Assessment of Vestibular Functions
A. Clinical Tests1. Spontaneous Nystagmus
It is defined as involuntary, rhythmical, oscillatory movement of eyes. It may be horizontal, vertical or rotatory. Vestibular nystagmus has a slow and a fast component, and by convention, the direction of nystagmus is indicated by the direction of the fast component.The examiner keeps his finger about 30 cm from the patient's eye in the central position and moves it to the right or left, up or down, but not moving at any time, more than 30° from the central position to avoid gaze nystagmus. Presence of spontaneous nystagmus always indicates an organic lesion
2. Fistula Test
The basis of this test is to induce nystagmus by producing pressure changes in the external canal which are then transmitted to the labyrinth. Stimulation of labyrinth results in nystagmus and vertigo. The test is performed by applying intermittent pressure on the tragus or by using Siegle's speculum. It is positive when there is erosion of horizontal semicircular canal as in cholesteatoma or (fenestration operation), abnormal opening in the oval window (post-stapedectomy fistula) or the round window (rupture of round window membrane). A positive fistula also implies that the labyrinth is still functioning; it is absent when labyrinth is dead3. Romberg Test
The patient is asked to stand with feet together, and arms by the side with eyes first open and then closed. With the eyes open, patient can still compensate the imbalance but with eyes closed, vestibular system is at more disadvantage.4. Gait
The patient is asked to walk along a straight line to a fixed point, first with eyes open and then closed.
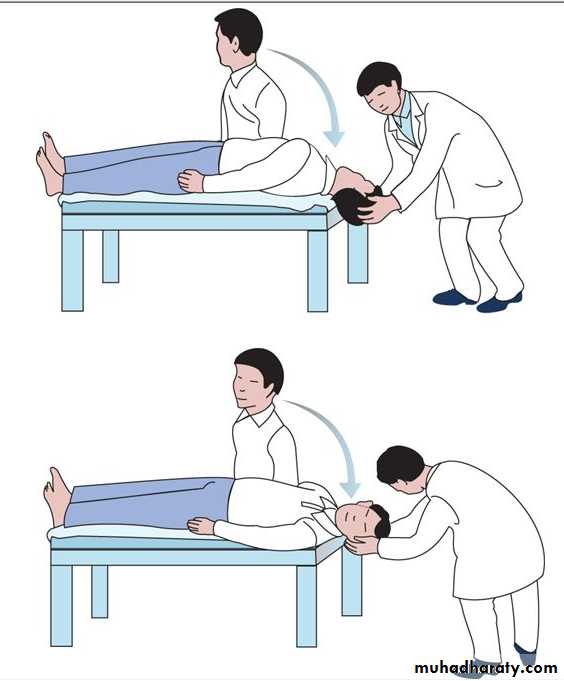
5. Dix-Hallpike Manoeuvre (Positional Test)
This test is particularly useful when patient complains of vertigo in certain head positions. It also helps to differentiate a peripheral from a central lesion.
Figure 6.1 Dix-Hallpike manoeuvre.
Test of Cerebellar DysfunctionAll cases of giddiness should be tested for cerebellar disorders. Disease of the cerebellar hemisphere causes: (i) Asynergia (abnormal finger-nose test) (ii) Dysmetria (inability to control range of motion) (iii) Adiadochokinesia (inability to perform rapid alternating movements) (iv) Rebound phenomenon (inability to control movement of extremity when opposing forceful restraint is suddenly released)
B. Laboratory Tests of Vestibular Function
1. Caloric TestThe basis of this test is to induce nystagmus by thermal stimulation of the vestibular system. Advantage is that each labyrinth can be tested separately..
(a) Modified Kobrak test
It is a quick office procedure. Patient is seated with head tilted 60° backwards to place horizontal canal in vertical position. Ear is irrigated with ice water for 60 seconds. Normally, nystagmus beating towards the opposite ear, will be seen with 5 ml of ice water. No response to 40 ml water indicates dead labyrinth.(b) Fitzgerald-Hallpike test (bithermal caloric test) In this test, patient lies supine with head tilted 30° forward so that horizontal canal is vertical . Ears are irrigated for 40 seconds alternately with water at 30°C and at 44°C (i.e. 7° below and above normal body temperature) and eyes observed for appearance of nystagmus till its end point. Time taken from the start of irrigation to the end point of nystagmus is recorded and charted on a calorigram . A gap of 5 minutes should be allowed between two ears. Cold water induces nystagmus to opposite side and warm water to the same side (remember mnemonic COWS: Cold-Opposite, Warm-Same).
(c) Cold-air caloric test
This test is done when there is perforation of tympanic membrane. The test employs Dundas Grant tube . It is only a rough qualitative test.
2. Electronystagmography
It is a method of detecting and recording of nystagmus . The test depends on the presence of corneoretinal potentials which are recorded by placing electrodes at suitable places round the eyes. The test is also useful to detect nystagmus which is not seen with the naked eye 3. Optokinetic Test Patient is asked to follow a series of vertical stripes on a drum moving first from right to left and then from left to right. Thus this test is useful to diagnose a central lesion.
4. Rotation Test
5. Galvanic Test6. Posturography
Disorders of vestibular systemA. Peripheral
which involve vestibular end organs and their first order neurons (i.e. the vestibular nerve). The cause lies in the internal ear or the VIIIth nerve. They are responsible for 85% of all cases of vertigo.B. Central
which involve central nervous system after the entrance of vestibular nerve in the brainstem and involve vestibulo-ocular, vestibulo-spinal and other central nervous system pathways.
Table 7-1. Vestibular disorders
Peripheral (Lesions of end organs vestibular nerve)
Central (Lesions of brainstem and central connections)Meniere's disease
Benign paroxysmal positional vertigo
Vestibular neuronitis
Labyrinthitis
Vestibulotoxic drugs
Head trauma
Perilymph fistula
Syphilis
Acoustic neuroma
Vertebrobasilar insufficiency
Posterior inferior cerebellar artery syndrome
Basilar migraine
Cerebellar disease
Multiple sclerosis
Tumours of brainstem and fourth ventricle
Epilepsy
Cervical vertigo
A. PERIPHERAL VESTIBULAR DISORDERS
1. Meniere's disease (endolymphatic hydrops)2. Benign paroxysmal positional vertigo (BPPV)
It is characterised by vertigofor seconds when the head is placed in a certain critical position(e.g rolling in bed). There is no hearing loss or other neurologic symptoms. Positional testing establishes the diagnosis and helps to differentiate it from positional vertigo of central origin . Disease is caused by a disorder of posterior semicircular canal though many patients have history of head trauma and ear infection.The vertigo is fatiguable on assuming the same position repeatedly due to dispersal of the otoconia but can be induced again after a period of rest. Thus, typical history and Hallpike manoeuvre establishes the diagnosis.
The condition can be treated by performing Epley's manoeuvre.
3. Vestibular neuronitischaracterised by severe vertigo of sudden onset with no cochlear symptoms. Attacks may last from a few days to 2 or 3 weeks. It is thought to occur due to a virus that attacks vestibular ganglion. Management of acute attack is similar to that in Meniere's disease. The disease is usually self-limiting.
4. Labyrinthitis.
There are three types of labyrinthitis:A-Circumscribed Labyrinthitis (Fistula of Labyrinth)or (Paralabyrinthitis)
There is thinning or erosion of bony capsule of labyrinth, usually of the horizontal semicircular canal.
Aetiology
•CSOM with cholesteatoma is the most common cause.
•Neoplasms of middle ear, e.g. carcinoma or glomus tumour.
•Surgical or accidental trauma to labyrinth.
Clinical features
A part of membranous labyrinth is exposed and becomes sensitive to pressure changes. Patient complains of transient vertigo often induced by pressure on tragus, cleaning the ear or performing Valsalva manoeuvre.
It is diagnosed by "fistula test" which can be performed in two ways.
(a) Pressure on tragus. Sudden inward pressure is applied on the tragus. Patient will complain of vertigo. Nystagmus may also be induced with quick component towards the ear under test. (b) Siegle's speculum.
Treatment
In chronic suppurative otitis media or cholesteatoma, mastoid exploration . Systemic antibiotic therapy should be instituted before and after operation .
B-Diffuse Serous Labyrinthitis
It is diffuse intralabyrinthine inflammation without pus formation and is a reversible condition if treated early.
Aetiology
• pre-existing circumscribed labyrinthitis associated with chronic middle ear suppuration or cholesteatoma.
•In acute infections of middle ear cleft inflammation spreads through annular ligament or the round window.
• It can follow stapedectomy or fenestration operation.
Clinical features
Mild cases complain of vertigo and nausea but in severe cases, vertigo is worse with marked nausea, vomiting and even spontaneous nystagmus. Quick component of nystagmus is towards the affected ear.
Cochlea is also affected with some degree of sensorineural hearing loss.
Serous labyrinthitis may pass onto suppurative labyrinthitis with total loss of vestibular and cochlear function.
Treatment
Medical.
(a) Patient is put to bed, his head immobilised with affected ear above.
(b) Antibacterial therapy is given in full doses to control infection.
(c) Labyrinthine sedatives, e.g. prochlorperazine (Stemetil).
(d) Myringotomy is done if labyrinthitis has followed acute otitis media and the drum is bulging. Pus is cultured for specific antibacterial therapy.
Surgical.
Cortical mastoidectomy (in acute mastoiditis) or modified radical mastoidectomy (in chronic middle ear infection or cholesteatoma). Medical treatment should always precede surgical intervention.
C-Diffuse Suppurative Labyrinthitis
This is diffuse pyogenic infection of the labyrinth with permanent loss of vestibular and cochlear functions.
Aetiology
It usually follows serous labyrinthitis, pyogenic organisms entering through a pathological or surgical fistula.
Clinical features
There is severe vertigo with nausea and vomiting . Spontaneous nystagmus will be observed with its quick component towards the healthy side. Patient is markedly toxic. There is total loss of hearing. Relief from vertigo is seen after 3-6 weeks due to adaptation.
Treatment
It is same as for serous labyrinthitis.
Rarely, drainage of the labyrinth is required, if intralabyrinthine suppuration is a source of intracranial complications, e.g. meningitis or brain abscess.
5. Vestibulotoxic drugs
Aminoglycoside antibiotics particularly streptomycin, gentamicin, kanamycin have been shown to affect hair cells of the crista ampullaris and to some extent those of the maculae. Certain other drugs which cause dizziness or unsteadiness are antihypertensives, labyrinthine sedatives, oestrogen preparations, diuretics, antimicrobials (nalidixic acid, metronidazole) and antimalarials.
6. Head trauma
Head injury may cause concussion of labyrinth, completely disrupt the bony labyrinth or VIIIth nerve, or cause a perilymph fistula. Severe acoustic trauma, such as that caused by an explosion can also disturb the vestibular end organ (otoliths) and result in vertigo.7. Perilymph fistula
In this condition, perilymph leaks into the middle ear through the oval or round window. It can follow as a complication of stapedectomy. It can also result from sudden pressure changes in the middle ear (e.g. barotrauma, diving, forceful Valsalva) or raised intracranial pressure (weightlifting or vigorous coughing). A perilymph fistula causes intermittent vertigo and fluctuating sensorineural hearing loss, sometimes with tinnitus and sense of fullness in the ear (compare Meniere's disease).8. Syphilis
9. Acoustic neuromaB. CENTRAL VESTIBULAR DISORDERS
1. Vertebrobasilar insufficiencyIt is a common cause of central vertigo in patients over the age of 50 years. There is transient decrease in cerebral blood flow. Common cause is atherosclerosis. Ischaemia in these patients may also be precipitated by hypotension or neck movements when cervical osteophytes press on the vertebral arteries during rotation and extension of head.
Vertigo is abrupt in onset, lasts several minutes and is associated with nausea and vomiting , with other neurological symptoms.
2. Posterior inferior cerebellar artery syndrome (Wallenberg's syndrome)
Thrombosis of the posterior inferior cerebellar artery cuts off blood supply to lateral medullary area. There is violent vertigo along with other neurological signs.3. Basilar migraine
Basilar artery migraine produces occipital headache, visual disturbances, diplopia and severe vertigo which is abrupt and may last for 5-60 minutes. Basilar migraine is common in adolescent girls with strong menstrual relationship and positive family history.4. Cerebellar disease
Cerebellum may be affected by haemorrhage (hypertension), infarction (occlusion of arterial supply), infection (otogenic cerebellar abscess) or tumours (glioma, teratoma or haemangioma).5. Multiple sclerosis
It is a demyelinating disease affecting young adults. Vertigo and dizziness are common complaints. There are other multiple neurological signs and symptoms, e.g. blurring or loss of vision, diplopia, dysarthria, paraesthesia and ataxia. Spontaneous nystagmus may be seen.6. Tumours of brainstem and floor of IVth ventricle
Gliomas, astrocytomas ; medulloblastoma, ependymomas, epidermoid cysts or teratomas . These tumours cause other neurological signs and symptoms in addition to vertigo and dizziness. Positional vertigo and nystagmus may also be the presenting features. CT scan and magnetic resonance imaging are useful in their diagnosis.7. Epilepsy
Vertigo may occur as an aura in temporal lobe epilepsy. The history of seizure and/or unconsciousness following the aura may help in the diagnosis. Sometimes, vertigo is the only symptom of epilepsy . E.E.G. may show abnormalities during the attack.
8. Cervical vertigo
Vertigo may follow injuries of neck 7-10 days after the accident. It is usually provoked with movements of neck to the side of injury. Examination shows tenderness of neck, spasms of cervical muscles and limitation of neck movements. X-rays show loss of cervical lordosis. Exact mechanism of cervical vertigo is not known.Other Causes of Vertigo
Ocular vertigoNormally, balance is maintained by integrated information received from the eyes, labyrinths and somatosensory system. A mismatch of information from any of these organs causes vertigo and in this case from the eyes. Ocular vertigo may occur in case of acute extraocular muscle paresis or high errors of refraction.
Psychogenic vertigo
This diagnosis is suspected in patients suffering from emotional tension and anxiety. Often other symptoms of neurosis, e.g. palpitation, breathlessness, fatigue, insomnia, profuse sweating and tremors are also present. Symptom of vertigo is often vague in the form of floating or swimming sensation or light-headedness. There is no nystagmus or hearing loss. Caloric test shows an exaggerated responseMeniere's Disease
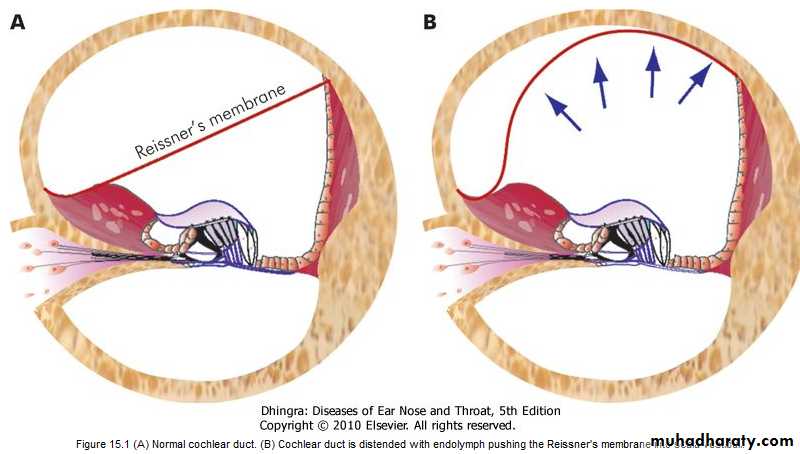
Meniere's Disease, also called endolymphatic hydrops, is a disorder of the inner ear where the endolymphatic system is distended with endolymph.Pathology
The main pathology is distension of endolymphatic system, mainly affecting the cochlear duct (scala media) and the saccule, and to a lesser extent the utricle and semicircular canals. The dilatation of cochlear duct is such that, it may completely fill the scala vestibuli; there is marked bulging of Reissner's membrane . The distended saccule may come to lie against the stapes footplate.
Aetiology
The main pathology in Meniere's disease is distension of endolymphatic system due to increased volume of endolymph. This can result either from increased production of endolymph or its faulty absorption or both. Normally, endolymph is secreted by stria vascularis, fills the membranous labyrinth and is absorbed through the endolymphatic sac .The exact cause of Meniere's disease is not yet known. Various theories have been postulated
1. Defective absorption by endolymphatic sac
Experimental obstruction of endolymphatic sac and its duct also produces hydrops. Ischaemia of sac has been observed in cases of Meniere's disease undergoing sac surgery. Distension of membranous labyrinth leads to rupture of Reissner's membrane and thus mixing of perilymph with endolymph, which is thought to bring about an attack of vertigo.2. Vasomotor disturbance
There is sympathetic over-activity resulting in spasm of internal auditory artery and/or its branches, thus interfering with the function of cochlear or vestibular sensory neuroepithelium. This is responsible for deafness and vertigo. Anoxia of capillaries of stria vascularis also causes increased permeability, with increased production of endolymph.3. Allergy
Nearly 50% of patients with Meniere's disease have concomitant inhalant and/or food allergy.
4. Sodium and water retention
Excessive amounts of fluid are retained leading to endolymphatic hydrops.5. Hypothyroidism
About 3% of cases of Meniere's disease are due to hypothyroidism. Such cases benefit from thyroid replacement therapy.6. Autoimmune and viral aetiologies (measles)
have also been suggested on the basis of experimental, laboratory and clinical observationsClinical Features
Age and sex. Disease is commonly seen in the age group of 35-60 years. Males are affected more than females. Usually, disease is unilateral but the other ear may be affected after a few years.
Cardinal symptoms of Meniere's disease are:
1. VertigoIt comes in attacks. The onset is sudden, with periods of spontaneous remission lasting for weeks, months or years. Usually, an attack is accompanied by nausea and vomiting with ataxia and nystagmus. Severe attacks may be accompanied by other symptoms of vagal disturbances such as abdominal cramps, diarrhoea, cold sweats, pallor and bradycardia.
2. Hearing loss
It usually accompanies vertigo or may precede it. Hearing improves after the attack and may be normal during the periods of remission. This fluctuating nature of hearing loss is quite characteristic of the disease. With recurrent attacks, improvement in hearing during remission may not be complete; leading to slow and progressive deterioration of hearing which is permanent.Distortion of sound. A tone of a particular frequency may appear normal in one ear and of higher pitch in the other leading to diplacusis. Music appears discordant.
Intolerance to loud sounds. due to recruitment phenomenon. They are poor candidates for hearing aids.
3. Tinnitus
It is low-pitched roaring type, and is aggravated during acute attacks. Change in intensity and pitch of tinnitus may be the warning symptom of attack.4. Sense of fullness or pressure
It also fluctuates. It may accompany or precede an attack of vertigo.Examination
Otoscopy NormalNystagmus
It is seen only during acute attack.
Tuning fork testsThey indicate sensorineural hearing loss. Rinne test is positive, absolute bone conduction is reduced in the affected ear and Weber is lateralised to the better ear.
Investigations
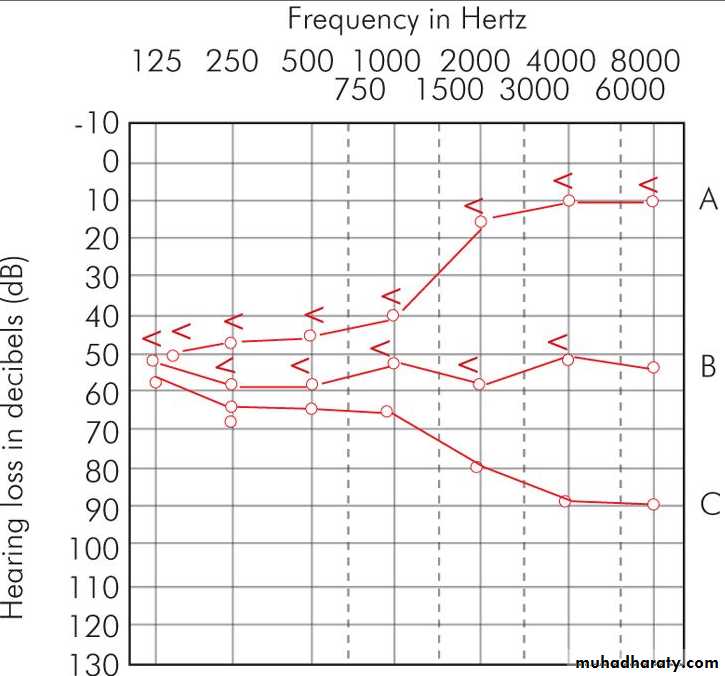
1. Pure tone audiometry
There is sensorineural hearing loss. In early stages, lower frequencies are affected and the curve is of rising type. When higher frequencies are involved curve becomes flat or a falling type .2. Speech audiometry
Discrimination score is usually 55-85% between the attacks but discrimination ability is much impaired during and immediately following an attack.3. Special audiometry tests
They indicate the cochlear nature of disease and thus help to differentiate from retrocochlear lesions, e.g. acoustic neuroma .
(a) Recruitment test is positive.
(b) SISI (short increment sensitivity index) test.
(c) Tone decay test.
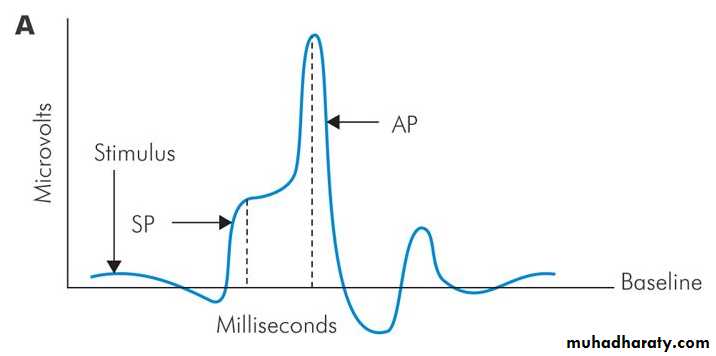
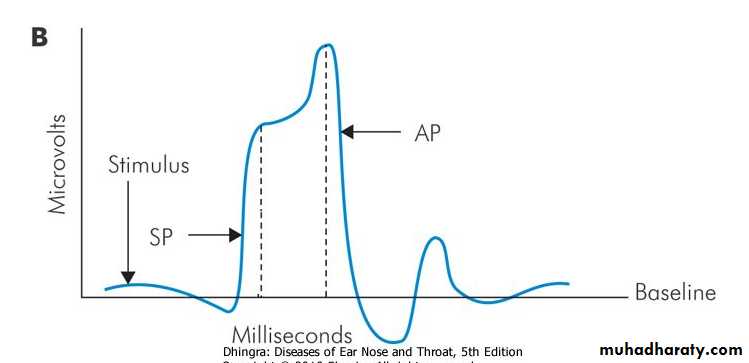
4. Electrocochleography
It shows changes diagnostic of Meniere's disease. Normally, ratio of summating potential (SP) to action potential (AP) is 30%. In Meniere's disease, SP/AP ratio is greater than 30% .5. Caloric test
shows reduced response on the affected side in 75% of cases( canal paresis)6. Glycerol test
Glycerol is a dehydrating agent. When given orally, it reduces endolymph pressure and thus causes an improvement in hearing.
Audiogram and speech discrimination scores are recorded before and 1-2 hours after ingestion of glycerol. An improvement of 10 dB or gain of 10% in discrimination score makes the test positive. There is also improvement in tinnitus and in the sense of fullness in the ear. The test has a diagnostic and prognostic value. These days, glycerol test is combined with electrocochleography
Treatment
A. General Measures1. Reassurance
2. Cessation of smoking3. Low salt diet
4. Avoid excessive intake of water5. Avoid over-indulgence in coffee, tea and alcohol
6. Avoid stress and bring a change in life-style Mental relaxation exercises and yoga are helpful to decrease stress7. Avoid activities requiring good body balance
professions such as flying, under-water diving or working at great heights should be avoided.
B. Management of Acute Attack
1. Reassuranceand psychological support to allay worry and anxiety.
2. Bed restwith head supported on pillows to prevent excessive movements.
3. Vestibular sedativesto relieve vertigo. They should be administered intramuscularly or intravenously if vomiting precludes oral administration. Drugs useful in acute attack are dimenhydrinate (Dramamine), promethazine (Avomine) or prochlorperazine (Stemetil).
Diazepam (Valium ) 5-10 mg may be given intravenously. It has a tranquillizing effect and also suppresses the activity of medial vestibular nucleus.
In some patients, acute attack can be stopped by atropine, 0.4 mg, given subcutaneously.
4. Vasodilators
(i) Inhalation of carbogen (5% CO2 with 95% O2). (ii) Histamine drip.
C. Management of Chronic Phase
When patient presents after the acute attack, the treatment consists of:1. Vestibular sedatives
Prochlorperazine (Stemetil) 10 mg, thrice a day, orally for two months and then reduced to 5 mg thrice a day for another month.2. Vasodilators
Nicotinic acid,Betahistine (Vertin or Betaserc) 8-16 mg, thrice a day, given orally, also increases labyrinthine blood flow by releasing histamine in the body.
3. Diuretics
Furosemide, 40 mg tablet, taken on alternate days with potassium supplement helps to control recurrent attacks, if not controlled by vasodilators or vestibular sedatives.4. Propantheline bromide
(Probanthine), 15 mg, thrice a day, can be given alone or in combination with vasodilator and is quite effective.
5. Elimination of allergen
Sometimes a food or inhalant allergen is responsible for attacks. It should be found and eliminated or desensitisation done.6. Hormones
Investigations should be directed to find any endocrinal disorder such as hypothyroidism, and appropriate replacement therapy given. Control of stress by change in life-style is important to prevent recurrent attacks. About 80% of the patients can be effectively managed by medical therapy alone.D. Surgical Treatment
It is used only when medical treatment fails.1. Conservative procedures
They are used in cases where vertigo is disabling but hearing is still useful and needs to be preserved. They are:(i) Decompression of endolymphatic sac (ii) Endolymphatic shunt operation. A tube is put, connecting endolymphatic sac with subarachnoid space, to drain excess endolymph.
(iii) Sacculotomy (Fick's operation). Cochleosacculotomy
(iv) Section of vestibular nerve.
(v) Ultrasonic destruction of vestibular labyrinth. Cochlear function is preserved.
(vi) Transtympanic corticosteroid infusion of middle ear.
(vii) Intratympanic gentamicin therapy
(chemical labyrinthectomy). Gentamicin is mainly vestibulotoxic. It has been used in daily or biweekly injections into the middle ear. Drug is absorbed through the round window and causes destruction of the vestibular labyrinth. Total control of vertigo spells has been reported in 60-80% of patients with some relief from symptoms in others. Hearing loss, sometimes severe and profound, has been reported in 4-30% of patients treated with this mode of therapy. Intermittent low pressure pulse therapy [Meniett device therapy]. A prerequisite for such a therapy is to perform a myringotomy and insert a ventilation tube