
Fifth stage
Dermatology
Lec. 9
.د
منار
16/3/2017
Cutaneous Manifestations of Internal Disease
Cutaneous Manifestations of Diabetes Mellitus
Approximately 30% of patients with diabetes mellitus develop a skin disorder sometime
during the course of disease:
Candida infections (mouth, genital)
Caroteneamia (yellow skin)
Diabetic bullae (in feet)
Diabetic dermopathy (shin spots)
Diabetic thick skin (stiff skin )
Erythema (face, lower legs, feet)
Otitis externa
Finger pebbles
Foot ulcers
Acanthosis nigricans (insulin resistance syndromes)
Gas gangrene (non clostridial)
Granuloma annulare (localized or generalized)
Insulin lipodystrophy
Necrobiosis lipoidica
Yellow nails
Perforating disorders
Eruptive xanthomas
Diabetic Dermopathy
This is the most common cutaneous marker of diabetes and
occurs in 40% of diabetics.
There is an unfavourable association with the three most common
microangiopathic complications of diabetes: neuropathy,
nephropathy and retinopathy.
There is also an association with coronary artery disease.
Clinically:
Asymptomatic, round, atrophic, hyperpigmented areas on shins
(shin spots).
They begin as round-to-oval, flat topped, red, scaly papules that
may become eroded. They eventually clear or heal with atrophy
and hyperpigmentation.
Shin spots may also occur on forearms, anterior lower thighs, and
sides of feet.
Men are affected twice as often as women.
May be initiated by trauma.

Diabetic Bullae (Bullosis Diabeticorum)
Etiology is unknown but may be ischemic.
Crops of bullae appear abruptly in diabetics, usually on feet and
lower legs but may occur on arms.
Usually develop over night without preceding trauma.
There is little pain or discomfort.
They arise on non-erythematous base and are usually multiple,
variable in size, and occasionally huge.
They are tense, and spontaneously rupture in 1 week leaving a
painless ulcer (that is difficult to heal) with firmly adherent crust.
Recurrences may occur.
Rx.
Necrobiosis Lipoidica
Necrobiosis lipoidica (NL) is a disease of unknown origin, but more
than 50% of the patients with NL are insulin dependent.
However, it is seen in less than 1% of the entire diabetic population.
The average age is 30 years.
Mostly lesions are confined to the anterior lower legs.
Clinically
The eruption begins as an oval, violaceous patch that expands slowly.
The advancing border is red, and the central area turns yellow-brown
then atrophies and exhibits a waxy surface; telangiectasias are
present.
Ulceration occurs, particularly following trauma.
Rx
Topical, intralesional and systemic steroids
Pentoxifylline
Aspirin
Dipyridamole
Cyclosporine
Tacrolimus ointment
Etanercept
Skin grafting.
Granuloma Annulare (GA)
The association of GA with diabetes is not documented but in one
study, 12% of patients with GA had diabetes.
The disease begins with an asymptomatic, flesh-colored or red
papule or plaque that undergoes central involution.
Over months, a ring of papules slowly increases in diameter to 0.5 - 5
cm.

The localized form is the most common; it is seen in young adult
females and usually found on the lateral or dorsal surfaces of the
hands and feet.
No scarring after resolution.
Patients who develop GA usually heal, remain healthy, and do not
usually develop other diseases.
The familial occurrence of GA is uncommon but has been noted.
Rx
Localized lesions are asymptomatic and are best left untreated.
Intralesional triamcinolone acetonide injected only into the elevated
border.
Also, topical steroids,
Imiquimod cream.
Acanthosis Nigricans
(AN) is a nonspecific reaction pattern that may accompany
Obesity
Diabetes
Excess corticosteroids
Pineal tumors
Endocrine disorders (insulin resistance plus hyperinsulinemia)
Genetic
Drugs such as nicotinic acid, estrogens, and corticosteroids
Adenocarcinoma.
AN is classified into:
Malignant (mostly gastric cancer)
Benign (obesity, hereditary and endocrine) forms.
In all cases the disease presents with symmetric, brown thickening of
the skin.
In time the skin may become quite thickened as the lesion develops a
leathery, warty, or papillomatous surface.
The most common site of involvement is the axilla, but also flexural
areas of the posterior neck, groin, belt line, dorsal surfaces of the
fingers, mouth, and around the areolae of the breasts and umbilicus.
Rx:
A 12% ammonium lactate or Retin-A cream
Xanthomas and dyslipoproteinemia
Xanthomas are lipid deposits in the skin and tendons that occur secondary to a lipid
abnormality.
These localized deposits are yellow and are frequently very firm.
Plane xanthomas occur in several areas of the body (palms) and are flat or slightly
elevated.
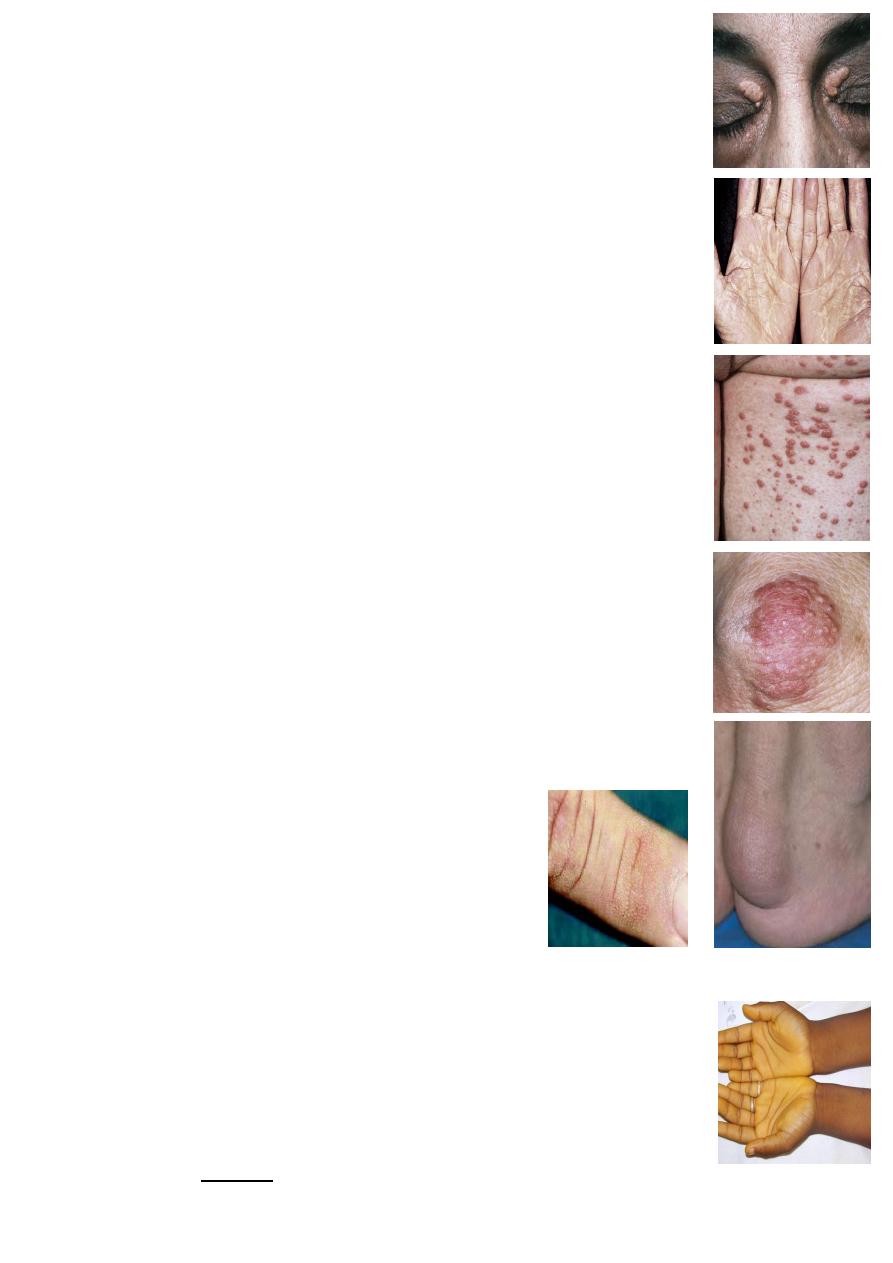
Xanthelasma
Is the most common form
About 50% of the patients with xanthelasma have normal cholesterol
levels.
However, patients with xanthelasma should be considered to have an
increased risk of cardiovascular disease independent to the level of
plasma lipids as there is increased risk for atherosclerosis.
Rx: Trichloroacetic acid (TCA).
Eruptive Xanthomas
These are yellow, 1- to 4-mm papules with a red halo around the base.
They appear suddenly in crops on extensor surfaces of the arms, legs,
and buttocks and over pressure points.
Pruritus is common.
Lesions clear rapidly when serum lipid levels are lowered.
They are a sign of hypertriglyceridemia and appear in secondary
hyperlipidemias (e.g., diabetes).
Tuberous Xanthomas
These are slowly evolving yellow papules, nodules, or mass like tumors
that occur on the knees, elbows, on the extensor surfaces
(on bone)
Tendinous Xanthomas
These smooth, deeply situated nodules are attached to tendons,
ligaments, and fascia.
They are most often found on Achilles tendons and the dorsal aspects
of the fingers.
Finger Pebbles
Finger pebbles are clinically described as fine
papillary structures over the dorsum of the
interphalangeal and metacarpophalangeal joints.
Although no definite cause for these lesions has
been identified, they are usually associated with
diabetes mellitus
Carotenemia
Carotenemia is a clinical condition characterized by yellow
pigmentation of the skin (xanthoderma) and increased beta-carotene
levels in the blood.
In most cases, the condition follows prolonged and excessive
consumption of carotene-rich foods, such as carrots and sweet
potatoes.
The condition of carotenemia is harmless, but it can lead to a mistaken
diagnosis of jaundice.
Tendinous Xanthomas
