Page 1
Fifth stage
Ophthalmology
Chapter-12
د
.
ﻧزار
6/3/2017
Retinal
vascular
disease
INTRODUCTION:
The eye is an organ in which much of the microcirculation is readily visualized. Vascular
disease affecting the eye can thus be seen directly .Furthermore the eye provides
important clues about pathological vascular changes in the rest of the body .
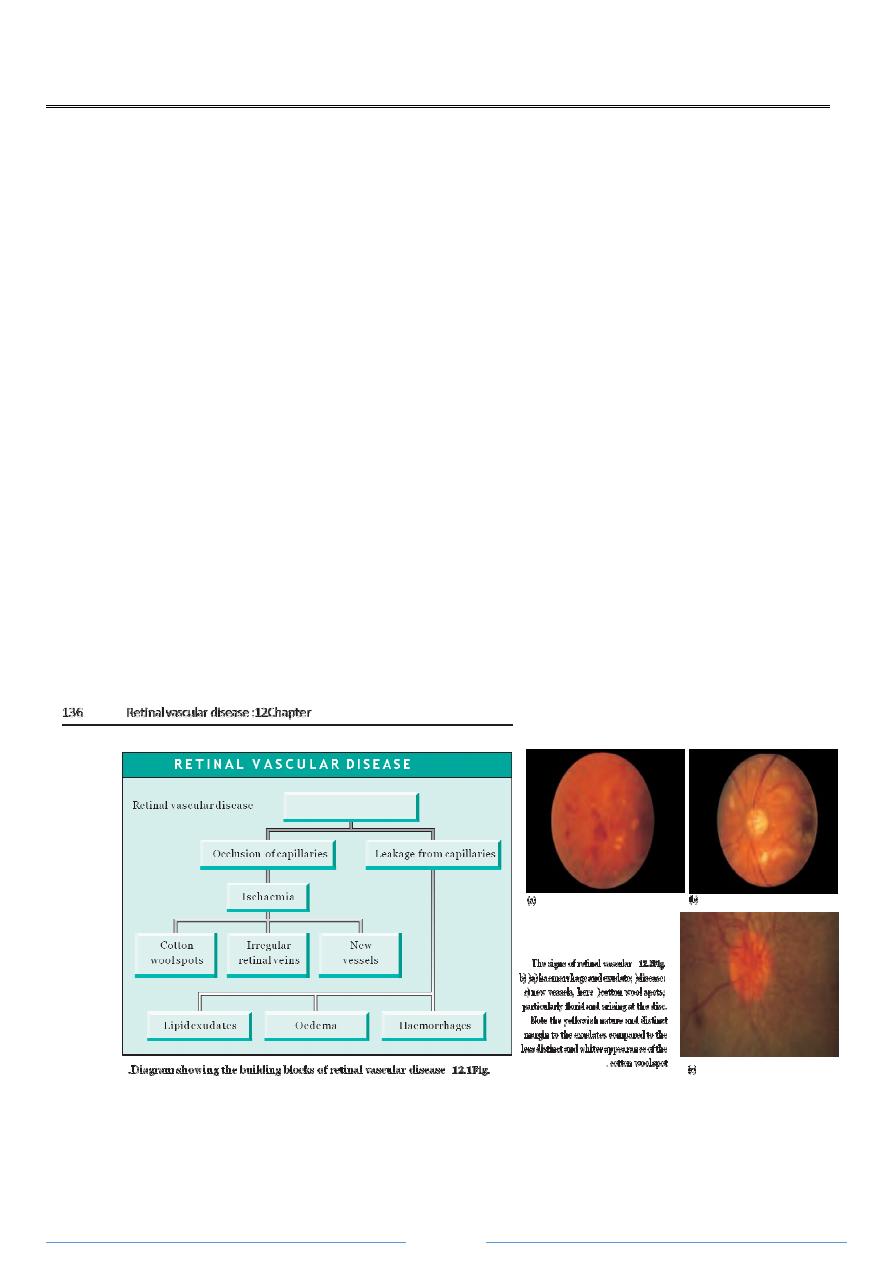
SIGNS OF RETINAL VASCULAR DISEASE :
The signs of retinal vascular disease result from two changes to the retinal capillary
circulation :
• leakage from the microcirculation ؛
• occlusion of the microcirculation .
Leakage from the microcirculation:
This results in :
• haemorrhages
caused by leakage of blood from damaged vessels ؛
• oedema
of the retina, the result of fluid leakage from damaged vessels ؛
• exudates
formed by lipids ،lipoprotein and lipid containing macrophages .These
are yellow in colour, with well-defined margins .
Page 2
Occlusion of the
microcirculation
:
This results in :
• Cotton
wool
spots
) previously termed soft
exudates.(These are caused by a build-
up of axonal debris in the nerve fibre layer of the retina ..Cotton wool spots are
found at the margins of ischaemic infarcts .Their visibility depends on nerve fibre
layer thickness so that they are seen close to the optic disc ،where the nerve fibre
layer is thick ،and not in the periphery where the nerve fibre layer is thin .They are
white in colour with indistinct borders .
• New
vessels .An ischaemic retina releases vasogenic factors
) e.g .VEGF (which
result in the growth of abnormal blood vessels and fibrous tissue onto the retinal
surface and forward into the vitreous .These intravitreal vessels are much more
permeable than normal retinal vessels ،and their abnormal position predisposes
them to break and bleed .
The diseases affecting the vasculature of the eye may be classified as shown in Box 12.1 .
OCULAR CIRCULATION
DIABETIC RETINOPATHY :
Diabetes results from a defect in both insulin secretion and action leading to
hyperglycaemia .
EPIDEMIOLOGY
Type I diabetes .Diabetic retinopathy appears about 5 years after onset .
.Because type II diabetes may be present for several years prior to diagnosis ،
retinopathy may be present at presentation .
Diabetes is associated with the following ocular events :
• retinopathy ؛
• cataract :a rare ،
’ snowflake ‘cataract in youth and a greater frequency and earlier
onset of age related cataract ؛
• glaucoma
)
• extraocular muscle palsy due to microvascular disease of the third ،fourth ،or sixth
cranial nerves .
Page 3
PATHOLOGY
Factors thought to be important in the development of diabetic retinopathy include :
• Duration of diabetes :80 %have retinopathy after 20 years of disease .
• Diabetic control .
• Coexisting diseases particularly hypertension .
• Smoking .
The development of retinopathy may also be accelerated by pregnancy and patients
require careful screening .
Retinal damage results from damage to the circulation .Pathological studies show that
there is a :
• decrease in the number of pericytes surrounding the capillary endothelium ؛
• development of microaneurysms on the capillary network which allow plasma to
leak out into the retina ؛
• development of arterio-venous shunts with closure of the capillary net resulting in
areas of ischaemic retina .
HISTORY
Diabetic retinopathy should be diagnosed before it is symptomatic .
All diabetics should have fundoscopy performed at least yearly .
Screening for sight-threatening retinopathy
) maculopathy and proliferative retinopathy (
should begin by 5 years after diagnosis in patients with type I disease ،and from the time
of presentation in type II disease .
Visual acuity may be reduced gradually by a maculopathy and suddenly from a vitreous
haemorrhage .
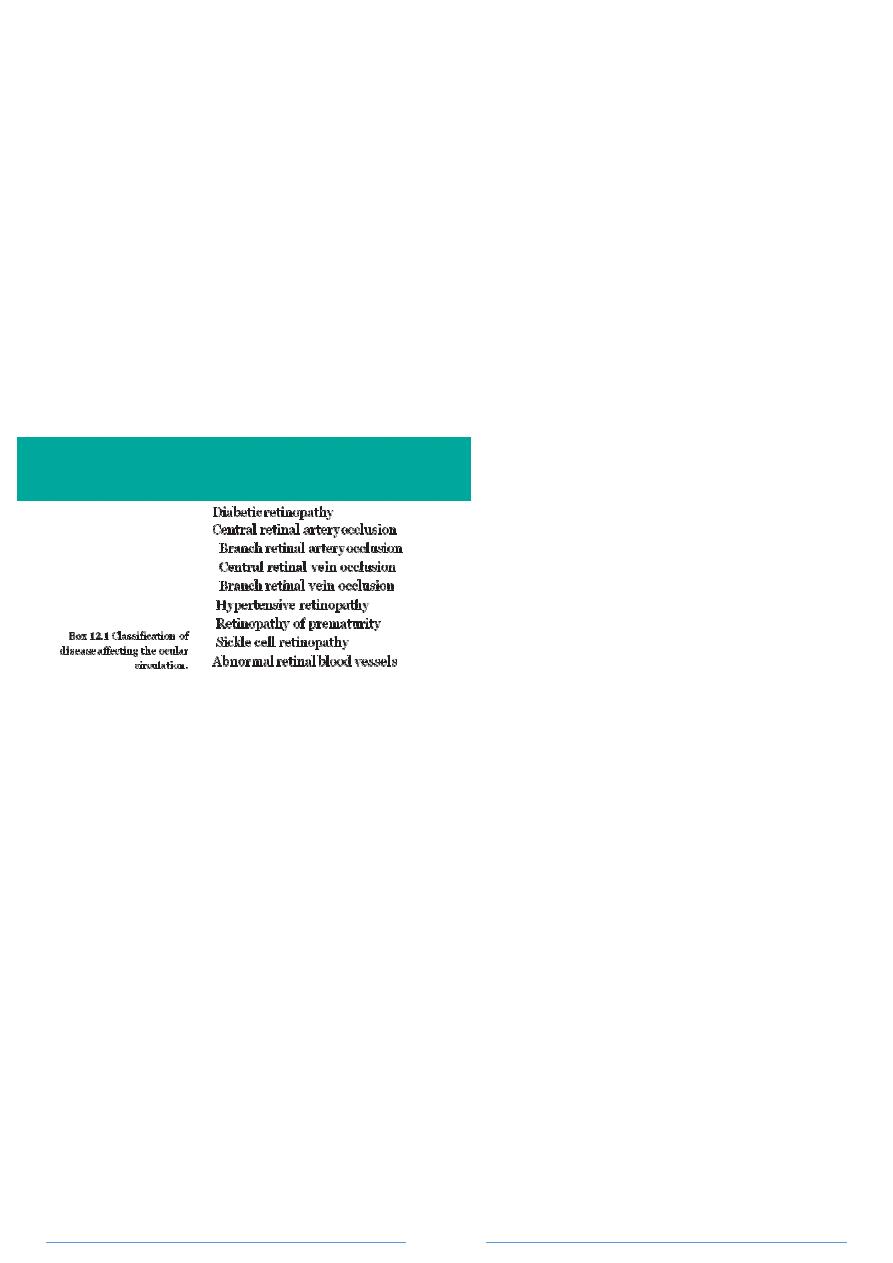
EXAMINATION
The building blocks of the disease are those of leakage and microvascular occlusion
discussed earlier .The classification of retinopathy is shown in Table 12.1 .
Page 4
TREATMENT
Patients with a maculopathy ،preproliferative or proliferative retinopathy or worse
require referral to an ophthalmologist .Any patient with unexplained visual loss should
also be referred .The mainstay of treatment for sight threatening diabetic retinopathy is
the laser .A fluorescein angiogram may be performed in some patients to assess the
degree of retinal ischaemia and to pinpoint areas of leakage both from microaneurysms
and new vessels .
Laser treatment of both the maculopathy and new vessels can be performed on an
outpatient basis .
• Diabetic maculopathy is treated by aiming the laser at the points of leakage .The
exudate is often seen to be in a circinate pattern with the focus of leakage or
microaneurysm in the middle .If effective the retinal oedema and exudate will
resorb although this may take some months .
• Optic disc and retinal new vessels are treated with scattered laser burns to the
entire retina leaving an untreated area around the macula and optic disc
) Fig.
12.4 .(The laser treatment eliminates ischaemic retina thus preventing the release
of vasoproliferative factors .This results in the regression of the new vessels and
prevents the development of advanced retinopathy .
•
•
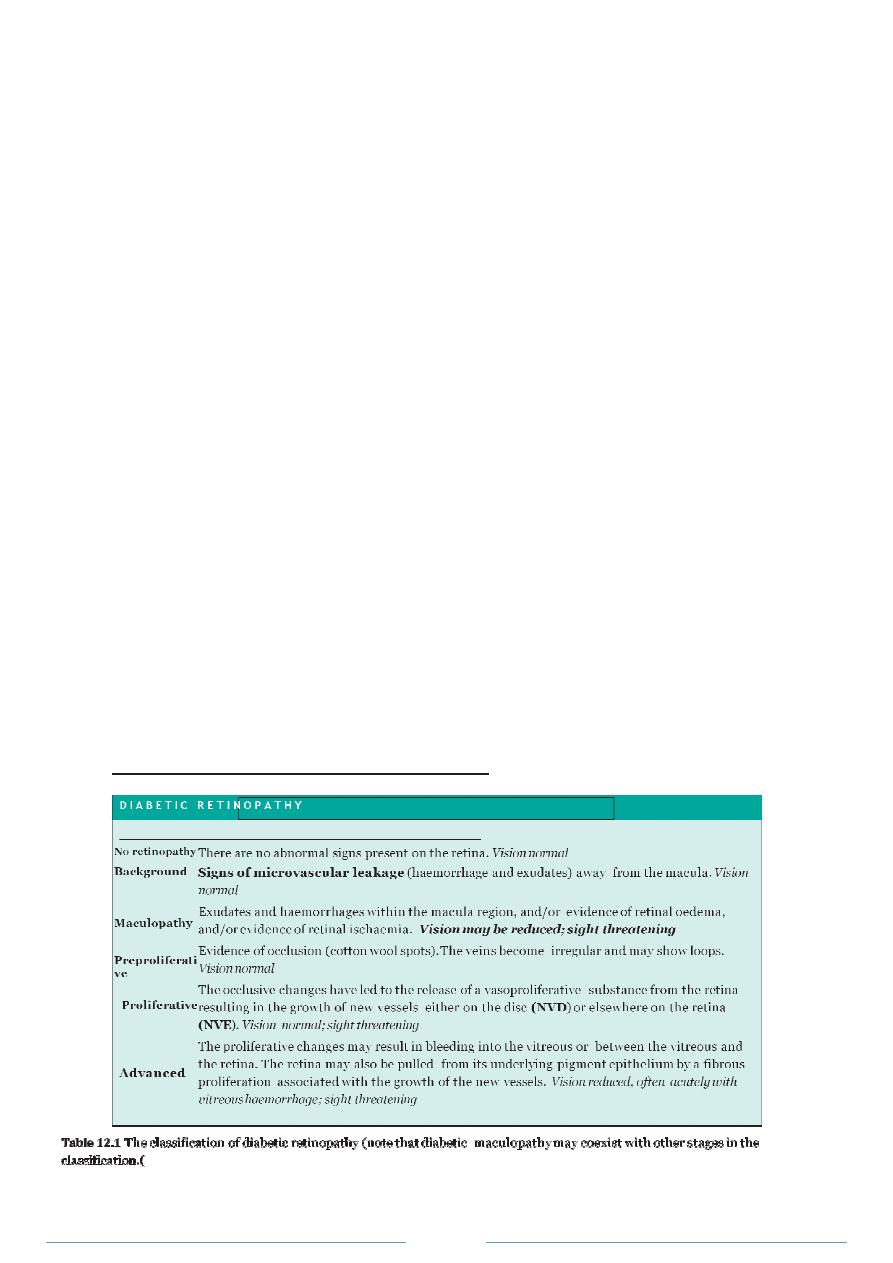
Fig .12.3 The signs of diabetic eye disease
( a) Background diabetic retinopathy .(b )Diabetic maculopathy ،note the
circinate exudate temporal to the macula
( c
) Preproliferative retinopathy with a venous loop
( d, e )Proliferative
retinopathy .New vessels have formed on the retina ،their
•
•
presence is demonstrated by leakage of fluorescein
( hyperfluorescence (
) on the fluorescein angiogram .Closure of
some of the retinal capillary network is demonstrated by its failure to fill with fluorescein
( f
) Advanced diabetic
retinopathy ،the neovascularization has caused a traction retinal detachment .

Page 5
Fig
.
٤.٢١
Typical appearance of retinal laser burns .
The development of vitreous haemorrhage which does not clear after a few months or
fibrous traction on the retina causing detachment from the underlying pigment
epithelium
) tractional retinal detachment (may require surgical treatment .A vitrectomy
is performed to remove the vitreous gel and blood and repair any of the detached
retina .
PROGNOSIS
Although laser and surgical treatments have greatly improved the prognosis of patients
with diabetic retinopathy the disease may still cause severe visual loss in some patients .
ARTERIAL OCCLUSION :
PATHOGENESIS
Central and branch retinal artery occlusions are usually embolic in origin .Three types of
emboli are recognized :
1 fibrin-platelet
emboli commonly from diseased carotid arteries ؛
2 cholesterol
emboli commonly from diseased carotid arteries
) Fig
.
٥.٢١
(
؛
3 calcific
emboli from diseased heart valves .
HISTORY :
The patient complains of a sudden painless loss of all or part of the vision .Fibrin
platelet emboli typically cause a fleeting loss of vision as the emboli passes through the
retinal circulation
) amaurosis
fugax .(This may last for some minutes and then clears .
Cholesterol and calcific emboli may result in permanent obstruction with no recovery in
vision
) they may also be seen in the retinal vessels of asymptomatic individuals .(A central
retinal artery obstruction is frequently caused by an embolus ،although as it lodges
further back in the arterial tree behind the optic nerve head ،it cannot be seen .
In young patients ،transient loss of vision may be caused by migraine .
SIGNS :
Occasionally ،a series of white platelet emboli can be seen passing rapidly through a
vessel ؛more often a bright yellow ،reflective cholesterol embolus is noted occluding an
arterial branch point .The acutely affected retina is swollen and white
) oedematous (
،
while the fovea is red
) cherry
red
spot (as it has no supply from the retinal circulation, is
not swollen ،and the normal choroid can be seen through it .After several weeks the disc
becomes pale
) atrophic (and the arterioles attenuated .The condition may also
occasionally be caused by vasculitis ،such as giant cell arteritis
) see p .160 .(

Page 6
INVESTIGATION :
Patients require a careful vascular work-up since disease in the eye may reflect systemic
vascular disease .A search for carotid artery disease should be made by assessing the
strength of carotid pulsation and listening for bruits .Ischaemic heart disease ،peripheral
claudication and hypertension may also be present .
A carotid endarterectomy may be indicated to prevent the possibility of a cerebral
embolus if a stenosis of the carotid artery greater than 75 %is present .Doppler
ultrasound allows non-invasive imaging of both the carotid and vertebral arteries to
detect such a stenosis .
TREATMENT
:
Acute treatment of central and branch artery occlusions is aimed at dilating the arteriole
to permit the embolus to pass more distally .Results are usually disappointing although a
trial is worthwhile if the patient is seen within 24 hours of onset of the obstruction .The
patient is referred to an eye unit where the following measures may be tried :
• lowering the intraocular pressure with intravenous acetazolamide ؛
• ocular massage ؛
• paracentesis
) a needle is inserted into the anterior chamber to release aqueous
and lower the intraocular pressure rapidly (
؛
• getting the patient to rebreath into a paper bag firmly applied around the mouth
and nose to use the vasodilatatory effect of raised carbon dioxide levels .
PROGNOSIS
Full visual recovery occurs with amaurosis fugax but more prolonged arterial occlusion
results in severe unrecoverable visual loss .
VENOUS OCCLUSION
:
PATHOGENESIS
Central retinal vein occlusion
) CRVO (may result from :
• abnormality of the blood itself
) the hyperviscosity syndromes and abnormalities in
coagulation (
؛
• an abnormality of the venous wall
) inflammation (
؛
• an increased ocular pressure.
• Systemic Arterial Hypertension
HISTORY
:
The patient complains of a sudden partial or complete loss of vision although onset may
be less acute than that of arterial occlusion .
SIGNS :
These contrast markedly with those of arterial occlusion .There is marked haemorrhage
and great tortuosity and swelling of the veins .
The optic disc appears swollen .Branch
retinal vein occlusion may originate at the crossing point of an arteriole and a vein
where the arteriole has been affected by arteriosclerosis associated with hypertension
(a/v nipping .
)
Subsequently :
Page 7
• Abnormal new vessels may grow on the retina and optic disc ،causing vitreous
haemorrhage .This happens if the retina has become ischaemic as a result of the
vein occlusion
) an ischaemic retinal vein occlusion .(
• In ischaemic retinal vein occlusion abnormal new vessels may grow on the iris
causing rubeotic glaucoma .
INVESTIGATION :
Investigation of a CRVO includes vascular and haematological work-up to exclude
increased blood viscosity .Central retinal vein occlusion is also associated with raised
ocular pressure ،diabetes and hypertension .
TREATMENT :
Retinal laser treatment is given if the retina is ischaemic to prevent the development
of retinal and iris new vessels
) see glaucoma ،p
.
٤٠١
.(
Laser treatment may improve
vision in some patients with a branch retinal vein occlusion by reducing macular
oedema .
PROGNOSIS :
The vision is usually severely affected in central ،and often in branch ،vein occlusion
and usually does not improve .Younger patients may fare better ،and there may well
be some visual improvement .
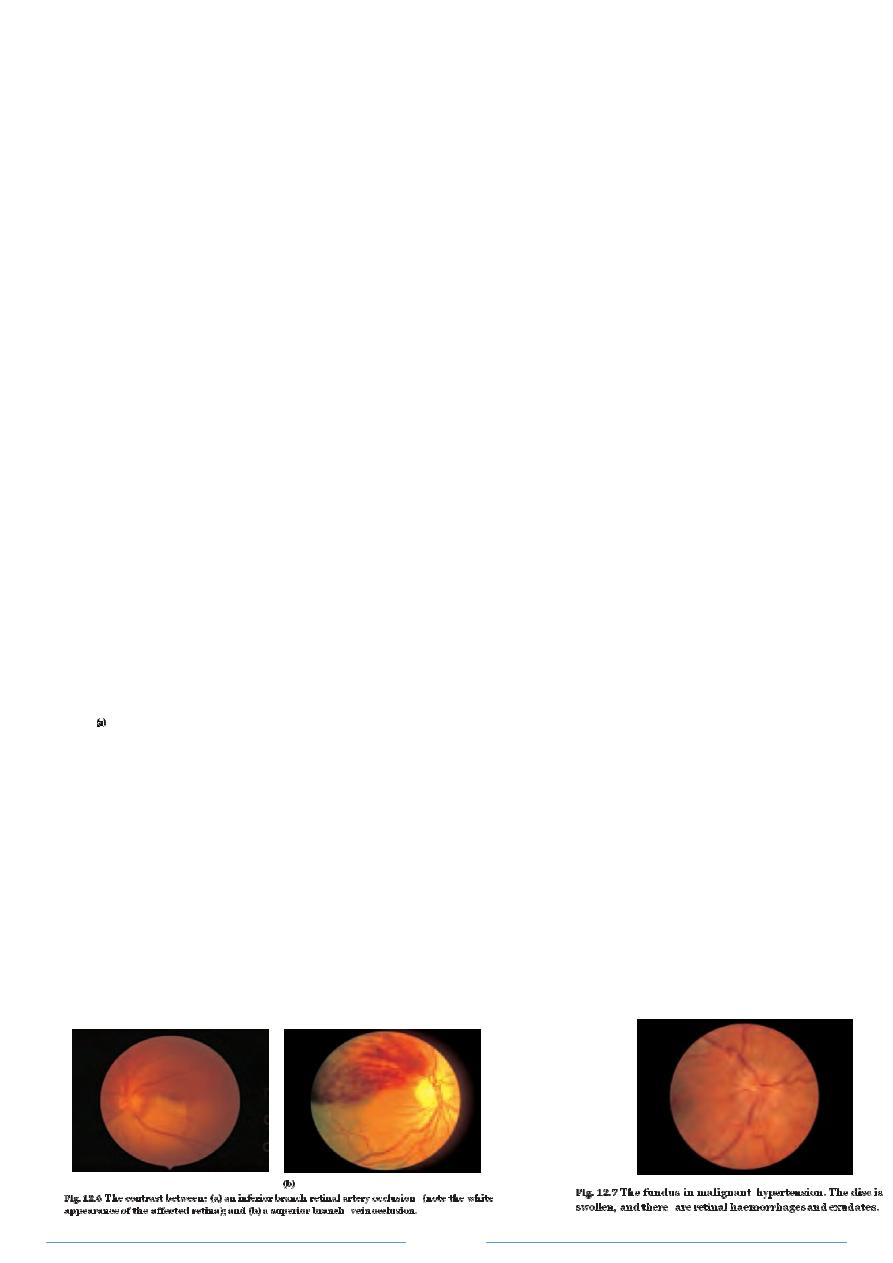
ARTERIOSCLEROSIS AND HYPERTENSION
:
Arteriosclerosis can be visualized in the eye as an attenuation of the
retinal arterial vessels
) sometimes referred to as copper
and silver wiring (and by the
presence of nipping of the retinal vein where it is crossed by an arteriole. Hypertension
in addition may cause focal arteriolar narrowing and a breakdown in the blood retinal
barrier resulting in the signs of vascular leakage
) haemorrhage and exudate .(These are
particularly prominent if the hypertension is of renal origin .If severe the retina may also
demonstrate signs of capillary occlusion
) cotton wool spots). Very high blood pressure
may cause swelling of the optic disc as well as these other signs
) accelerated
hypertension ؛Fig
.
٧.٢١
.(
The patient may complain of blurring of vision and episodes of
temporary visual loss ،though severe retinopathy may also be asymptomatic.
Treatment of the hypertension ،avoiding a rapid reduction which may precipitate vascular
occlusion ،results in the resolution of the retinal signs .This may take some months .

Page 8
RETINOPATHY OF PREMATURITY :
PATHOGENESIS
There is an initial failure of normal retinal vascularization followed by a phase of
aggressive new vessel formation extending forward into the vitreous and causing traction
detachment .
Risk factors associated with retinopathy of prematurity include :
• gestation less than 32 weeks ؛
• birth weight below 1500
i
g ؛
• exposure to supplemental oxygen ؛
• apnoea ؛
• sepsis ؛
• duration of ventilation ؛
• blood transfusion ؛
• the presence of intraventricular haemorrhage ؛
• retinal light exposure .
The incidence of the condition in infants weighing less than 1500
i
g is between 34 and
60 %.
SIGNS
The retinal appearance depends on the severity of the condition but includes :
• new vessels ؛
• the development of retinal haemorrhage ؛
• increased tortuosity and dilation of the retinal vessels .In severe disease blindness
can result from :
• bleeding into the vitreous ؛
• retinal detachment .
TREATMENT
At-risk infants are screened on a regular basis.The severe complications of the condition
can be reduced by applying cryotherapy or laser to the avascular retina .
SICKLE CELL RETINOPATHY :
Signs include :
• tortuous veins ؛
• peripheral haemorrhages ؛
• capillary non-perfusion ؛
• pigmented spots on the retina ؛
• new vessel formation, classically in a ’sea-fan ‘pattern ،which may occur as a result
of peripheral retinal artery occlusion .
New vessels may cause vitreous haemorrhage and traction retinal detachment .As with
diabetes this may require treatment with laser photocoagulation and vitrectomy .
