Infertility
General objectives:Students will gain an appreciation and understanding infertility and know causes and management.
Instructional (Specific) Objectives
After attending lecture, the student will can:Define infertility.
List prerequist for fertilization in male and female.
Know the causes of female infertility.
Discuss history, examination, investigation and treatment.
Know monitoring of patient with ovulation induction
List complications of each type of treatment.
Infertility
Infertility
Infertility is defined as the inability to conceive (become pregnant ) despite regular frequent, unprotected sexual intercourse over a specific period of time, usually either 1 or 2 years.
Peak human fertility (the chance of pregnancy per menstrual cycle in the most fertile couples) is no higher than 33%.
Within a year of regular intercourse, 90% of fertile couples should become pregnant. After two years, this rises to 95%. Thus, 510% of normal fertile couples take more than a year or two to conceive. Some
couples therefore present with a delay in conceiving purely by chance.
infertility classified as:
primary infertility:those who have never conceived in the past and who have regular, unprotected intercourse for 12 months.
Secondary infertility:
Those who have conceived in the past (even though this episode did not result in a live birth, as miscarriage or ectopic pregnancy or Hydatidiform mole) and who have regular, unprotected intercourse for 12 months.Voluntary infertility:
Those who have taken contraception to avoid pregnancy.Requirements for normal fertility:
General factors affecting fertility:
The likelihood of spontaneous live birth in infertile couples is stronglyinfluenced by:
1. female age.
Fertility in women is at it's height in the late teens and early 20s and declines slowly after age of 35 where fertility is halved. Fertility declines sharply after the age of 37.
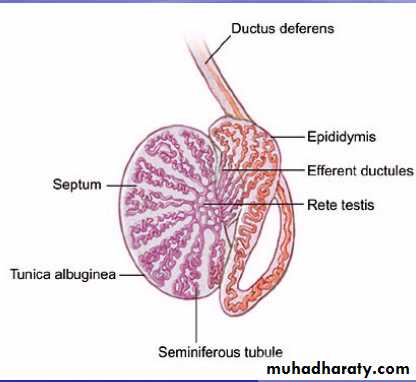
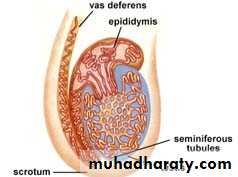
In the male, spermatogenesis commences actively at puberty and continues throughout life, but aging reduces fertility to a variable extent after 60 years.
2. duration of infertility. less than 3years had a better chance of conception.
3. previous pregnancies. A previous full term pregnancy is associated with a better chance of conception, either naturally or after treatment4. cause of infertility.
5. General health and nutrition.( Extremes of weight loss or obesity reduce female fertility).
6. Psychological factors (Anxiety and tension are common in modern life and may exacerbate subfertilitry in some individuals. Stress can cause changes in the neuroendocrine control of ovulation) .
7. Smoking, particularly by women, reduces fertility.
Complications of infertility:
Complications of being infertile on male and female may include:Depression.
Guilt .
Anger.
Stress.
Disappointment.
Resentment.
Blame.
Fear of losing partner because of infertility.
Diminished confidence and self-esteem.
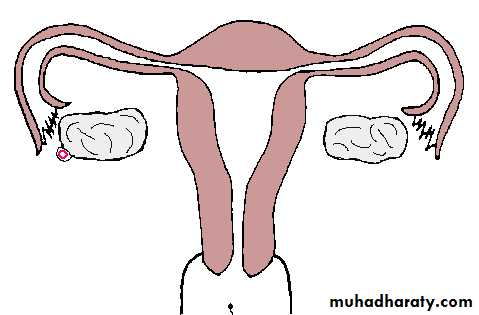
Requirements for normal fertility:
Normal fertility requires :
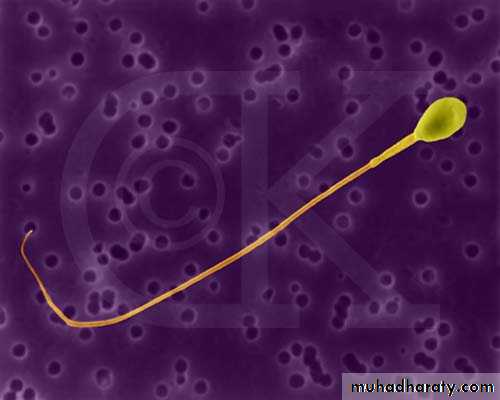
*Production of gametes (gametogenesis).
release of a normal preovulatory oocyte and production of adequate spermatozoa
Requirements for normal fertility:
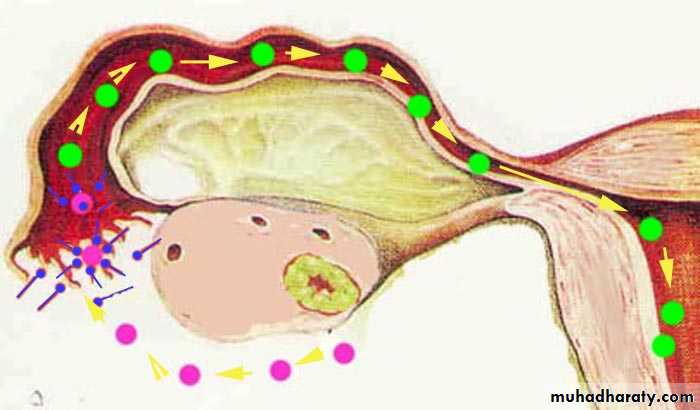
*Their transport to the site of their fusion (gamete transport).Requirements for normal fertility:
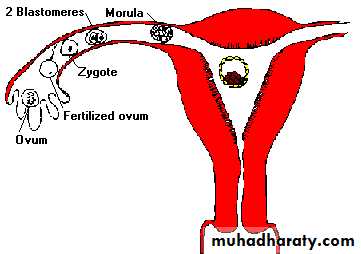
*Appropriate mechanisms for their approximation and fusion (coitus and fertilization).Requirements for normal fertility:
the subsequent transport of the cleaving embryo up to the endometrial cavity for its normal implantation and further development (endometrial preparation). Receptive endometrium to allow the resulting embryo to implant which is limited to days 16-19 (of a 28-day cycle) and it is important that the hatched blastocyst adheres to the endometrium during this time if pregnancy is to occur.Requirements for normal fertility:
Causes of infertility:
To categorize infertility, both partners should be investigated simultaneously.Causes could be due to female cause, male cause , a male and a female factor coincide and the etiology is unknown in 15 % (unexplained infertility) .
Causes of female infertility:Anovulatory infertility:
The cause of anovulation can be classified as:A. group I. Hypogonadotrophic hypoestrogenic (WHO type I):
low FSH, Low oestradiol, normal prolactin. the cause in hypothalamus and pituitary and it is caused by:Kallman’s Syndrome.
Hypothalamic dysfunction secondary to excessive exercise, psychological stress or anorexia nervosa.
pituitary tumour
Pituitary inflammatory reaction as in tuberculosis.
Sheehan's syndrome.
Radiation.
B. group II normogonadotrophic Normoestrogenic (WHO type II):
normal FSH, normal estradiol, normal prolactinOnce hypogonadotrophic and hypergonadotrophic states have been excluded the likely cause of anovulation lies at the level of ovary. Such normogonadotrophic anovulation is usually seen in:
Polycystic ovary syndrome (PCOS).
congenital adrenal hyperplasia,
adrenal tumours
androgen producing ovarian tumours.
C. group III : Hypergonadotrophic hypogonadism WHO type III:
high FSH, low estradiol, normal prolactin
This occur as a result of failure of the ovary to respond to gonadotrophic stimulation by the pituitary gland. There is excessive secretion of FSH and LH. It result from:
Premature ovarian failure.
Resistant ovary syndrome.
Turners Syndrome (XO)
gonadal dysgenesis.
autoimmune disorders.
irradiation or chemotherapy.
unknown cause.
D. Hyperprolactinaemic
low FSH, low estradiol, high prolactin.Increased levels of prolactin interfere with normal pulsatile secretion of GnRH, resulting in anovulation, amenorrhoea and occasionally galactorrhoea associated with low FSH and oestradiol levels. Hyperprolactinaemia is caused by:
prolactin producing pituitary .
primary hypothyroidism
chronic renal failure
drugs (such as the combined oral pill, dopamine depleting agents (reserpine, methyldopa) and dopamine receptor inhibiting agents (metoclopramide and phenothiazines)).
E. Other discrete causes:
Endocrine disordersHypothyroidism (more cases),Hyperthyroidism.
Cushing's syndrome.
Badly controlled diabetes .
Luteinized unruptured follicle :
The dominant follicle is luteinized but remains unruptured and no ovulation will occurred. They may be drug induced (prostaglandin synthetase inhibitors) or associated with endometriosis and can be diagnosed by ultrasound or laproscopy. It may be treatable by administration of human chorionic gonadotrophin at the right time to mimic LH surge.
2. Tubal infertility:
The fallopian tube is more than just a tube, a number of key events occur within the tube including capacitation of sperm, fertilization and the early development of zygote and embryo. Investigations can only test tubal patency but not function.Tubal disease accounts for 15–20% of cases of primary infertility and approximately 40% of secondary infertility.
causes of tubal infertility:
• a. tubal blockage:• causes of tubal blockage:
• * PID mainly by Chlamydia trachomatis in most cases, Gonorrhoea.
• *Pelvic infection or abscess caused by appendicitis, bowel disorder or
• septic abortion.
• *Iatrogenic as in:
• tubal ligation for sterilization.
• As consequence of pelvic surgery.
• *others as:Tuberculosis, schistomiasis, viral infection and Crohn's disease.
b. Endometriosis (Discussed in other lecture).
In severe endometriosis can lead to mechanical tubal damage due to adhesion formation.3. Uterine factor:
*Submucous fibroid
*congenital uterine abnormalities
*endometrial polyps
*Asherman's syndrome(intrauterine adhesion.).(Discussed in other lecture).
*Tuberculous endometritis.
4. Unexplained infertility
Completion of routine investigation of infertility fails to reveal a cause in 15-30% of cases. it dose not indicate absence of a cause, but rather inability to identify it.evaluation of the female partner:History:
History about both wife and her husband must include details about:Important historic points in female:
*Age
*occupation (presence far away from home for a period).
*Duration of infertility.
*Detailed menstrual history.
menarche , Details of the menstrual cycle can help determine whetherthe cycles are ovulatory or anovulatory. A menstrual cycle length of 21
to 35 days suggests ovulatory cycles, as does the presence of
mittelschmerz, dysmenorrhoea.
*Vaginal discharge:
If any character, amount, if associated with irritation or soreness.
*A history of weight changes, hirsutism, frontal balding, and acne, *galactorrhoea should also be addressed.
*Past obstetric history and Prior pregnancies. (if present in details), *history of breast feeding
*Prior contraceptive use (COCP, long acting progestogens, IUD)
*sexual history
Frequency of intercourse and relation to fertile periods.sexual dysfunction as dyspareunia.
the use of lubricants or other products, use of vaginal douches after
intercourse that may impair fertility.
*Gynecologic history (pelvic inflammatory disease (PID), endometriosis, fibroids, cervical dysplasia).
*Previous illness and Medical history. (e.g., genetic disorders, endocrine disorders, diabetes, renal disease).
*surgical history. Surgical operation especially in abdomen and pelvis.
*Drug history (hormone therapy), Substance abuse as caffeine, toxin exposure.
*Previous investigations or treatment of infertility.*A family history is particularly helpful from the woman, as it might suggest a genetic predisposition to polycystic ovary syndrome, endometriosis.
*A complete review of systems may be helpful to identify any endocrinological or immunological problem that may be associated with infertility.
Examination:
Full general examination :physical development, Sign of chromosomal abnormality, evidence of endocrine disorder, body mass index (BMI).
Signs of hyperandrogenism (e.g., hirsutism, acne, clitoromegaly).
Carefully evaluate the thyroid gland to exclude gland enlargement or thyroid nodules.
Breast examination to evaluate breast development and galactorrhoea.
Abdominal examination: scars, tenderness, masses.
Pelvic examination: genital development ,State of introitus, any discharge, any tenderness, size and mobility of uterus, enlargement of ovaries.
Investigations of female
The aim of these investigations is to assess ovulation, tubal patency and uterine factors.Tests for ovulation:
A history of regular periods usually indicates ovulation (not always).Most of the initial investigations for ovulatory disorder must be undertaken at specific stages of the menstrual cycle.
Tests for ovulation:
1. Mid-luteal phase is approximately 7 days before the next expected period, i.e. day 21 and day 28 in 28-day and 35-day cycles respectively. it is a reliable, safe and inexpensive test. Levels in excess of 30nmol/L are diagnostic of ovulation. Lower level may be due to incorrect timing of blood sampling or may be caused by a luteinized unruptured follicle.Tests for ovulation:
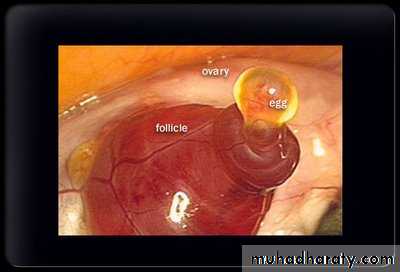
2. ultrasound examination:Vaginal ultrasound can be used to demonstrate the development of a follicle within the ovary (Follicular tracking by ultrasound).
Detailed ultrasound scan performed between days 10-12 will establish follicular and endometrial maturity. The endometrium reflects the local and systemic action of reproductive steroid hormones measuring up to 8-10 mm in late follicular phase. measuring up to 14 mm in the mid-luteal phase.
Tests for ovulation:
Dominant follicle can be seen and its daily increase in size (about 2 mm/ day). A sudden reduction in size around the expected mid-cycle (from about 20-25 mm) is suggestive of rupture of dominant follicle and release of oocyte occurred. Confirmation of ovulation can only be established with serial scans.Failure of oocyte release known as lutinized unruptured follicle syndrome. It may be treatable by administration of human chorionic gonadotrophin at the right time to mimic LH surge.
Tests for ovulation:
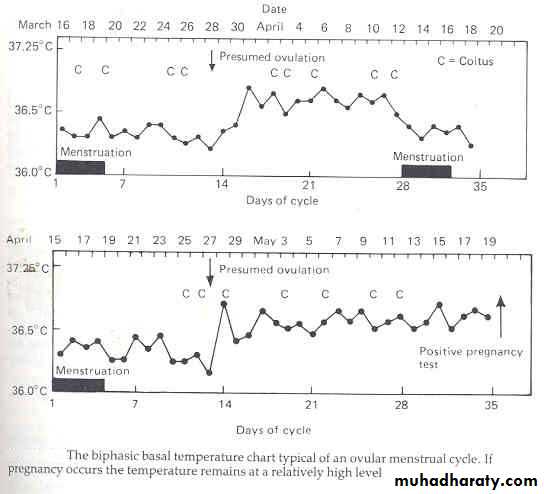
3. basal body temperature.
Women take her basal body temperature each day with special thermometer and write it down on a chart. Immediately before ovulation, the temperature drops briefly. Within 12 hours of ovulation the BBT rises slightly, of about 0.5° c due to progestron secretion and this is fertile period in which intercourse encouraged.
Tests for ovulation:
4. LH detection kits:serial measurement of urinary luteinizing hormone using home prediction kit. A system of hormone monitoring designed to better define the fertile period involves placement of disposable test sticks in a small battery powered device to detect urinary estrone-3 glucuronide and LH. This device (Persona) can serves as both an aid to fertility and a form of contraception
Tests for ovulation:
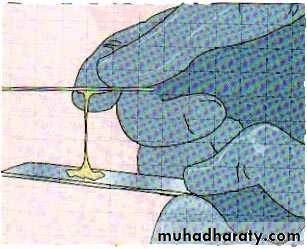
5. Change in cervical mucus:Dominant follicle release estrogen and cause a profound transient change in cervical mucus. Mucus become more copious, less viscous in consistency, increase in stringiness (spinnbarkheit) and become a cellular with decrease in cross-linking of mucine molecules. Once ovulation has occurred and progesterone level rise mucus become scanty, viscid and cellular.
There is no justification for routine assessment of FSH, LH, prolactin and thyroid function in ovulatory women.
Test for anovulation:
1. assess ovarian reserve (women older than 35 years) by:measurement of FSH and estradiol levels on (day 1-3) of the menstrual cycle.
clomiphene citrate (Clomid) challenge test,
transvaginal ultrasonography for antral follicle count
Test for anovulation:
2. Prolactin level.(level > 1000µu/L are significant and needs CT scan of pituitary fossa).3. Thyroid function test.
There is no value in measuring thyroid function or prolactin in women with a regular menstrual cycle, in the absence of galactorrhoea or symptoms of thyroid disease .
Test for anovulation:
4. testosterone (if hyperandrogenism suspected).5. 17alpha-hydroxyprogesterone (if hyperandrogenism suspected),
Tubal patency tests:
Once preliminary investigations suggest that a woman is ovulating and semen parameters are satisfactory, the next step should be assessment of tubal status. It can be assessed by three different methods:a. Hystrosalpingography
b. laproscopy and dye hydrotubation.
c. ultrasound and dye hydrotubation.
a. Hysterosalpingogram (HSG)
A radio-opaque contrast medium is injected through cervix into the uterus under X- ray control to assess uterine cavity and patency of fallopian tubes by seeing free spill into peritoneal cavity. It is usually carried out in first 10 days of menstrual cycle in order to avoid disruption of an early pregnancy. It will cause period-like pain.
Test preceded by taking cervical swabs for Chlamydia in any patient before carrying intrauterine instrumentation. Some physicians prescribe several days of antibiotics for their patients to attempt to reduce the risk of infection after HSG.
Complications with a hysterosalpingogram:
1. allergic reaction to the dye(manifests as a rash), which is uncommon.2. Vasovagal attack.
3. flare up of pelvic inflammatory disease( PID).
4.Pelvic infection.
5. uterine perforation (very uncommon).
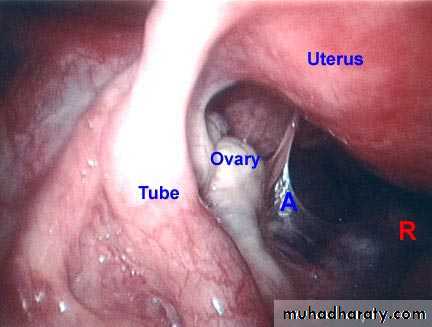
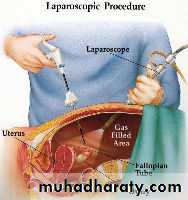
b. Laparoscopy and chromotubation (Laproscopy and dye test):
It is the investigation of choice as it is able to demonstrate tubal patency (Visualize the passage of methlene blue dye through fallopian tubes) aswell as assess the pelvis for the presence of endometriosis and adhesions.
it is indicated in:
1.Women with history of pelvic pain and inconclusive HSG.2. Patient with history suggestive of endometriosis, previous PID or previous pelvic surgery.
3. Abnormal result of HSG.
4. Unexplained infertility.
c. Ultrasound scan and hydrotubation:
(Hysterosalpingo contrast sonography (HyCoSy)):Contrast medium is slowly injected into uterine cavity under direct visualization of ultrasound, with imaging of uterine cavity and of flow along the fallopian tubes and avoid exposure to X-rays.
Assessment of uterus:
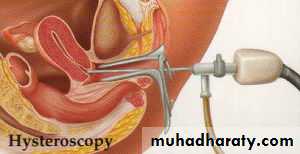
Transvaginal pelvic ultrasound (TVS): enables pelvic structures to be visualized and provides more information than a bimanual examination. It can identify endometrioma, ovarian cysts, polycystic ovaries, fibroids and hydrosalpinges.Uterine anatomy can be visualized by Hysterosalpingography or Hysterosalpingo contrast sonography or Hysteroscopy:
hysteroscopy is useful for diagnosis and treatment.
Postcoital test:
It provides information concerning the ability of sperm to penetrate and survive in cervical mucus. It has high false-positive rate and it's result dose not change treatment so it is not recommended in the routine investigation of the infertile couple.Treatment of female infertility:
It should begin with a description of physiology of the cycle, information about the fertile period, life style issues, including advice on smoking.discuss frequency of intercourse.
Correction of coital difficulties:
Treatment of female infertility:
Timed intercourse was found to be the most emotionally stressful activity in the initial infertility evaluation. Although the greatest probability of conception is in the two days before ovulation and the day of ovulation itself, as Sperm survive in the female reproductive tract for up to 72 hours, and an ovum can be fertilized for up to 24 hours after ovulation. It may be counterproductive to restrict intercourse only to this time as semen quality, measured in terms of motility and morphology, declines with >10 days' abstinence. Regular intercourse, e.g. 2-3 times a week, should ensure that intercourse falls within the fertile period.
advice to avoid any lubricant with sexual intercourse and vaginal douching after it.
Treatment of female infertility:
women should be advised to lie on her back for at least 15 minutes after coitus to prevent sudden loss of semen from vagina.Further planning of treatment protocols will depend on the presumed cause of the problem and Treatment policies must be indivualized.
Treatment of female infertility:
Many factors affecting conception rates would include:Female age's
Baseline FSH level. (greated than 10 U/L have poor prognosis)
Previous conception.
Associated sperm dysfunction.
Treatment of female infertility:
Peak human fertility (the chance of pregnancy per menstrual cyclein the most fertile couples) is no higher than 33%, and it is unrealistic to expect a higher chance of pregnancy than this from any fertility treatment.
treatment of anovulatory infertility:
Select method depends on the cause of anovulation.Normalization of body weight in underweight and obese patients can help to regain ovulation without the need for medical intervention.
Ovulation induction
1. medical induction (Fertility drugs):Fertility drugs are the primary treatment for women who are infertile due to ovulation disorders. These medications regulate or induce ovulation. Before starting therapy , the male's semen must be analyzed.
Commonly used ovulation induction drugs ( fertility drugs) include:
Clomiphene citrate (Clomid).
It is non steroidal agent with both oestrogenic and non-oestrogenic properties stimulate the release of FSH and LH, by blocking oestradiol receptors which result in follicle stimulation.it is taken orally usually at 50 mg daily from 2-6 of menstrual cycle and increased up to 150 mg daily if there is no response.Women with PCOS responds to 25mg daily from 2-6 of cycle.
It can be prescribed up to maximum of six cycles if ovulation is occurring. Monitoring of treatment cycles with serial ultrasound scans is recommended.
Risks of treatment and side effect with clomiphene citrate:
Multiple pregnancy.10%Ovarian hyperstimulation syndrome <1%.
visual disturbance.
thickening of cervical
mucus and hot flushes
Other side effects
include abdominal distension (2%), abdominal pain, nausea, vomiting, headache, breast tenderness and reversible hair loss.
Gonadotrophin therapy:
Used in women with Clomiphene-resistant and in Clomiphene-resistant PCOS.It is either :
*FSH (urinary or recombinant) (Gonal-F,). subcutanouslly
*Human menopausal gonadotropin, or hMG (combination of FSH and LH derived from postmenopausal women urine) (Pergonal). intramuscularly directly stimulate the ovaries.
Can be given as daily dose or in alternate daily injection from early follicular phase until follicular maturation is confirmed. Cycles monitored with serial ultrasound scans
Risks:
Multiple pregnancy. Up to 25%.
Ovarian hyperstimulation syndrome.
Gonadotropin-releasing hormone (GnRH) analogs.
Can treat hypothalamic anovulatory cases. Administered with an infusion pump either subcutaneously or intravenously in a pulsataile fashion.Letrozole (Femara).
This drug is in a class of medications called aromatase inhibitors given for women who haven't responded to treatment with clomiphene citrate. The drug's manufacturer has warned doctors not to use the drug for fertility purposes because of possible adverse health effects. These adverse effects may include birth defects and miscarriage.Dopamine agonists:
Anovulation due to hyperprolactinaemia is effectively treated with dopamine agonists. Bromocriptin is an ergot alkaloid with dopaminic properties.It is administered in a daily dose of 1.25mg at bed time with a snack, and
gradually increasing up to 2.5 mg three times a day with food over 2 to 3 weeks.it causes gastrointestinal side effect and hypotension.
Cabergoline and Quinogolide are newer dopamine agonists which have recently been used for treatment of hyperprolactinaemia. they have fewer side effects and longer half-lives and allow a once daily dose for
quinogolide and a twice weekly dose for Cabergoline.
Metformin (Glucophage).
This oral drug is taken to boost ovulation. It's used when insulin resistance is known or suspected.Human chorionic gonadotropin, or hCG (Ovidrel, Pregnyl).
used in combination with clomiphene, hMG and FSH, this drug stimulates the follicle to release its ovum (ovulate).2. surgical induction of ovulation:
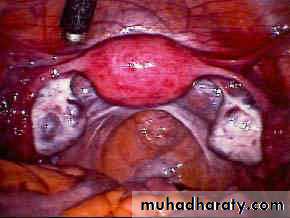
Laparoscopic ovarian drilling in women with poly cystic ovary syndrome (PCOS) .
Management of tubal infertility:
a. Tubal surgery. Has a place in less severe forms of disorder.b. In Vito Fertilization- Embryo Transfer (IVF-ET).
c. selective salpingography and tubal cannulation don at hysteroscopy useful to treat proximal tubal damage.
Management of endometriosis-related infertility: (disscused in endometriosis lecture)
Management of uterine factor infertility:treatment should be considered if failure of implantation seems to be the only cause of an unsuccessful IVF-ET treatment. treatment according to case.
Management of unexplained infertility:
Treatment is empiricalConservative management
Ovulation induction with or without intrauterine insemination.
IVF-ET has diagnostic and therapeutic values as it provides information about fertilization and egg and embryo quality.