Blood groups
Introduction:The surfaces of the RBCs contain numerous glycoprotein markers known as antigens (Ag).
There are many different types of antigens, but the most common are:
A, B, and D antigens (D is also known as the Rh factor).
The presence or absence of these antigens determines the blood type of the individual.
About six months after birth, lymphocytes begin to produce certain antibodies (Ab), which are proteins that circulate in the blood plasma.
These antibodies are isolated from the plasma and used as anti-sera in the laboratory to determine blood types.
Mixing these anti-sera with whole blood stimulates a process called agglutination (clumping).
For example, mixing anti-A serum with type A blood will cause the anti-A antibodies in the serum to "stick to" the A antigens on the erythrocytes.
This Ag-Ab reaction will give the slide a beaded appearance.
Blood Types…
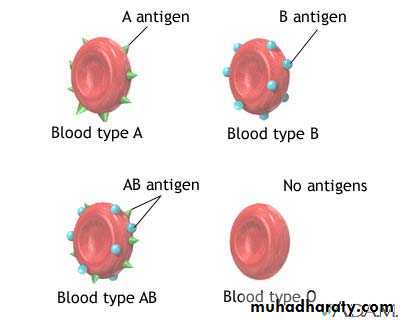
There are four different types of blood
A, B, AB, O
They are determined by the antigen found on the RBC
Type A, has antigen A on the RBC
Type B, has antigen B on the RBC
Type AB, has both antigen A and B on the RBC
Type O, has neither antigen on the RBC
Blood groups
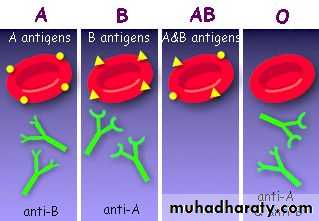
Type A would have B agglutinins (antibody) in the plasma.Type B would have A agglutinins (antibody) in the plasma.
Type AB would not have agglutinins (antibody) in the plasma.
Type O would have A and B agglutinins (antibody) in the plasma.
Notes
The person who is of a blood group AB is called universal recipientThe person of blood group O is called universal donor
Major ABO Blood Group
The underlying table shows the relation between blood group and the presence of agglutinogens and agglutinins and their frequency.Blood type
Agglutinogens
Agglutinins
Frequency
O
----
Anti A, anti B
46%
A
A
Anti B
42%
B
B
Anti A
9%
AB
A,B
-----
3%
Rh system:
There are 6 common types of Rh antigens these are C, D, E, c, d, e.
The most common is the D antigen.
Any body that has D agglutinogens is Rh positive.
The antibodies to the Rh antigen do not occur naturally but can occur after blood transfusion and during pregnancy.
The percentages of people who are Rh + ve are 75%-85%
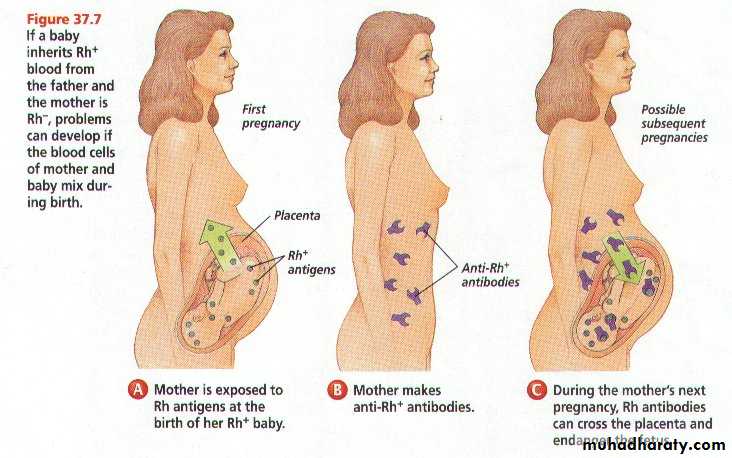
Pregnancy and blood type
Father is Rh+ blood
Mother is Rh–
Child could be Rh +.
1st pregnancy--if the baby is Rh +, then there are no complications.
However, the mother will start to develop antibodies against the Rh factor
Second pregnancy, if the child is Rh+, the mother’s antibodies can cross the placenta and start to attack the fetus’ blood cells, causing hemolysis.
Hemolysis : breakdown of RBC and the release of hemoglobin into the plasma which can damage organs.
This is called erythroblastosis fetalis , can cause severe anemia, jaundice and possibly death.
Procedure:
Use WBC pipetteSuck blood to 0.5 and dilute it with normal saline (0.9% NaCl) to 11
Shake for 10 seconds
Get rid of the first 4 drops
Put on the slide one drop of anti A, anti B , anti D ( keep a good space between each other )
Add drop of the diluted blood on each anti serum
Mix with an applicator stick and wait for about 2 minutes
Examine by eye and by microscope
Mixing the anti-serum with the blood sample to determine blood type.
Blood type
Anti A
Anti B
Anti D
AntiD
A
+
-
+
A+
-
A-
B
-
+
+
B+
-
B-
AB
+
+
+
AB+
-
AB-
o
-
-
+
O+
-
O-
Cross match
This is a direct test of compatibility of donor's cells versus recipient serum.
In this test the donors RBC are mixed with the recipient serum on a slide.
If agglutination occurs this means that the donor's blood is incompatible with the recipient blood and it should not be given to him.
We do blood typing & cross matching before blood transfusion.