
1
Fifth stage
Gynecology
Lec
د
.أحمد جاسم
20/3/2017
Infertility
General objectives:
Students will gain an appreciation and understanding infertility and know causes and
management.
Instructional (Specific) Objectives
After attending lecture, the student will can:
Define infertility.
List prerequist for fertilization in male and female.
Know the causes of female infertility.
Discuss history, examination, investigation and treatment.
Know monitoring of patient with ovulation induction
List complications of each type of treatment.
Infertility :
Infertility is defined as the inability to conceive (become pregnant ) despite
regular frequent, unprotected sexual intercourse over a specific period of time, usually either
1 or 2 years.
Peak human fertility (the chance of pregnancy per menstrual cycle in the most fertile
couples) is no higher than 33%.
Within a year of regular intercourse, 90% of fertile couples should become pregnant.
After two years, this rises to 95%. Thus, 510% of normal fertile couples take more
than a year or two to conceive. Some
couples therefore present with a delay in conceiving purely by chance.
infertility classified as:
primary infertility: those who have never conceived in the past and who have regular,
unprotected intercourse for 12 months.
Secondary infertility: Those who have conceived in the past (even though this episode
did not result in a live birth, as miscarriage or ectopic pregnancy or Hydatidiform
mole) and who have regular, unprotected intercourse for 12 months.
Voluntary infertility: Those who have taken contraception to avoid pregnancy.

2
General factors affecting fertility:
The likelihood of spontaneous live birth in infertile couples is strongly influenced by:
1. female age.
Fertility in women is at it's height in the late teens and early 20s and declines
slowly after age of 35 where fertility is halved. Fertility declines sharply after the
age of 37.
In the male, spermatogenesis commences actively at puberty and continues
throughout life, but aging reduces fertility to a variable extent after 60 years.
2. duration of infertility. less than 3years had a better chance of conception.
3. previous pregnancies. A previous full term pregnancy is associated with a better
chance of conception, either naturally or after treatment
4. cause of infertility.
5. General health and nutrition.( Extremes of weight loss or obesity reduce female
fertility).
6. Psychological factors (Anxiety and tension are common in modern life and may
exacerbate subfertilitry in some individuals. Stress can cause changes in the
neuroendocrine control of ovulation) .
7. Smoking, particularly by women, reduces fertility.
Complications of infertility:
Complications of being infertile on male and female may include:
1. Depression.
2. Guilt .
3. Anger.
4. Stress.
5. Disappointment.
6. Resentment.
7. Blame.
8. Fear of losing partner because of infertility.
9. Diminished confidence and self-esteem.
3
Requirements for normal fertility:
Normal fertility requires :
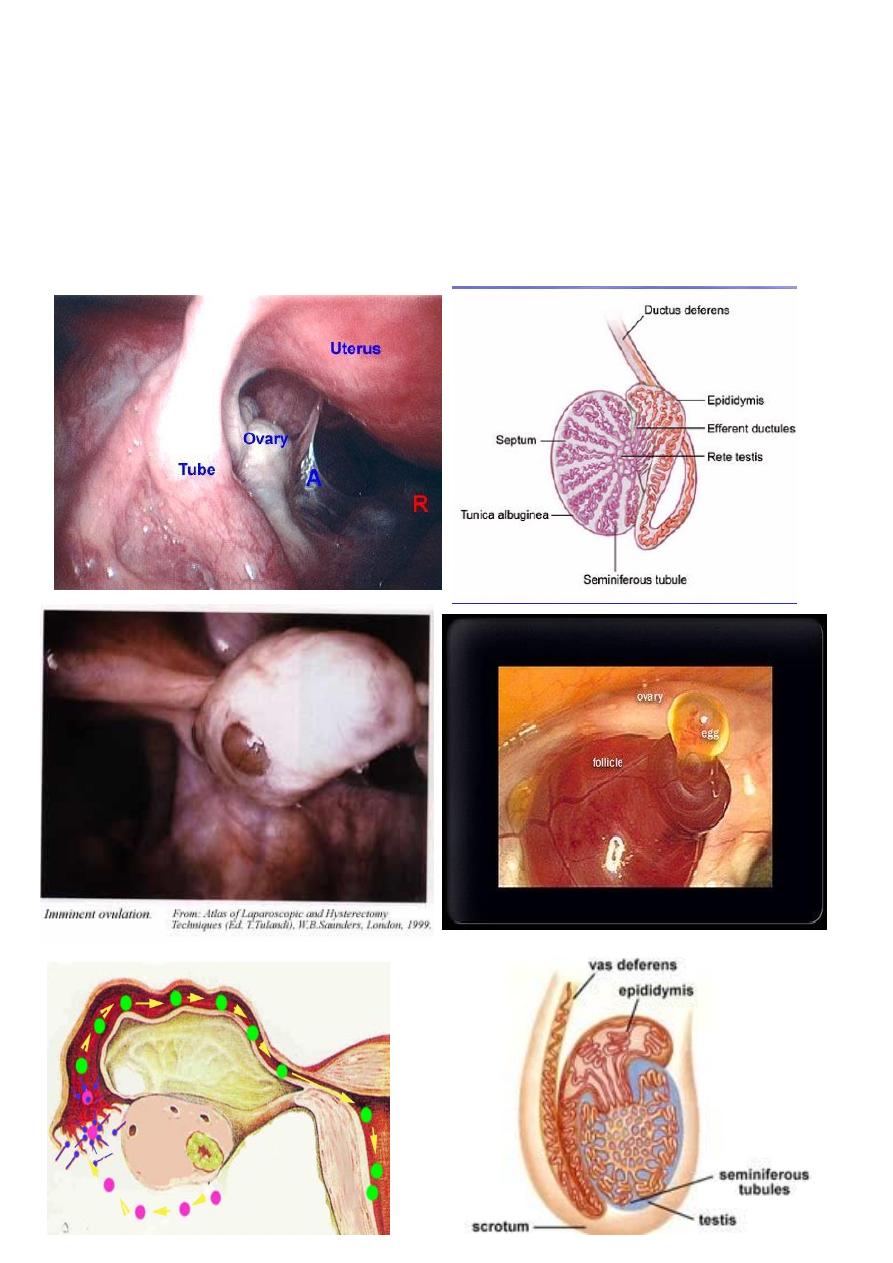
*Production of gametes (gametogenesis).
release of a normal preovulatory oocyte and production of adequate spermatozoa
Their transport to the site of their fusion (gamete transport).
Appropriate mechanisms for their approximation and fusion (coitus and fertilization).
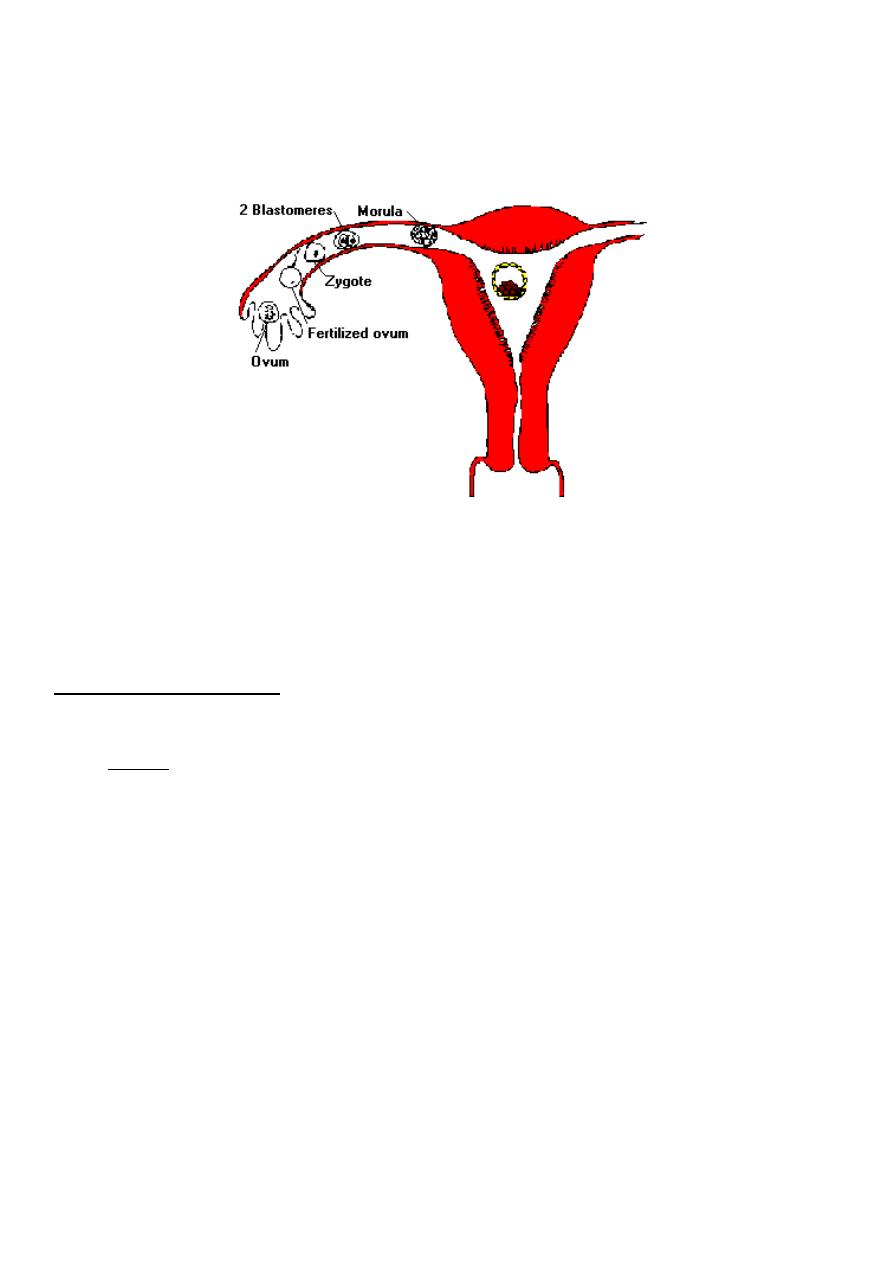
4
the subsequent transport of the cleaving embryo up to the endometrial cavity for its
normal implantation and further development (endometrial preparation). Receptive
endometrium to allow the resulting embryo to implant which is limited to days 16-19
(of a 28-day cycle) and it is important that the hatched blastocyst adheres to the
endometrium during this time if pregnancy is to occur.
Causes of infertility:
To categorize infertility, both partners should be investigated simultaneously.
Causes could be due to female cause, male cause , a male and a female factor coincide
and the etiology is unknown in 15 % (unexplained infertility) .
1- Anovulatory infertility
The cause of anovulation can be classified as:
A. group I. Hypogonadotrophic hypoestrogenic (WHO type I):
.low FSH, Low oestradiol, normal prolactin,
the cause in hypothalamus and pituitary and it is caused by:
1. Kallman’s Syndrome
2. Hypothalamic dysfunction secondary to excessive exercise, psychological stress or
anorexia nervosa.
3. pituitary tumour
4. Pituitary inflammatory reaction as in tuberculosis.
5. Sheehan's syndrome.
6. Radiation.
5
B. group II : Normogonadotrophic Normoestrogenic (WHO type II):
, normal FSH, normal estradiol, normal prolactin .
Once hypogonadotrophic and hypergonadotrophic states have been excluded the likely
cause of anovulation lies at the level of ovary. Such normogonadotrophic anovulation is
usually seen in:
1. Polycystic ovary syndrome (PCOS).
2. congenital adrenal hyperplasia,
3. adrenal tumours
4. androgen producing ovarian tumours.
C. group III : Hypergonadotrophic hypogonadism (WHO type III):
. high FSH, low estradiol, normal prolactin .
This occur as a result of failure of the ovary to respond to gonadotrophic stimulation by
the pituitary gland. There is excessive secretion of FSH and LH. It result from:
1. Premature ovarian failure.
2. Resistant ovary syndrome.
3. Turners Syndrome (XO)
4. gonadal dysgenesis.
5. autoimmune disorders.
6. irradiation or chemotherapy.
7. unknown cause
D. Hyperprolactinaemic
. low FSH, low estradiol, high prolactin .
Increased levels of prolactin interfere with normal pulsatile secretion of GnRH, resulting
in anovulation, amenorrhoea and occasionally galactorrhoea associated with low FSH and
oestradiol levels. Hyperprolactinaemia is caused by:
1. prolactin producing pituitary .
2. primary hypothyroidism
3. chronic renal failure
4. drugs (such as the combined oral pill, dopamine depleting agents (reserpine,
methyldopa) and dopamine receptor inhibiting agents (metoclopramide and
phenothiazines)).
6
E. Other discrete causes:
Endocrine disorders
1. Hypothyroidism (more cases),Hyperthyroidism.
2. Cushing's syndrome.
3. Badly controlled diabetes .
Luteinized unruptured follicle :
The dominant follicle is luteinized but remains unruptured and no ovulation will
occurred. They may be drug induced (prostaglandin synthetase inhibitors) or
associated with endometriosis and can be diagnosed by ultrasound or laproscopy. It
may be treatable by administration of human chorionic gonadotrophin at the right time
to mimic LH surge.
2. Tubal infertility
:
The fallopian tube is more than just a tube, a number of key events occur within the
tube including capacitation of sperm, fertilization and the early development of zygote
and embryo. Investigations can only test tubal patency but not function.
Tubal disease accounts for 15–20% of cases of primary infertility and approximately
40% of secondary infertility.
causes of tubal infertility
:
a. tubal blockage: causes of tubal blockage:
1. PID mainly by Chlamydia trachomatis in most cases, Gonorrhoea.
2. Pelvic infection or abscess caused by appendicitis, bowel disorder or septic
abortion.
3. Iatrogenic as in:
tubal ligation for sterilization.
As consequence of pelvic surgery
4. others as:Tuberculosis, schistomiasis, viral infection and Crohn's disease.
b. Endometriosis (Discussed in other lecture). In severe endometriosis can lead to
mechanical tubal damage due to adhesion formation.
3. Uterine factor:
1. Submucous fibroid
2. congenital uterine abnormalities
3. endometrial polyps
7
4. Asherman's syndrome(intrauterine adhesion.).(Discussed in other
lecture).
5. Tuberculous endometritis.
4. Unexplained infertility
Completion of routine investigation of infertility fails to reveal a cause in 15-30% of
cases. it dose not indicate absence of a cause, but rather inability to identify it.
Evaluation of the female partner:
History
:
History about both wife and her husband must include details about. Important historic
points in female:
1. Age
2. occupation (presence far away from home for a period).
3. Duration of infertility.
4. Detailed menstrual history.
menarche
Details of the menstrual cycle can help determine whether the cycles are ovulatory
or anovulatory. A menstrual cycle length of 21 to 35 days suggests ovulatory
cycles, as does the presence of mittelschmerz, dysmenorrhoea.
Vaginal discharge: If any character, amount, if associated with irritation or
soreness.
5. A history of weight changes, hirsutism, frontal balding, and acne, *galactorrhoea should
also be addressed.
6. Past obstetric history and Prior pregnancies. (if present in details), *history of breast
feeding
7. Prior contraceptive use (COCP, long acting progestogens, IUD)
8. sexual history
Frequency of intercourse and relation to fertile periods.
sexual dysfunction as dyspareunia.
the use of lubricants or other products, use of vaginal douches after
intercourse that may impair fertility.
9. Gynecologic history (pelvic inflammatory disease (PID), endometriosis, fibroid
cervical dysplasia).

8
10. Previous illness and Medical history. (e.g., genetic disorders, endocrine disorders
,diabetes, renal disease).
11. surgical history. Surgical operation especially in abdomen and pelvis.
12. Drug history (hormone therapy), Substance abuse as caffeine, toxin exposure.
13. Previous investigations or treatment of infertility.
14. A family history is particularly helpful from the woman, as it might suggest a genetic
predisposition to polycystic ovary syndrome, endometriosis.
15. A complete review of systems may be helpful to identify any endocrinological or
immunological problem that may be associated with infertility.
R
