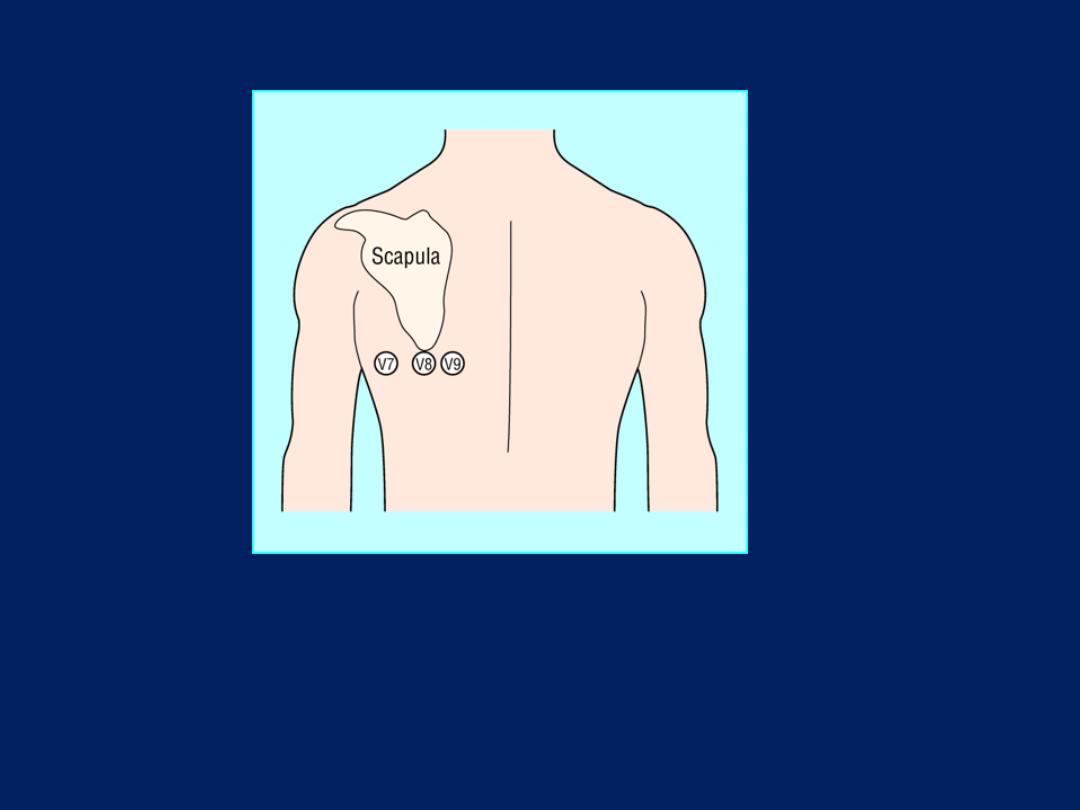
V7 – Left posterior axillary line, in the same horizontal plane as V6.
V8 – Tip of the left scapula, in the same horizontal plane as V6.
V9 – Left paraspinal region, in the same horizontal plane as V6.
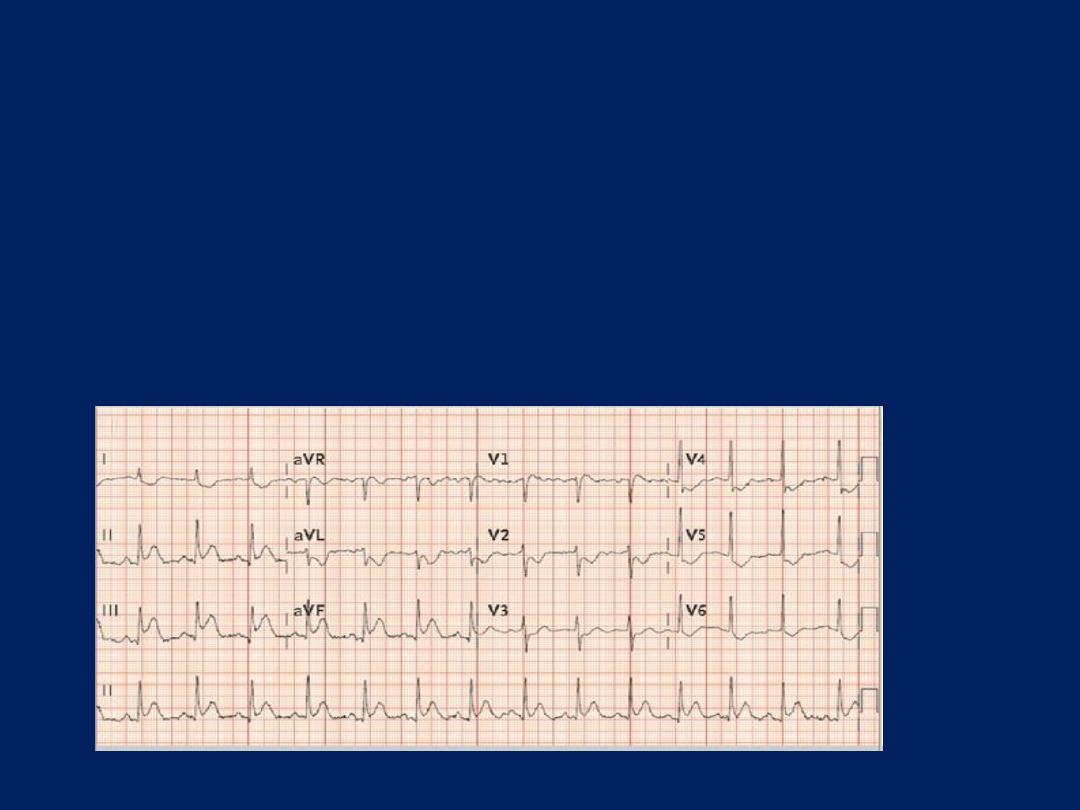
Posterior Myocardial Infarction
Clinical Significance
Posterior infarction accompanies 15-20% of STEMIs,
usually occurring in the context of an inferior or lateral
infarction.
Isolated posterior MI is less common (3-11% of infarcts).
Posterior extension of an inferior or lateral infarct implies
a much larger area of myocardial damage, with an
increased risk of left ventricular dysfunction and death.
Isolated posterior infarction is an indication for emergent
coronary reperfusion. However, the lack of obvious ST
elevation means that the diagnosis is often missed.
Posterior MI is suggested by the following changes in V1-3:
1. Horizontal ST depression
2. Tall, broad R waves (>30ms)
3. Upright T waves
4. Dominant R wave (R/S ratio > 1) in V2
Posterior infarction is confirmed by the
presence of ST elevation and Q waves in the
posterior leads (V7-9).
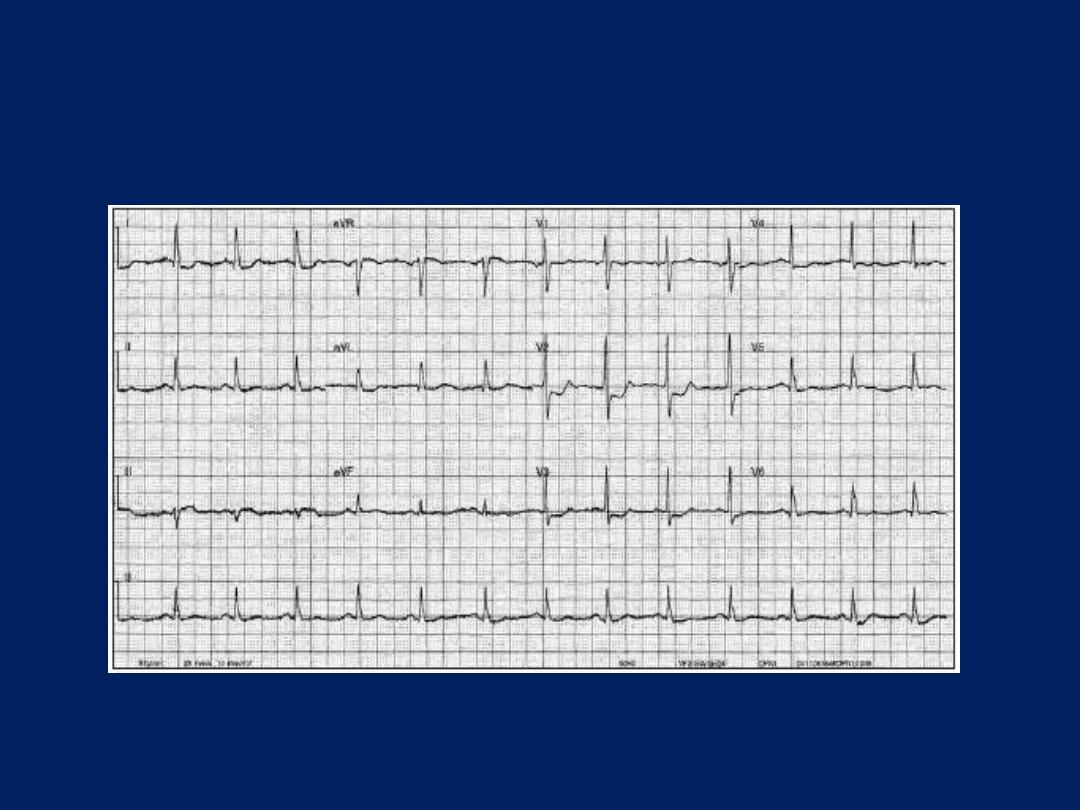
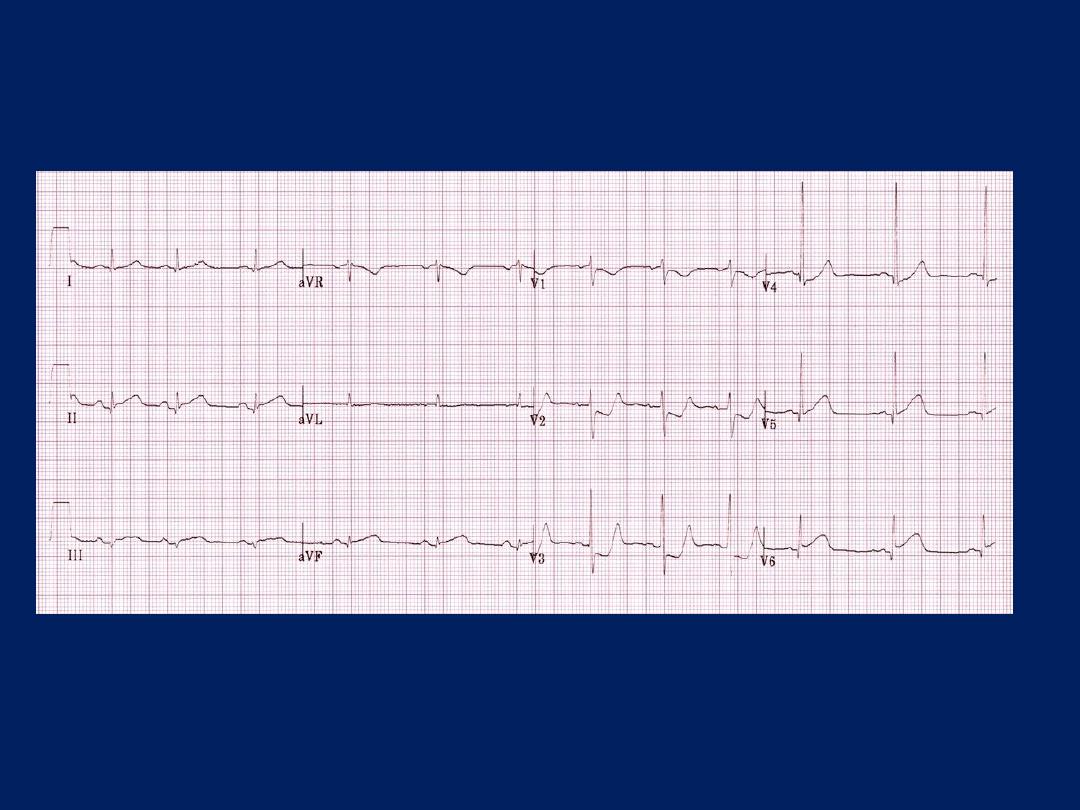
Posterior MI
What is the most likely diagnosis in a man with chest
pain, hypotension, dizziness, and this ECG finding?
1. Cardiac tamponade
2. Left ventricle rupture
3. Right ventricle aneurysm
4. Right coronary artery occlusion
5. Left anterior descending artery occlusion
Answer
Right coronary artery occlusion
Right coronary artery occlusion is the correct answer. The
ECG shows ST-segment elevation in leads II, III, aVF, and
V1, which is concerning for inferior wall and right ventricle
involvement. Right ventricular infarction should be suspected
when ST-segment elevation is seen in leads V1-V2, and an
ECG with right-sided precordial leads should be
performed. The right ventricle and the inferior wall of the
heart are typically supplied by the right coronary artery.
The right ventricle
i
s
a thin
-walled chamber that functions at
low oxygen
demands
and pressure. It is
perfused throughout
the cardiac cycle in both systole and diastole, and its ability to
extract oxygen is increased during hemodynamic stress. All of
these factors make the right ventricle less susceptible to
infarction than the left ventricle.
Patients with right ventricular infarctions associated with
inferior infarctions have much higher rates of significant
hypotension, bradycardia requiring pacing support, and in-
hospital mortality than isolated inferior infarctions.
Isolated right ventricular infarct is extremely rare and may
be
interpreted erroneously as left ventricular anteroseptal
infarction because of ST-segment elevation in leads V1 -V4,
usually is noted in association with inferior MI , the incidence of
right ventricular infarction in such cases ranges from 10-50%.
All patients with inferior wall
myocardial infarction should have
a right-sided ECG.
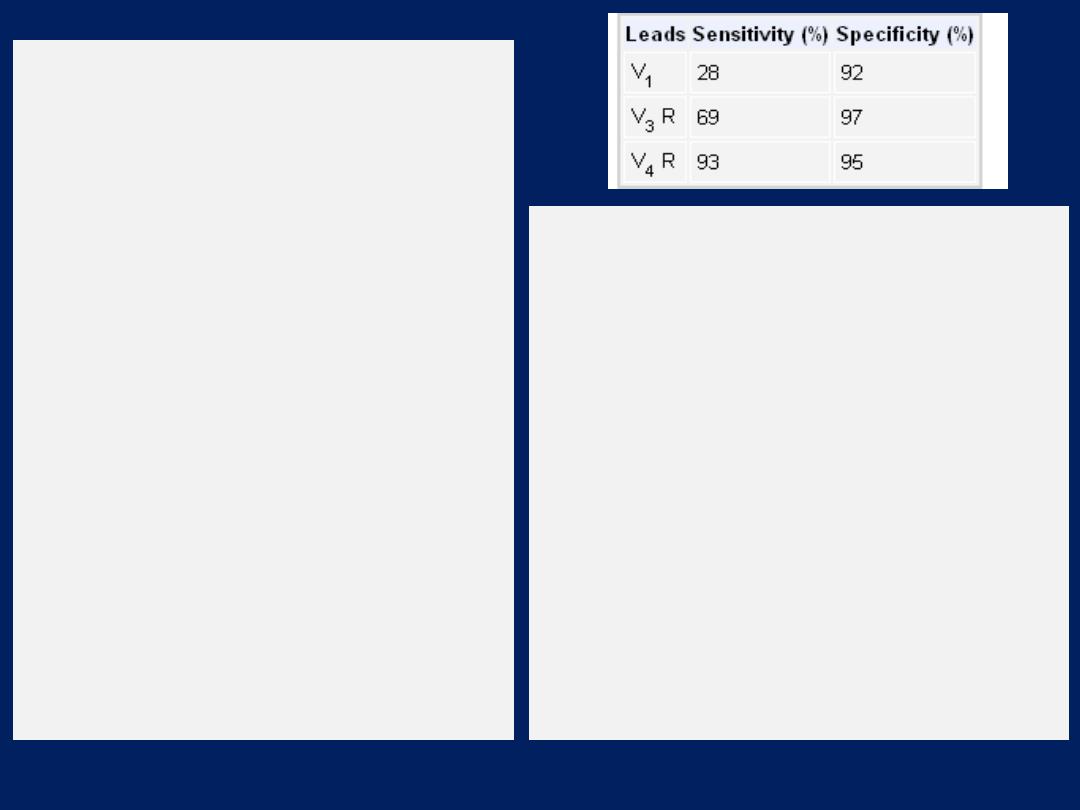
ST-segment
elevation in lead V4R is the single
most powerful predictor of right
ventricular involvement, identifying
a high-risk subset of patients in the
setting of inferior wall myocardial
infarction. The ST-segment elevation
is transient, disappearing in less
than 10 hours following its onset in
half of patients. The following table
demonstrates the sensitivity and
specificity of more than 1 mm of ST-
segment elevation in V1, V3 R, and
V4 R. Sensitivity and Specificity of
more than 1 mm of ST-Segment
Elevation in V1, V3 R, and V4 R
The classic clinical triad of right
ventricular infarction
includes
distended neck veins, clear lung
fields, and hypotension.
Infrequent clinical manifestations
include right ventricular third and
fourth heart sounds, audible at the
left lower sternal border and
increase with inspiration.
On hemodynamic monitoring,
disproportionate elevation of right-
sided filling pressures compared
with left-sided hemodynamics
represents the hallmark of right
ventricular infarction
Hemodynamic monitoring
Disproportionate elevation of right-sided filling
pressures when compared with left-sided
hemodynamics represents the hallmark of right
ventricular infarction.
Increase in venous
or right atrial pressure with
inspiration
(ie, Kussmaul sign)
Exaggeration
of the normal inspiratory decline in
systemic arterial pressure
(ie, pulsus paradoxus)
Echocardiography is useful as a modality to rule out
pericardial disease and tamponade, which are the
major differential diagnoses in the setting of a right
ventricular infarction.
Trapezius ridge
How does acute pericarditis present clinically, and
what are the diagnostic criteria?
Chest pain
is the presenting symptom in virtually all
patients. Although the differential diagnosis of chest
pain is extensive, certain features point strongly to
pericarditis, especially pleuritic pain that is relieved by
sitting forward and that
radiates to the trapezius ridge
(the bottom portion of scapula on the back) (the latter
feature is virtually
pathognomonic
).
The diagnosis of acute pericarditis is established when a
patient has at least two of the following symptoms or
signs: chest pain consistent with pericarditis, pericardial
friction rub, typical ECG changes, or a pericardial
effusion.
Because the rub and ECG findings may be transient,
frequent auscultation and ECG recordings can be
helpful in establishing the diagnosis.
NEJM December 18, 2014
Typical EKG changes in acute pericarditis includes
stage 1 -- diffuse, positive, ST elevations with
reciprocal ST depression in aVR and V1. Elevation of
PR segment in aVR and depression of PR in other
leads especially left heart V5, V6 leads indicates
atrial injury.
stage 2 -- normalization of ST and PR deviations
stage 3 -- diffuse T wave inversions (may not be
present in all patients)
stage 4 -- EKG becomes normal OR T waves may be
indefinitely inverted.
Coronary artery dominance
The artery that supplies the posterior descending
artery (PDA) . determines the coronary
dominance. If the posterior descending artery is
supplied by the right coronary artery (RCA), then
the coronary circulation can be classified as
"right-dominant".
If supplied by the circumflex artery (CX), a branch
of the left artery, then the coronary circulation can
be classified as
"left-dominant".

If the PDA is supplied by both RCA and the CX
artery, then the coronary circulation can be
classified as "co-dominant".
Approximately 70% of the general population are
right-dominant, 20% are co-dominant, and 10%
are left-dominant. A precise anatomic definition of
dominance would be the artery which gives off
supply to the AV node i.e. the AV nodal artery.
Most of the time this is the right coronary artery.



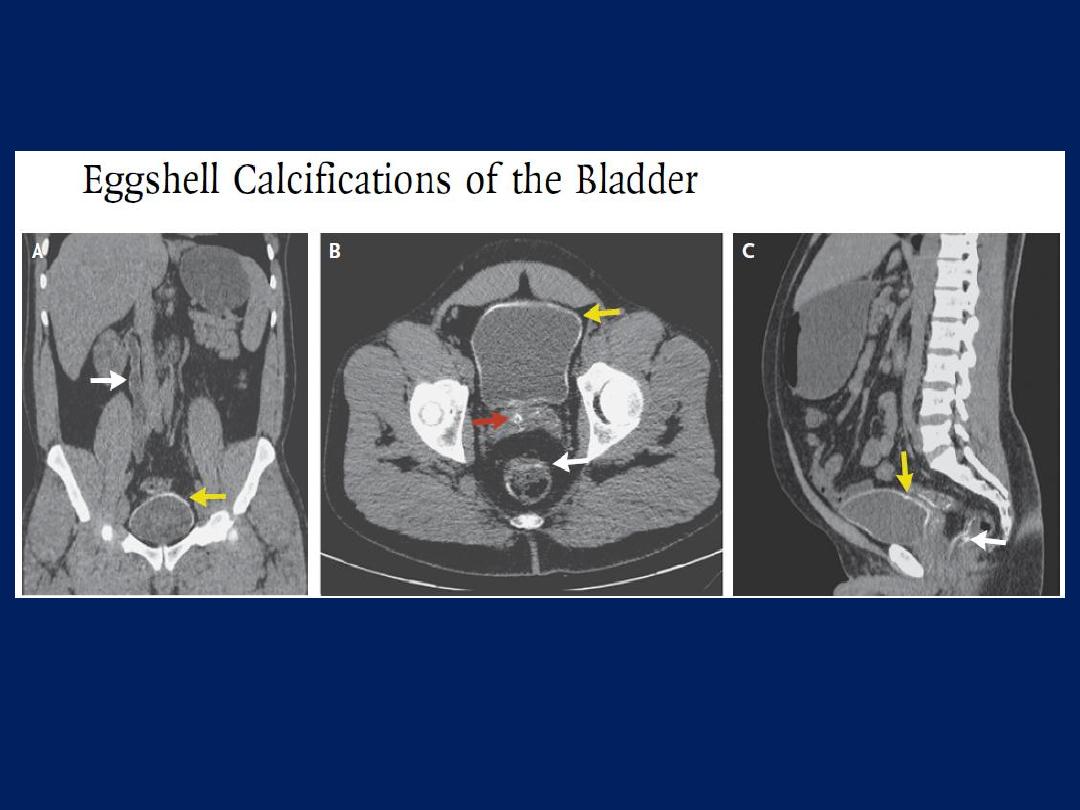
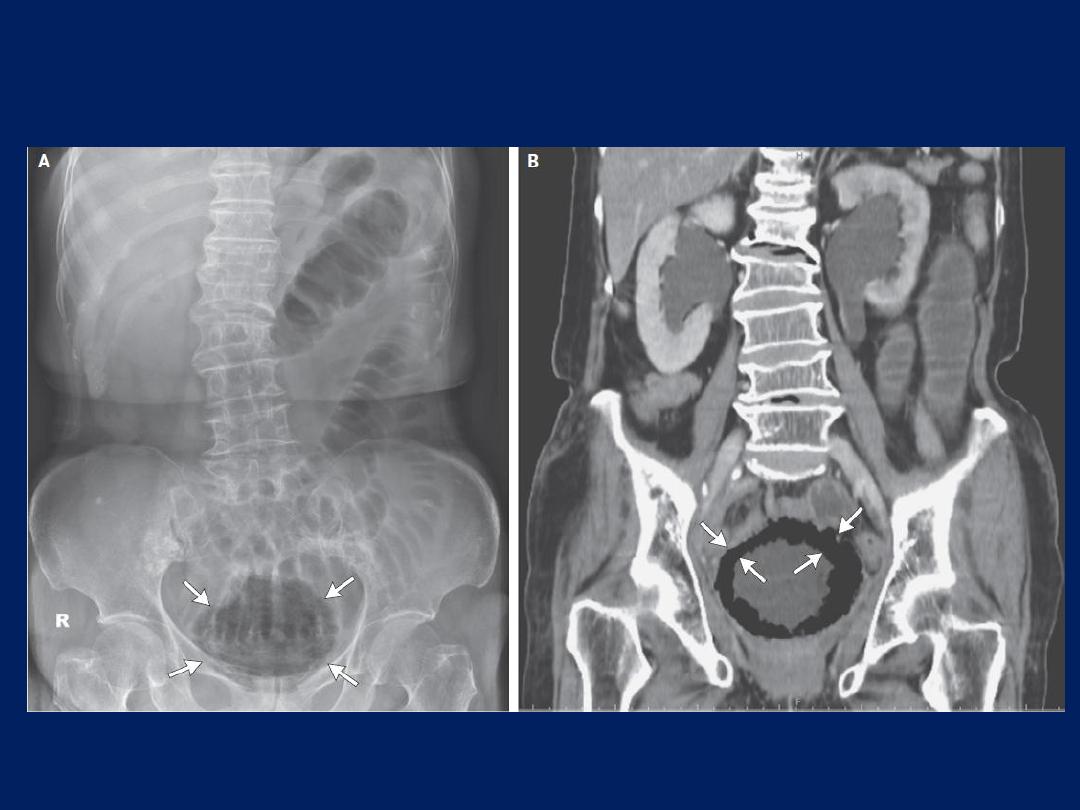
Eggshell Calcifications of the Bladder
A 43-year-old man presented with a 1-month history of dysuria and
intermittent hematuria.
Similar episodes had occurred several times in the 6
months preceding presentation, along with episodes of rectal bleeding.
The physical examination was unremarkable. Laboratory investigations revealed
an elevated albumin:creatinine ratio (96 mg of albumin per millimole of
creatinine), with dysmorphic red cells in the urine. Two urine cultures were sterile.
A serum schistosoma antibody titer was 1:256. Renal ultrasonography
revealed mild hydroureteronephrosis.
CT of the abdomen and pelvis without contrast revealed hydroureteronephrosis
of the right ureter and kidney, with faint mural calcification of the ureter (Panel
A, white arrow) and smooth mural calcification of the bladder (Panels A, B, and
C, yellow arrows). There was also calcification of the seminal vesicles (Panel B,
red arrow) and the wall of the rectosigmoid bowel (Panels B and C, white
arrows). This pattern of calcification is typical of chronic genitourinary and
gastrointestinal schistosomiasis,
in which the larvae of the schistosoma parasite are deposited on the walls of
the organs and become calcified. Diagnosis is based on a history of exposure
along with a strong clinical suspicion of infection and the characteristic
radiographic findings. Tuberculosis may also cause calcification of the
bladder wall and should be considered in the differential diagnosis.
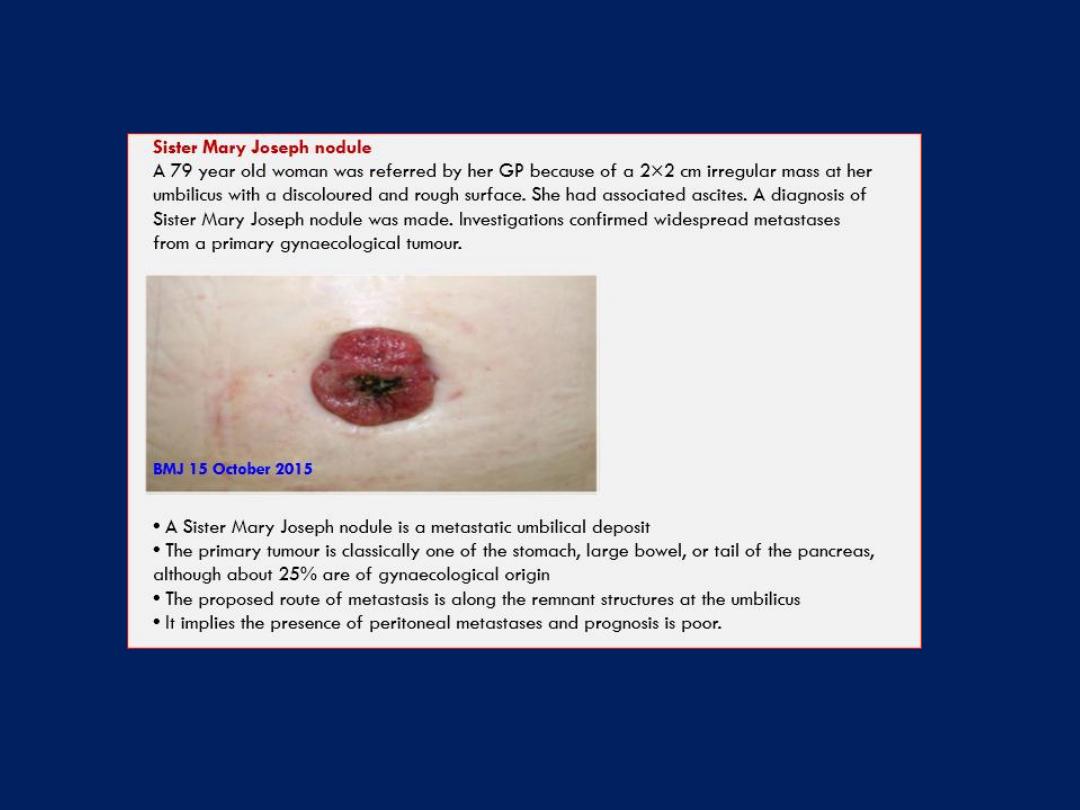
A supraclavicular swelling
BMJ 6 May 2016
A supraclavicular swelling
A 63 year old man presented with a longstanding right sided
supraclavicular mass that had recently increased in size .
Clinical examination suggested a giant lipoma (>5 cm), although
a liposarcoma could not be excluded. The mass was excised
and histological examination confirmed a giant lipoma. His
recovery was uneventful. Liposarcomas are the most common
soft tissue sarcoma, often seen in men during the fourth to sixth
decade. Liposarcomatous change in an existing giant lipoma is
rare (<0.1%) but documented.
A sudden increase in
size,
change in
consistency,
onset of
pain,
or
development of
lymphadenopathy
should prompt urgent referral
to exclude malignancy. First line treatment is surgery with close
follow-up because metastasis can occur in certain subtypes.
BMJ 6 May 2016
The radiograph shows
extensive calcification of the
intervertebral ligaments,
bilateral ossification of the
outer layer of the annulus
fibrosis (forming bony
bridges called marginal
syndesmophytes), and
apophyseal joint ankyloses
all gave the appearance of
a bamboo spine.
This is most
consistent with a diagnosis of
ankylosing spondylitis.
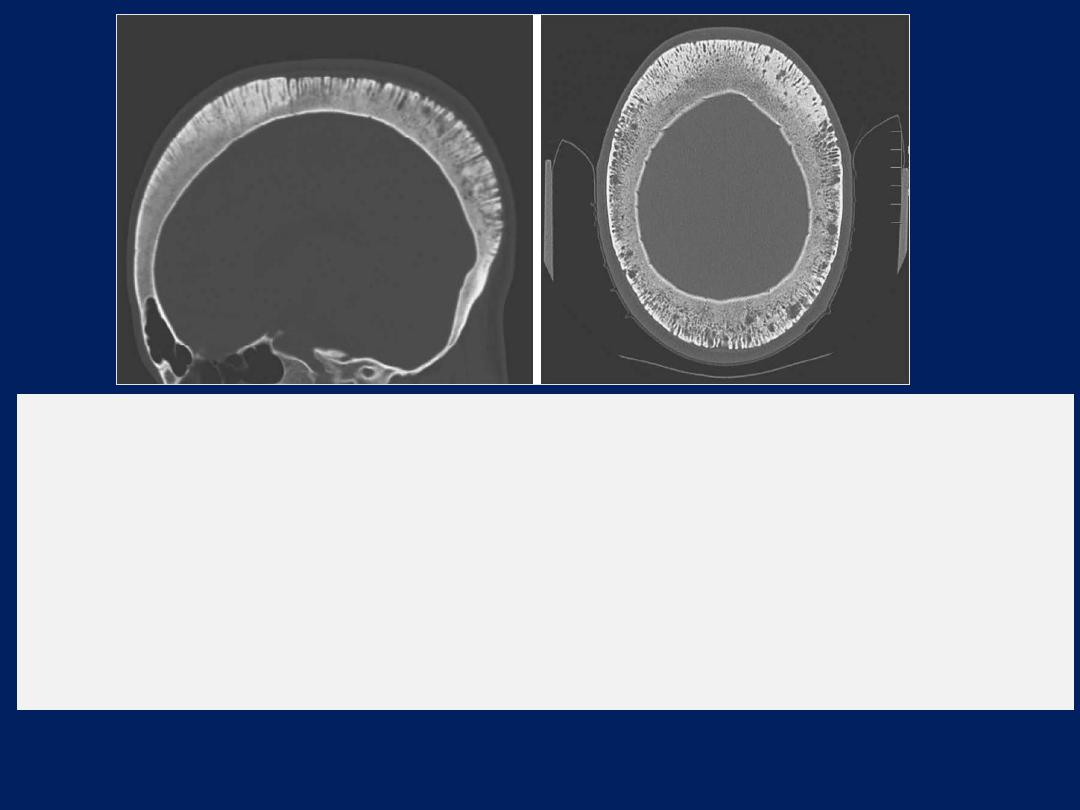
The non-contrast CT of the head
shows a thickened calvaria with
perpendicular proliferation of the trabeculae, a finding termed the
hair-on-end sign.
These skull changes are a result of red marrow
proliferation leading to alternating thickened and opaque trabeculae
with radiolucent marrow hyperplasia. This finding can be seen in the
context of hemolytic anemias, such as sickle cell disease, thalassemia
major, and glucose-6-phosphate dehydrogenase deficiency.
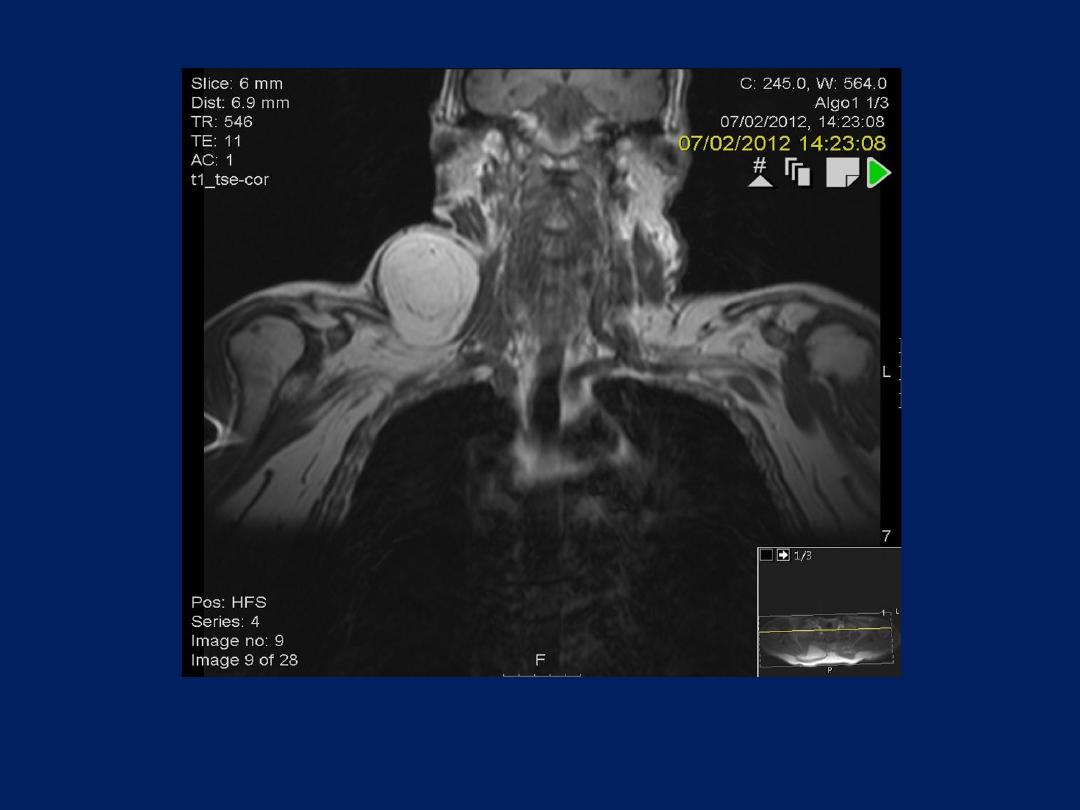
NEJM May, 2016
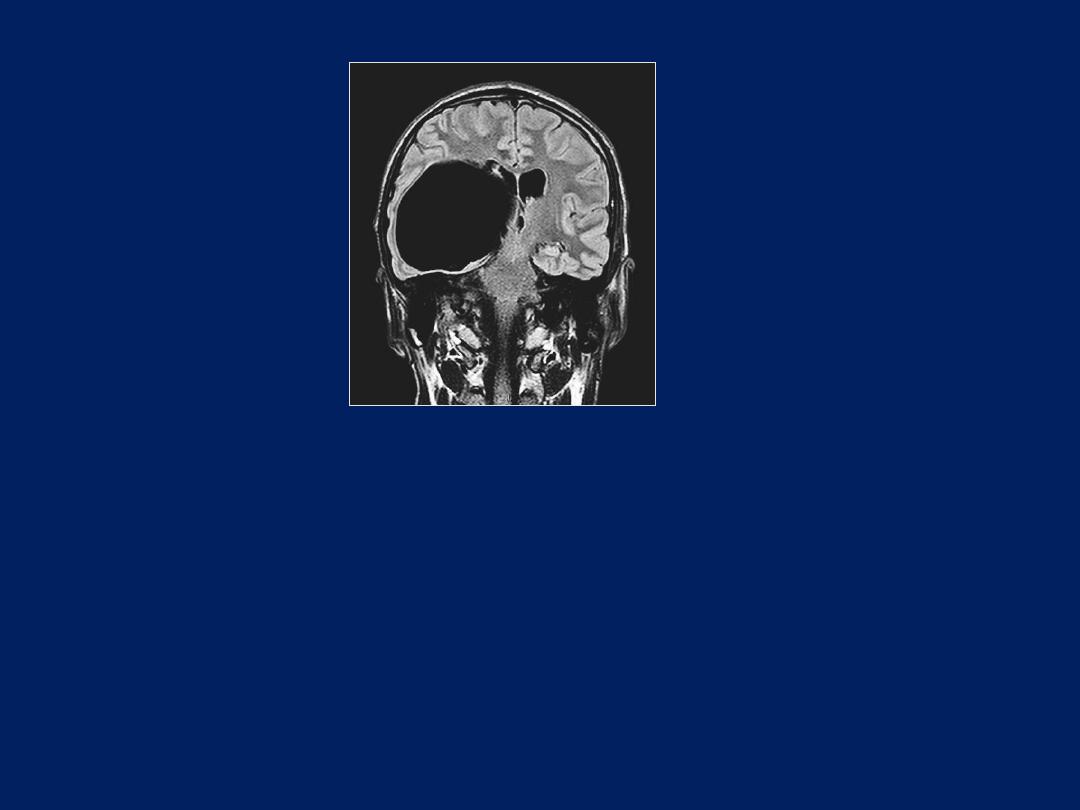
Which of the following is the most likely diagnosis for this incidental finding
on an MRI?
1. Type 1 Chiari malformation
2. Cavernous angioma
3. Asymptomatic cortical infarct
4. Aneurysm
5. Arachnoid cyst

Answer:
Arachnoid cyst
Arachnoid cysts are collections of cerebrospinal fluid
within the layers of the arachnoid membrane. They are
also known as leptomeningeal cysts. They can arise from
both the cranial and spinal meninges. They are
histologically benign but may cause symptomatic
compression of surrounding structures.
Meningioma
This well-circumscribed and
highly calcified extra-axial
mass is most consistent with a
meningioma.
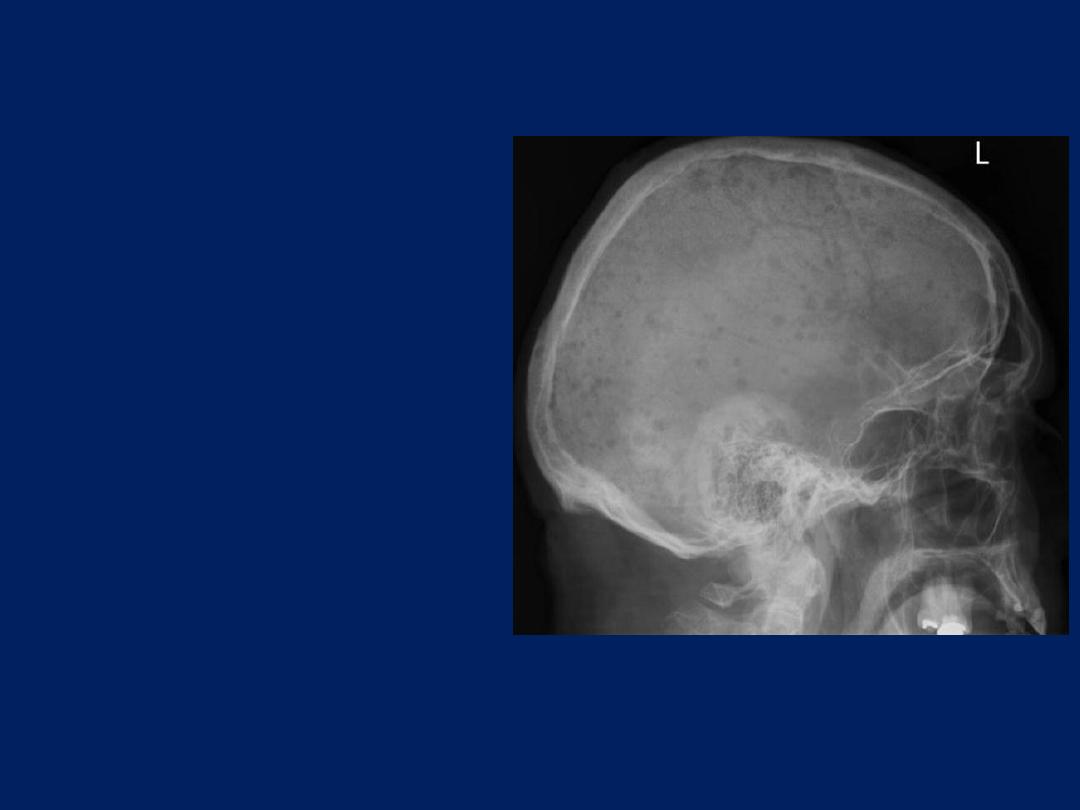
1.What are the radiographic
findings?
2 .what is the most likely
diagnosis?
3 .What further
investigations would you
request and why?
1.The skull radiograph shows the typical appearance of a
“pepper
pot” skull,
characterised by numerous well defined “punched out”
lytic lesions.
2.Multiple myeloma.
3.Serum electrophoresis will detect paraproteins in the blood as
a band of monoclonal immunoglobulins. Urine electrophoresis
will check for free light chains (Bence-Jones proteins) in the
urine. Immunofixation will establish the immunoglobulin
subtype in the blood and the subtype of light chain in the urine.
Bone marrow aspiration and biopsy will confirm the degree of
marrow infiltration and presence of malignant plasma cells by
immunohistochemistry. Serum immunoglobulin concentrations
are typically reduced. A radiological skeletal survey is necessary
to screen for osteolytic lesions.
Left upper lobe collapse
Plain film chest radiograph showing veil-like opacity
in the left upper zone. Note the deviation of the left hilum
and the loss of clarity of the hilar outline secondary to the
adjacent collapse (black arrows)

The plain film chest radiograph shows
the characteristic
radiological features of left upper lobe collapse :
A mediastinal shift to the left side with volume loss in the
lefthemithorax. Note the hilar and left diaphragmatic
elevation associated with
a veil-like increased density
of
the left upper lobe sparing the lingula (the left heart
border is clearly seen suggesting that the lingula is
aerated). The most likely diagnosis in an adult with a
collapsed upper lobe is that of a central obstructing
tumour, and this was confirmed in this patient.
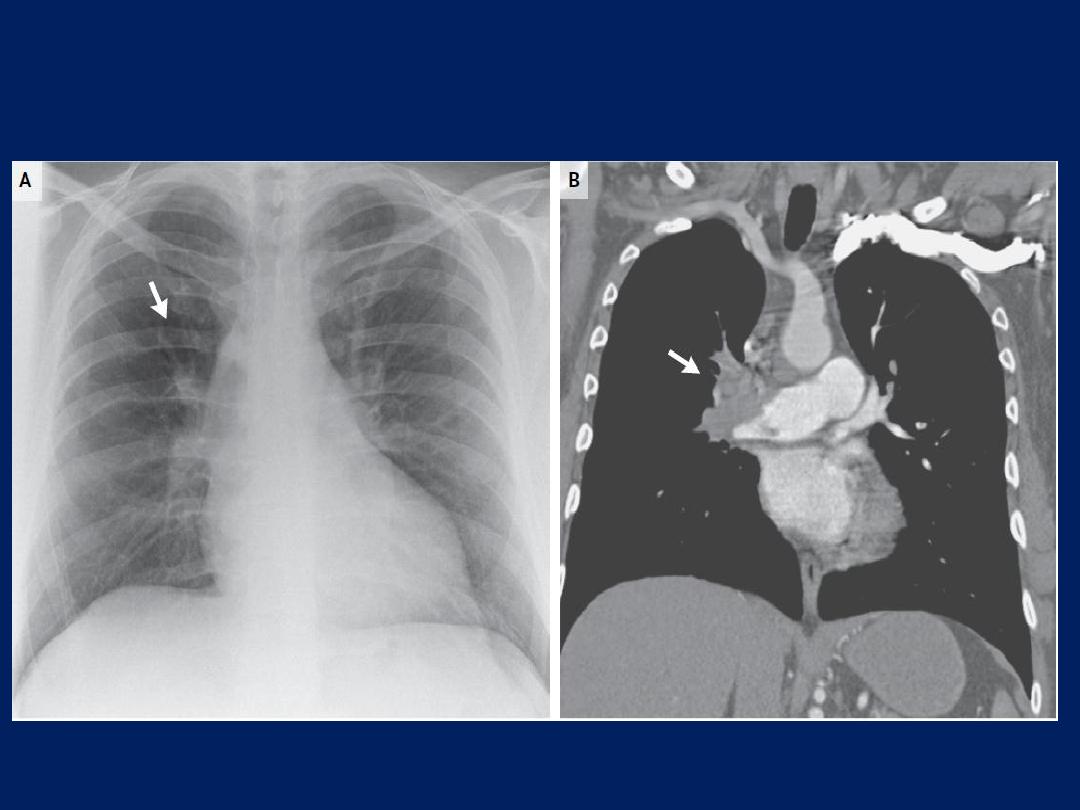
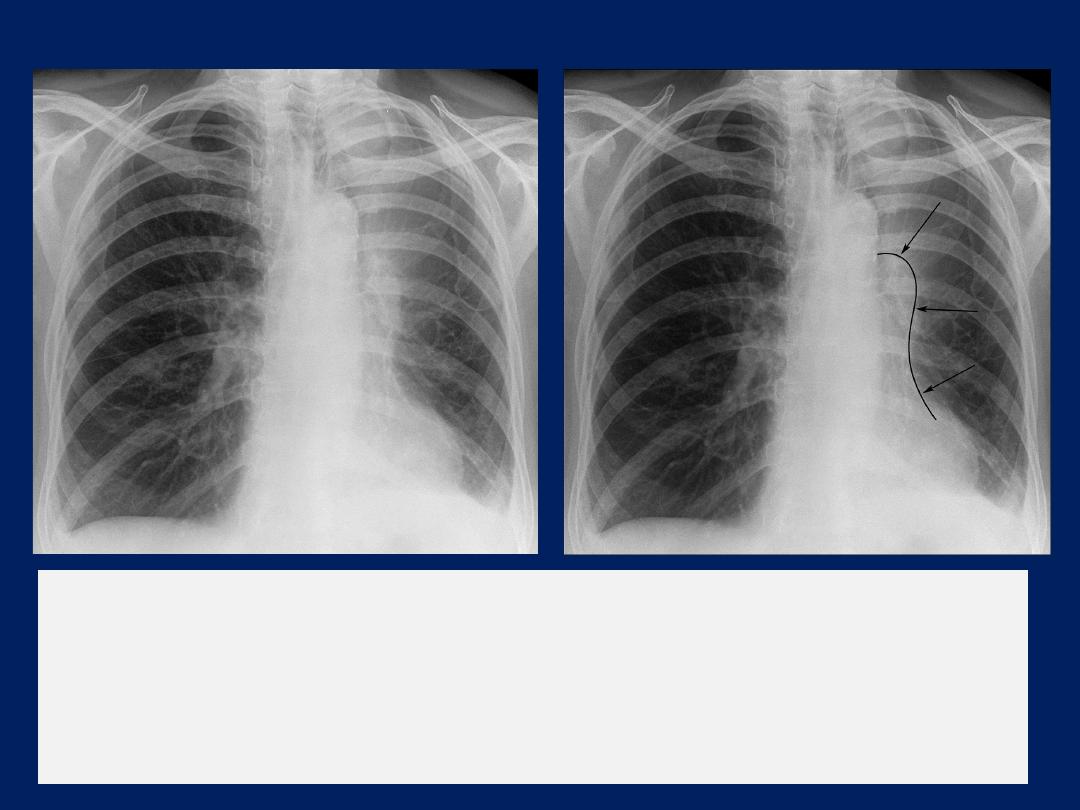
Westermark Sign in Pulmonary Embolism
A 47-year-old woman presented to the emergency department
with acute shortness of breath
and hypoxemia. Her medical
history included sex reassignment, for which she was taking
estrogen, and a deep-vein thrombosis on the left side, for which
she had required treatment with warfarin. She had a family
history of fatal pulmonary emboli. An electrocardiogram revealed
right bundlebranch block and right axis deviation .Blood tests
revealed an elevated d-dimer level of 2073 ng per milliliter. A
chest radiograph showed
a Westermark sign
(Panel A, arrow),
with a focal area of oligemia in the right middle zone and cutoff
of the pulmonary artery in the upper lobe of the right lung.
Computed tomographic pulmonary angiography confirmed the
presence of a thrombus in the right pulmonary artery (Panel B,
arrow), with an occlusive thrombus in the pulmonary arteries of the
right upper and middle lobes. Another thrombus could be seen in
multiple branches of the left pulmonary artery. The patient was
given warfarin and made a good recovery.
Giant right atrium
This man was found to have new atrial
fibrillation, tricuspid regurgitation, and
right-sided heart failure. Transthoracic
echocardiography revealed a giant
right atrium, dilated right ventricle, and
tricuspid regurgitation.
Right atrial enlargement can be
caused by
pulmonary hypertension,
tricuspid-valve stenosis, and Ebstein’s
anomaly. Giant right atrium is a rare
congenital condition that causes
tricuspid regurgitation and right-sided
heart failure.


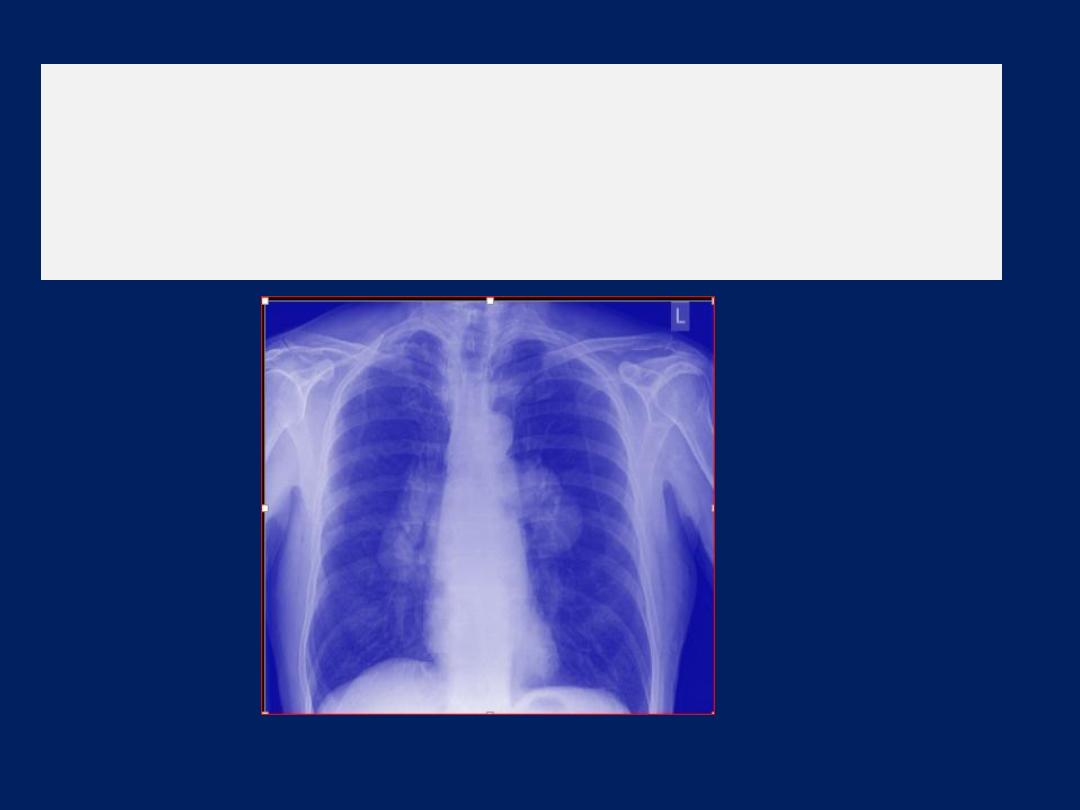
Symmetrical lobular
enlargement of both pulmonary
hila, with no signs of cardiomegaly or vascular
abnormality This appearance is consistent with
bilateral hilar lymphadenopathy
.
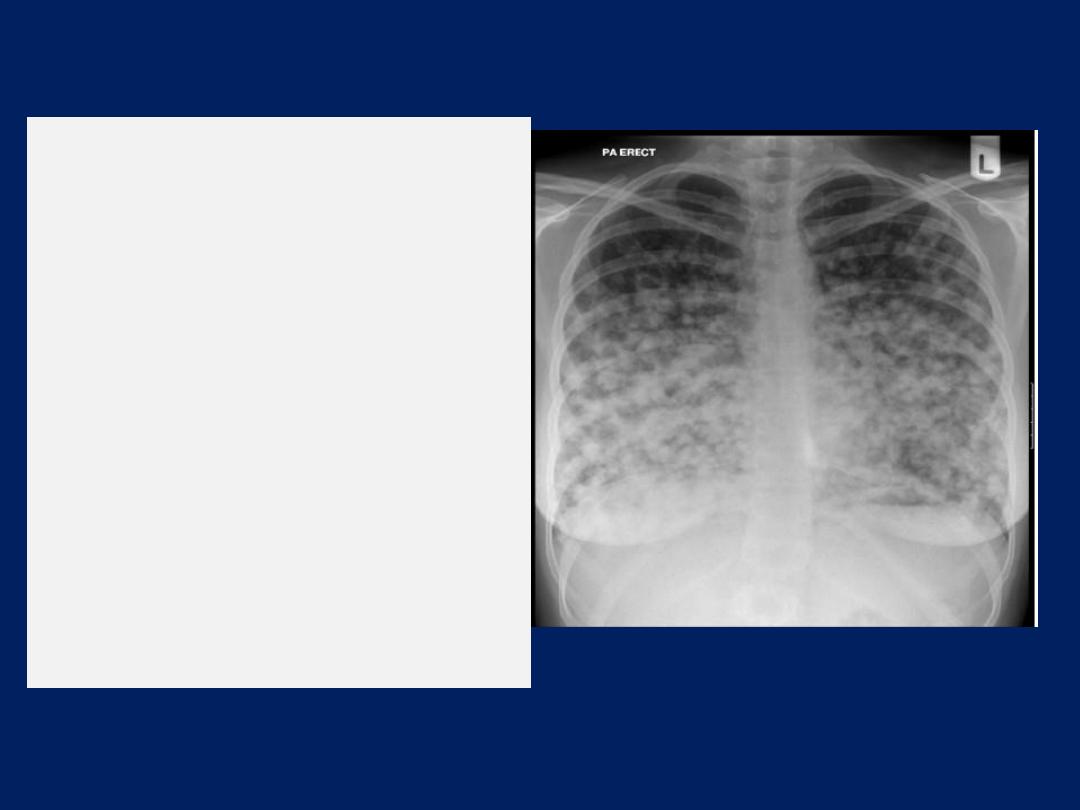
The chest x ray
shows
bilateral multiple nodules.
Pulmonary nodules can be
benign or malignant.
Common benign causes
include infectious
granuloma, bronchial
adenoma, and benign
hamartoma. Malignant
causes include primary lung
cancer and metastases.
There are absent lung markings
with a hyperlucent right
hemithorax. The visceral pleura can
be visualised as a curvilinear line
that parallels the chest wall,
separating the partially collapsed
lung centrally from pleural air
peripherally.
An expiratory chest
x ray aids in the detection of a
small pneumothorax by
decreasing the volume
of aerated
lung
relative to the
pneumothorax.
Varying
appearances of
pleural effusion.
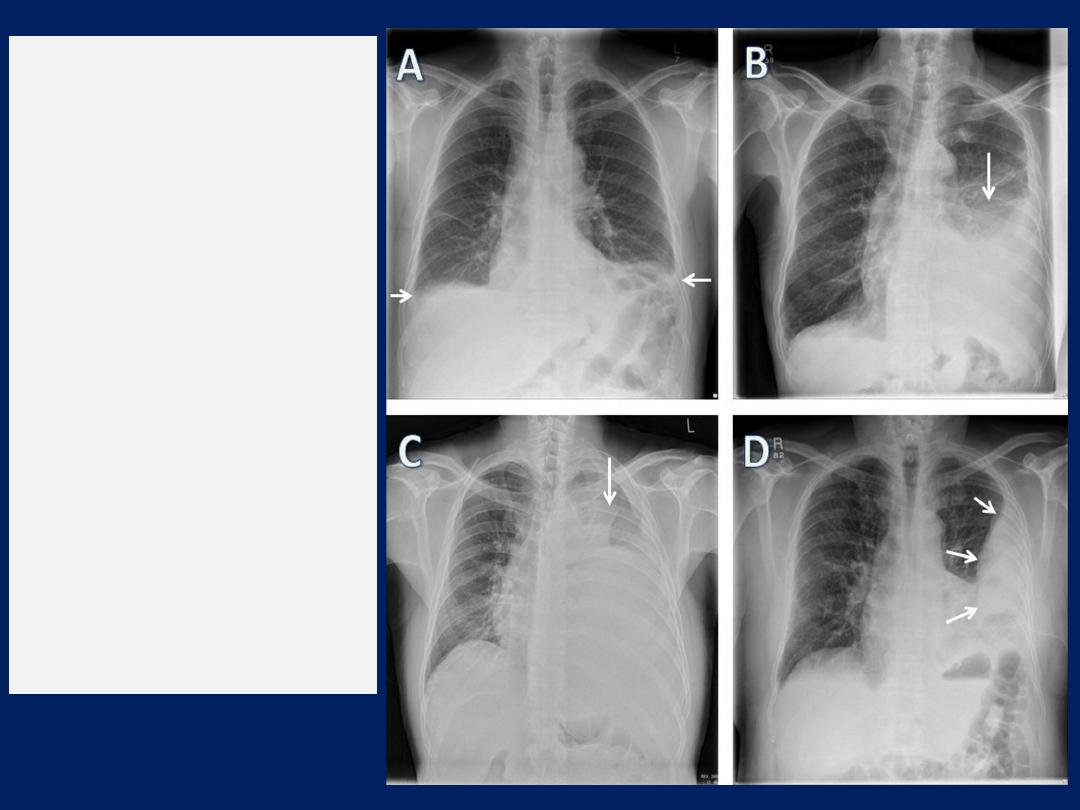
(A) Small bilateral
effusions,
(B) moderate left
sided effusion,
(C) large left
sided effusion, and
(D) left sided
loculated pleural
effusion with intercostal
drain in situ

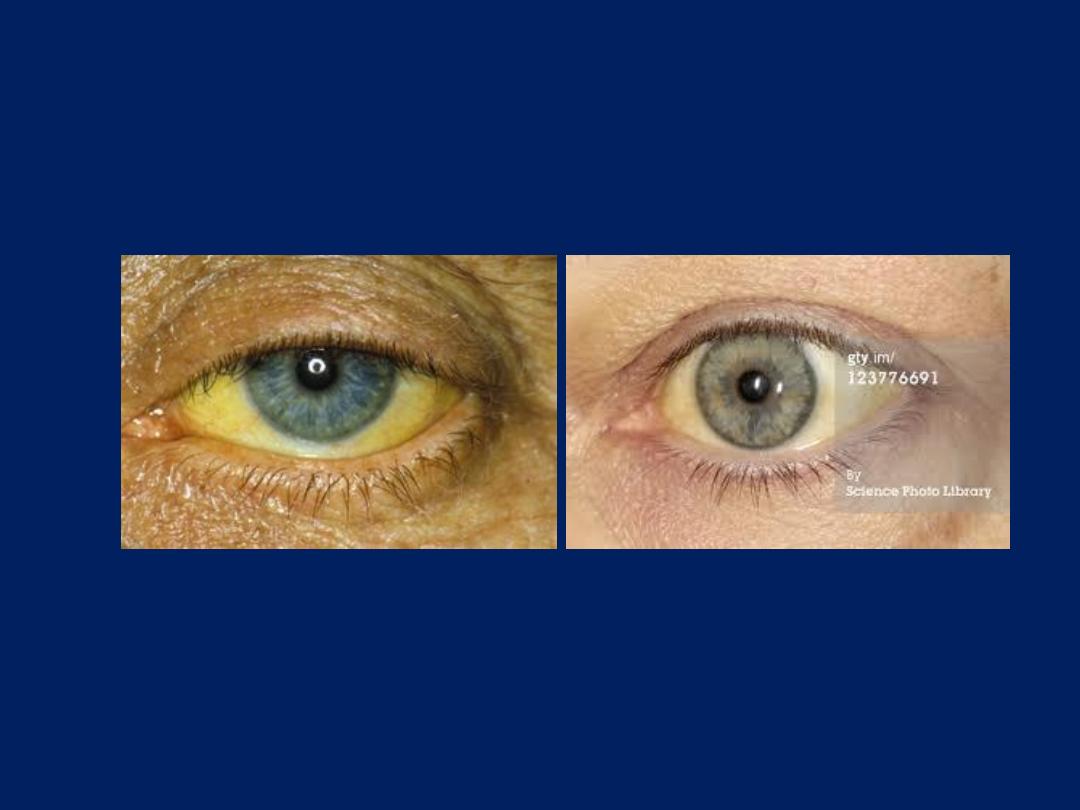
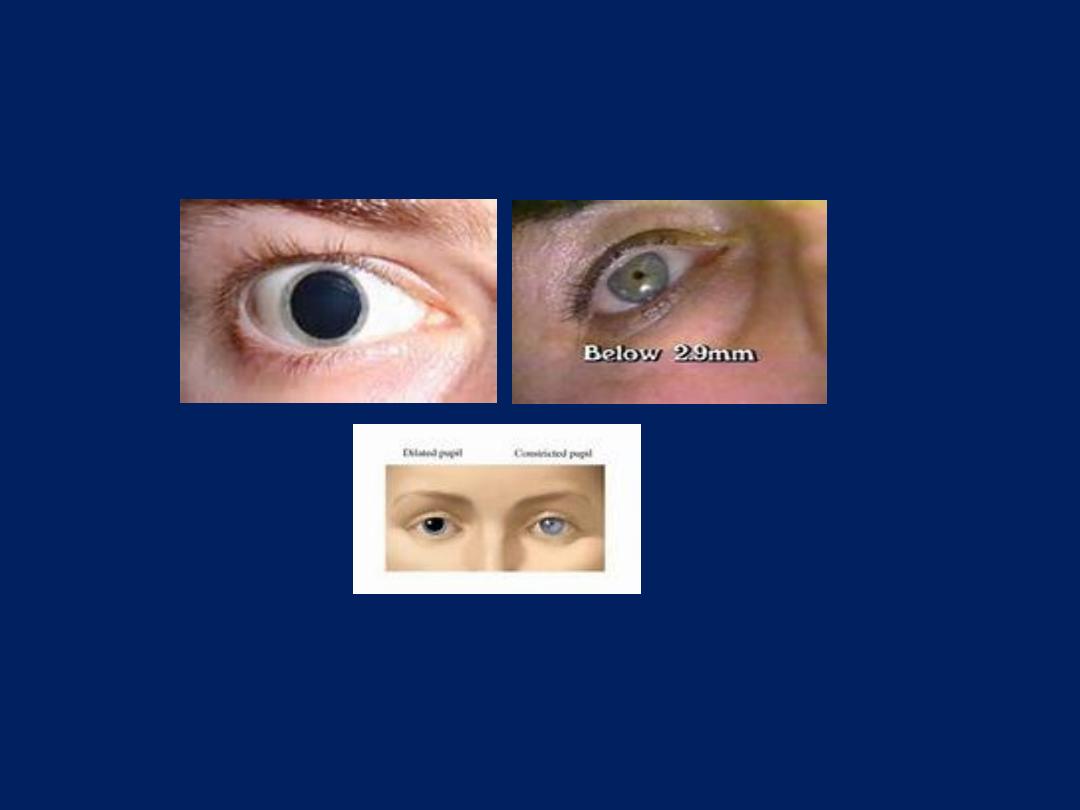
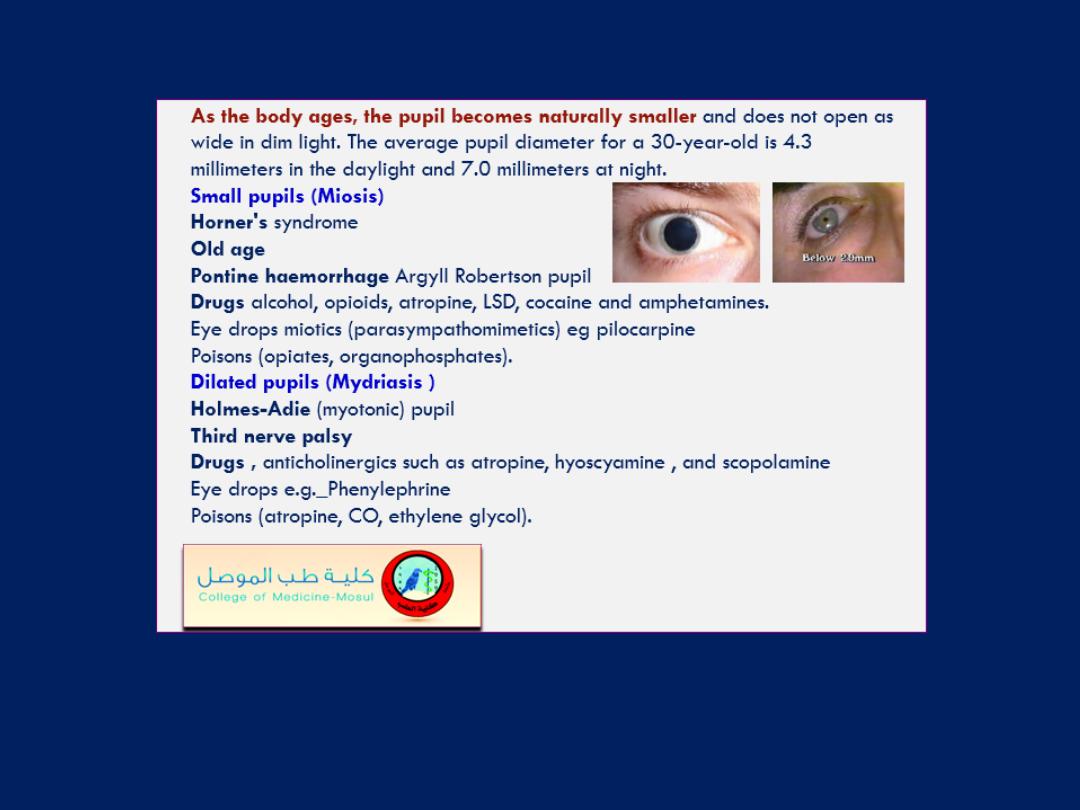
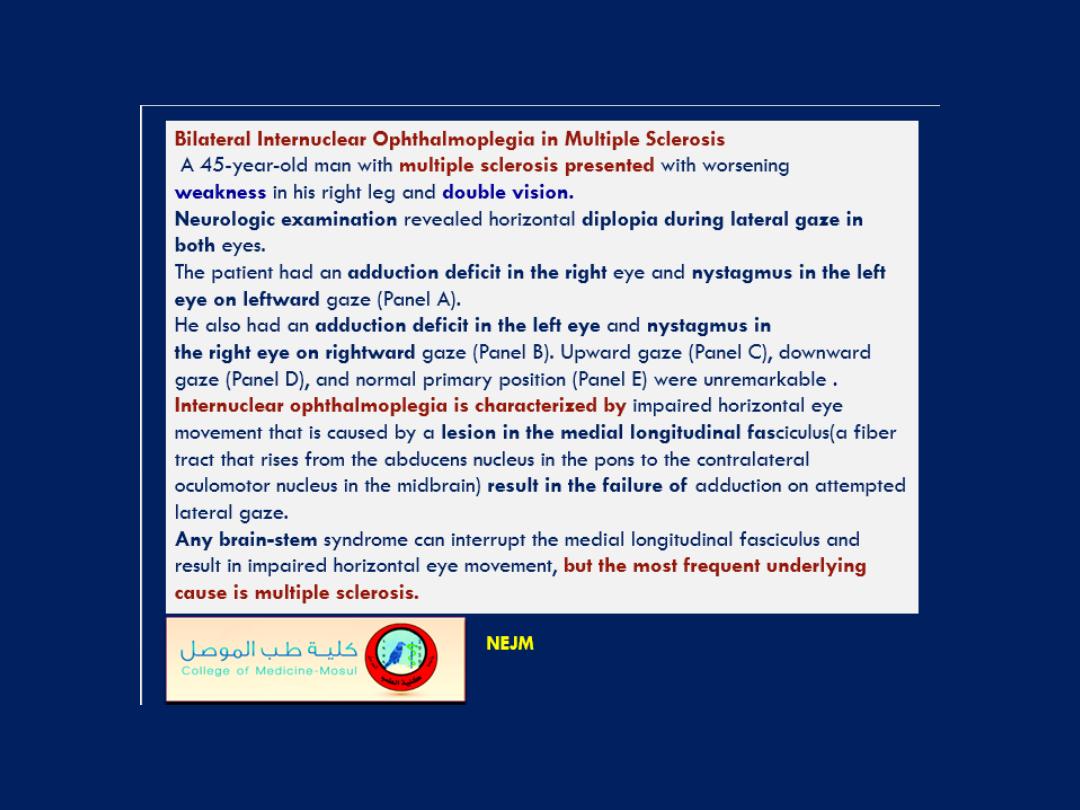
Tabes Dorsalis and Argyll Robertson Pupils
NEJM November 17, 2016
Argyll Robertson pupils,
which are nonreactive to bright light
but
briskly constrict when focusing on a near object . Magnetic
resonance imaging showed high signal changes in the dorsal columns
of the thoracic spine, and samples of blood and cerebrospinal fluid
were positive for syphilis on Venereal Disease Research Laboratory
(VDRL) testing and Treponema pallidum particle agglutination assay.
The patient was treated with intravenous penicillin for 14 days, and
gabapentin was started for the neuropathic leg pains.
Tabes dorsalis
is a form of neurosyphilis that is characterized by
degeneration of the nerves in the dorsal columns of the spinal cord.
Along with Argyll Robertson pupils, the condition is associated with
ataxia and loss of proprioception. After treatment, the patient’s
symptoms and mobility slowly improved, although the shooting pains
in his legs have continued despite pharmacotherapy. The serum VDRL
level fell appropriately, and the result on VDRL testing of the
cerebrospinal fluid was negative.
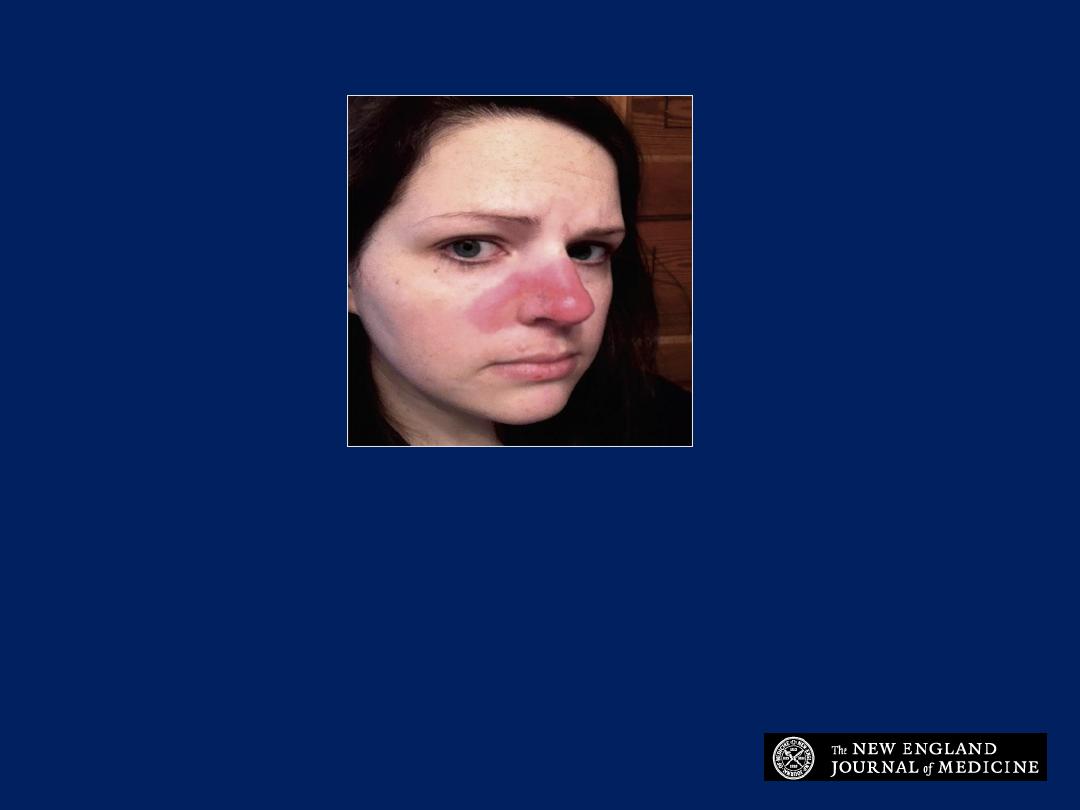
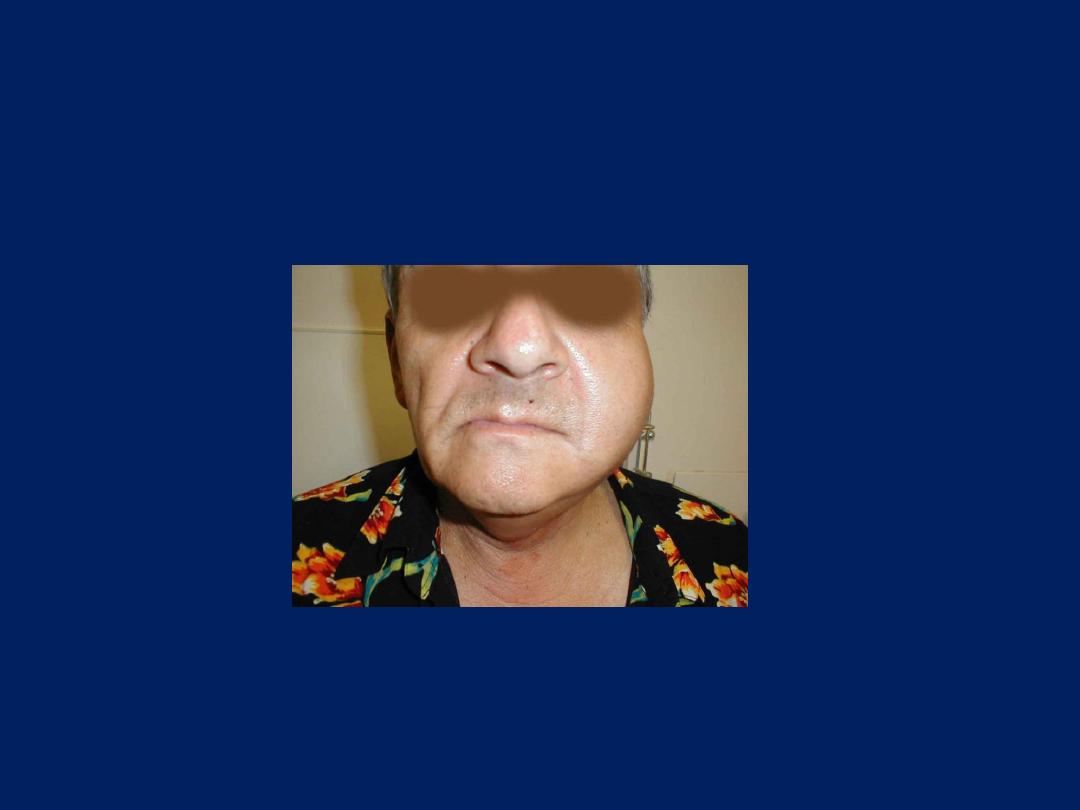
Image Challenge
A 28-year-old woman had a painful vesicular lesion that erupted into this
erythematous rash, which did not improve with antibiotics. What is the
diagnosis?
1. Cutaneous lupus
2. Erysipelas
3. Dermatomyositis
4. Rosacea
5. Fixed drug eruption
NEJM October 20, 2016

Cutaneous lupus
The correct answer is cutaneous lupus erythematous.
Cutaneous lupus is an inflammatory disorder that may
occur independently or in association with systemic
lupus and is often provoked by sun exposure.
Workup may include positive serum autoantibodies
(Ro/La) and diagnosis confirmed with punch biopsy.
Photoprotection, topical steroids, and oral antimalarials
are the treatments of choice.

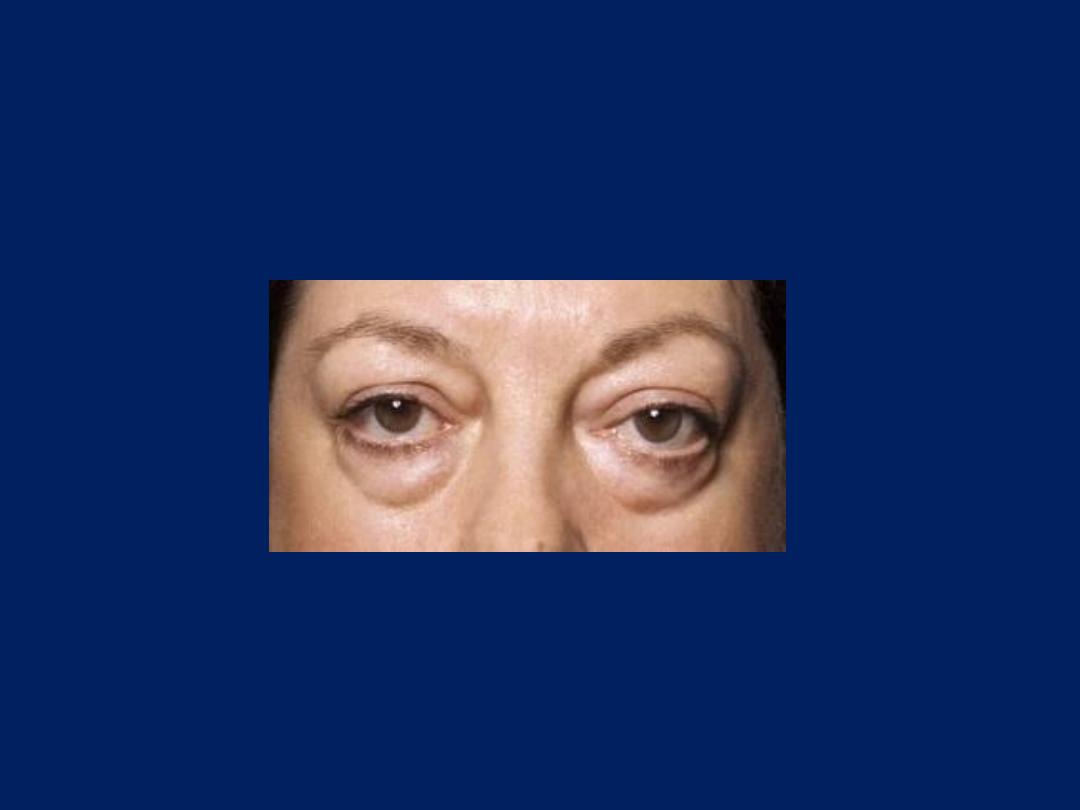
Diagnosing Myasthenia Gravis with an Ice Pack
NEJM November 10, 2016
A 68-year-old man
presented with unilateral ptosis and no
other symptoms. The neurologic examination revealed ptosis of the
left eye after a sustained upward gaze (Panel A). The movements
of the extraocular muscles were normal. Myasthenia gravis was
suspected, and the ice-pack test was performed with the placement
of an instant cold pack over the left eye (Panel B).
After 2 minutes, the ptosis was substantially diminished (>5 mm),
indicating a positive test (Panel C). The diagnosis was further
supported by the presence of serum anti–acetylcholine receptor
antibodies and by electrodiagnostic testing, which showed a
decremental response to repetitive nerve stimulation.
The ice-pack test
can be a useful bedside test to distinguish
myasthenia gravis from other causes of ptosis or ophthalmoparesis.
The inhibition of acetylcholinesterase activity at a reduced muscle
temperature is thought to underlie the observed clinical
improvement. The patient was treated symptomatically with
pyridostigmine, and the ptosis was diminished.
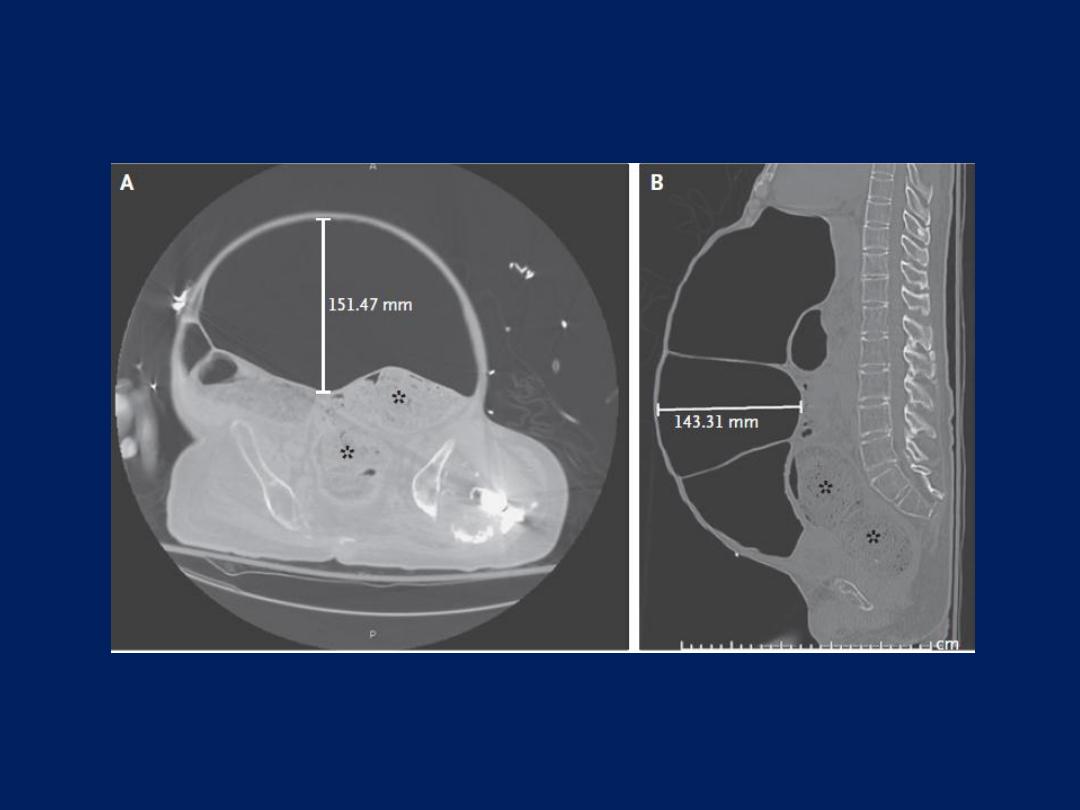
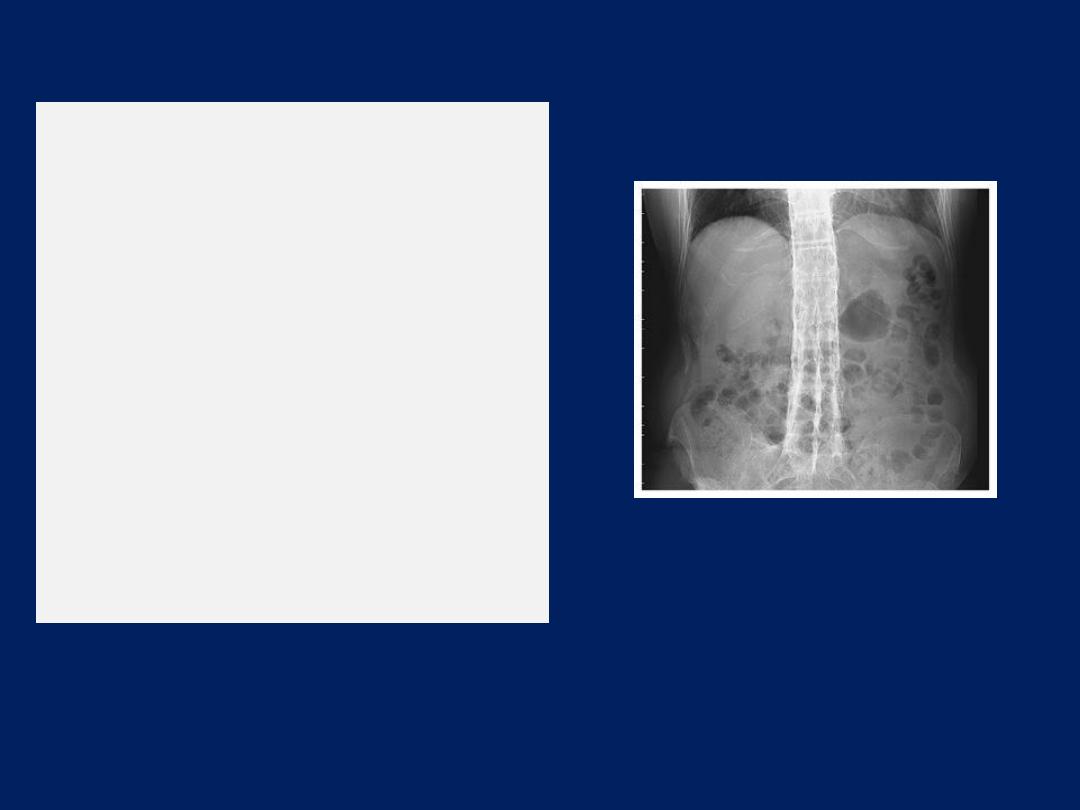
Neurogenic Megacolon in Spinal Cord Injury
NEJM December 1, 2016
A 44-year-old man
with a 20-year history of quadriplegia from a gunshot wound
to the neck presented to the emergency department with symptoms of a urinary
tract infection. His medical history included chronic megacolon and neurogenic
bladder, and he had been admitted to the hospital many times for the
management of urinary tract infections and constipation. On physical examination,
his abdomen was distended, soft, nontender, and tympanic to percussion, with
normal bowel sounds. Extremely large, intermittent waves of peristalsis were noted
(see video), and the patient reported mild cramping and a bloating sensation in
association with this finding. Computed tomography of the abdomen revealed
massive dilatation of the transverse
(Panels A and B),
descending, and sigmoid
colon of up to 18 cm. There was also a substantial fecal burden as a result of
neurogenic dysfunction (Panels A and B, asterisks). Stool softeners and laxatives
were administered, and the patient was told to avoid antimotility agents.
Megacolon is prevalent in patients with spinal cord injuries, especially in older
patients and in those with injuries that have been present for more than 10 years.
Complications of megacolon
include abdominal compartment syndrome, volvulus,
and fecal impaction.
Definitive treatment
includes colectomy, colostomy, or both. This patient opted for
conservative management in accordance with his symptoms.
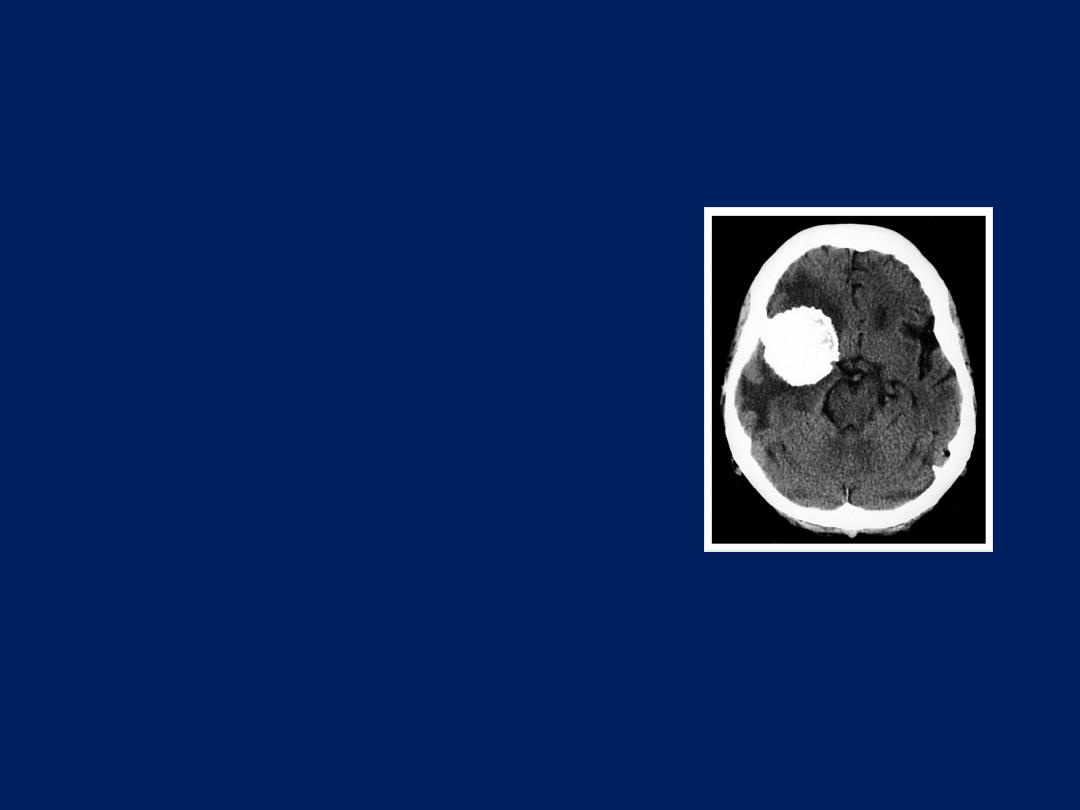
Emphysematous Cystitis
NEJM November 3,2016
A 72-year-old woman
with poorly controlled hyperlipidemia and diabetes
presented to the emergency department with a 5-day history of lower abdominal
pain. She also had fever and reported nausea and vomiting.
Physical examination revealed lower abdominal tenderness. Blood tests revealed
leukocytosis associated with a left shift (neutrophil count of 11,800 per cubic
millimeter) and elevation of the levels of C-reactive protein (24.0 mg per
deciliter) and glucose (735 mg per deciliter [41 mmol per liter]). A plain
radiograph of the kidneys, ureters, and bladder showed air surrounding the
bladder
(Panel A, arrows).
An abdominal computed tomographic scan revealed
an area of gas dissecting the bladder wall, bilateral hydronephrosis, and
intramural gas with a cobblestone or beaded-necklace appearance (Panel B,
arrows), findings consistent with emphysematous cystitis. The patient was treated
with broad-spectrum antimicrobial agents and placement of a Foley catheter.
Subsequently, a urine culture was positive for Escherichia coli; the patient was
treated with antibiotics and recovered uneventfully.
Emphysematous cystitis
is a urinary tract infection that is associated with gas
formation and is commonly caused by E. coli and Klebsiella pneumoniae.

A 51-year-old male with diabetes presented with 2 weeks of general
malaise and fever. What is the diagnosis?
1. Small bowel obstruction
2. Emphysematous pyelonephritis
3. Paralytic ileus
4. Renocolic fistula
5. Splenic abscess
Image Challenge

Emphysematous pyelonephritis
The correct answer is emphysematous pyelonephritis.
On presentation, the patient had acute kidney injury and
leukocytosis, and subsequently was found to have
Escherichia coli bacteremia. Abdominal computed
tomography further revealed gas in the renal
parenchyma and perinephric space. The greatest risk
factors for development of emphysematous pyelonephritis
are poorly controlled diabetes mellitus and ureteric
obstruction. The patient improved with antibiotics.
