LEC:2
E.N.Tد. عماد ناظم الكواز
EAR
16/3/2017
Diseases of the External EarCongenital
Anotia: Complete absence of pinna.
Microtia: small pinna.
Accessory auricle.
Atresia of the EAM.
Protruding ear (bat ear).
Preauricular sinus and cyst.
Haematoma of the auricle (Haematoma auris)
An extravasations of blood under the perichondrium leading to bluish swelling of the auricle. The ear may be slightly tender with a feeling of heat and discomfort. If untreated, the pinna may become distorted and thickened due to replacement of necrosed cartilage with fibrous tissue. A "cauliflower ear" – often seen in wrestlers- may result.Treatment
Aspiration or incision and drainage under aseptic precautions followed by firm dressing or suturing of silastic sheets on pinna.
Foreign Body in the Ear
F.B. in the ear are usually found in children. They are either animate FB (flies and larvae) or inanimate FB; inanimate are either vegetable or non-vegetable ( as buttons and disc battery).
Clinical Picture
1. Suggestive history + Conductive deafness and tinnitus.
2. Pain and reflex cough due to stimulation of auricular branch of vagus N.
3. FB is visible by otoscope.
Treatment
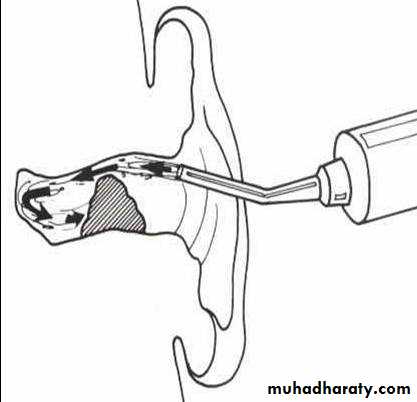
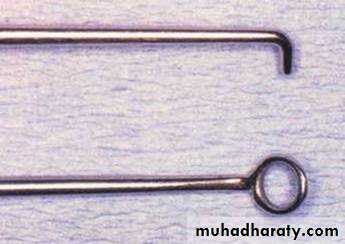
Animate FB are killed by alcohol and removed by ear wash or crocodile forceps.Non-vegetable FB are removed by aural syringing except disc battery which should be removed as emergency procedure by crocodile forceps or Jobson- Horn probe.
Vegetable FB: Here syringing is contraindicated as it may swell and become wedged in the bony meatus. These are best removed with forceps or probe.
General anesthesia may be needed in impacted FB and uncooperative children. FB in the ear must be removed by experienced surgeon to avoid damage to tympanic membrane and ossicles.
Perichondritis
Is infection and inflammation of the perichondrium of auricular cartilage.Causes;
Infected haematoma auris.
Complication of severe otitis externa.
Injury to auricle as laceration or surgical operation involving the auricular cartilage as mastoidectomy.
High ear piercing
Clinical Picture:
Pinna is uniformly enlarged and thickened and its surface is red and shiny, with severe pain and tenderness.
Bacteriology: Pseudomonus aeruginosa is the commonest causal organism.
Treatment:
Vigorous parenteral antibiotic treatment.
Application of soothing dressing such as ichthamol in glycerin.
If subperichondrial abscess is formed it must be incised and drained with removal of all necrotic cartilage, followed by daily dressing. Cauliflower deformity may result if the condition is not treated early.
Impacted Wax (Cerumen)
Wax is a mixture of secretions of ceruminous and sebaceous glands with desquamated skin cells. The glands are situated in the cartilaginous portion of the EAM. Normally, it is expelled outside the canal by movement of chewing and by underlying epithelial migration. Cerumen protects the ear from various bacterial and fungal infections, helps in cleaning and lubrication, and also protects the sensitive skin of the ear canal.
Clinical Picture:
1. Deafness and discomfort in the ear.
2. Tinnitus and disturbance of balance due to pressure of the wax on TM.
3. Reflex cough due to stimulation of the auricular branch of the vagus (Arnold nerve).
Examination
Otoscopic examination: brown, yellowish or black plug obscuring the TM.
Treatment:
Syringing with water at 37°C. If too hot or too cold, a caloric response may be induced in the labyrinth causing vertigo. Jet of water is directed to postero-superior wall of EAC.
Removal with the ring end of Jobson-Horn probe is often better with old, dry and hard plugs.
Suction through the operating microscope when a perforation in the tympanic membrane is present or in previous ear surgery. If the wax is hard then preliminary softening by the use of repeated instillation of 5% sodium bicarbonate in glycerin, olive oil or diluted hydrogen peroxide.
Inflammatory conditions of the external auditory canal (Otitis Externa)
Bacterial:Diffuse OE
Localized OE: frunculosis
Malignant OE (Necrotizing OE)
Viral:
Bullous myringitis
Herpes Zoster oticus
Fungal: (Otomycosis)
Non infective (Allergic OE, Seborrhoic OE)
Diffuse otitis externa
Diffuse inflammation of the skin lining of the external auditory canal
Predisposing factors:
Skin laceration: self-inflicted or iatrogenic by ear wash or instruments.
Skin maceration: hot humid atmosphere and swimmer ear.
Symptoms:
Severe earache increased on moving the jaw.
When edema is severe: conductive deafness.
Signs:
Tenderness on moving the auricle or pressure on the tragus.
Tender pre and post auricular LN
Otoscopic exam: red edematous canal with scanty discharge.
Treatment:
Meticulous cleaning followed by antibiotic/steroid drops.
If the canal is very swollen, a strip of ribbon gauze (wick) impregnated with 8% aluminium acetate or antibiotic/steroid cream is inserted, and it may need to be changed daily.
Furunculosis
Localized suppurative inflammation of a hair follicle in the skin of the outer cartilaginous part of the canal caused by Staph aureus.Precipitating factors: Scratching of ear canal and DM.
Symptoms:
Earache: Severe and increase on moving the jaw.Deafness when edema is severe leading to obstruction of the canal.
Signs:
Tenderness on moving the auricle or pressure on the tragus.
Tender pre and post auricular LN.
It is difficult to examine the external canal by otoscope because there is localized area of tenderness in the skin of the outer canal.
No or scanty purulent otorrhea.
Investigations:
Blood glucose level especially in recurrent and bilateral cases.
Differential diagnosis: acute mastoiditis
Treatment:
If the canal is very swollen, a strip of ribbon gauze (wick) impregnated with 8% aluminium acetate or antibiotic/steroid cream, and these may need to be changed daily.
Meticulous cleaning followed by antibiotic/steroid drops.
Antibiotics ( flucloxacillin for 5 days )
Analgesics and heat application to the ear by a covered hot water bottle.
Incision of a boil should be delayed until it is clearly pointing to the skin.
Malignant otitis externa (Necrotizing otitis externa)
Invasive potentially fatal infection of the external canal which cause osteomyelitis of skull base leading to high morbidity and mortality. The condition is encountered in uncontrolled diabetic and elderly immune-compromised patients. The offending organism is pseudomonas aeuruginosa.
Clinical picture
Constant deep otalgia which increase at night and does not respond to analgesics.
Granulations at the floor of the external canal at the attachment of bony and cartilaginous part.(This is very important sign).
Scanty, sanguineous and purulent otorrhea.
Investigations:
Blood glucose level.CT scan of the temporal bone & skull base.
Radio-isotope scan ( Technetium 99) to assess severity & prognosis.
Complications:
Osteomyelitis of the temporal bone & skull base.
Facial nerve paralysis at the stylomastoid foramen.
Last 4 cranial nerves paralysis at the jugular foramen.
Treatment:
Prompt control of diabetes / and good analegsia.
Systemic antibiotics: e.g. amikacin + ciprofloxacin, the latter should be continued for 6 weeks.
Local antibiotic ear drops after debridement of granulation tissue .
Surgical excision or mastoidectomy is to be avoided or postponed.
Bullous myringitis (Otitis externa haemorrhagica)
It’s a painful condition characterized by formation of haemorrhagic blebs on the tympanic membrane, caused by viral infection as its often seen in influenza epidemics.
Clinical picture
Severe extreme pain preventing sleep or work with almost normal hearing. On examination haemorrhagic bullae are found on the drum, dark bluish or red in colour. The bullae are prone to spontaneous rupture, with blood stained aural discharge.
Treatment
Analgesia and keeping the ear dry. Incision of the bullae is not indicated.
Herpes Zoster Oticus
Etiology: Herpes zoster virusClinically:
Pain in and around the ear
Vesicles on the auricle and external canal
Ramsay-Hunt syndrome: Vesicles+ facial nerve palsy+SNHL& Vertigo.
Treatment:
Antiviral drugs
Corticosteroid if there is affection of VII & VIII nerve.
Fungal otitis externa or Otomycosis
Fungal infection of the skin of the exernal canal.Organism:
Aspirigillus Niger.
Candida albicans.
Symptoms:
Itching is usually the only symptom.
Pain only if there is secondary bacterial infection.
Deafness if the external canal is obstructed.
Signs:
The external canal contains whitish mass with black spots like wet newspaper.
Treatment:
Aural toilet: removal of the fungal mass by suction.
Antifungal: nystatin, or salicylic acid (2%) as a keratolytic in alcohol as fungicidal. Regular attendance for treatment lasting 3 or 4 weeks is necessary for elimination of the infection.
Osteoma and Exostosis
They are bony outgrowth from the wall of the EAM. Osteoma is a single tumor composed of cancelous bone located at outer part of bony canal. Exostosis is multiple growth composed of ivory bone located at deep meatus. Aetiology is unknown but it is more common in cold water swimmers.
Symptoms: Hearing loss if the external canal is obstructed by large osteoma or wax.
Treatment: Asymptomatic: observation. If obstructing the canal: excision.