1
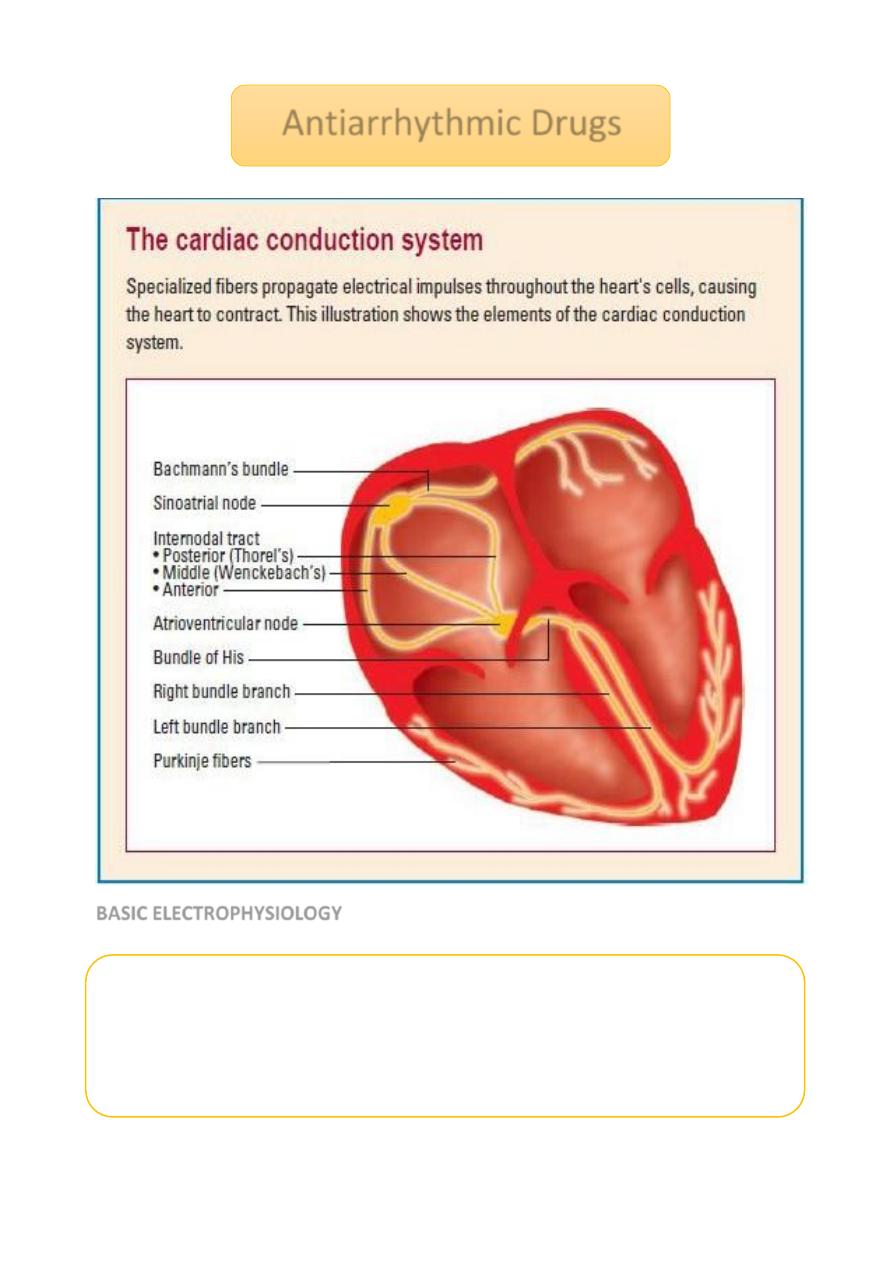
BASIC ELECTROPHYSIOLOGY
Antiarrhythmic Drugs
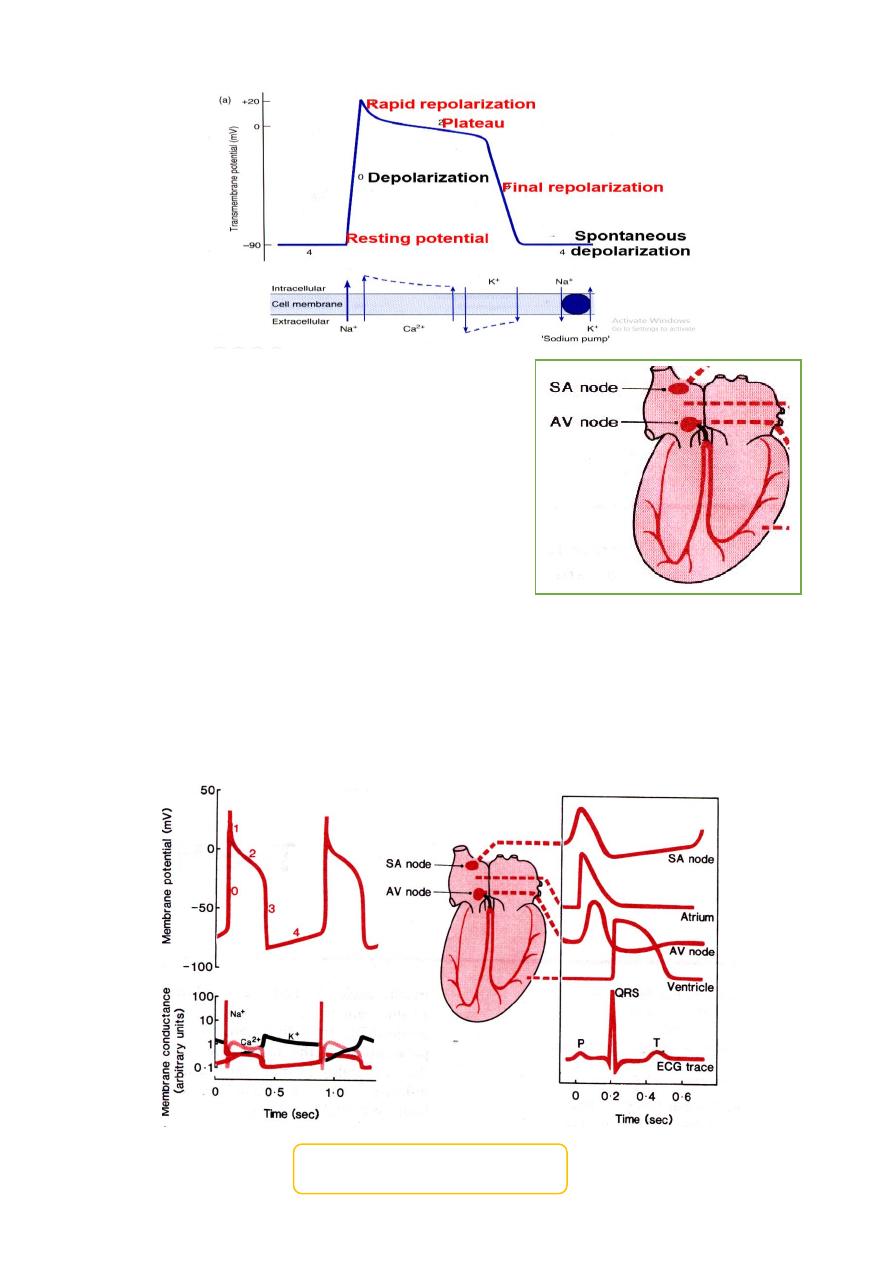
Myocardial cells maintain transmembrane ion gradients by movement of the
Na
+
, Ca
2+
and K
+
through membrane channels.
The resting potential of a cardiac cell is– 85 mV compared to the extracellular
environment.
Depolarization is initiated by a rapid influx of Na
+
(phase 0).
2
In the AV node depolarization is due to the
slower influx of calcium ions.
This results in slower conduction of the
impulse through the AV node than in other
parts of the heart.
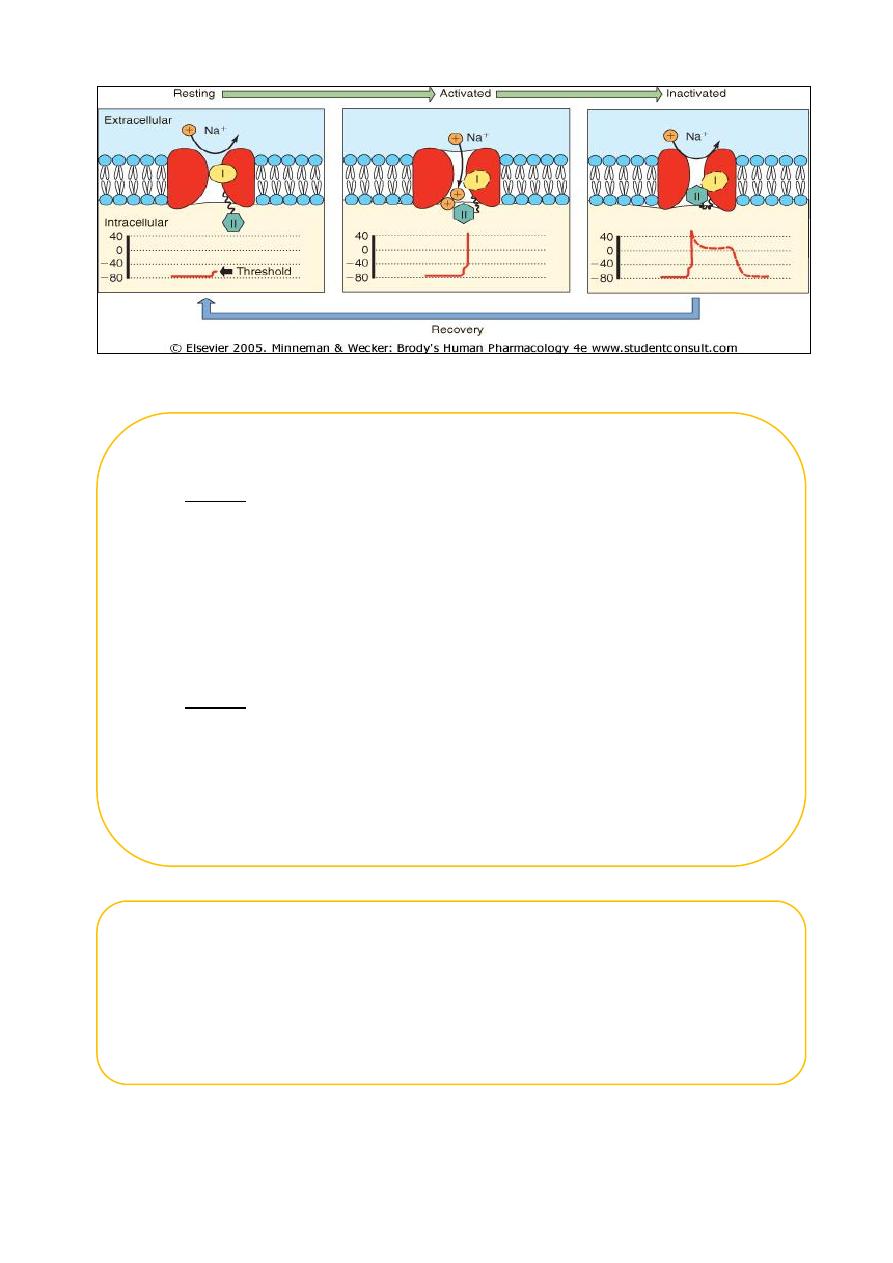
During the period between phase 0 and the end of phase 2, the cell is refractory to the
further depolarization (absolute refractory period) since the sodium channels are
inactivated.
During phase 3, a sufficiently large stimulus can open enough sodium channels to over-
come the potassium efflux. This is the relative refractory period.
The cardiac action potential
3
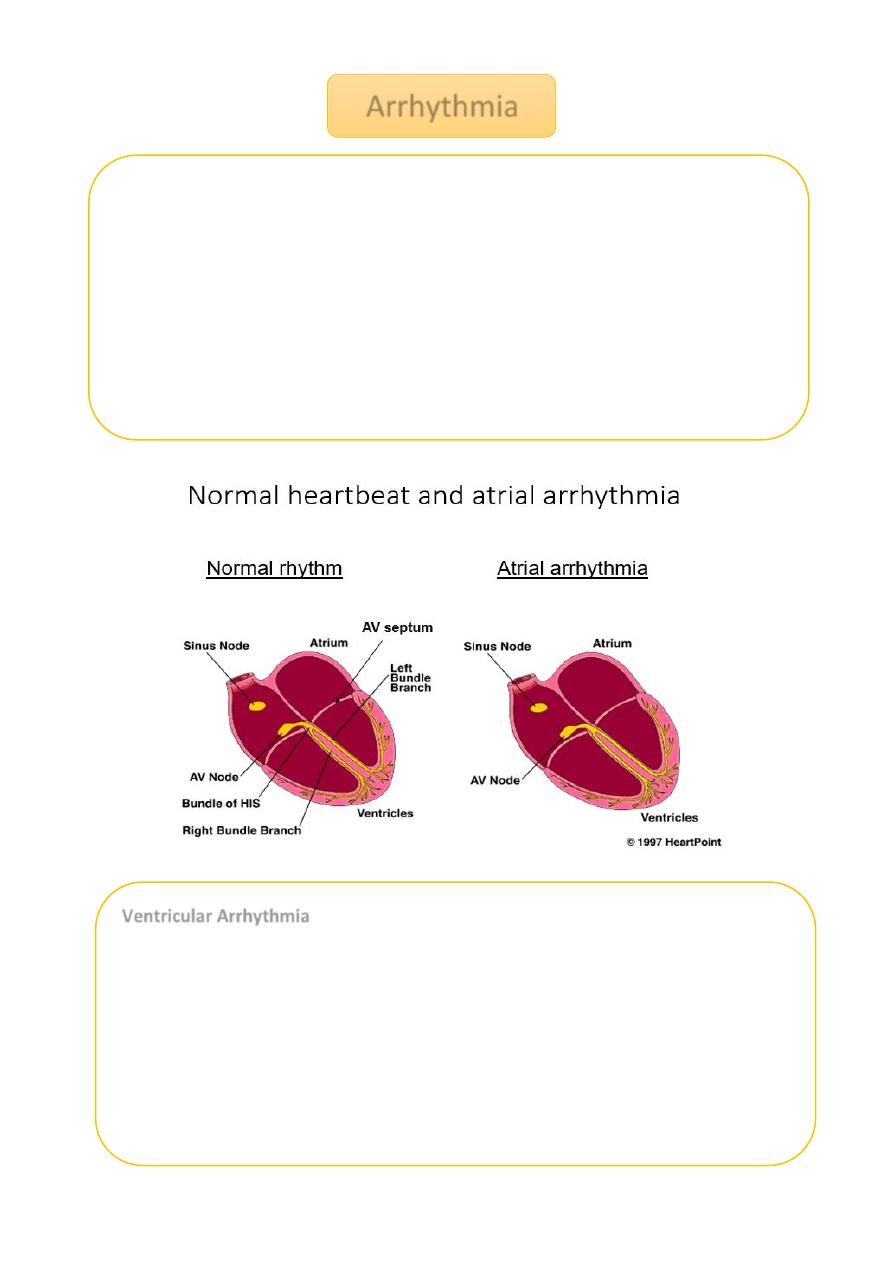
Arrhythmia
Heart condition where disturbances in
Pacemaker impulse formation
Contraction impulse conduction
Combination of the two
Results in rate and/or timing of contraction of heart muscle that is insufficient to
maintain normal cardiac output (CO)
To understand how antiarrhythmic drugs work, need to understand
electrophysiology of normal contraction of heart
Ventricular Arrhythmia
Ventricular arrhythmias are common in most people and are usually not a
problem but…
VA’s are most common cause of sudden death
Majority of sudden death occurs in people with neither a previously
known heart disease nor history of VA’s
Medications which decrease incidence of VA’s do not decrease (and may
increase) the risk of sudden death treatment may be worse then the
disease!
4
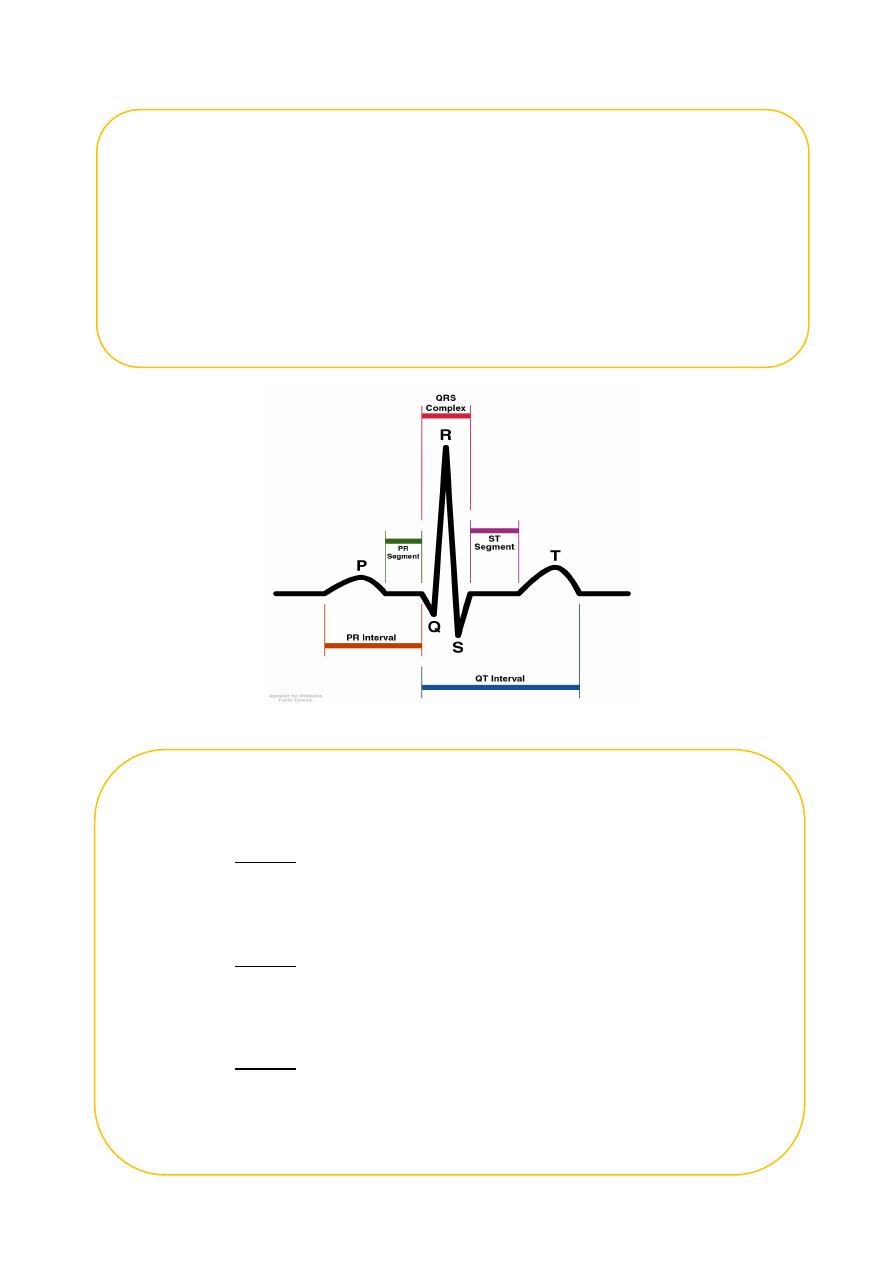
ECG (EKG) showing wave segments
Electrophysiology - resting potential
A transmembrane electrical gradient (potential) is maintained, with the
interior of the cell negative with respect to outside the cell
Caused by unequal distribution of ions inside vs. outside cell
o Na
+
higher outside than inside cell
o Ca
+
much higher “ “ “ “
o K
+
higher inside cell than outside
o Maintenance by ion selective channels, active pumps and exchangers
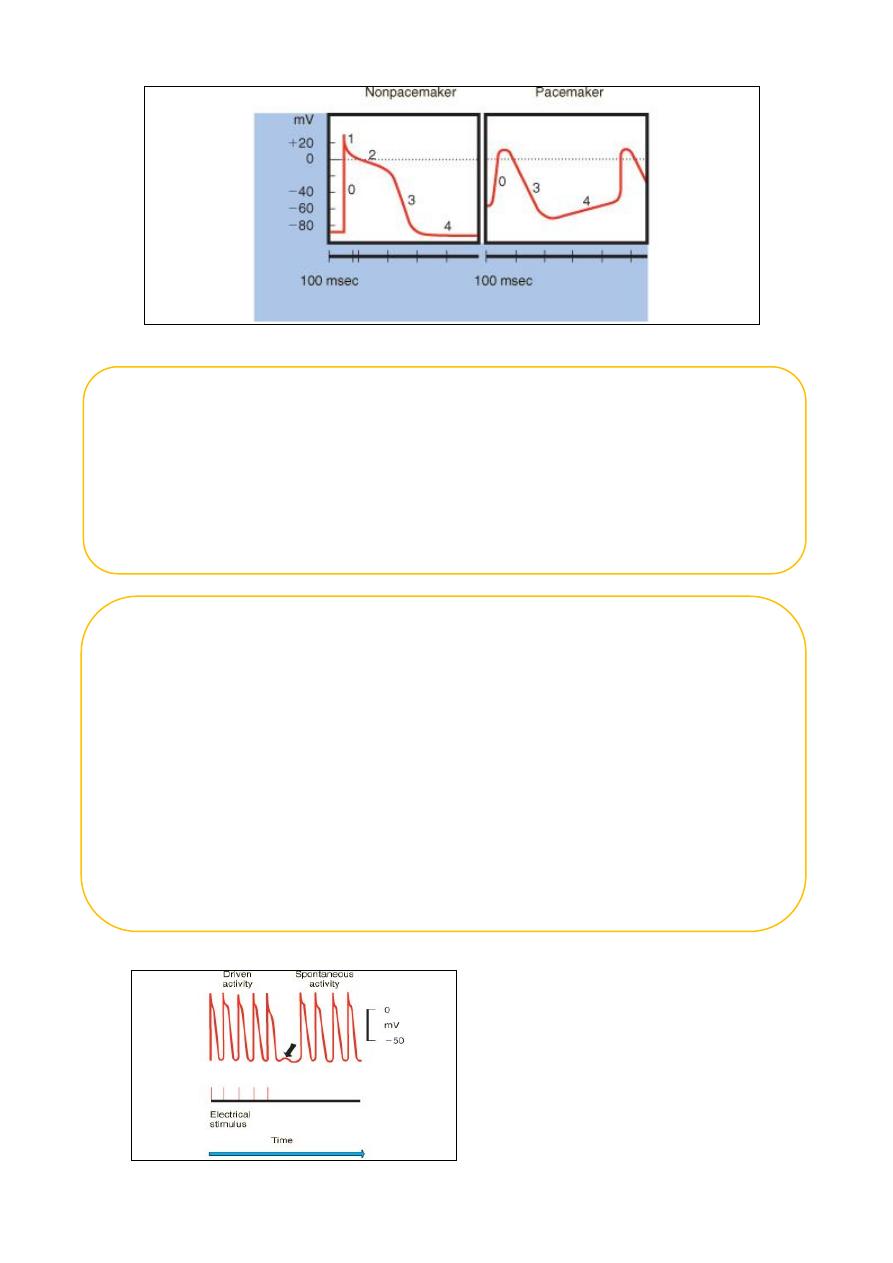
Cardiac Action Potential
Divided into five phases (0,1,2,3,4)
o Phase 4 - resting phase (resting membrane potential)
Phase cardiac cells remain in until stimulated
Associated with diastole portion of heart cycle
Addition of current into cardiac muscle (stimulation) causes
o Phase 0 – opening of fast Na channels and rapid depolarization
Drives Na
+
into cell (inward current), changing membrane
potential
Transient outward current due to movement of Cl
-
and K
+
o Phase 1 – initial rapid repolarization
Closure of the fast Na
+
channels
Phase 0 and 1 together correspond to the R and S waves of
the ECG
5
Cardiac Na+ channels
Differences between nonpacemaker and pacemaker cell action potentials
PCs - Slow, continuous depolarization during rest
Continuously moves potential towards threshold for a new action potential
(called a phase 4 depolarization)
Cardiac Action Potential (con’t)
Phase 2 - plateau phase
o sustained by the balance between the inward movement of Ca
+
and outward movement of K
+
o Has a long duration compared to other nerve and muscle tissue
o Normally blocks any premature stimulator signals (other muscle
tissue can accept additional stimulation and increase contractility
in a summation effect)
o Corresponds to ST segment of the ECG.
Phase 3 – repolarization
o K
+
channels remain open,
o Allows K
+
to build up outside the cell, causing the cell to repolarize
o K
+
channels finally close when membrane potential reaches certain
level
o Corresponds to T wave on the ECG
6
Mechanisms of Cardiac Arrhythmias
Result from disorders of impulse formation, conduction, or both
Causes of arrhythmias
o Cardiac ischemia
o Excessive discharge or sensitivity to autonomic transmitters
o Exposure to toxic substances
o Unknown etiology
Disorders of impulse formation
No signal from the pacemaker site
Development of an ectopic pacemaker
o May arise from conduction cells (most are capable of spontaneous activity)
o Usually under control of SA node if it slows down too much conduction
cells could become dominant
o Often a result of other injury (ischemia, hypoxia)
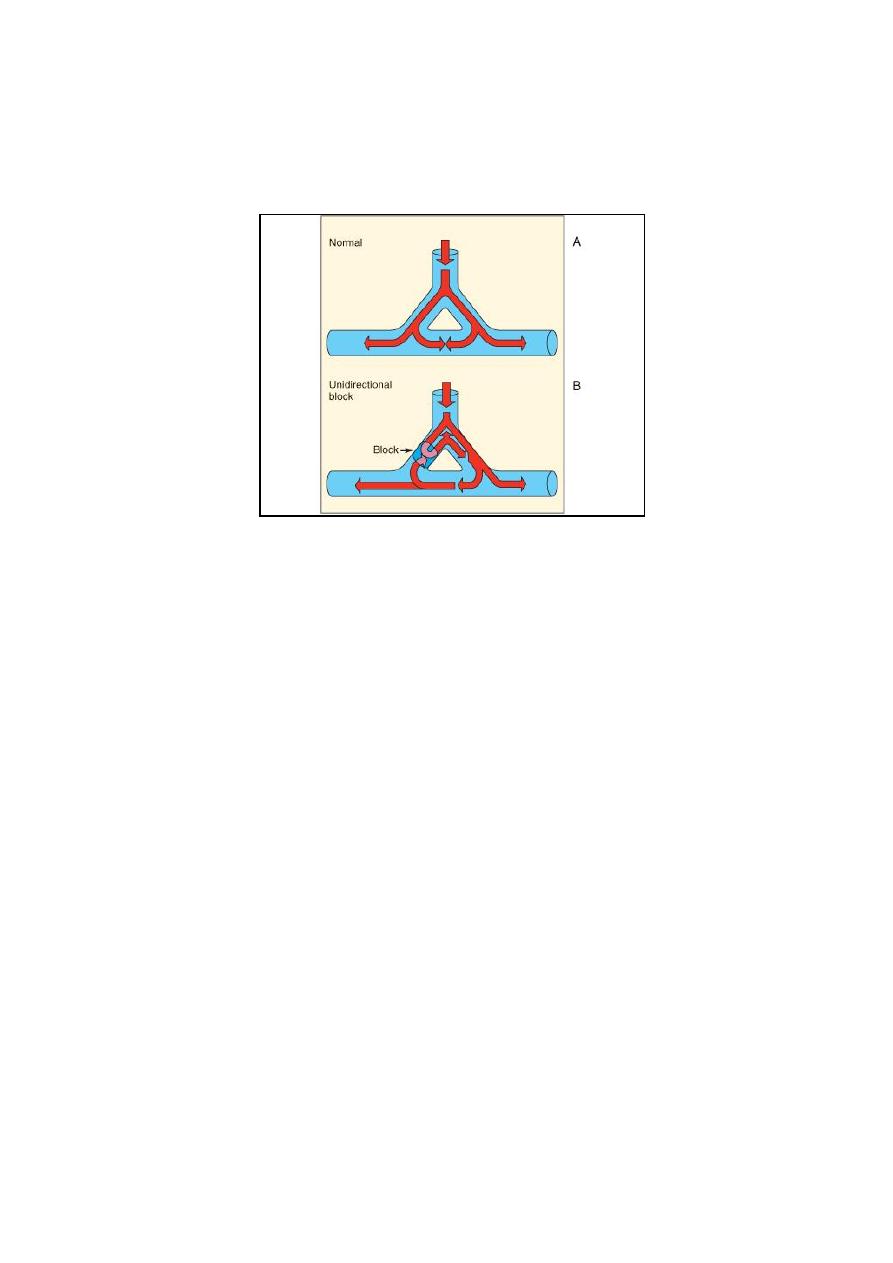
Development of oscillatory afterdepolariztions
o Can initiate spontaneous activity in nonpacemaker tissue
o May be result of drugs (digitalis, norepinephrine) used to treat other
o cardiopathologies
Afterdepolarizations
7
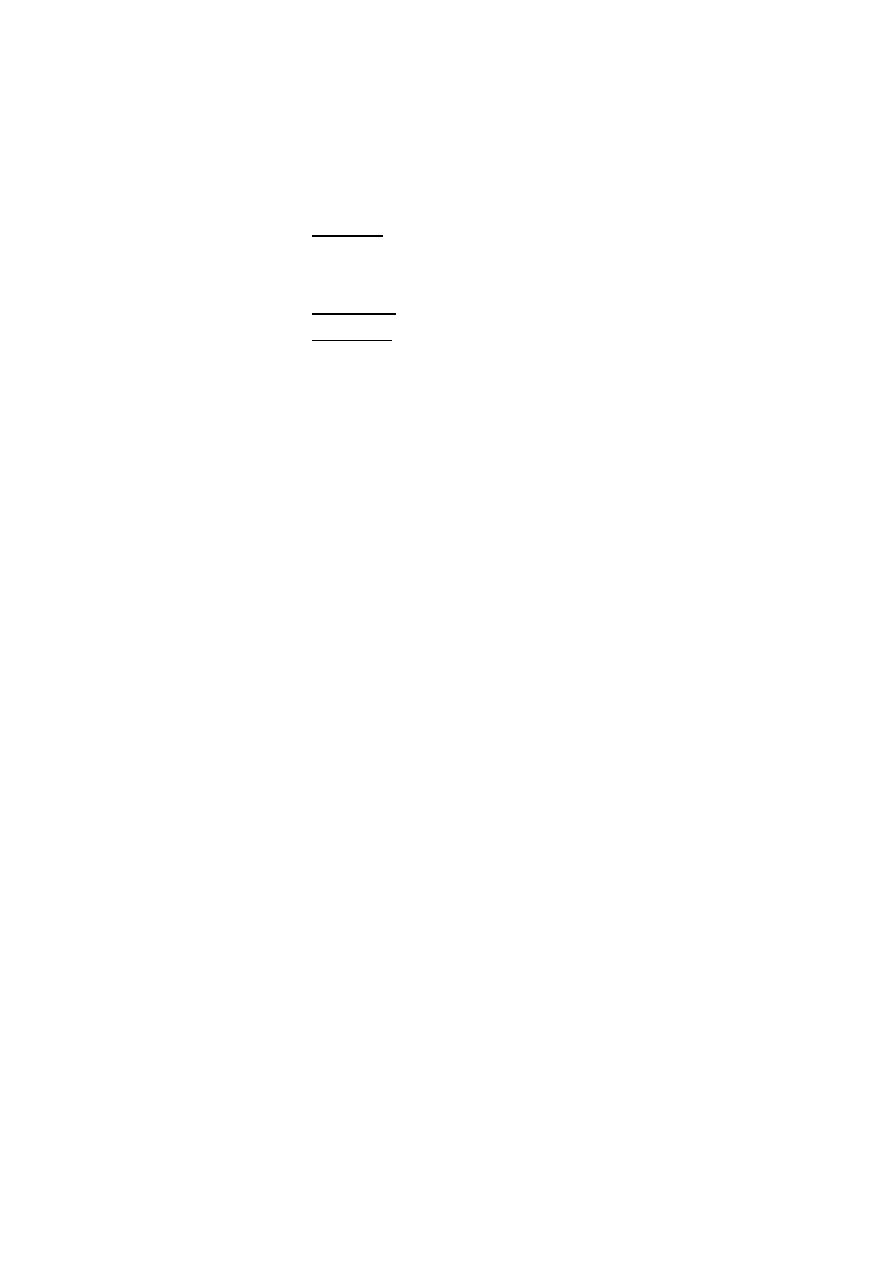
Disorders of impulse conduction
May result in
o Bradycardia (if have AV block)
o Tachycardia (if reentrant circuit occurs)
Reentrant circuit
Antiarrhythmic drugs
Biggest problem – antiarrhythmics can cause arrhythmia!
Example: Treatment of a non-life threatening tachycardia may cause fatal
ventricular arrhythmia
Must be vigilant in determining dosing, blood levels, and in follow-up when
prescribing antiarrhythmics
Therapeutic overview
Na
+
channel blockade
β-adrenergic receptor blockade
Prolong repolarization
Ca
2+
channel blockade
Adenosine
Digitalis glycosides
Classification of antiarrhythmics (based on mechanisms of action)
Class I – blocker’s of fast Na
+
channels
o Subclass IA
Cause moderate Phase 0 depression
Prolong repolarization
Increased duration of action potential

8
Includes
Quinidine – 1
st
antiarrhythmic used, treat both atrial and
ventricular arrhythmias, increases refractory period
Procainamide - increases refractory period but side effects
Disopyramide – extended duration of action, used only for
treating ventricular arrthymias
Class IA - Na+ Channel Blockers
Procainamide/Quinidine/Disopyramide
Mode of action
o Depress conduction and prolong refractoriness
Atrial, His-Purkinje, ventricular tissue
o Peripheral alpha block
o Vagolytic
o Negative inotrope
ECG changes
o Increase PR, QRS (Diso: PR á > QRS á )
o Toxicity: QTc increases by 30% or QT > 0.5 sec
o Ca
++
channel blockade / potent anticholinergic (Diso)
Uses
o SVT (reentry) or VT
o Afib/flutter (on digoxin)
Drug interactions-Decrease metabolism of Amiodarone
Dose
o IV: load 15 mg/kg over 1 hour, then 30-80 mg/kg/min
(level 5-10 ng/ml)
o PO: 30-70 mg/kg/day
Side effects: Lupus- in slow acetylators
o ANA + : 50-90% Symptoms: 20-30 %
Arrhythmia Therapy
Procainamide has been a long-used intravenous
o infusion for a wide range of dysrhythmias:
o Narrow complex tachycardia:
Atrial tachycardia, resistant re-entrant tachycardia
o Wide-complex tachycardia:
Ventricular tachycardia
Downside:
o Side effects, negative inotrope, pro-arrhythmic
9
Subclass IB
Weak Phase 0 depression
Shortened depolarization
Decreased action potential duration
Includes
Lidocane (also acts as local anesthetic) – blocks Na+ channels
mostly in ventricular cells, also good for digitalis-associated
arrhythmias
Mexiletine - oral lidocaine derivative, similar activity
Phenytoin – anticonvulsant that also works as antiarrhythmic
similar to lidocane
Class IB
Lidocaine/Mexiletine/Phenytoin
Mode of action
o Little effect on normal tissues
o Decreases Purkinje ERP/ automaticity
o Increases Ventricular fibrillation threshold
o Depresses conduction, esp. at high rates (Mexiletine)
o Suppresses dig-induced delayed afterdepolarizations (Phenytoin)
ECG changes
o Slight ↓ QTc (Lidocaine/Phenytoin)
Class IB Lidocaine
Use: VT (acute)
o Acts rapidly; no depression of contractility/AV conduction
Kinetics
o t
1/2
: 5-10 min (1st phase); 80-110 min (2nd phase)
Drug interactions
o Decreased metabolism w/ CHF/hepatic failure, propranolol, cimetidine
o Increased metabolism w/ isuprel, phenobarbital, phenytoin
Dose
o 1 mg/kg, then 20-50 mg/kg/min (level: 2-5 mg/ml)
Side effects
o CNS toxicity w/ levels > 5 mg/ml
Class IB Mexiletine
Use: VT (post-op CHD)
Kinetics: t
1/2
= 8 - 12 hrs
Drug interactions- rare
Dose

10
3-5 mg/kg/dose (adult 200-300mg/dose) po q 8 hrs
Side effects
Nausea (40%)
CNS - dizziness/tremor (25%)
Class IB Phenytoin
Uses
VT (post-op CHD), digoxin-induced arrhythmias
Drug interactions
Coumadin- á PT; Verapamil- á effect (displaces from protein)
Dose
PO: 4 mg/kg q 6 hrs x 1 day, then 5-6 mg/kg/day ÷ q 12hr
IV: bolus 15 mg/kg over 1 hr; level 15-20 mg/ml
Side effects
Hypotension, gingival hyperplasia, rash
Arrhythmia-focused Therapy
Class IB antiarrhythmics are very effective and very safe.
Little or no effect on “normal” tissues
First line for ischemic, automatic arrhythmia's (Ventricular tachycardia)
Not a lot of effect on normal conduction tissue – not a good medicine for reentry
and atrial tachycardias.
Subclass IC
Strong Phase 0 depression
No effect of depolarization
No effect on action potential duration
Includes
1. Flecainide (initially developed as a local anesthetic)
Slows conduction in all parts of heart,
Also inhibits abnormal automaticity
2. Propafenone
Also slows conduction
Weak β – blocker
Also some Ca
2+
channel blockade
11
Class IC
Flecainide/Propafenone/Ethmozine
Mode of action
o Depresses abnormal automaticity (Flec/Ethmozine)
o Slows conduction in AV node, AP, ventricle (Flec/Prop)
o Shortens repolarization (Ethmozine)
o Negative inotrope (Propafenone)
o Prolongs atrial/ventricular refractoriness (Propafenone)
ECG changes
o ↑ PR, QRS
o ↑ QTc (Propafenone)
Uses: PJRT, AET, CAT, SVT, VT, Afib
Kinetics
t
1/2
= 13 hrs (shorter if between 1-15 mos old)
Drug interactions
Increases digoxin levels (slight)
Amiodarone: increases flecainide levels
Dose
70-225 mg/m
2
/day ÷ q 8-12 hr
Level: 0.2-1.0 mg/ml
Side effects
Negative inotrope- use in normal hearts only (NO POST-OPs)
PROARRHYTHMIA - 5-12% (CAST)
Arrhythmia –focused Therapy
• IC’s have a lot of side effects that make them appropriate for use only by
experienced providers.
Class II – β–adrenergic blockers
Based on two major actions
1. blockade of myocardial β–adrenergic receptors
2. Direct membrane-stabilizing effects related to Na
+
channel blockade
Includes
Propranolol
• causes both myocardial β–adrenergic blockade and membrane-stabilizing
effects
• Slows SA node and ectopic pacemaking
• Can block arrhythmias induced by exercise or apprehension
• Other β–adrenergic blockers have similar therapeutic effect

12
Metoprolol
Nadolol
Atenolol
Acebutolol
Pindolol
Stalol
Timolol
Esmolol
Class III – K
+
channel blockers
1. Developed because some patients negatively sensitive to Na channel
blockers (they died!)
2. Cause delay in repolarization and prolonged refractory period
Includes
Amiodarone – prolongs action potential by delaying K
+
efflux but many other
effects characteristic of other classes
Ibutilide – slows inward movement of Na
+
in addition to delaying K
+
influx.
Bretylium – first developed to treat hypertension but found to also suppress
ventricular fibrillation associated with myocardial infarction
Dofetilide - prolongs action potential by delaying K
+
efflux with no other effects
Can be very powerful antiarrhythmics but limited indications for first-line use – beyond
the spectrum of primary care providers
Amiodarone: may become a first-line medicine for a broad spectrum of arrhythmias,
currently still high-risk
Class IV – Ca
2+
channel blockers
slow rate of AV-conduction in patients with atrial fibrillation
Includes
Verapamil – blocks Na
+
channels in addition to Ca
2+;
also slows SA node in
tachycardia
Diltiazem
Purinergic Agonists
Adenosine
Mode of action
• Vagotonic
• Anti-adrenergic
• Depresses slow inward Ca
++
current
• Increases K
+
conductance (hyperpolarizes)
13
ECG/EP changes
• Slows AV node conduction
Uses
• SVT- termination of reentry
• Aflutter- AV block for diagnosis
Kinetics
• t
1/2
= < 10 secs
• Metabolized by RBCs and vascular endothelial cells
Dose
• IV: 100-300 mg/kg IV bolus
Drug interactions
• Methylxanthines (caffeine/theophylline)
Side effects
• AFib/ sinus arrest/ sinus bradycardia
• Bronchospasm
• Flushing/headache
• Nausea
Great medicine: quick onset, quick degradation.
Digoxin
Mode of action
• Na-K ATPase inhibition
• Positive inotrope
• Vagotonic
ECG changes
• Increases PR interval
• Depresses ST segment
• Decreases QT interval
Use: SVT (not WPW)
Kinetics
• t
1/2
= preemie (61hrs), neonate (35hrs), infant (18hrs), child (37hrs), adult
(35-48hrs )
14
Interactions
Coumadin- ↑ PT
↑ Digoxin level
Quinidine, amiodarone, verapamil
↓ renal function/renal tubular excretion (Spironolactone)
Worse with ↓ K
+
, ↓ Ca
++
Digoxin Toxicity
Nausea/vomiting, lethargy, visual changes
Metabolic
• Hyper K
+
, Ca
++
• Hypo K
+
, Mg
++
• Hypoxemia
• Hypothyroidism
Proarrhythmia
• AV block- decreased conduction
• SVT- increased automaticity
• VT- delayed afterdepolarizations
Digoxin Toxicity
Treatment
• GI decontamination
o Ipecac/lavage/charcoal w/ cathartic
• Arrhythmias
o SA node /AV node depression- Atropine; if dig > 6, may need pacing
o SVT- Phenytoin or b -blocker
o VT- Lidocaine (1 mg/kg) or Phenytoin
• DC Cardioversion may cause refractory VT/VF!!
Mubark A. Wilkins
