
1
Fifth stage
Psychiatry
Lec-6
د. الهام الجماس
6/10/2015
Child Psychiatry (1)
The practice of child psychiatry differs from that of adult psychiatry in 5 ways:
Children seldom initiate the consultation.
The child’s problems may reflect the problems of other people.
The child’s stage of development must be considered.
Children are generally less able to express themselves in words.
The emphasis of treatment is different.
Normal Development
The first year of life:
3 wks / smiles at faces
6 months / selective smiling
8 months / fear of strangers
Shortly after 8 months / separation anxiety.
Bowlby (1980) attachment and bonding.
By the end of the first year, the child should have formed a close and secure relationship with
the mother or other close carer. There should be an ordered pattern of feeding and sleeping.
Learn about simple causal and spatial relationships.
By the end of the first year, they enjoy making sounds and may say “mama”, “dada”, and
perhaps one or two other words.
Year 2
Children begin to wish to please their parents and appear anxious when they disapprove.
They begin to learn to control their behavior. By now, attachment behavior should be well
established. Temper tantrums occur, particularly if exploratory wishes are frustrated. These
tantrums don’t last long, and should lessen as the child learns to accept constraints. By the
end of second year they should be able to put two or three words together as simple
sentence.

2
Pre-school years (2-5 years)
Social development occurs as child learn to live within the family.
Further increase in intellectual abilities, (language).
Identify with parent.
Concentration increase gradually.
Fantasy life is rich.
Transitional objects.
Sexual identity.
Defense mechanism develop.
Ride a tricycle
Help to dress and undress
Recall part of a story
Sing a song
Temper tantrum gradually disappear before school.
Middle childhood
Learn to cope with school.
Learn to read and write.
Acquire numerical concepts.
Social behavior develop further.
Adolescence
Self-awareness increase.
Consider where they want to go in life.
Some experience emotional turmoil and feel alienated from their family.
Peer group importance.
Interest in other sex.
Developmental psychopathology
The influence of genes:
Susceptibility genes have been identified for autism, ADHD, and specific reading
disorder.
Genes may indirectly cause stressful life events, for example they may control
personality traits of impulsiveness and irritability that lead to repeated break down of
relationships.

3
The influence of the environment
:
Poor parental care and risk of depression (caring relations with other people may protect,
yet this experience is not always protective, it does not reduce the risk of depression
following child abuse).
Changes in hormones:
In newborn the hypothalamo-pituitary-adrenal system is highly responsive. It becomes
progressively less responsive over the next 2 years. And there is some evidence that
this change is greater in securely attached than in insecurely attached infants (Gunnar,
1998).
These differences in responsiveness could be relevant to the development of
psychopathology.
The dividing line between normal and abnormal:
Many childhood disorders are at the extreme of a continuum of a normal behavior. Despite
this we need yes or no answers regarding treatment, so a cut-off point should be set.
Continuities and discontinuities:
Over activity and difficulties is management in 3 years of age is associated with
offending in adulthood (Stevenson and Goodman 2001).
Anxiety in childhood is less likely to persist in adulthood.
Classification of psychiatric disorder in children and adolescents
1. Adjustment reactions;
2. Pervasive developmental disorders;
3. Specific developmental disorders;
4. Conduct (antisocial or externalizing) disorder;
5. AHDH;
6. Emotional (neurotic or internalizing) disorders;
7. Symptomatic disorders.
Epidemiology
Behavioral and emotional disorders are common in childhood.
Rates in different developed countries are similar, also similar to developing countries.
In the UK, the prevalence of child psychiatric disorder in ethnic minority groups are
similar to that in the rest of population.

4
The landmark study was carried out more than 30 years ago in the Isle of Wight in the
UK, concerned with the health, intelligence, education, and psychological difficulties
in all the 10 and 11 years old attending state schools in the island- a total of 2193
children (Rutter et at., 1970).
The one year prevalence of rate of psychiatric disorder was about 7%, with the rate in
males being twice that in females.
Conduct disorders were 4 times more frequent among boys than girls, whereas
emotional disorders were more frequent in girls in a ratio of almost 1.5:1
There was no correlation between psychiatric disorder and social class, but the
prevalence increase as intelligence decrease.
It was associated also with physical handicap and esp. with evidence of organic brain
damage.
There was also strong association between reading retardation and conduct disorder.
In 1975, Rutter et at., done another study in London and rates of all types of disorders
were twice of those in the Isle of Wight.
The results of the landmark study were confirmed in subsequent studies carried out in
different countries.
Evidence about adolescence was provided originally by a 4 years follow-up of the Isle
of Wight study (Rutter et al., 1976)
At the age of 14, the 1 year prevalence rate of significant psychiatric disorder was
about 20%
In the UK there is evidence of a substantial increase in conduct and emotional
problems in adolescents over the past 25 years (Collishaw et al., 2004)
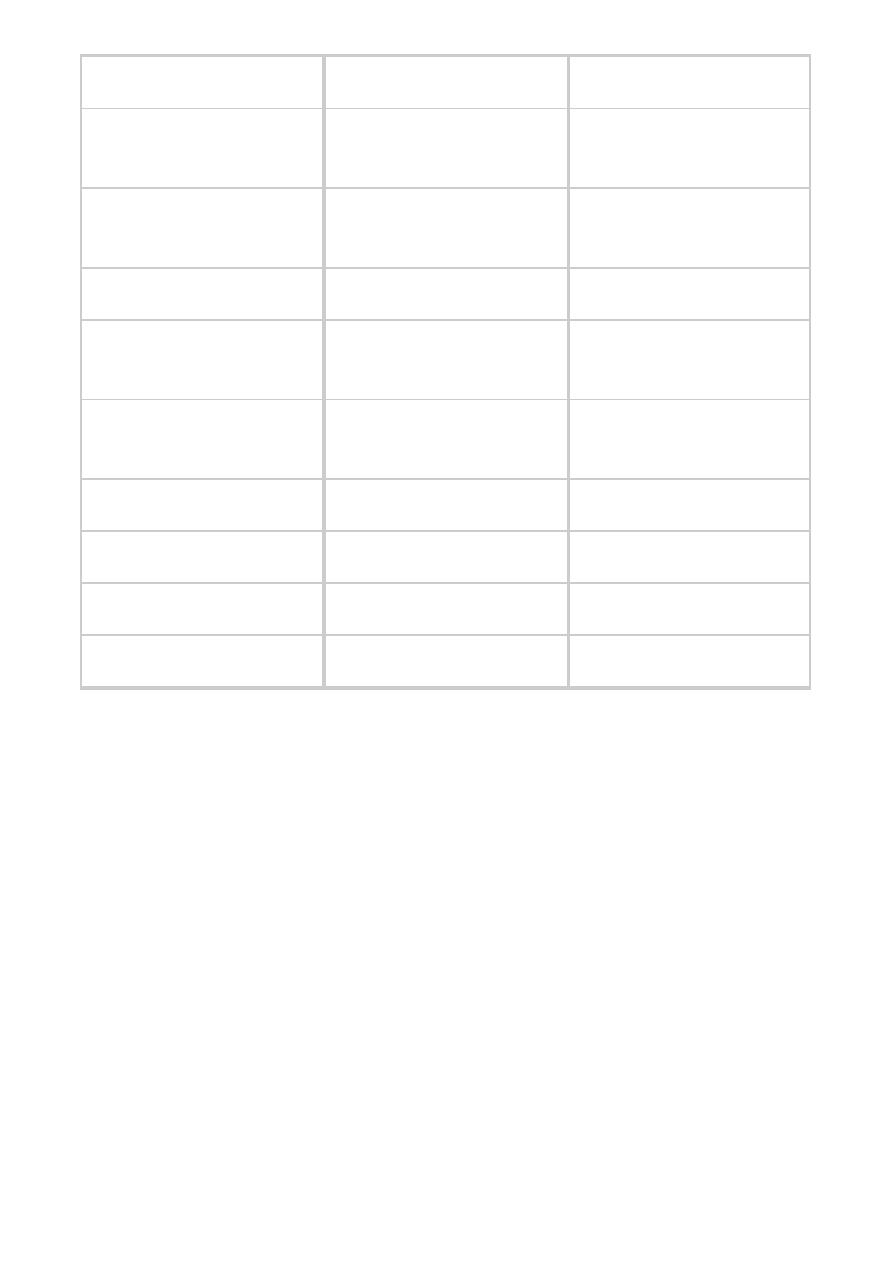
Variations with gender and age:
Before puberty, disorders are more frequent overall among males than among females; after
puberty, disorders are more frequent among females. ((check out the table in page 5))
Disorders which usually begins after puberty:
Depressive disorder
Mania
Psychosis
Agoraphobia and panic
Eating disorders
Substance abuse
Deliberate self-harm
Suicide and
Juvenile delinquency.
5
More freq. in females
Equal
More freq. in males
Depression after puberty
Depression
before
puberty
PDD
Specific phobias
School refusal
Specific
developmental
disorders
Eating disorders
Selective mutism
Hyperactivity disorders
Daytime enuresis
Oppositional-defiant
disorder
Deliberate self-harm after
puberty
Conduct disorder
Juvenile delinquency
Nocturnal enuresis
Tic disorder
suicide
