Lecture-3
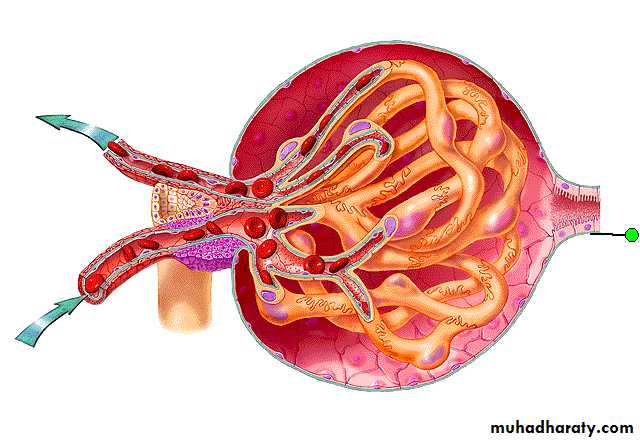
Forces that regulate GFR:Forces favoring filtration (mmHg):
Glomerular hydrostatic pressure = 60 mmHg.
Bowman’s capsule colloid osmotic pressure = 0 mmHg.
Forces opposing filtration (mmHg):
Bowman’s capsule hydrostatic pressure = 18 mmHg.
Glomerular capillary colloid osmotic pressure = 32 mmHg.
Net filtration pressure = 60- 18 - 32 = 10 mm Hg.
H Pr = 18 mmHg
Osm Pr = 0mmHg
H Pr = 60 mmHg
Osm Pr= 32mmHg
Physiological control of renal blood flow (RBF) and GFR
The factors that affect the RBF and GFR are:Neural factor
Hormonal factor
Autoregulation
Neural factor (Sympathetic nervous system):
All the blood vessels of kidneys are richly innervated by sympathetic nerve fibers. Strong activation of renal sympathetic nervous can constrict the renal arterioles and decrease RBF and GFR.
NOTE: Renal sympathetic nerves stimulation are important in reducing RBF and GFR during sever hemorrhage or brain ischemia this will lead to decrease the GFR and decrease the urine out- put and keep the blood volume within normal .
Hormonal factors:
Norepinephrine, Epinephrine, and Endothelin: constrict blood vessels and decrease RBF & GFR. Blood level of these hormones parallel the activity of the sympathetic nervous system especially under extreme conditions such as sever hemorrhage and brain ischemia.
Angiotensin II: constrict efferent arterioles lead to increase GFR.
Endothelial-derived Nitric Oxide: decrease renal vascular resistance and increase RBF and GFR.
Prostaglandin and Bradykinin: tend to increase GFR.
Auto-regulation of GFR and renal blood flow:
It is intrinsic mechanism by which the kidneys normally keep renal blood flow and GFR relatively constant, despite marked changes in arterial blood pressure.
For example: Normally GFR is about 180 L/ day and tubular reabsorption is 178.5 L / day, leaving 1.5 L / day of fluid excreted in the urine. In the absence of autoregulation a relatively small increase in blood pressure (100→125 mmHg) would cause an increase in GFR (180→225 L/ day) if tubular reabsorption remained constant at (178.5 L/day), this increase urine flow to 46.5 L/day, increase in urine of more than 30 fold. This change would quickly deplete the blood volume,
but such change in arterial pressure exert less effect on urine volume…How?
There are negative feedback mechanism provide the degree of GFR and renal blood flow that is required. These mechanisms are:
Tubuloglomerular mechanism: Which occur through:
The afferent arteriolar vasodilator feedback mechanism:
In cases of low GFR (for any causes like dehydration, hypervolemia) causes a low flow rate of tubular fluid which lead to over absorption of Na and Cl ions in ascending limb of the loop of Henle and decrease the ion concentration at the macula densa, this decrease in ion concentration initiates a signal from the macula densa to dilate the afferent arteriole with result to an increased blood flow into glomerulus causing an increase in glomerular pressure and GFR back toward the required level.
B. The efferent arteriolar vasoconstrictor feedback mechanism:
In cases of low Na an Cl ions at the macula densa cause stimulation for Juxtaglomerulus cells to release renin, this in turn causes the formation of angiotensin II, which constrict efferent arterioles more than afferent arterioles, cause increase the pressure in glomerulus and this leading to increase in GFR back to normal.
NOTE: Renin is an enzyme that release from renal Juxtaglomerular cells and act on angiotensinogen. It increase if: Renal perfusion pressure and renal blood flow is decreased and in stimulation of renal nerve.
Myogenic mechanism: When arterial pressure rises, stretches the wall of the arteriole, this in turn causes a secondary constriction of the arteriole, this decreases the renal blood flow and GFR back toward normal. When pressure falls too low, allows the artery to dilate and therefore increase the blood flow and GFR.
Absorption and secretion of tubules
Basic mechanism of absorption and secretion of PCT:
Normally about 65% of filtered Na, water, and lower percentage of Cl, much of K, Ca, phosphate and urea almost all the filtered glucose, amino acid, organic acids, small amount of protein, are reabsorbed here.
Na ions are reabsorbed by passive diffusion, facilitated diffusion (by co-transport with glucose, amino acids, and by counter-transport in an exchange with H ions). All are depending primarily on the electrochemical gradient of Na ions created by active Na-K ATPase pump.
Cl ions are reabsorbed by passive and co-transport mechanisms.
Water is reabsorbed by osmosis.
Proteins are reabsorbed through the brush border of the proximal tubule by process of pinocytosis.
The concentration of Na and the total osmolarity remains relatively constant (isotonic) because water reabsorption proportional to Na reabsorption.
The proximal tubules is also the site for secretion of organic acids and bases (bile salts, oxalate, urate, catecholamines), drugs and toxins.
Basic mechanism of absorption and secretion of loop of Henle:
About 20% of filtered water is reabsorbed in the thin descending limb.
About 25% of filtered Na, Cl and K(other ions such as Ca, HCO3, Mg) are reabsorbed in the thick ascending limb.
Na ions are reabsorbed by secondary active to Na-K-2Cl co-transport and by Na-H secondary active counter-transport mechanisms.
Because the thick segment of ascending loop of Henle is impermeable to water, most of the water remain in tubule, tubular fluid becomes very dilutes as it flow toward the distal tubule (hypotonic).
Basic mechanism of absorption and secretion of DCT:
Early part of the distal convoluted tubules:
Has characteristic of thick segment of ascending limb of loop of Henle.
It reabsorbs most of ions including Na, K, Cl, impermeable to water and urea.
The second half of the DCT and cortical collecting tubules are:
Reabsorb of Na ion in an exchange with K ions (via Na-K ATPase pump) under effect of aldosterone hormone.
Secretion of H ions by (H-ATPase pump).
Permeability to water is controlled by ADH. These segments are permeable to water in present ADH and impermeable to water in absent of this hormone.
Basic mechanism of absorption and secretion of medullary collecting ducts:
Reabsorb of less than 10% of the filtered water and Na under the control of ADH.
Secreting H ions against concentration gradient.
Permeable to urea.
So it plays an important role in determining the final urine output of water and solutes.