Malignant disease of the body of the uterus
By Dr. Dalya mutheferuterine cancer.
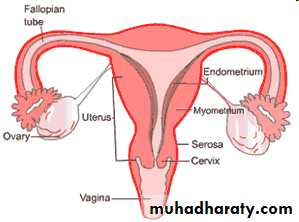
Endometrial cancer may sometimes be referred to as uterine cancer. However, different cancers may develop not only from the endometrium itself but also from other tissues of the uterus, including cervical cancer, sarcoma of the myometrium, and trophoblastic disease.Corpus cancer accounts for 3% of cancer in females.
1.Endometrial carcinoma which arise from the lining of the uterus.0r 2.Sarcoma arise from the stroma of endometrium or from myometrium.
Endometrial carcinoma
The incidence is at 60 years & more ,75% of cases usually occur in the post menopausal period
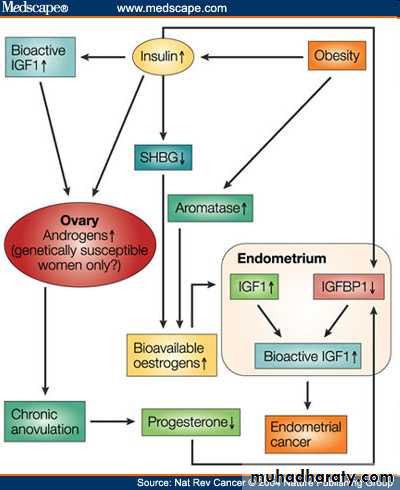
Risk factors for Endometrial Cancer
high levels of estrogenendometrial hyperplasia
obesity
hypertension
polycystic ovary syndrome[citation needed]
nulliparity (never having carried a pregnancy)
infertility (inability to become pregnant)
early menarche (onset of menstruation)
late menopause (cessation of menstruation)
endometrial polyps or other benign growths of the uterine lining
diabetes
Tamoxifen
high intake of animal fat[citation needed]
pelvic radiation therapy
breast cancer
ovarian cancer
heavy daily alcohol consumption (possibly a risk factor) [3]
Factors reduce risk of endometrial carcinoma
oral contraception.progestogens.
Smoking.
Pathology
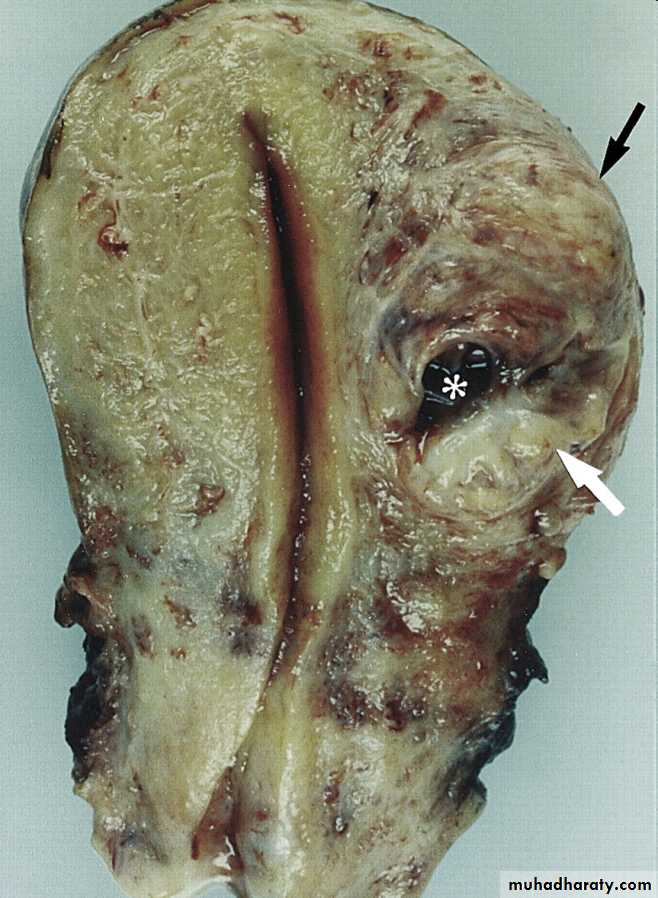
The histopathology of endometrial cancers is highly diverse. The most common finding is a well-differentiated endometrioid adenocarcinoma, which is composed of numerous, small, crowded glands with varying degrees of nuclear atypia, mitotic activity, and stratification. This often appears on a background of endometrial hyperplasia.
Lymphatic spread occurs later and is less frequent than in cases of cervical carcinoma.
Remote metastases in lungs, bones or else-where are not common but occur more often than with cervical carcinoma
Clinical presentation
Symptoms1. The classic symptom is bleeding
A. Post menopausal bleeding in 75-80 %.
This symptom should be assumed to be caused by carcinoma of endometrium until proved otherwise. Women with post menopausal bleeding in women not taking hormone replacement therapy has 10% risk of having a genital tract cancer
B. In premenopausal women may present as:
* intermenstrual bleeding
*menorrhagia.
2. Watery or purulent vaginal discharge (blood stained).
3. Pain is a late symptom and denotes extensive spread of disease.
4. Abnormal screening test.
Signs
A full general and systematic examination is indicated.
Enlarged lymph nodes in the groin or supraclavicular fossa may be found.
Breast should be palpated.
Uterine enlargement can be palpated.
Pelvic examination:
Bleeding through cervix.
Secondary metastasis in vagina, urethra.
Investigations
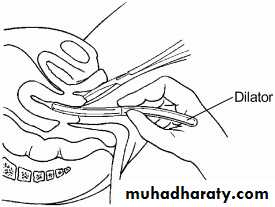
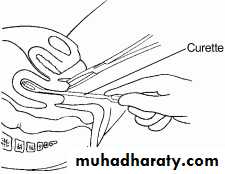
A Pap smear may be either normal or show abnormal cellular changes.Endometrial curettage is the traditional diagnostic method. Both endometrial and endocervical material should be sampled.
If endometrial curettage does not yield sufficient diagnostic material, a dilation and curettage (D&C) is necessary for diagnosing the cancer.
Hysteroscopy allows the direct visualization of the uterine cavity and can be used to detect the presence of lesions or tumours. It also permits the doctor to obtain cell samples with minimal damage to the endometrial lining (unlike blind D&C).
Endometrial biopsy or aspiration may assist the diagnosis.
Transvaginal ultrasound to evaluate the endometrial thickness in women with postmenopausal bleeding is increasingly being used to evaluate for endometrial cancer.
An endometrial thickness exceeding 4 to 5 mm on ultrasound is suggestive of endometrial pathology in such women.
Sonohysterography:
It may improve delineation of endometrial polyps.
both D&C and Pipelle biopsy curettage give 65-70% positive predictive value. But most important of these is hysteroscopy which gives 90-95% positive predictive value.
Recently, a new method of testing has been introduced called the TruTest, offered through Gynecor. It uses the small flexible Tao Brush to brush the entire lining of the uterus. This method is less painful than a pipelle biopsy and has a larger likelihood of procuring enough tissue for testing. Since it is simpler and less invasive, the TruTest can be performed as often, and at the same time as, a routine Pap smear, thus allowing for early detection and treatment
Magnetic resonance imaging (MRI):
It is expensive and not practical to screen all women.It used for evaluation of endometrial thickness and to predict myometrial invasion.
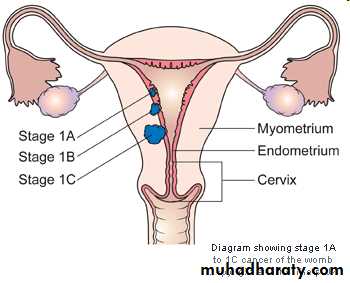
Staging of Endometrial Cancer
I: Confined to uterine corpusIA: limited to endometrium
IB: invades less than ½ of myometrium
IC: invades more than ½ of myometrium
Staging of Endometrial Cancer
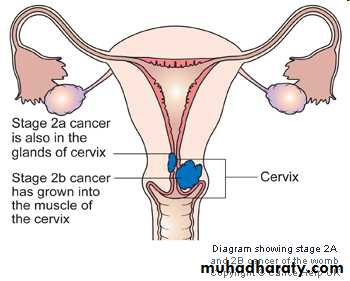
II: invades cervix but not beyond uterus
IIA: endocervical gland involvement only
IIB: cervical stroma involvement
Staging of Endometrial Cancer
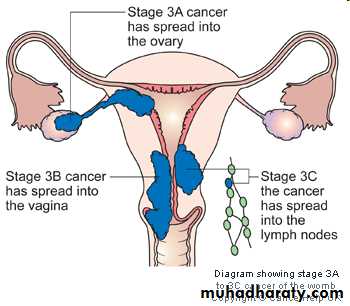
III: local and/or regional spreadIIIA: invades serosa/adnexa, or positive cytology
IIIB: vaginal metastasis
IIIC: metastasis to pelvic or para-aortic lymph nodes
Staging of Endometrial Cancer
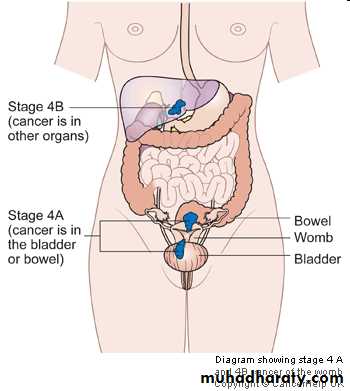
IVA: invades bladder/bowel mucosaIVB: distant metastasis
Five Year Survival
Stage I: 81-91%72% diagnosed at this stage
Stage II: 71-78%
Stage III: 52-60%
Stage IV: 14-17%
3% diagnosed at this stage
Spread Patterns
Direct extensionmost common
Transtubal
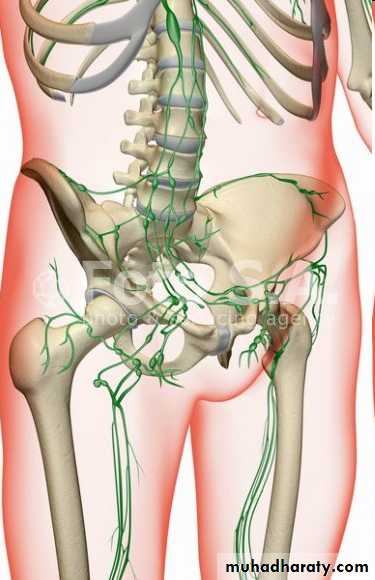
Lymphatic
Pelvic usually first, then para-aortic
Hematogenous
Lung most common
Liver, brain, bone
Treatment
Stage IB or less: total hyst/BSO/PPALND, cytologyStage IC to IIB: total hyst/BSO/PPALND, cytology, adjuvant pelvic XRT
Stage III: total hyst/BSO/PPALND, cytology, adjuvant chemotherapy
Stage IV: palliative XRT and chemotherapy
Methods of Endometrial Cancer Treatment:
The treatment of endometrial carcinoma is usually:* surgical.
* Radiotherapy
* Hormone therapy: Progestogens inhibit the rate of growth and spread of endometrial carcinoma.
Other Types of Uterine Cancer
LeiomyosarcomaRapidly growing fibroid should be evaluated
Stromal sarcoma
Carcinosarcoma (MMMT)
leiomyosarcoma
MMMTUterine Sarcomas
Account for fewer than 10% of all corpus cancers.Types:
( Carcinosarcoma, leiomyosarcoma, Endometrial stromal sarcoma, adenosarcoma)
Exposure to radiation may enhance the development of pelvic sarcomas
Abnormal vaginal bleeding most frequent presenting symptom for all histologic types.
No specific staging system (commonly use staging of endometrial carcinoma)
Management of Uterine Sarcomas:
Surgery is the hallmark of treatment with total abdominal hysterectomy and bilateral salpingo-oopherectomy (TAH/BSO) being the standard procedure.