Gastrointestinal System
Dr.Nadwa S.Al-azowAssis.prof.pathology Department
The gastrointestinal (GI) tract is a hollow tube extending from the oral cavity to the anus that consists of anatomically distinct segments, including the esophagus, stomach, small intestine, colon, rectum, and anus
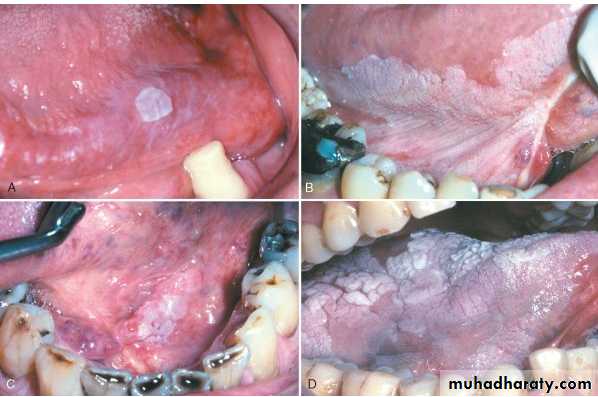
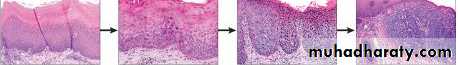
LEUKOPLAKIA
a white patch or plaque that cannot be scraped off and cannot be characterized clinically or pathologically as any other diseaseApproximately 3% of the world's population have leukoplakic lesions, and somewhere between 5% and 25% of these lesions are premalignant
SALIVARY GLANDS
There are three major salivary glandsparotid, submandibular, and sublingual
as well as innumerable minor salivary glands distributed throughout the mucosa of the oral cavity.
All these glands are subject to inflammation or to the development of neoplasms.
Inflammation (Sialadenitis)Causes :
TrumaticViral (Mumps)
Bacterial
Autoimmune (Sjögren syndrome)
PLEOMORPHIC ADENOMA
60% of tumors in the parotid, are less common in the submandibular glands, and rarely in minorbenign tumors that consist of a mixture of ductal (epithelial) and myoepithelial cells, and therefore they show both epithelial and mesenchymal differentiation.
epithelial elements dispersed throughout the matrix along with varying degrees of myxoid, hyaline, chondroid (cartilaginous), and even osseous tissue
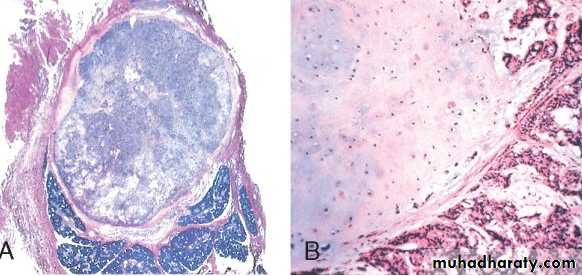
WARTHIN TUMOR (papillary cystadenoma lymphomatosum)
almost exclusively in the parotidmore commonly in males than in females, usually in the fifth to seventh decades of life.
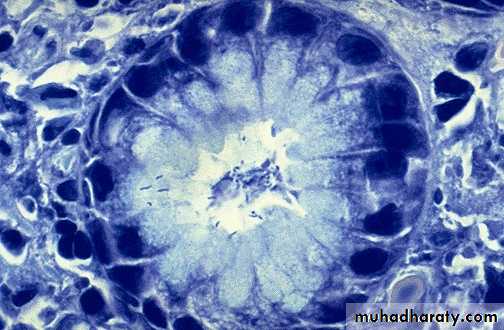
On microscopic examination cystic spaces are lined by a double layer of neoplastic epithelial cells resting on a dense lymphoid stromaAdenoid cystic carcinoma
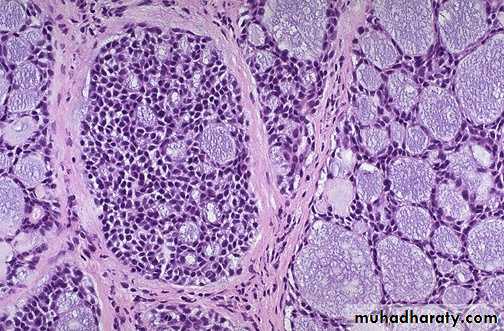
uncommon tumor, which in approximately 50% of cases is found in the minor salivary glands , the major salivary glands affected are parotid & submandibularMicroscopically: solid growth of small hyperchromatic neoplastic cells surrounding small (microcystic) spaces filled with mucinous secretions giving rise to cribriform appearance
CONGENITAL ANOMALIES
ECTOPIC TISSUE (gastric, sebaceous, pancreatic)Atresia/Fistula/Stenosis/”Webs”
MOST COMMON
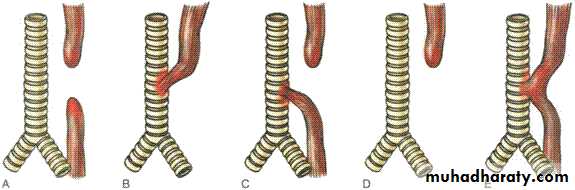
MOTOR DISORDERS• Achalasia
• Hiatal Hernia (sliding [95%], paraesophageal)
• “ZENKER” diverticulum
• Esophagophrenic diverticulum
• Mallory-Weiss tear
Achalasia
Achalasia is a Greek term meaning ‘failure to relax’ is characterized by poor relaxation of the functional lower oesophageal sphincter.
Causes: most of the cases is unknown ,but could be due to systemic sclerosis and South American trypanosomiasis (Chagas’ disease)
may present at any stage in life, usually with dysphagia and regurgitation of undigested food material. Aspiration pneumonia is a significant problem
Microscopically, the disease is characterized by a reduction in the numbers of neurones in the muscular (myenteric) plexus of the lower oesophagus, dilatation of proximal esophagus ,Inflammation &ulceration of mucosa .
Esophagitis:
Inflammation of esophagial mucosaCauses:
Reflux oesophagitis : refluxed gastroduodenal contents
Infectious agents (Candida, herpes simplex
virus) rarely in immunocompromised patient.
The oesophagus may be involved in Crohn’s disease and in systemic sclerosis.
Oesophageal obstruction (tumour, achalasia)
leads to a secondary proximal oesophagitis.
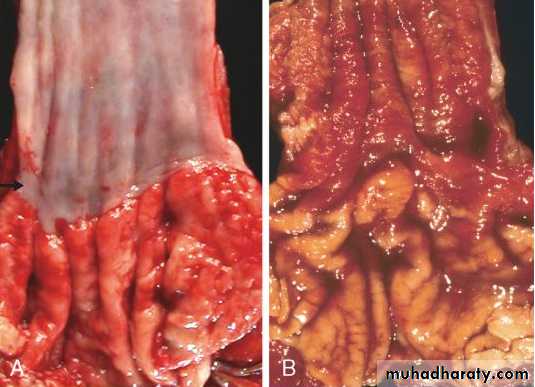
Barrett Esophagus:
characterized by intestinal metaplasia within the esophageal squamous mucosa10% of individuals with symptomatic Gastroesophageal reflux diseases
most common in white males and it typically presents between 40 and 60 years of age.
The signifigance of it: an increased risk of esophageal adenocarcinoma.
ESOPHAGEAL VARICES
development of a congested subepithelial and submucosal venous plexus within the distal esophagus. These vessels, termed varices,develop in 90% of cirrhotic patients, most commonly in association with alcoholic liver disease. Hepatic schistosomiasis is the second most common cause of varices.
they may rupture, causing massive hematemesis half of the patients die from the first bleeding episode either as a direct consequence of hemorrhage or following hepatic coma triggered by hypovolemic shock.
Esophageal Tumors
Benign TumorsMalignant tumors
Surface epith.T.
(Papilloma)
Mesenchymal
Leiomyoma,lipoma,
Hemangioma…..
Surface epith
Squa.cell Ca.
Adenocarcinoma
Others: melanoma,
Carcinoid
sarcoma
Squamous Cell Carcinoma
Arise from Sq.epithelium as exophytic, ulcerative
masses that partly or almost totally occlude the lumen.Adenocarcinomas
generally arise in Barrett’s oesophagus, this is a disease of Western societyStomach
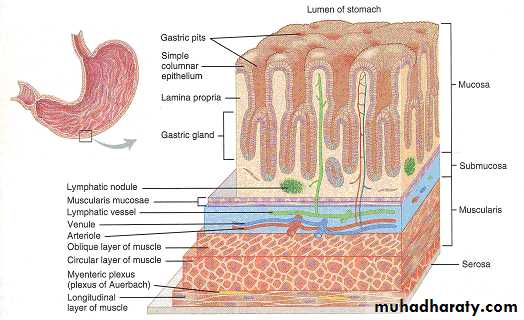
Inflammation of the stomach (Gastritis)Acute chronic
Gastric TumorsAcute Gastritis
is a transient mucosal inflammatory processPathogenesis:
Acute or chronic gastritis can occur following disruption of any of these protective mechanisms
Mucin secreted by surface foveolar cells forms a thin layer of mucus (defect occur as in elderly,
bicarbonate ion secretion ( NSAI drugs reduce producti on), chemotherapy
rich vascular supply
Clinically:
Mild cases the pt. presented with nausea, vomiting in severe cases causes bleeding
Microscopically :
Mild condition show neutrophils infiltrated the surface epithelium & glands in lamina propria with lymphocytes and plasma chronic inflammatory cellsIn severe cases there are erosion of surface epithelium , ulceration , bleeding and hemorrhage.
ACUTE GASTRIC ULCERATION
Stress ulcers are most common in individuals with shock, sepsis, or severe traumaUlcers occurring in the proximal duodenum and associated with severe burns or trauma are called Curling ulcers.
Gastric, duodenal, and esophageal ulcers arising in persons with intracranial disease are termed Cushing ulcers and carry a high incidence of perforation.
• Pathogenesis.
Acute gastritis: hyperemic erythmatous edematous gastric mucosa with foci of superficial erosions. There are many causes for acute gastritis: alcoholism, drugs, infections, etc
Chronic Gastritis
Causes :The most common cause of chronic gastritis is infection with the bacillus Helicobacter pylori.
Others : psychological stress, caffeine, alcohol, and tobacco .
Autoimmune gastritis ( cause atrophic gastritis, 10%of chronic gastritis in the absence of H.pylori)
Less common causes : radiation injury, chronic bile reflux, mechanical injury, and involvement by systemic disease such as Crohn disease, amyloidosis, or graft-versus-host disease.
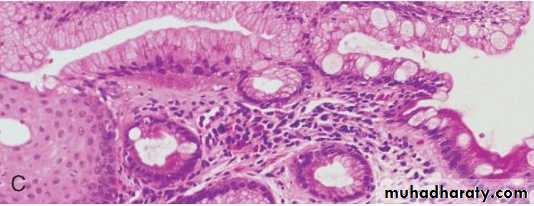
HELICOBACTER PYLORI GASTRITIS
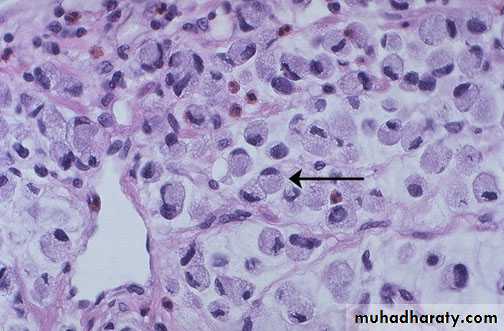
spiral-shaped or curved bacilliPresented in almost all patients with duodenal ulcers and the majority of individuals with gastric ulcers or chronic gastritis.
H. pylori has important roles in gastric and duodenal diseases.( peptic ulcer disease, increased risk of gastric cancer)
H-pylori This small curved to spiral rod-shaped bacterium is found in the surface epithelium of most patients with active gastritis. The rods are seen here with a methylene blue stain.
Pathogenesis.
H.Pylori causes Antral gastritis with high acid secretion , progress to involve the fundic and body mucosa , in advanced untreated conditions lead to pangatritis associated with multifocal mucosal atrophy, reduced acid secretion, intestinal metaplasia, and increased risk of gastric adenocarcinoma.Morphological Features of H.pylori asssociated chronic gastritis:
H.Pylori is concentrated within the superficial mucus overlying epithelial cells in the surface and neck regions.H. pylori are typically found in the antrum ,
neutrophilic cells infiltration within the lamina propria
In addition, the superficial lamina propria includes large numbers of plasma cells, often in clusters or sheets, and increased numbers of lymphocytes and macrophages.
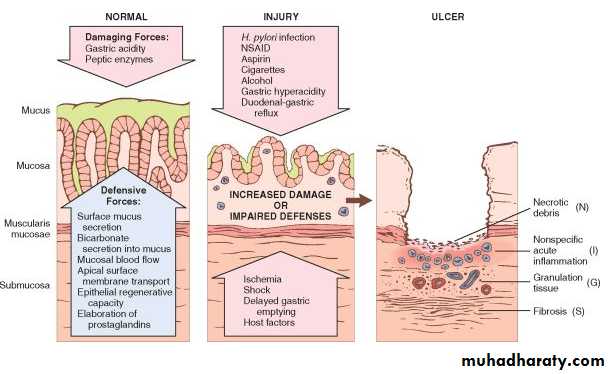
PEPTIC ULCER DISEASE
85% -100% are duodenal ulcers65% gastric ulcer
Epidemiology.
The imbalances of mucosal defenses and damaging forces that cause chronic gastritis are also responsible for PUD
the main causes for hyperacidity: H.pylori, parietal cell hyperplasia, hypergastrinemia, ….
Co-factors NSAIDrugs direct injury to the mucosa
Smoking , alcohol consumption affect the blood supply of mucosa
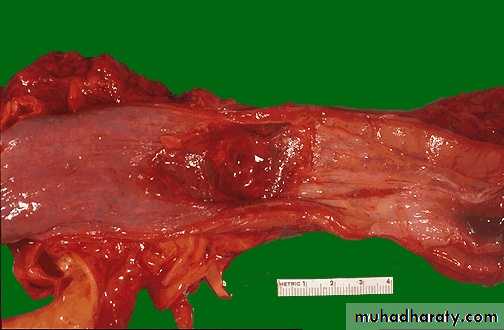
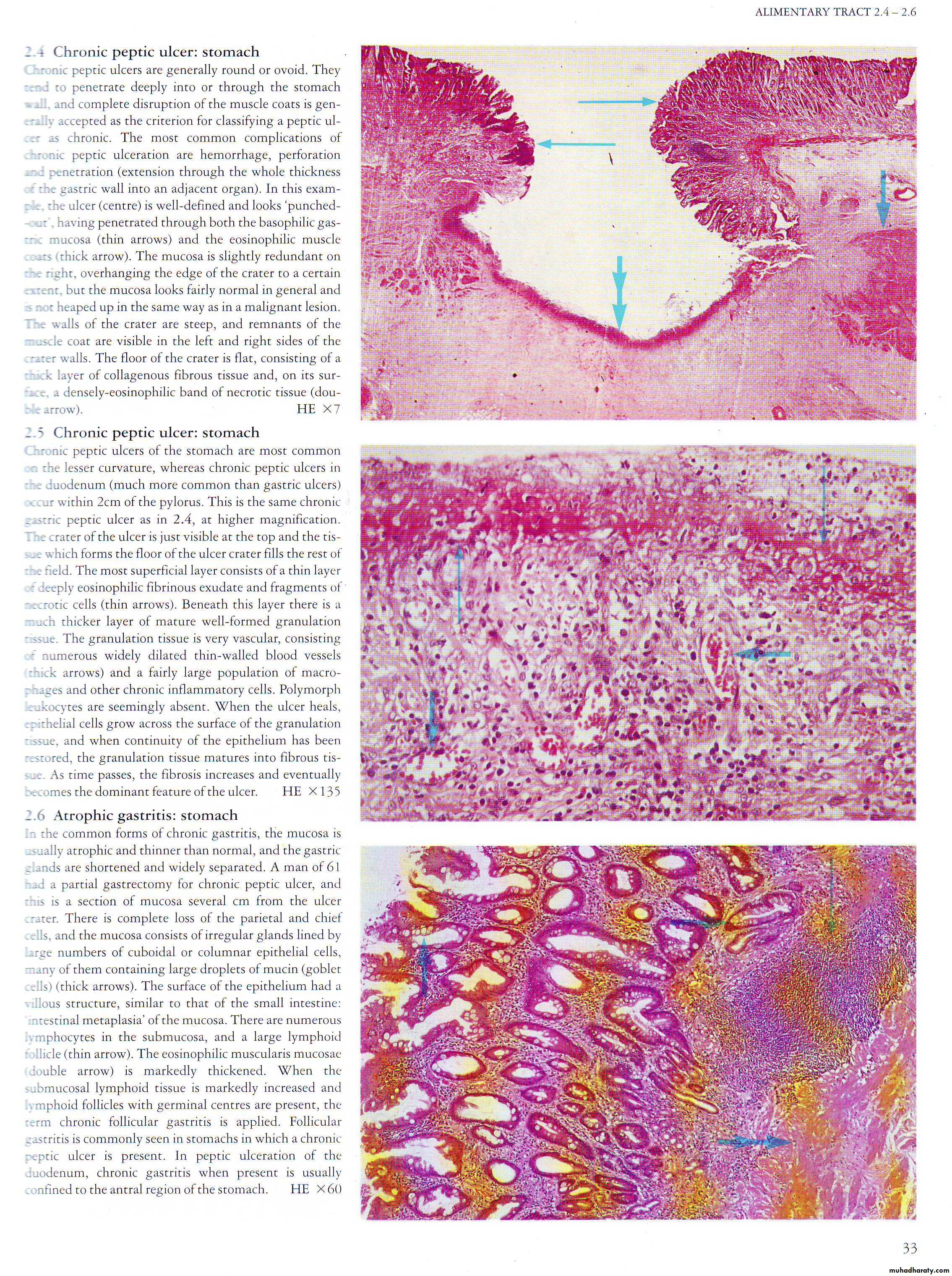
Morphology:
Duodenal ulcers involve the anterior duodenal wall.Gastric peptic ulcers are predominantly located along the lesser curvature near the interface of the body and antrum.
80% solitary ,round to oval, sharply punched-out defect, hang out the surrounding mucosa
The base show fibrinoid material, Beneath this, active granulation tissue infiltrated with mononuclear leukocytes and a fibrous or collagenous scar
Complications of Peptic Ulcers:
BleedingOccurs in 15% to 20% of patients
Most frequent complication
May be life-threatening
Accounts for 25% of ulcer deaths
May be the first indication of an ulcer
Perforation
Occurs in about 5% of patients
Accounts for two thirds of ulcer deaths
Rarely, is the first indication of an ulcer
Obstruction from edema or scarring
Occurs in about 2% of patients
Most often due to pyloric channel ulcers
May also occur with duodenal ulcers
Causes incapacitating, crampy abdominal pain
Rarely, may lead to total obstruction with intractable vomiting
Malignant transformation of peptic ulcers is very rare
GASTRIC TUMORS
BENIGN:“POLYPS*” (HYPERPLASTIC vs. ADENOMATOUS)
LEIOMYOMAS
LIPOMAS
MALIGNANT
(ADENO)-Carcinoma
LYMPHOMA
Others
Gastro-Intestinal “Stromal” Tumor (GIST)
CARCINOID (NEUROENDOCRINE)
RISK FACTORS
H. PyloriType of food : Nitrites, smoked meats, pickled, salted, chili peppers,
Low Socioeconomictobacco
Chronic gastritis, Barrett’s, adenomas
Family history
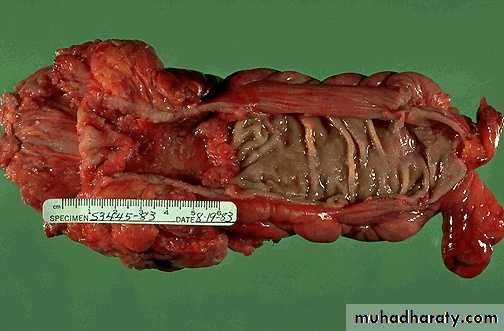
Morhophology: Adenocrcinoma
Intestinal Type :
Grossly : Exophytic , Nodular, ulcerative Excavaeted.
Microscopically: glandular component of malignant cells.
Diffuse type:
Infitrative to gastric wall , malignant cells had intracellular mucin push the nucleus to the periphery (Linitis Plastica)SMALL INTESTINE AND COLON
The small intestine and colon account for the majority of GI tract length and are the sites of a broad array of diseases
SI = 6 meters (100% intraP, except for duodenum), LI = 1.5 meters (50% retroP)
Mucosa, submucosa, muscularis, serosa
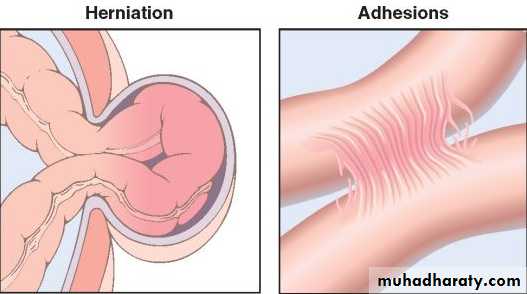
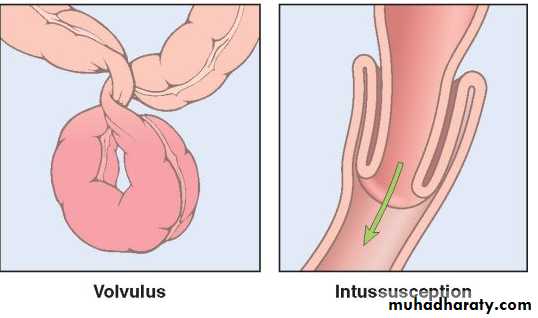
Intestinal Obstruction
small intestine is most often involved because of its relatively narrow lumen.Hernias,
Intestinal adhesions,Intussusception
Volvulus account for 80% of mechanical obstructions
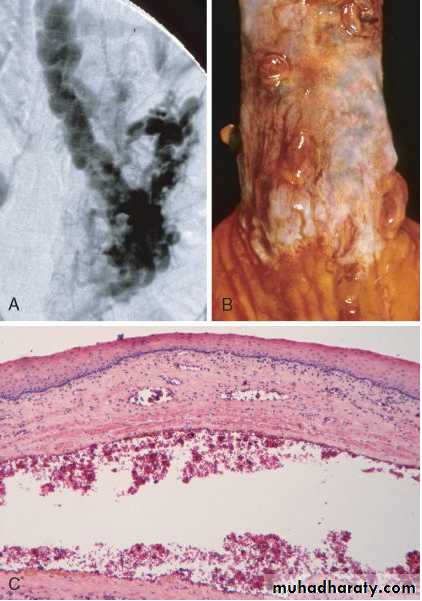
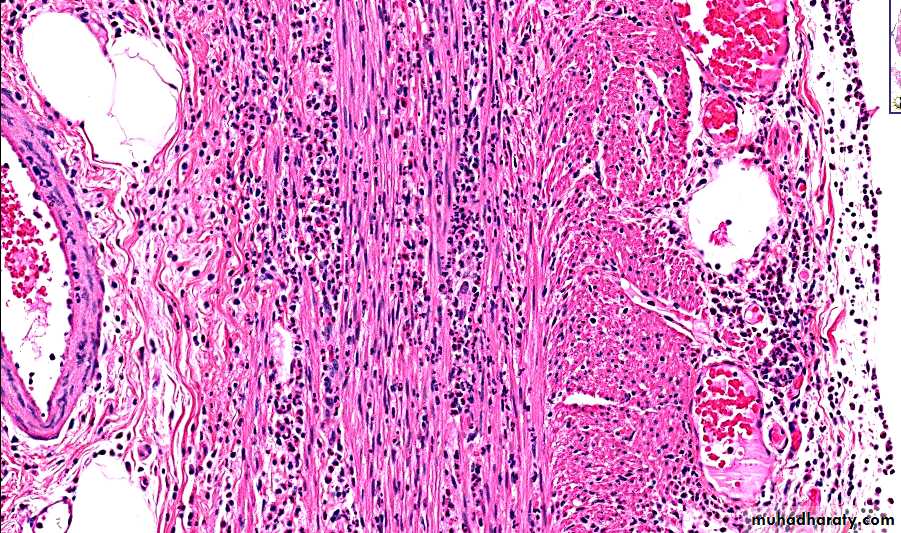
PSEUDOMEMBRANOUS COLITIS
caused by Clostridium difficile, is also known as antibiotic-associated colitis or antibiotic-associated diarrheadisruption of the normal colonic flora by antibiotics allows C. difficile overgrowth
Morphologically: formation ofpseudomembranes made up of an adherent layer of inflammatory cells and debris at sites of colonic mucosal injury.
The surface epithelium is denuded, and the superficial lamina propria contains a dense infiltrate of neutrophils and occasional fibrin thrombi within capillaries.
These exudates coalesce to form the pseudomembranes
Malabsorption:
is defective in nutrient absorption , presents most commonly as chronic diarrhea, causes :INTRALUMINAL (PANCREATIC DEFECTIVE/REDUCED BILE
BACTERIAL OVERGROWTH)Defect in the wall (defect in mucosal function , mucosal atrophy….)
Out side the intestine( like adhesion , tumor outside)CELIAC DISEASE
Also called NON-tropical SPRUEAlso called GLUTEN-SENSITIVE ENTEROPATHY
• Sensitivity to GLUTEN, a wheat protein, gliadin
• Immobilizes T-cells
• Also in oat, barley, rye
• The histopathology is characterized by increased numbers of intraepithelial CD8+ T lymphocytes (intraepithelial lymphocytosis), crypt hyperplasia, and villous atrophy .
• Relieved by gluten withdrawal
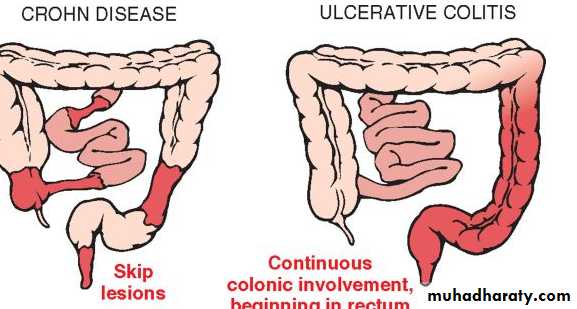
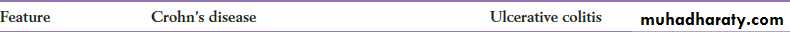
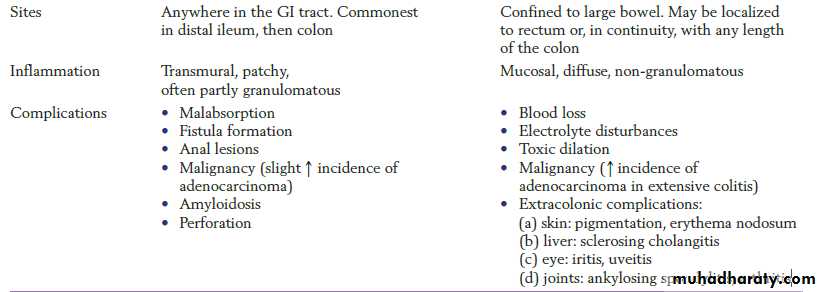
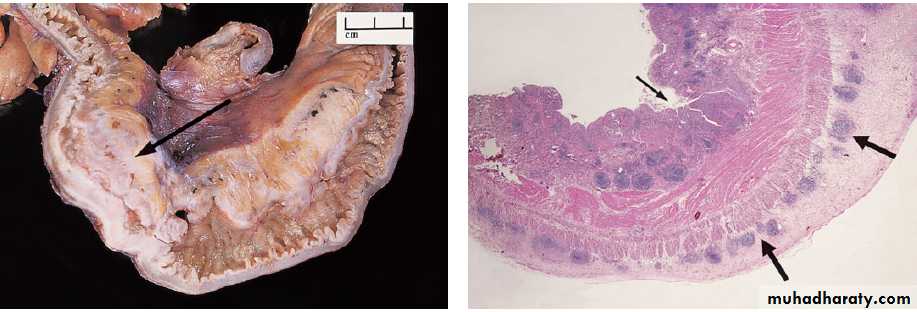
Inflammatory Bowel Diseases
Crohn disease : affecting the small & large intestine ( oral to anus) mainly ileocecal regionUlcerative Colitis : only large intestine, sigmoid region
Charcteristic Features :
IDIOPATHIC
DEVELOPED COUNTRIES
COLONIC INFLAMMATIONSIMILAR Rx
Ulcerative Colitis increased CANCER RISKDiverticulosis :
acquired pseudo-diverticular outpouchings of the colonic mucosa and submucosa.rare in persons under age 30, but the prevalence approaches 50% in Western adult populations over age 60.
Occur due to increased intraluminal pressure in the sigmoid , due to constipation (low fiber diet)
Complication
UlcerationBacterial infection & abscess formation
Perforation & peritonitisFistula formation (with bladder , vagina)
Intestinal Polyps :
Non-neoplastic polypHyperplastic Polyp( seen in large bowel in Inflammatory disases as crohn’s disease or ulcerative colitis)
Hamartomatous polyp : autosomal dominant inherited condition of Peutz– Jeghers syndrome,
Neoplastic polyp: more common in the large
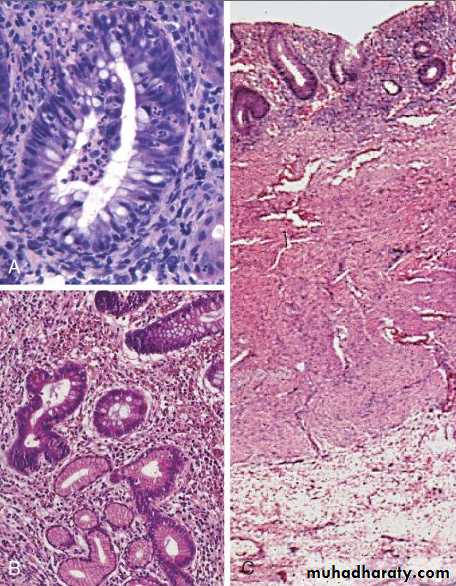
than small bowel , about one-third of individuals at 70 years of ageThe tubular adenoma:
tubular crypts arising from a lobulated surfaceThe villous adenoma : less common type has a small intestine like velvety surface made up of numerous epithelial-lined projections .
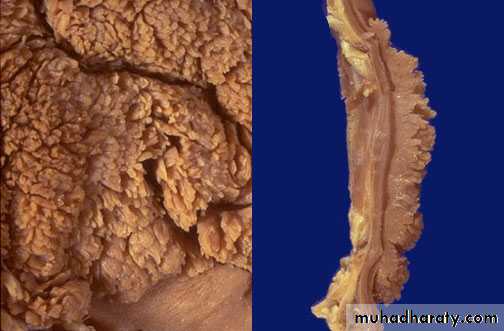
FAMILIAL ADENOMATOUS POLYPOSIS
(FAP) is an autosomal dominant disorderpatients develop numerous colorectal adenomas as teenagers.
It is caused by mutations of the adenomatous polyposis coli (APC) gene.
100-1000 in no.in the whole large bowel
Colorectal adenocarcinoma develops in 100% of untreated FAP patients, often before age 30Y.
total colectomy is Rx of choice to decrease the incidence of colon Ca.
Colorectal Carcinoma :
Cancers of the large bowel are among the most common neoplasms in Western societyLow fiber diet , high intake of refind carbohydrate &Fat.
Low antioxidant Vit A,C,E
(all had a role in developing adenocarcinoma of large bowel.
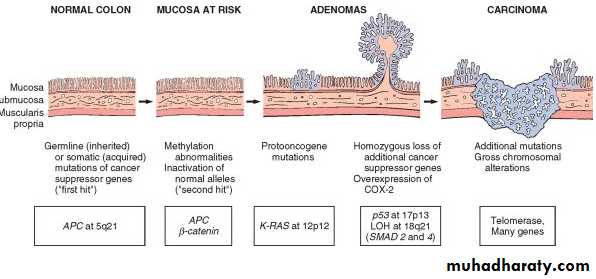
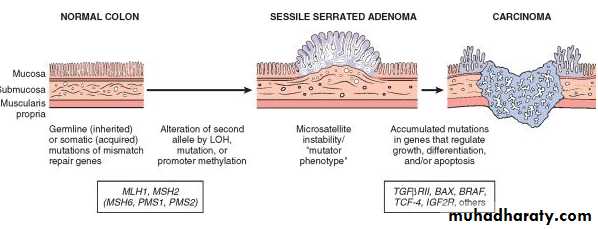
Pathogenesis :
Two genetic pathways
the APC/β-catenin pathway adenoma-carcinoma sequencemicrosatellite instability pathway, which is associated with defects in DNA mismatch repair
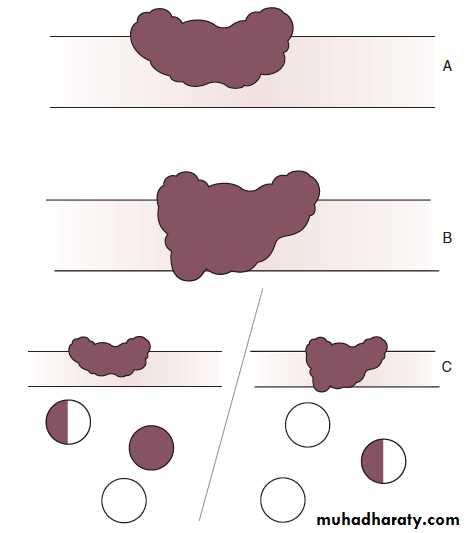
Morphology :
About one-half are found in the rectum, a furtherone-third in the sigmoid, and the rest are spread equally
across the remainder of the colon
Tumors of proximal colon appear as exophytic or ulcerative mass rarely cause obstruction
In distal part presented as annular lesion cause narrowing of lumen and obstruction .
Tumors composed of glandular structures lined by malignant cells at different differentiation
Some times signet ring ca. as in gastric Ca.
Many systems for staging of colorectal ca. one of them Dukes Staging System
ANAL CANAL CARCINOMAS
MORE LIKELY TO BE SQUAMOUS, or “basaloid”WORSE IN PROGNOSIS
HPV RELATED
THE APPENDIX
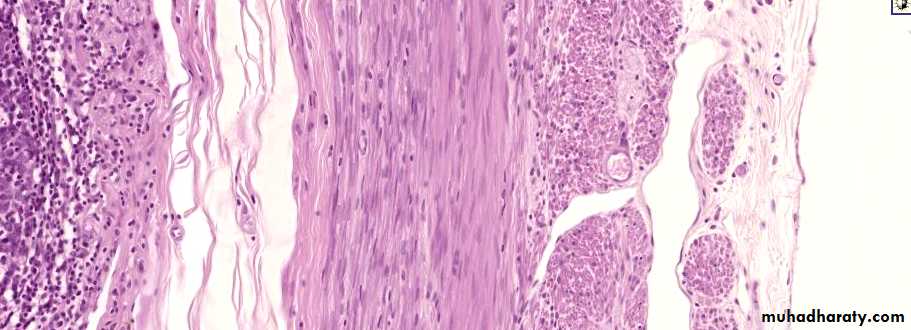
is a normal true diverticulum of the cecum that is prone to acute and chronic inflammationAcute Appendicitis
initiated by progressive increases in intraluminal pressure that compromise venous outflow. In 50% to 80% of cases, acute appendicitis is associated with overt luminal obstruction caused by stool (fecolith, oxyuriasis vermicularis (worm), tumor…)
Microscopically: transmural infiltration of neutrophils with ulceration of linning mucosa
ACUTE APPENDICITIS