
The Thyroid Gland
M Kamil
Department of Surgery
2016
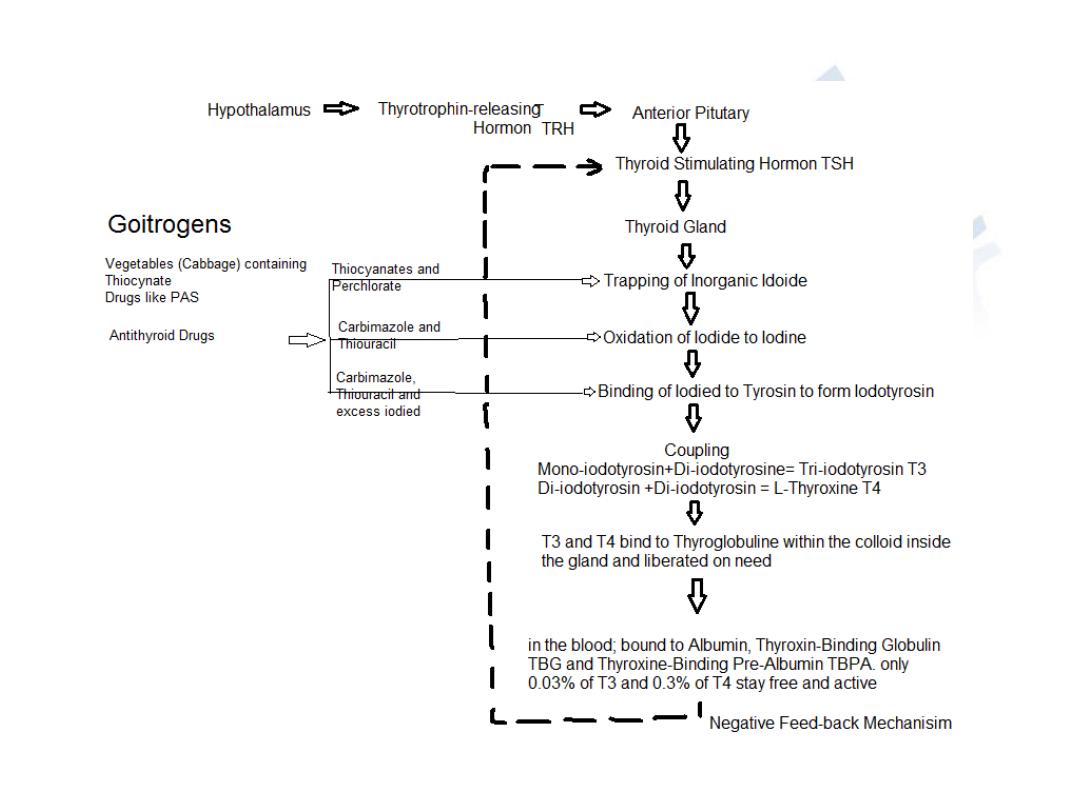
Physiology
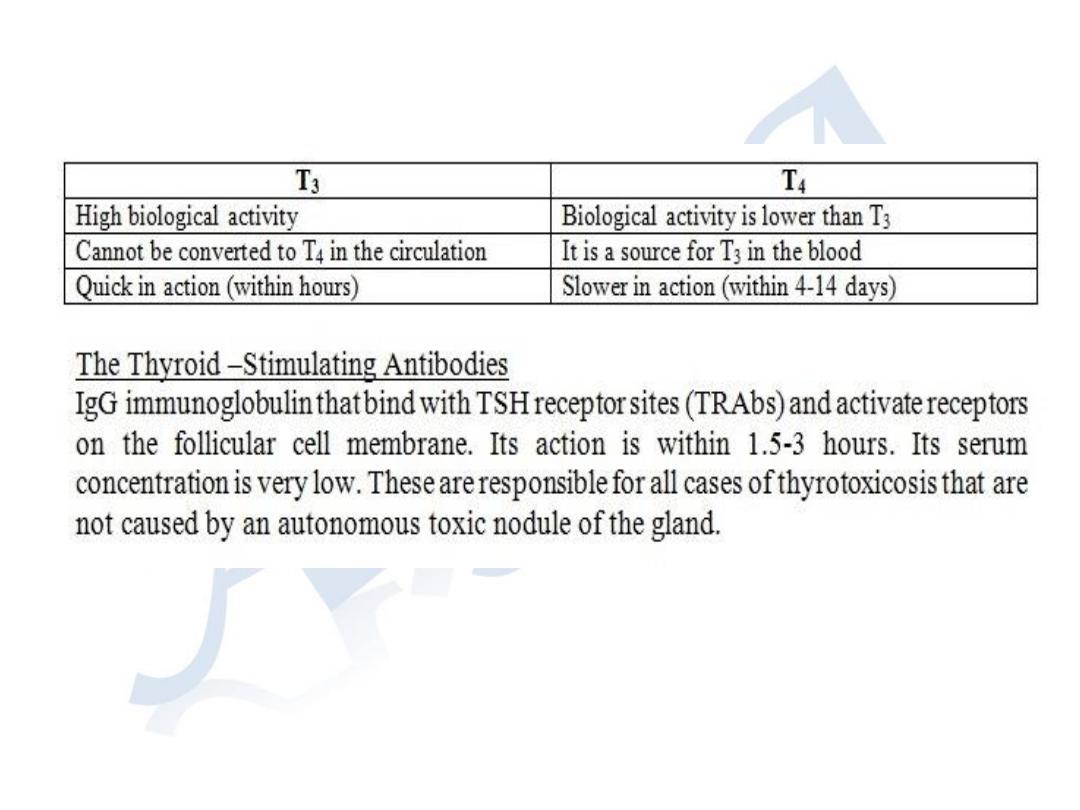
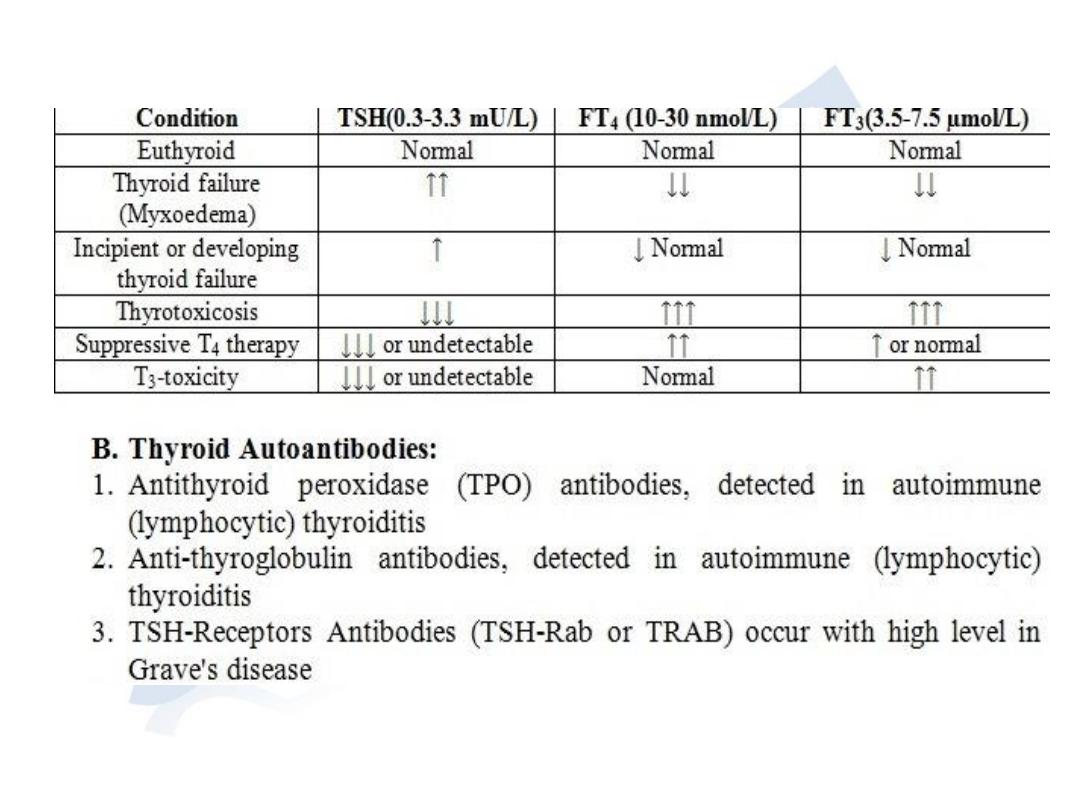
Tests of thyroid function
Investigations
Thyroid imaging:
Chest and thoracic inlet x-ray for:
•
Retrosternal extension
•
Tracheal deviation
•
Pulmonary metastasis
Ultrasound:
•
Nature of thyroid swelling (Solid versus Cystic)
•
For assessment of nodal involvement from thyroid cancer
•
Identification of parathyroid swellings and large adenomas
CT-scan and MRI:
•
Assessment of the extent of retrosternal goitre
•
Assessment of thyroid malignancy
•
Prior to surgery in specific cases of recurrent goitre after resection
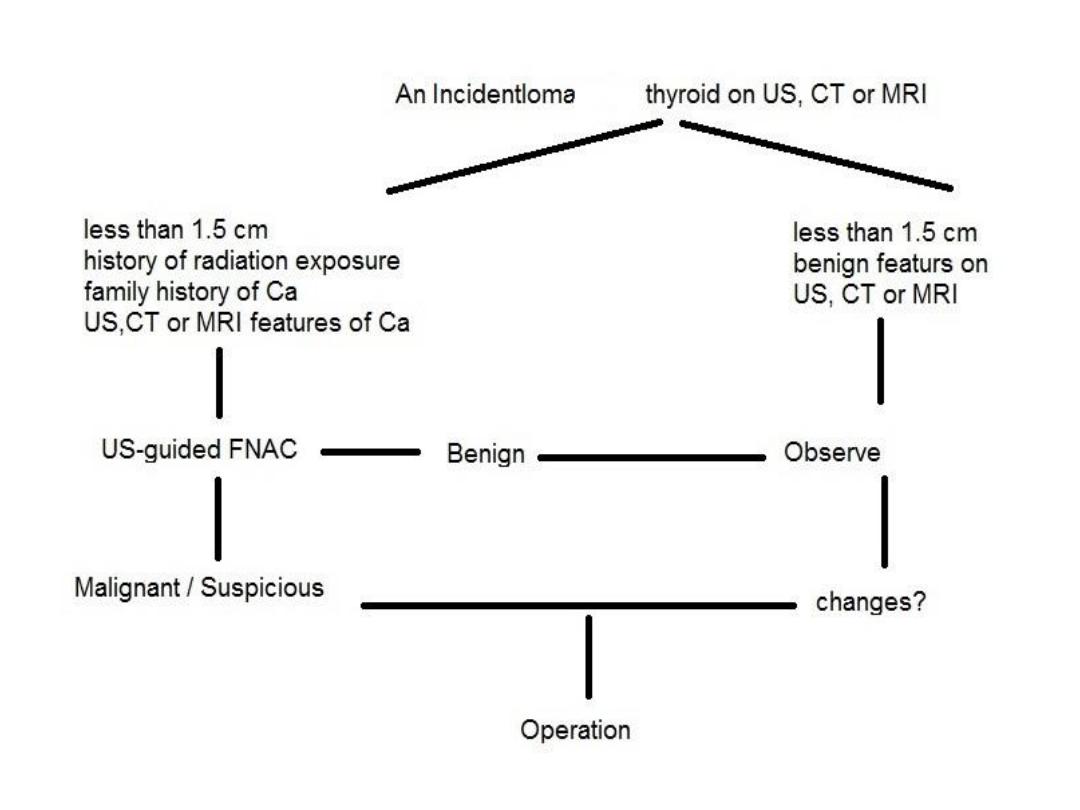
PET/CT scan:
•
For incidental thyroid cancer
•
For recurrent thyroid carcinoma
Investigations
Isotope scanning:
Study the uptake of thyroid tissue for
123
I or
99m
Tc which demonstrate
the activity of the gland. It is used in toxic patient with a nodule or
nodularity of the thyroid. Localization of overactivity helps in
differentiating a toxic nodule with suppression of the rest of the
gland from toxic nodular goitre.
"Cold", no uptake
"Warm", moderate uptake (Normal)
"Hot", high uptake
It has a limited value in malignancy because 80% of cold swellings are
benign and some 5% of active swellings are malignant.
For the use of whole body scan, it is necessary that all active thyroid
tissue have been ablated either by radio-iodine therapy or by total
thyroidectomy. Whole body scan is used principally for detection of
metastatic thyroid tissue.
Investigations
Hypothyroidism
Etiology:
1. Autoimmune (chronic lymphocytic) thyroiditis
A.
No goitre- primary myxoedema
B.
Goitre- Hashimoto's disease
2. Iatrogenic
A.
After thyroidectomy
B.
After
123
I therapy
C.
Drug induced
PAS
Excess Iodide therapy
Antithyroid drugs
3. Others
A.
Endemic Cretinism, often goitreous and due to Iodine
deficiency
B.
Dyshormonogenesis
C.
Secondary to pituitary or hypothalamic disorders
D.
Agenesis of the thyroid gland

Cretinism (Fetal or Infantile hypothyroidism)
Features:
1.
It is the consequence of inadequate
thyroid hormons production during fetal
and neonatal life
2.
The endemic type is due to dietary iodine
deficiency while the sporadic cases are
due to errors of thyroid metabolism or
complete or partial agenesis of the gland
3.
The infant is born with specific features
of hoarse cry, Macroglossia and umblical
hernia
4.
Women on antithyroid drugs may give
birth to a hypothyroid baby and radio-
active iodine therapy is contraindicated
during pregnancy
5.
Immediate diagnosis is possible and the
treatment is thyroxin replacement
therapy.
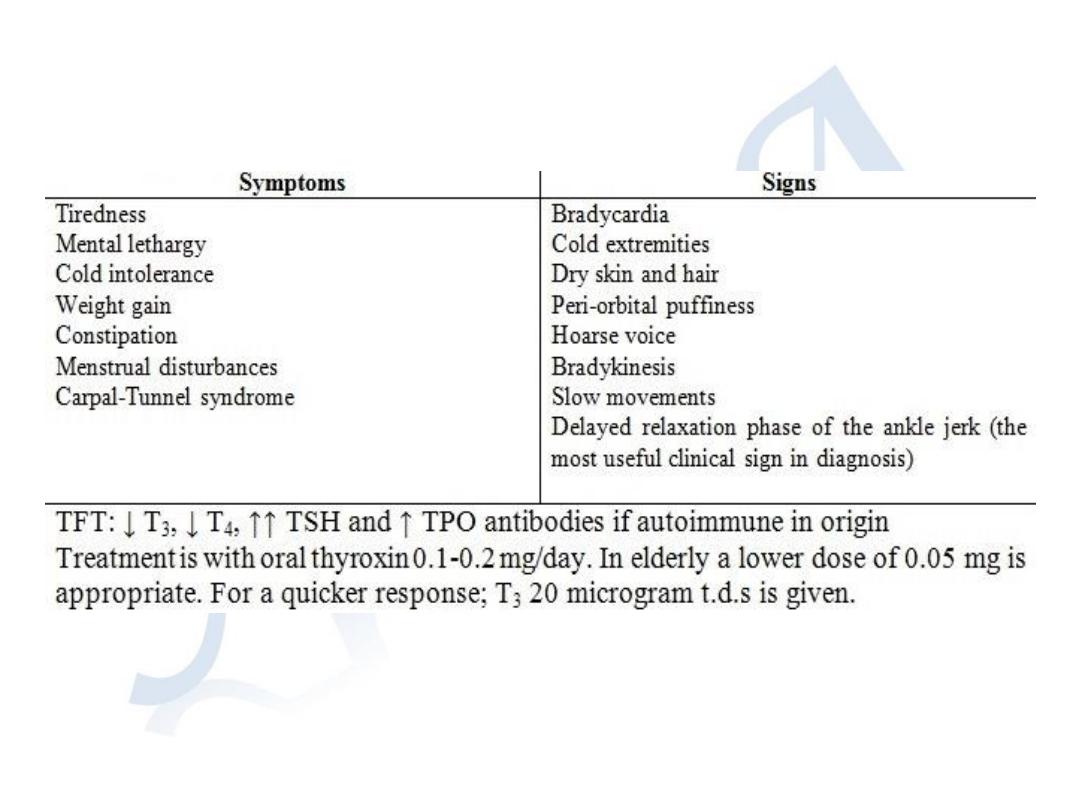
Adult hypothyroidism

Myxoedema
It is the accentuated signs and symptoms of adult hypothyroidism.
Features are:
1)
Typical facial appearance of bloated look, pouting lips and dull
expression
2)
Supraclavicular puffiness
3)
Malar flush
4)
Yellow tinge of the skin
5)
Harsh, slow monotonous voice
Myxoedema coma is the condition describing an altered mental state
and hypothermia precipitated by a comorbid medical condition like
cardiac failure. The treatment is:
1)
Urgent T
4
0.5 mg or T
3
10 microgram i.v 6 hourly
2)
Slow rewarming for severe hypothermia (temp. ˂30
0
C)
3)
i.v broad spectrum antibiotics
4)
i.v hydrocortisone in divided doses

Dyshormonogenesis
Features:
1) Represent a minority of cases of neonatal
hypothyroidism with goitre
2) It is inherited as an autosomal recessive pattern
3) There is a genetic deficiency in the enzyme
controlling synthesis of thyroid hormons
4) A family history is common
5) Classically; TPO deficiency (Pendred's syndrome)
or defective thyroglobulin synthesis is found
Thyroid enlargement
Goitre
generalised enlargement of the thyroid gland.
A
single nodule
(swelling) is a discrete swelling in the thyroid with no other
palpable abnormality.
A
dominant nodule
(swelling) is a palpable swelling with evidence of discrete
swellings elsewhere in the gland.
Classification of thyroid swellings:
Simple goitre
; can be diffuse hyperplastic or multinodular. It can be
physiological, pubertal or occurring due to pregnancy
Toxic goitre
; can be diffuse (Grave's disease, multinodular or a toxic adenoma
Neoplastic
; benign or malignant
Inflammatory
:
• Autoimmune – chronic lymphocytic thyroiditis (Hashimoto's disease)
• Granulomatous-De Quervain's thyroiditis
• Fibrosing- Riedel's thyroiditis
• Infective- acute (bacterial or viral), chronic (TB or syphilis)
• Amyloidosis
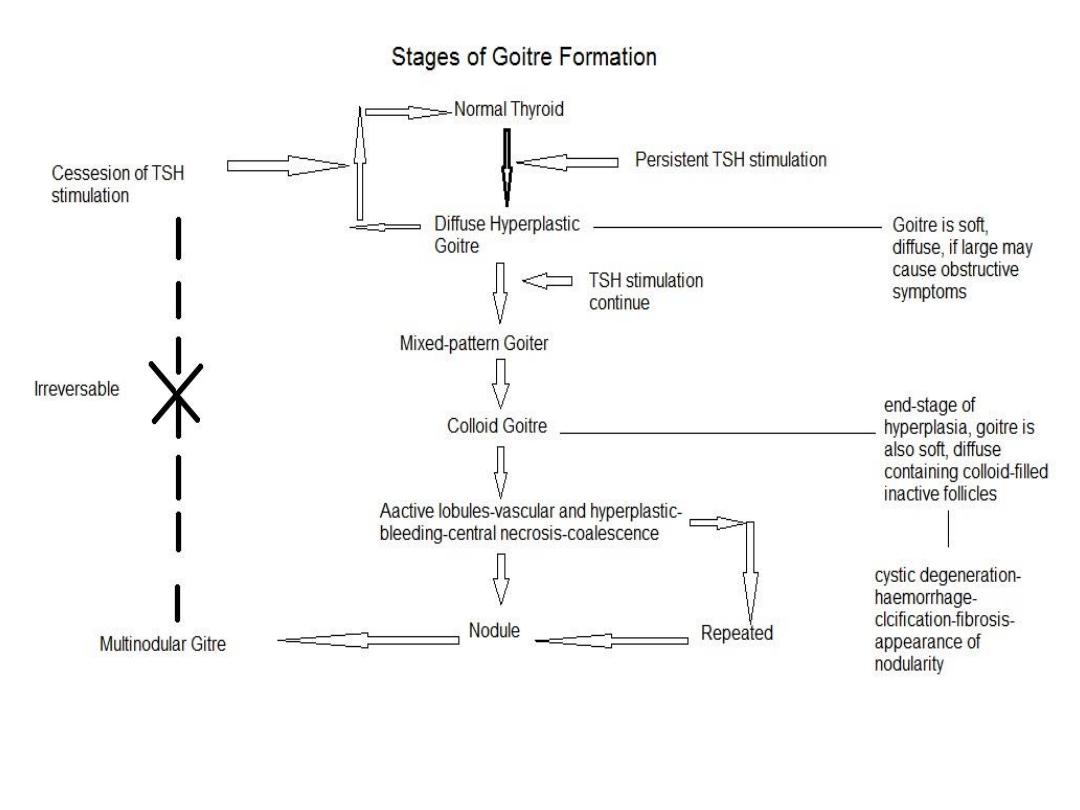
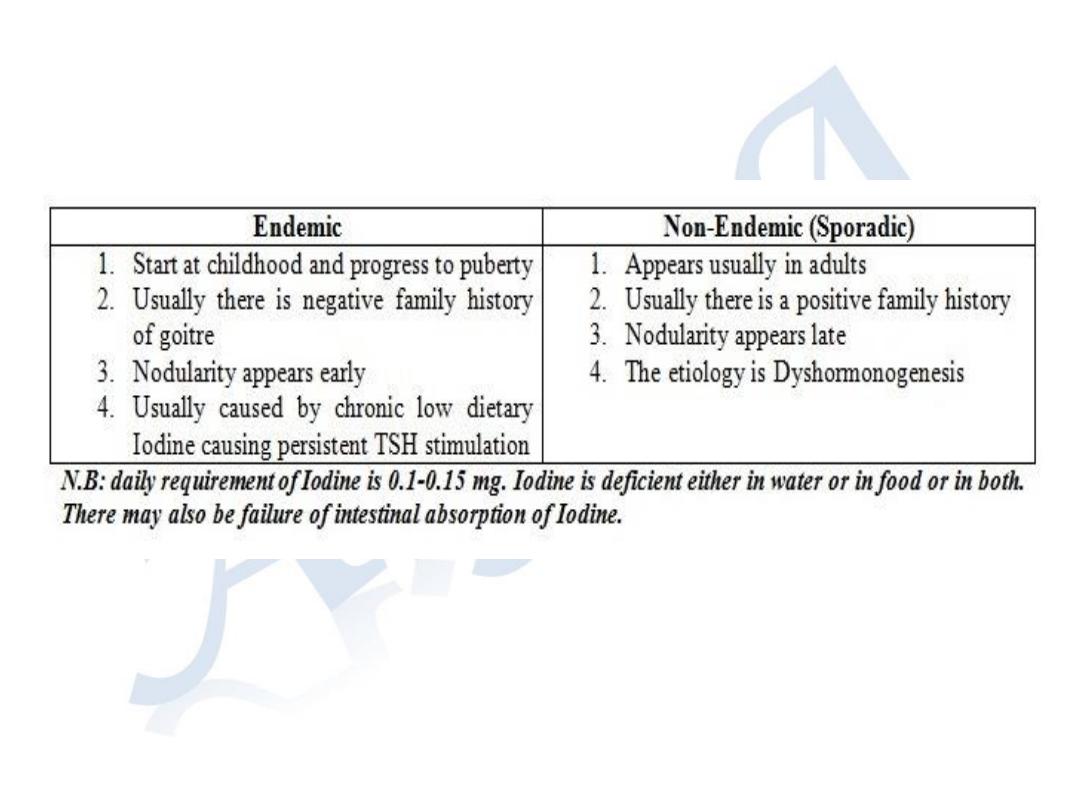
Simple Goitre

Simple Goitre
Clinical diagnosis:
1)
Patient is Euthyroid
2)
Nodules are palpable and often visible
3)
Goitre is usually smooth soft to firm and not hard
4)
It is usually painless
5)
Moves freely on swallowing
6)
Palpable areas of hardness and irregularity are usually due to
calcifications (it need to be differentiated from carcinoma)
7)
Painful nodule is usually due to haemorrhage inside a nodule
8)
Sudden appearance, rapid enlargement and painful nodule indicates that
a carcinoma need to be excluded
Investigations
Complications
1)
Tracheal obstruction by lateral pressure of a large goitre or
anteroposterior compression by retrosternal extension of a goitre
2)
Secondary thyrotoxicosis; usually mild and transient occurring in 1/3 of
cases
3)
Carcinoma; usually of the follicular type in endemic goitre. Dominant,
long standing or rapidly growing nodules should be assessed by FNAC

Simple Goitre
Prevention and treatment of simple goitre:
Endemic goitre is prevented by provision of Iodide salt
Hyperplastic diffuse early goitre may regress with replacement thyroxin therapy (150-
200 µgm Eltroxine tab) for few months
Multinodular goitre is irreversible but the size of nodules may regress on thyroxin
replacement therapy
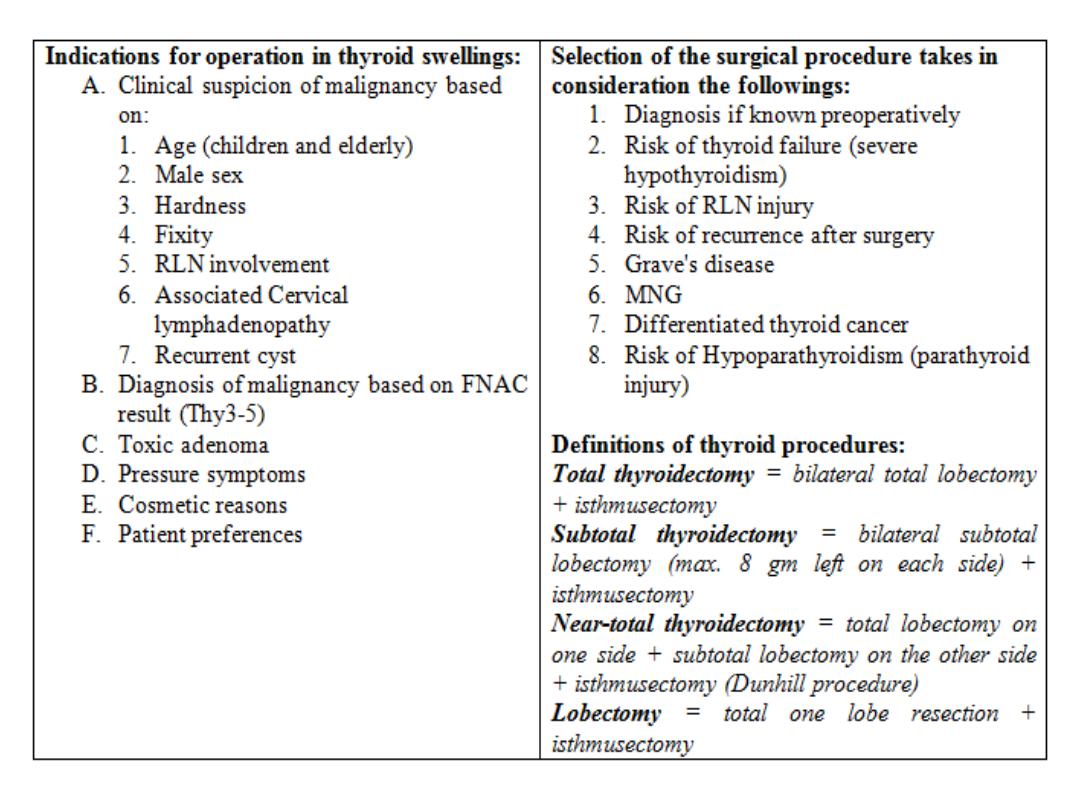
Surgery is indicated in the following circumstances:
1)
On cosmetic grounds
2)
For pressure symptoms of a large or retrosternal goitre
3)
For a dominant nodule and possibility of neoplastic changes
4)
In response to patient anxiety
Options of surgery:
Total thyroidectomy with immediate life-long replacement therapy
Subtotal thyroidectomy and no need to life-long replacement therapy
Total lobectomy plus isthmusectomy for a unilateral lobe enlargement with no
intervention or subtotal resection for the other lobe; it can also be therapeutic for
incidental carcinoma
For recurrent MNG after surgery; reoperation is more difficult and hazardous and
radioactive iodine therapy is a safer option to reduce the size of recurrent goitre
and may be the best for patients with previous multiple thyroid resections
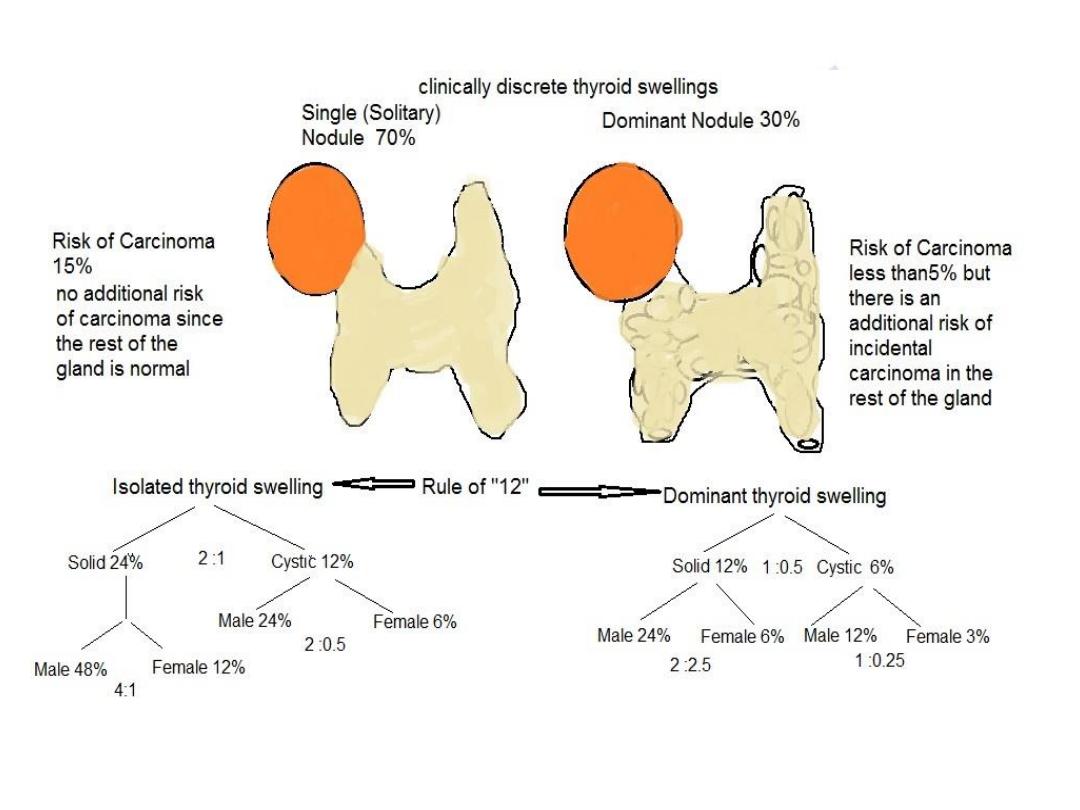

Clinically discrete thyroid swelling
According to the Rule of "12":
The risk of cancer in a thyroid swelling is greater in
Isolated compared with a dominant swelling
The risk is greater in a solid compared with a cystic
swelling
The risk is greater in Men compared with Women
Investigations:
Serum TSH assay and assay of FT
3
and FT
4
Autoantibodies titer
Isotope scan

Clinically discrete thyroid swelling
Ultrasound; determine the physical characteristic of a
thyroid swelling:
1) Detect subclinical nodularity
2) Detect cyst formation
3) Differentiate solid from cystic swellings
4) Aids in localization of FNAC specimen
5) Can help in diagnosing possible Neoplasia by
detecting the following features:
Microcalcifications - suggestive
Increase vascularity - suggestive
Macroscopical capsular breach - diagnostic
Nodal involvement – diagnostic
Clinically discrete thyroid swelling
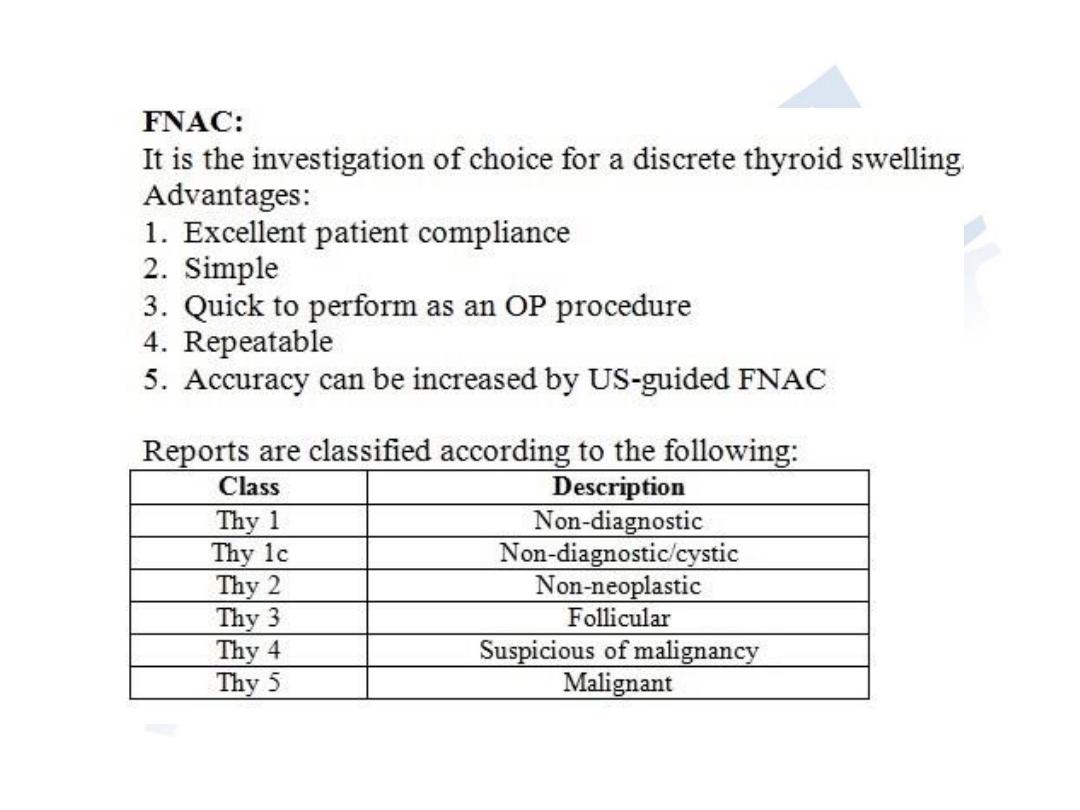
FNAC; features:
1)
Investigation of choice for a discrete thyroid swelling
2)
Simple and quick outpatient procedure
3)
Good patient compliance
4)
Readily repeatable
5)
It can be diagnostic as well as therapeutic like for cystic swelling which do not recur after
aspiration; those which recur should be surgically removed
Limitations:
A.
Cannot distinguish between a benign follicular adenoma and a follicular carcinoma
B.
Few false-positive results with respect to malignancy
C.
False-negative results with respect to benign and malignant swellings
D.
High rate of unsatisfactory aspirate; recently the adoption of US guided FNAC reduced
the rate of unsatisfactory aspirate
Thyroid conditions that can be diagnosed by FNAC include:
Colloid nodules
Thyroiditis
Papillary carcinoma
Medullary carcinoma
Anaplastic carcinoma
Lymphoma

Clinically discrete thyroid swelling
Radiology;
chest and thoracic inlet x-ray
CT and MRI
scanning are useful in assessment of:
•
Retrosternal extension
•
Recurrent swelling
•
Malignancy
PET-CT
scan for localizing tissue that does not take up radioiodine
Flexible laryngoscopy
Core-biopsy (Tru-cut):
•
Take a strip of tissue for histological rather than cytological assessment
•
Has a high diagnostic accuracy
•
Requires local anesthesia
•
May be associated with complications such as pain, bleeding, tracheal and
recurrent laryngeal nerve injury
It is mainly indicated in the following situations:
1)
For locally advance unresectable malignancy like anaplastic carcinoma or
lymphoma to obviate the need for operative biopsy
2)
When FNAC reported as THY 1 inadequate specimen and the risk of malignancy
is low
It is unlikely to be useful in differentiating benign from malignant Thy3( follicular
lesions)

Clinically discrete thyroid swelling
Treatment:
Main indication for surgery is the risk of Neoplasia. There
are relative and strong criteria for surgical removal of
solitary thyroid swellings;
relative
include:
1) Age (young and elderly)
2) Sex; female to male of 3 : 1
3) Patient preference
Strong
criteria include:
1) Hard irregular swelling with any unusual fixity
2) RLN involvement (hoarseness and non-occlusive
cough)
3) Deep cervical lymphadenopathy (suggestive of
papillary carcinoma)

Thyroid cysts
Features:
More than 30% of clinically isolated swellings of the thyroid gland
are cystic or partially cystic (as proved by US or FNAC)
Tense cysts may feel hard and mimic carcinoma
Sudden painful swelling may indicate bleeding in to a cyst.
Aspiration reveals altered blood but re-accumulation is frequent
Around 50% of cysts are the result of colloid degeneration, most of
the reminder represent involution in to a follicular adenoma
10-15% of cystic swellings are histologically malignant. Papillary
carcinoma is often associated with cyst formation
Most of the patients are women 20-40 years old
FNAC is the most appropriate investigation to verify the nature of a
cystic swelling in the thyroid gland. It can be diagnostic and
therapeutic when the cyst disappear but if the cyst recur; excision is
indicated

The Retrosternal Goitre
Retrosternal extensions usually arise from the lower pole of a MNG. If the neck is
short and the pretracheal muscles are strong; the lower pole is drawn down in the
superior mediastinum, enlarge and form the retrosternal part. It may move out of the
retrosternal space by swallowing if the retrosternal extension is short.
Clinical features:
It is often symptomless and discovered on routine chest x-ray
Symptomatic:
1)
Dyspnoea particularly at night
2)
Cough and stridor
3)
Harsh respiratory sounds
4)
Dysphagia
5)
Engorged neck and chest wall veins and there may be signs of superior vena cava
obstruction
Chest and thoracic inlet x-ray show a soft tissue shadow in the superior
mediastinum with calcifications and there may be deviation and compression of
the trachea
CT scan accurately visualize the retrosternal part
Pulmonary Functions Tests may document significant tracheal compression and
can be used to monitor progression of the disease and indicate the need for
surgery. Changes should be reversed by operation

Treatment:
Combined obstructive symptoms with thyrotoxicosis do not
indicate antithyroid drugs or radio-iodine therapy because it
may increase the size of the retrosternal goitre
Surgery is preferable and it can be always performed from the
neck but median sternotomy may be needed
Principles in the surgical procedure that aids resection
include:
1) Cervical part should be mobilized first
2) Isthmus should be divided early
3) Traction helps delivering the retrosternal part of the goitre
4) Bleeding is rarely a problem
5) RLN is particularly endangered and should be identified
6) Any difficulty in mobilisation indicate sternotomy
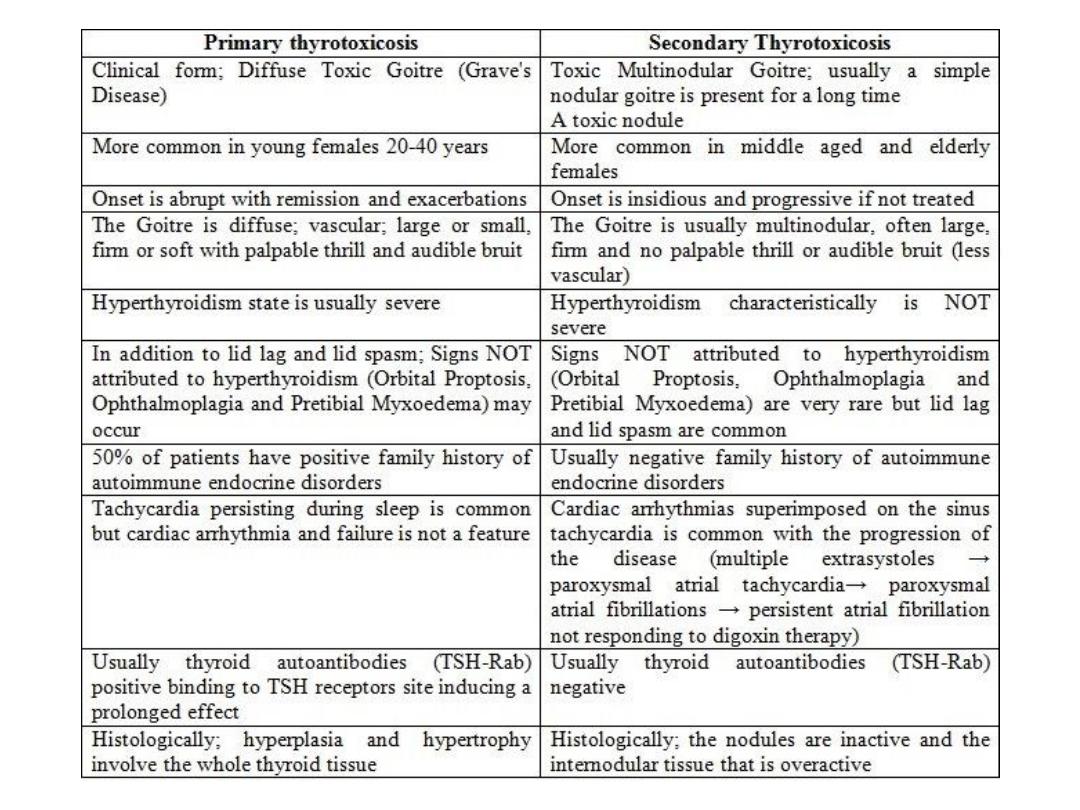
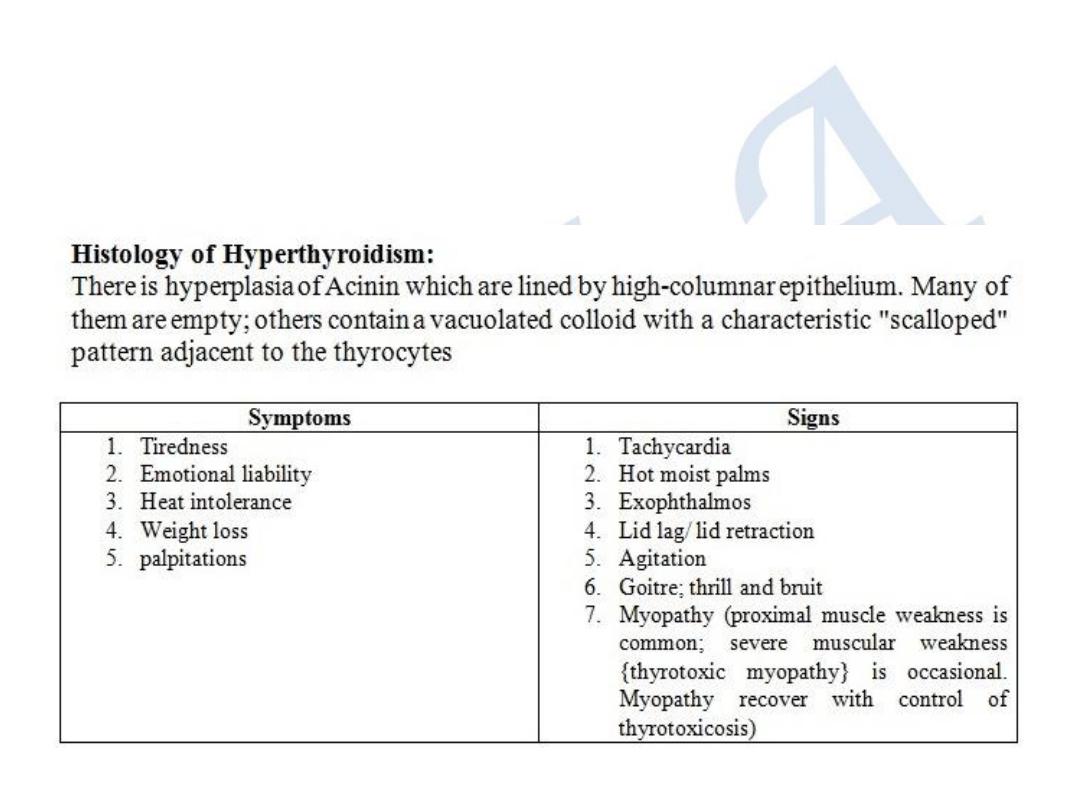
Hyperthyroidism
Thyrotoxicosis:
Clinical types
A.
Diffuse Toxic Goitre (Grave's disease)
(Primary Hyperthyroidism)
B.
Toxic Nodular Goitre
(Secondary Hyperthyroidism)
C.
Toxic Nodule
D. Hyperthyroidism due to rare causes
Thyrotoxicosis Facitia; hyperthyroidism induced by high doses of
thyroxin exceeding 250 µgm/day
Jod-Basedow Thyrotoxicosis; temporary hyperthyroidism induced
by high doses of iodine given for Hyperplastic Endemic Goitre
De Quervain's Thyroiditis; mild hyperthyroidism occurring in the
early stage of subacute or acute autoimmune thyroiditis
Secondary large carcinoma mass rarely cause a mild hyperthyroid
state
Neonatal thyrotoxicosis; temporary thyrotoxicosis in babies born to
mothers who are thyrotoxic. It gradually subsides in 3-4 weeks. It is
due to TSH-Rab crossing the placenta
A Toxic Nodule
There is a solitary active nodule either part of a generalised nodularity or a true toxic
adenoma. It is autonomous and there is no TSH-Rab in the blood. There is increase in
circulating thyroid hormons and decrease in TSH level. On scanning; only the nodule is
active and the normal thyroid tissue surrounding the nodule is suppressed and
inactive.
Eye Signs demonstrated in a thyrotoxic state
Exophthalmos;
proptosis of the eye caused by infiltration of the
retrobulbar tissue with fluid and round cells
Malignant Exophthalmos
• severe and progressive oedema of the eye lids, conjunctival
injection and Chemosis along with papilloedema and corneal
ulceration. The eye may be destroyed.
• tends to improve with time and with control of thyrotoxic state.
• Hypothyroidism secondary to treatment of thyrotoxicosis may
worsen exophthalmos and proptosis and should be avoided.
• Lateral tarsorrhaphy will help protect the eye but will not prevent
progression.
• Massive doses of steroid can help proptosis but intraocular steroid
injection is dangerous and contraindicated.
• Total thyroid ablation by
123
I therapy is not helpful and orbital
decompression may be needed for endangered eye.
Eye Signs demonstrated in a thyrotoxic state
Lid spasm/ lid retraction
sympathetic overactivity affecting the
innervation of the levator palpabrae Superiors muscle causing its tonic
spasm and widening of the palpebral fissure so that the sclera can be
seen clearly above the upper margin of the iris and cornea (above the
limbus).
Spasm and retraction usually disappear with the control of
thyrotoxicosis. It can be improved by β-adrenergic blockers like
Guanithidine eye drops.
Diplopia
is the result of weakness of the extraoccular muscles
particularly the inferior oblique muscle.
Grave's ophthalmopathy
is an autoimmune disease in which there is
antibody-mediated effect on ocular muscles
Pretibial myxoedema (thyroid dermopathy) is a rare condition. There
is thickening of the skin usually in areas of trauma commonly over the
tibia by deposition of hyaluronic acid in the dermis and subcutis. It
usually occurs in few years after the onset of thyrotoxicosis and
responds to control of the thyrotoxic state along with topical steroid
therapy but the thickening will not disappear
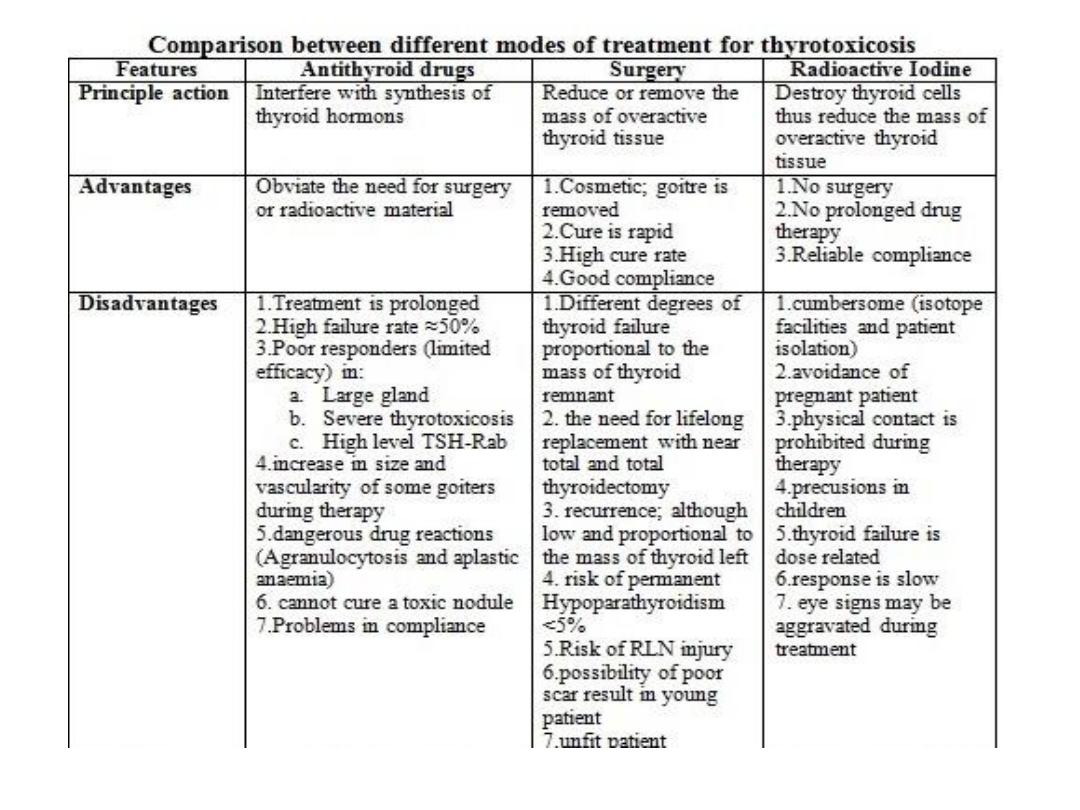
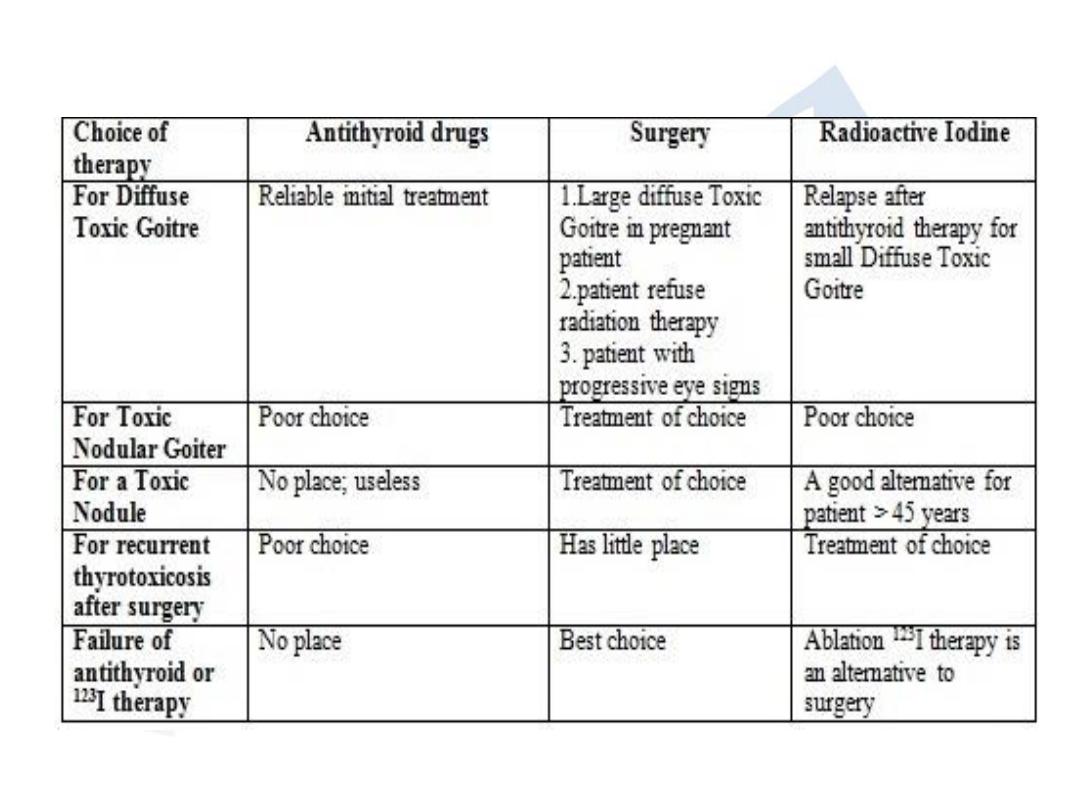
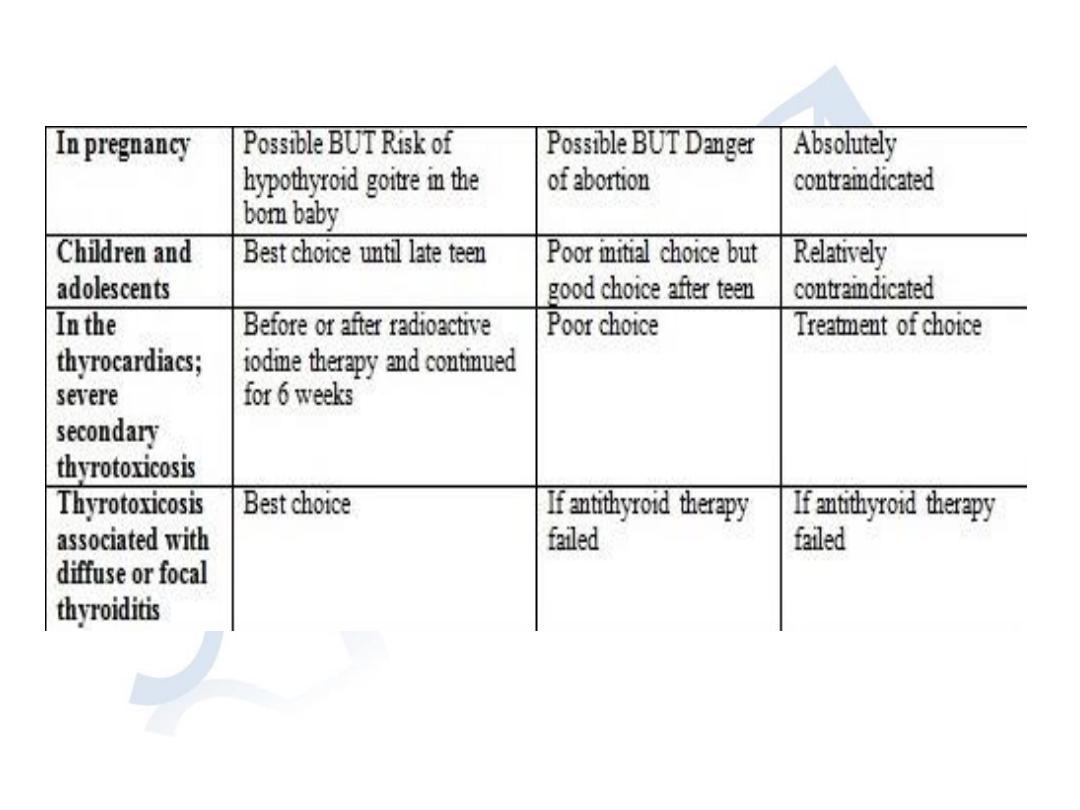
Antithyroid drug surgery Radioactive Iodine

Antithyroid drugs include:
1)
Carbimazol and Propylthiouracil
2)
β-adrenergic (Propranolol and Nadolol)
3)
Iodides
The β-adrenergic block the cardiovascular effect of elevated
thyroxin. The β-Adrenergic blockers act on the target organs and
not the gland to abolish the symptoms. Propranolol also inhibits
peripheral conversion of T
4
to T
3
. Nadolol is longer in action than
Propranolol
Iodides reduce the vascularity of the gland and Lugol's iodine
solution is only indicated as immediate preoperative preparation 10
days before surgery
Dose of Carbimazol is 10 mg t.d.s or q.d.s for 7-14 days then a
maintenance dose of 5 mg for 6-24 months
"Block and Replacement" therapy may be used; a high inhibitory
blocking dose of antithyroid drug along with Eltroxine replacement
100-150µgm/day

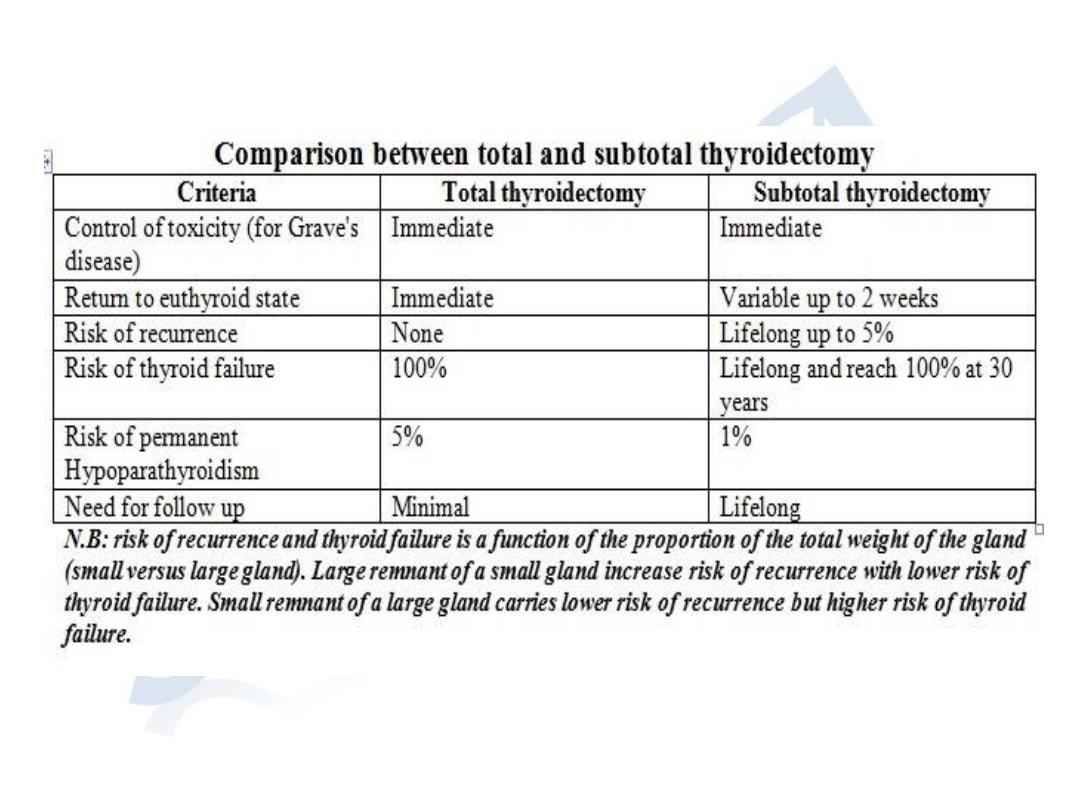
Surgery for thyrotoxicosis
Principles for preoperative preparation:
• The aim is to make the patient biochemically Euthyroid at the time of
operation
• It is an outpatient procedure. Rarely; admission is needed for:
1.
Severe symptoms at presentation
2.
Failure to control on outpatient session
3.
Non-compliance to medication
• Drugs and dosage:
1.
Carbimazol; 30-40 mg/day is the drug of choice. 8-12 weeks period is
needed to control after that dose can be reduced. An alternative is the
use of "Block and Replace" regime. The last dose of Carbimazol is to be
given the night before operation.
2.
Propranolol dose is 40-80 mg t.d.s. Nadolol dose is 160-320 mg/day.
Response is rapid and patients may be euthyroid within few days.
Because β-Adrenergic blocked do not interfere with synthesis of thyroid
hormons; its level stay high for few days after operation thus it is
important to continue therapy for 3 days after operation
3.
Iodine in the form of Lugol's Iodine solution for 10 days before operation
produce a transient remission and reduce the vascularity of the gland

Surgery for thyrotoxicosis
Preoperative investigations:
1.
Thyroid function tests; FT
3
and FT
4
along with TSH assay
2.
Thyroid antibodies tests
3.
Serum calcium
4.
An isotope scan for patients with toxic MNG if total thyroidectomy
is not planned
5.
Preoperative laryngoscopy to check integrity of the vocal cords
Surgery:
The extent of resection depends on:
1.
The size of the gland
2.
The age of the patient
3.
The experience of the surgeon
4.
The need to minimize the risk of recurrence
5.
The wish to avoid lifelong thyroid replacement therapy
Postoperative complications
1. Haemorrhage (Tension and SC Haematoma)
2. Respiratory obstruction
3. RLN injury and change of voice
4. Thyroid insufficiency
5. Parathyroid insufficiency
6. Thyrotoxic crisis (thyroid storm)
7. Recurrent thyrotoxicosis
8. Wound infection
9. Hypertrophic or Keloid scar
10.Stitch granuloma
A malignant thyroid should be suspected in the following
circumstances:
1. A rapidly enlarging solitary swelling in the thyroid
2. Hardiness of part or the whole of the swelling
3. A change in a long standing goitre
4. Loss of upward or lateral mobility of the gland with
swallowing
5. Difficulty in feeling the carotid pulsation on the side of the
swelling (the artery is encased by the growth); the so called
Berry's sign
6. Tracheal obstruction: this incident may occur with
retrosternal goitre, tracheomalacia and Riedel's thyroiditis
7. Hoarseness of voice (RLN involvement by the tumor)
8. Horner's syndrome
9. Associated cervical lymphadenopathy
10. Pain; referring to the ear is more frequent with infiltrating
carcinoma
Clinical Diagnosis, differential diagnosis and investigations of thyroid
neoplasms:
1.
female sex is predominant (♂:♀=1:3). Older patient have more
aggressive disease with a worse prognosis
2.
diagnosis is obvious on clinical examination in cases of undifferentiated
anaplastic carcinoma.
3.
Localised forms of granulomatous and lymphocytic thyroiditis may
simulate carcinoma especially follicular carcinoma
4.
A solitary nodule in a young male is highly suspicious
5.
Biochemical investigations are not very much helpful
6.
Failure to take up
123
I is characteristic of almost all thyroid carcinoma
7.
FNAC play a key role in diagnosis
8.
Incisional or core needle biopsy is justifiable in anaplastic or advanced
obviously irremovable carcinoma
9.
US and/or MRI give valuable information about extent of invasion and
on nodal involvement permitting preoperative planning of resection
10. Frozen section biopsy has a limited role

Surgical treatment:
• For large, locally aggressive or metastatic differentiated thyroid cancer
(high-risk patient); total thyroidectomy with excision of adjacent
involved structures with LNs dissection followed by radioactive iodine
ablation with long-term TSH suppression
• For low-risk differentiated thyroid cancer; a tumor less than 1 cm total
thyroidectomy with central compartment node dissection followed by
123
I-scan postoperatively to detect and ablate metastasis. The clue for
cure is the undetectable thyroglobulin level.
Additional measures:
• Thyroxine for replacement and suppression of endogenous TSH
•
123
I; used for detection and ablation of metastasis. All normal thyroid
tissue must be removed or ablated prior to this therapy. It is mainly
indicated in:
1.
Unresectable disease
2.
Local recurrence
3.
Metastatic disease
4.
High-risk patient
5.
Patient with rising serum thyroglobulin level (a sensitive marker for
differentiated thyroid cancer recurrence)
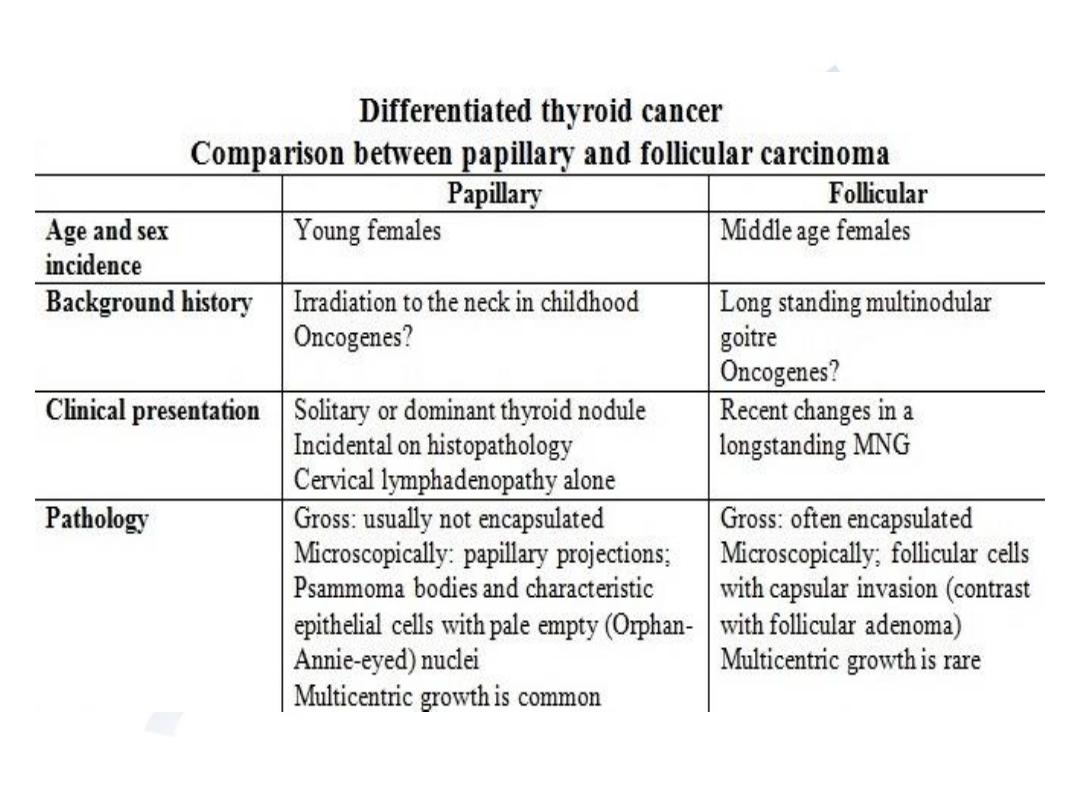
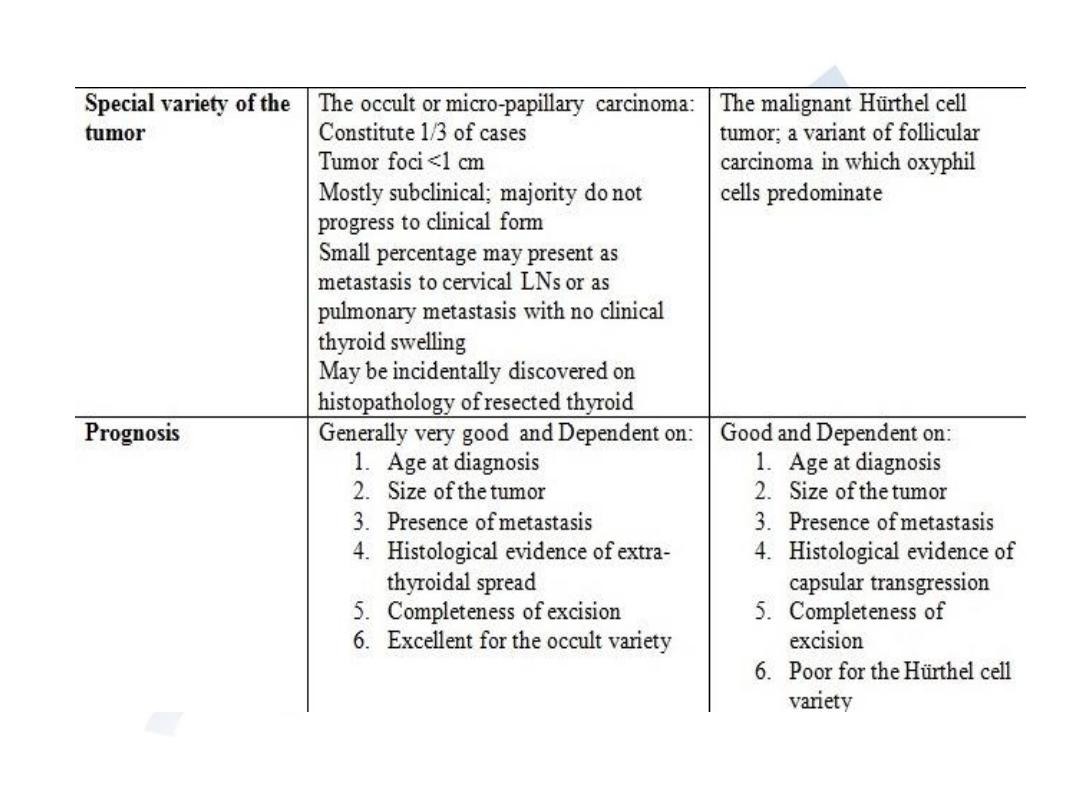
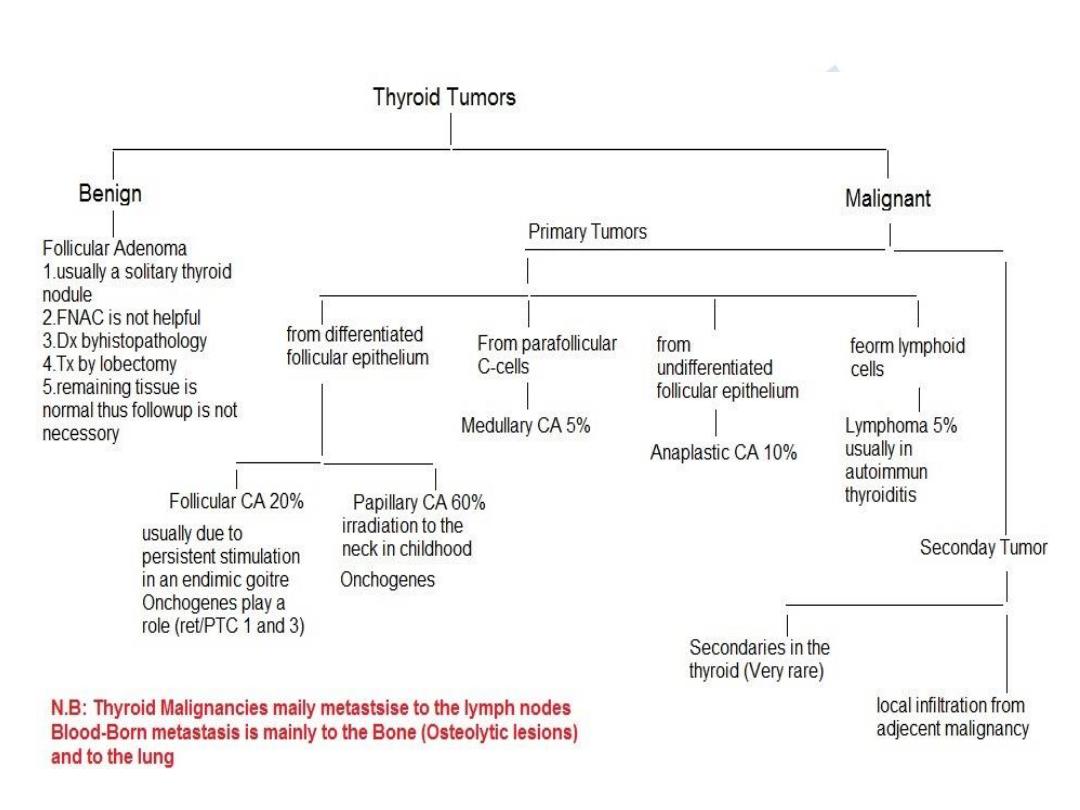
Papillary Follicular

The undifferentiated (Anaplastic) carcinoma
• Occur mainly in elderly females
• Lethal tumor with very low survival rate
• Local infiltration is an early feature
• Spreads by lymphatic and blood
• Complete resection is only possible in the minority of patients
• For cases with tracheal obstruction; tracheostomy is best avoided.
Tracheal decompression by isthmusectomy is indicated and
material is submitted for histopathological assessment
• Radiotherapy generally is indicated in all cases
• Chemotherapy is not useful
Malignant lymphoma
• Most of the cases occur on a background of lymphocytic
thyroiditis
• Diagnosis is usually by core needle or open biopsy
• Highly responsive to radiotherapy thus surgery is unnecessary
• Prognosis is good if there is no involvement of cervical LNs

Medullary carcinoma
•
from Parafollicular C-cells derived from neural crest. Cells mimic that of carcinoid
tumor with characteristic amyloid stroma. not TSH dependent and do not take up
radioactive iodine
•
Diarrhoea in 1/3 of cases (5-hydroxytryptamine or prostaglandins produced by
tumor cell)
•
High levels of serum calcitonin and CEA are considered as serum markers
•
10-20% incidence of familial tumors. + adrenal pheochromocytoma and
parathyroid hyperplasia (Multiple Endocrine Neoplasia type 2A or MEN-2A). it
usually affect children and young adults while sporadic cases may occur at any
age with no sex predominance. Medullary thyroid carcinoma associated with
prominent mucosal neuroma of the lips, tongue and inner aspect of the eye lids
along with marfanoid features constitute the syndrome of MEN-2B
•
Lymph nodes involved in 50-60% of cases especially in familial cases and blood-
born metastasis is also common
•
a slowly progressive malignancy with long term survival even with no cure
•
Treatment for sporadic cases is by total thyroidectomy with central and bilateral
cervical LNs dissection
•
Familial cases are now detected by genetic screening for “RET” mutation
supplemented by serum calcitonin assay in the basal state and after stimulation.
Prophylactic surgery is indicated in infants with genetic traits.
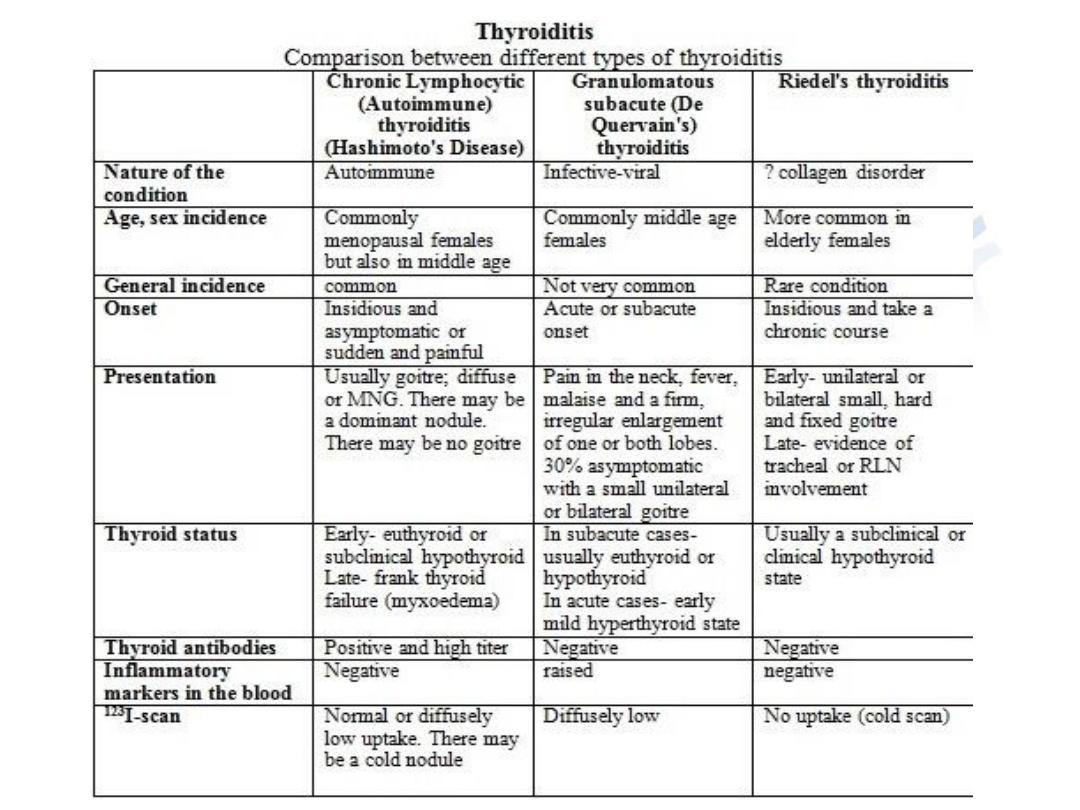
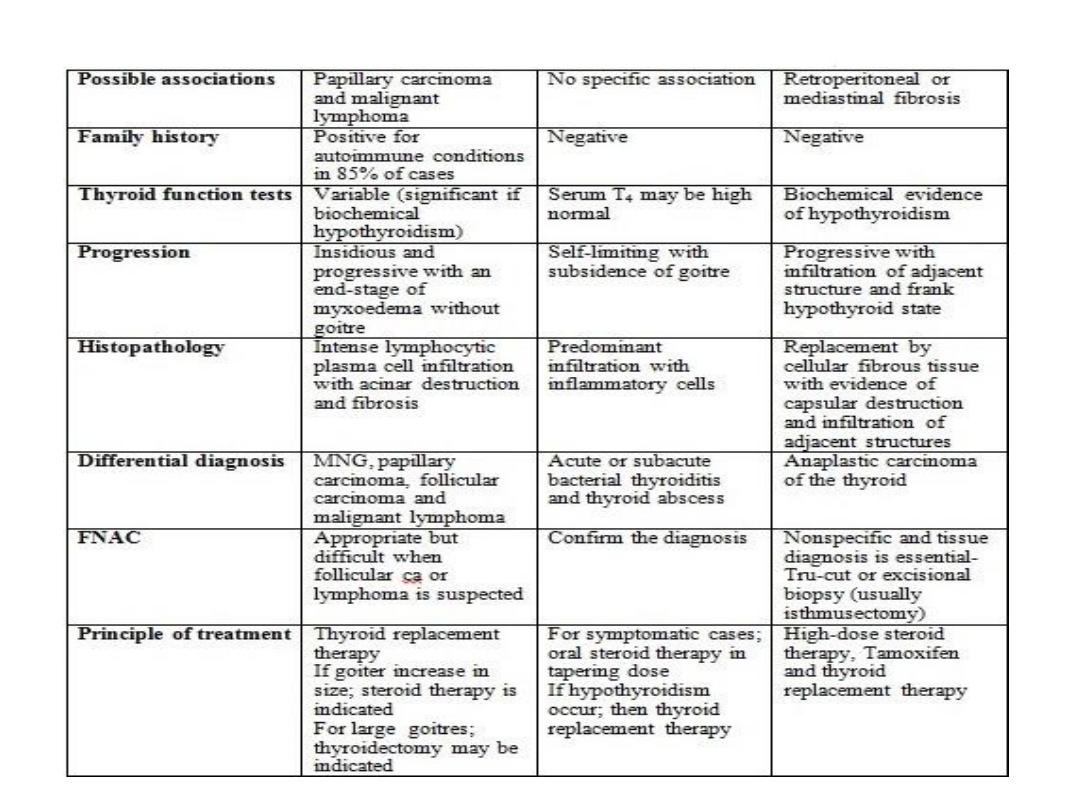
Chronic lymphocytic Granulomatous Riedel's
