Physiology of cardiovascular system l 3,4 Dr.Abdul-Aziz Ahmed
Refractory Period
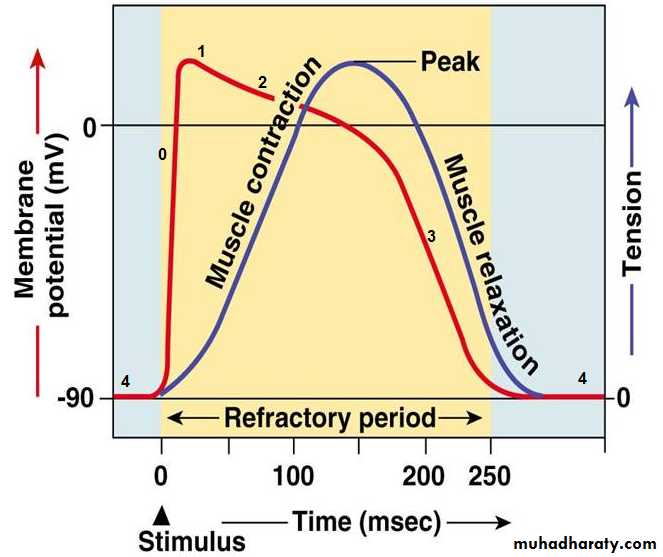
Following contraction, the cardiac myocytes must enter a relaxation or refractory phase during which they cannot be depolarized. The refractory period is defined by the time interval following excitation during which the cell remains unexcitable. This is due to the lack of availability of depolarizing current (which is Na+ in muscle cells). It is classified as either absolute or relative, depending on whether it is completely unexcitable or needs a greater stimulus than normal. The refractory period of cardiac muscle is almost as long as the contraction period. The long refractory period means that cardiac muscle cannot be restimulated until contraction is almost over and this makes summation and tetanization of cardiac muscle impossible. This is essential in maintaining the alternating contraction and relaxation of cardiac muscles which is essential to the pumping action of the heart and for the prevention of fatal arrhythmias.Figure 1: the refractory period.
The ventricular muscle cells have a long, effective (absolute) refractory period from the onset of phase 0 to midway through phase 3. This protects against circular (reentry) conduction, in which control by the pacemaker fails and each spread of excitation through the ventricles triggers the next. Treatment with drugs such as beta blockers and calcium channel blockers, which extend the refractory period, can be effective at preventing reentry arrhythmias. The long refractory period of the AV nodal cells also protects against conduction of rapid atrial arrhythmias to the ventricles.SA node as the pacemaker of the heart
The SA node is the normal pacemaker of the heart because it has the most rapid firing rate (70-80 impulse/min). Thus, each time the sinus node discharges, its impulse is conducted into different part of the cardiac muscle, leading to depolarization of all cardiac tissues. During this time all parts of the heart will be in refractory state, thus they cannot respond to another impulse developed in A-V node or other excited fibers within the heart. The pacemaker of the heart shifts from the sinus node to other area whensome other part of the heart like A-V node or the Purkinje fibers develops a rhythmical discharge rate that is more rapid than that of the sinus node.
The AV node becomes the pacemaker if the SA node fails or transmission to the AV node fails. These patients are in AV nodal rhythm and typically have resting heart rates of 45–55 beats/min.
In patients with complete heart block, there is no transmission through the AV node; the His-Purkinje fibers pace the heart between 20 and 40 beats/min.
A pacemaker elsewhere than the sinus node is called an “ectopic” pacemaker.
Electrocardiography
The ECG is a recording of the electrical activity of the heart. The electrical currents generated by the heart spread through the body to the skin, where they can be sensed by appropriately placed electrodes, amplified, and viewed on an oscilloscope or chart recorder. A standard ECG is obtained by placing an electrode on each limb and at six specific locations on the anterior chest wall. In a lead, one electrode is regarded as the positive side of a voltmeter and another is the negative
side.
ECG Leads
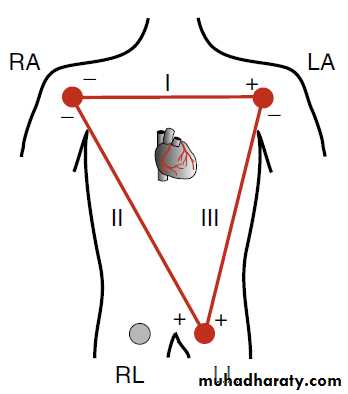
A lead reports changes in voltage difference between the positive and negative electrodes. By varying which electrode is regarded as positive or which is negative, a standard set of 12 leads provides a range of views of electrical events in the heart:1.Bipolar limb Leads(standard limb leads) include :
lead I, the positive electrodes are connected to the left arm and negative electrodes are connected to the right arm.
lead II, positive electrodes are connected to the left leg and negative electrodes are connected to the right arm.
lead III the positive electrodes are connected to the left leg and negative electrodes are connected to the left arm.
Figure2: Bipolar limb Leads
2.Unipolar limb Leads (Augmented limb leads) include :Leads aVR: the exploring electrode on (right arm), and the left arm and left leg connected together to form an indifferent electrode.
Lead aVL: the exploring electrode on (left arm), and the right arm and left leg connected together to form an indifferent electrode.
Lead aVF: the exploring electrode on (left foot), and the left arm and right connected together to form an indifferent electrode.
The unipolar limb leads designated by the letter a (aVR, aVL, aVF), because their potential is amplified by 50% without any change in configuration.
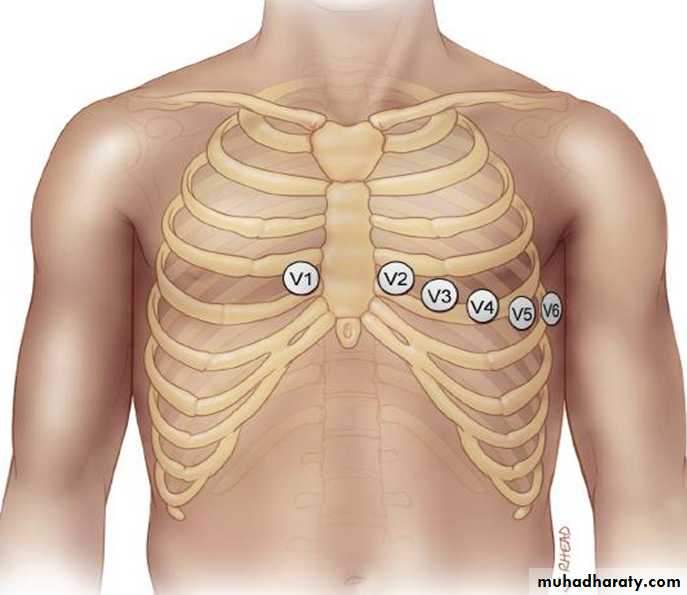
3.Unipolar chest Leads include :
lead V1,the exploring electrode placed in the fourth intercostal space, just to the right of the sternum.
lead V2, the exploring electrode placed in the fourth intercostal space, just to the left of the sternum.
lead V3, the exploring electrode placed in the midway between V2 and V4.
lead V4, the exploring electrode placed in the midclavicular line, left fifth intercostal space.
lead V5, the exploring electrode placed in the anterior axillary line, left fifth intercostal space.
lead V6, the exploring electrode placed in the midaxillary line, left fifth intercostal space.
Figure3 .Unipolar chest Leads
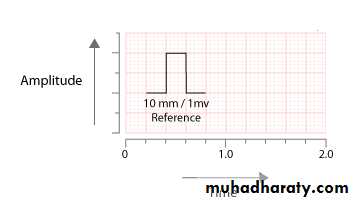
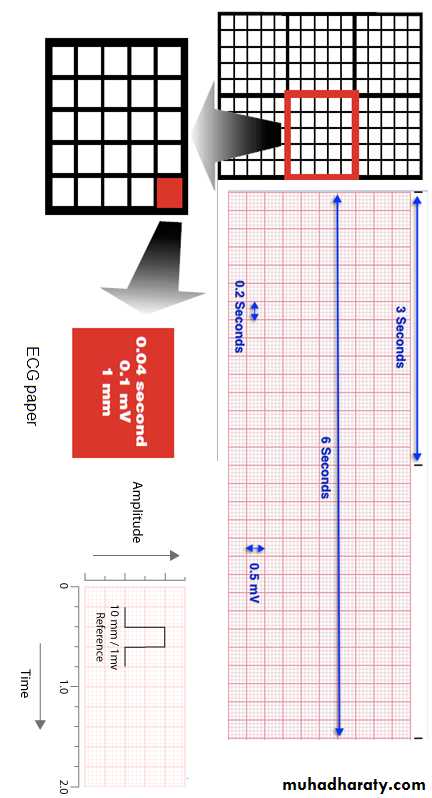
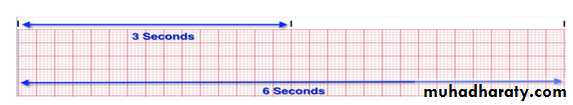
ECG PaperECG paper contain light and dark lines running vertically and horizontally. The light lines circumscribe small squares of 1 X 1 mm; the dark lines delineate large squares of 5 X 5 mm. The horizontal axis measures time. The distance across one small square represents 0.04 seconds. The distance across one large square is five times greater, or 0.2 seconds. The electrocardiogram is recorded on to standard paper travelling at a rate of 25 mm/s.
The vertical axis measures voltage. The distance along one small square represents 0.1 mV, and along one large square, 0.5 mV. The electrocardiogram machines are calibrated so that a signal with an amplitude of 1 mV moves the recording stylus vertically10 mm( 2 large squares).
Figure4: standard ECG calibration.
Normal ECG record
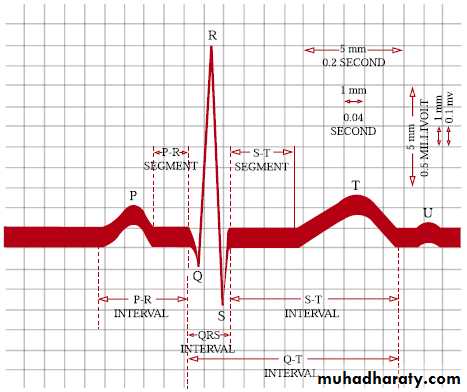
The normal ECG record include a number of waves:
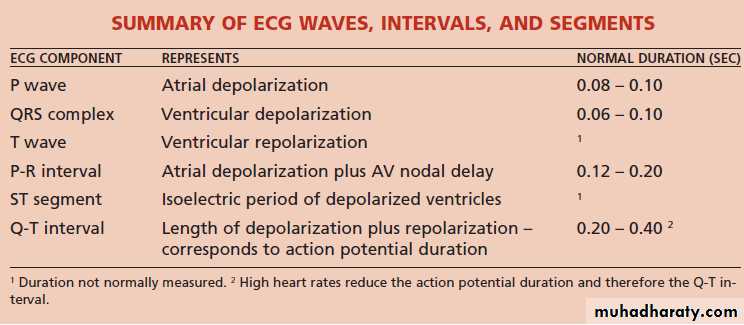
P wave
The P wave represents atrial depolarization. In normal ECGs, the P-wave preceeds the QRS complex. It looks like a small bump upwards from the baseline. The amplitude is normally 0.05 to 0.25mV (0.5 to 2.5 small boxes). Normal duration is 0.06-0.11 seconds (1.5 to 2.75 small boxes). The shape of a P-wave is usually smooth and rounded.
PR interval
The PR interval is the time between the onset of atrial depolarisation and the onset of ventricular depolarization. The normal duration of the PR interval is three to five small squares (0.12-0.20 s).
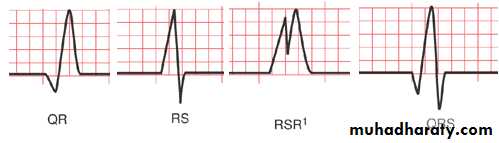
QRS complex
The QRS complex represents the ventricular depolarisation. The duration of the QRS complex should not exceed two and a half small squares (0.10 s).
(Note: Capital letters (Q, R, S) denote large-amplitude deflections (≥5 mm or 0.5 mV), whereas lowercase letters (q, r, s) signify low-amplitude deflections (≤5 mm or 0.5 mV).
Figure5: various morphology of QRS complex
Figure 6:ECG Paper
ST segmentThe ST segment is the line that from the end of the QRS complex to beginning of the T wave. Normally the ST segment is flat, being neither positive or negative relative to the baseline.
T wave
T wave produced by ventricular repolarisation. Tall T waves may be seen in acute myocardial ischaemia and are a feature of hyperkalaemia. The amplitude of T wave is usually less than 2/3 of the amplitude of the corresponding R wave .
QT interval
The QT interval is measured from the beginning of the QRS complex to the end of the T wave and represents the total time taken for depolarisation and repolarisation of the ventricles. As a general guide the QT interval should be 0.35- 0.45 second.
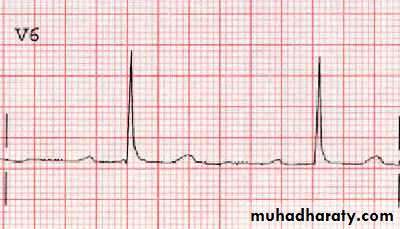
U wave
The U wave is an inconstant finding, believed to be due to slow repolarization of the papillary muscles , it is a small rounded deflection (≤ 1 mm) that follows the T wave. Prominent U waves may be found in athletes and are associated with hypokalaemia and hypercalcaemia or due to drugs (e.g., amiodarone, sotalol, quinidine, procainamide, disopyramide) .
Figure 7: U – wave.
Calculation of Heart rate:
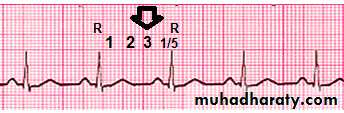
A. When the rhythm is regular(R-R intervals are nearly equal):Heart rate = 300/ number of large squares between two successive R wave.
Or Heart rate = 1500/ number of small squares between two successive R wave.
Example: in the following ECG trace the space between two successive R wave is (3.5) large square so the heart rate will be
Heart rate = 300/3.5
Heart rate = 86 beat/ min.
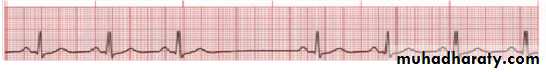
B. When the heart rate is irregular(unequal R-R intervals)
The heart rate calculate by counting the number of R wave (QRS complex) in a 6-sec strip(30 large squares) and multiply by 10.Example: in the following ECG trace there are (7) R wave is (30) large square or (6) second so the heart rate will be
Heart rate = number of R wave (QRS complex) in a 6-sec x 10
Heart rate = 7 x 10 = 70 beat/ min.
Arrhythmias
Cardiac arrhythmias are prevalent among humans across all age ranges and may occur in the setting of underlying heart disease as well as in structurally normal hearts. While arrhythmias are widely varied in their clinical presentations, they possess shared electrophysiologic properties at the cellular level .the main causes of Cardiac arrhythmias are:
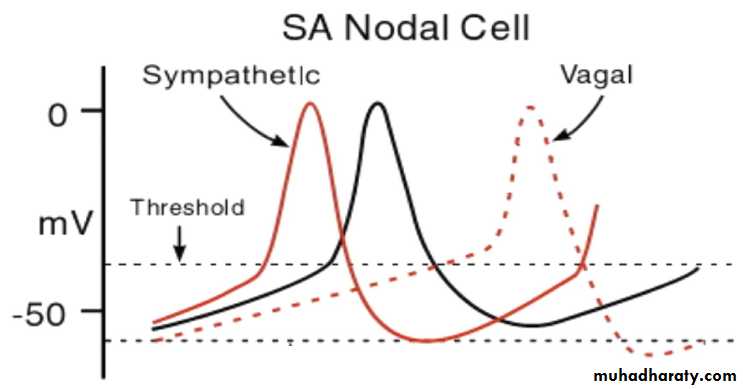
1.Altered Normal Automaticity
It is well known that some specialized heart cells, such as sinoatrial nodal cells, the atrioventricular (AV) node, and the His-Purkinje system, as well as some cells in both atria, possess the property of pacemaker activity or automaticity. Suppression or enhancement of this activity may lead to clinical arrhythmias. Under normal conditions, the sinoatrial nodal cells have the fastest rate of firing and the normal pacemaker. Pacemaker activity is controlled by the autonomic nervous system and can be modulated by a variety of systemic factors, including metabolic abnormalities and endogenous or pharmacologic substances. Parasympathetic activity reduces the discharge rate of the pacemaker cells. Conversely, sympathetic activity increases the sinus rate. Metabolic abnormalities such as hypoxia and hypokalemia can lead to enhanced normal automatic activity as a result of Na/K pump inhibition. Clinical examples: sinus tachycardia associated with exercise, fever, and thyrotoxicosis.
figure 8: effect of autonomic nervous system on SASA node automaticity
2.Abnormal AutomaticityAtrial and ventricular nonpacemaker myocardial cells, which in the normal heart typically do not exhibit spontaneous activity, may exhibit automaticity properties. The intrinsic rate of an automatic abnormal focus depends on the membrane potential; the more positive the membrane potential, the faster the automatic rate. Abnormal automaticity is thought to play a role in cases of elevated extracellular potassium, low intracellular pH, and catecholamine excess. Clinical examples: premature beats, atrial tachycardia, accelerated idioventricular rhythm, ventricular tachycardia (VT).
3.Triggered Activity
Triggered activity (TA) is defined by impulse initiation caused by afterdepolarizations (membrane potential oscillations that occur during or immediately following a preceding AP). Afterdepolarizations occur only in the presence of a previous AP (the trigger), and when they reach the threshold potential, a new AP is generated. This may be the source of a new triggered response, leading to self-sustaining TA.After depolarization.
Are spontaneous depolarization that appears during repolarization (phase3)or shortly after repolarization (phase4):
When small cause small oscillation of membrane potential
When large cause triggered response which are important causes of lethal arrhythmias.
It is of two type
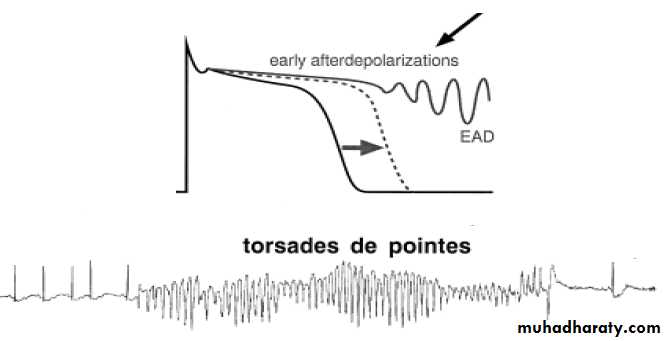
A. Early after depolarization(EAD).
Occurs at the end of (phase2)or early phase 3
it is more likely to occur when the action potential is prolonged which manifests on the surface electrocardiogram (ECG) as QT prolongation.
Mechanism: Some antiarrhythmic agents, such as Class IA antiarrhythmic drugs (quinidine, disopyramide, procainamide), • Class IB antiarrhythmic drugs (flecainide, encainide, indecainide Class III antiarrhythmic drugs (amiodarone, sotalol, bretylium) may become proarrhythmic because of their therapeutic effect of prolonging the AP. Many other drugs can predispose to the formation of EADs, particularly when associated with hypokalemia and/or bradycardia, additional factors that result in prolongation of the AP. Clinical examples include torsades de pointes (“twisting of the tips”), the characteristic polymorphic Ventricular tachycardia seen in patients with long QT syndrome.
Figure 9: . Early after depolarization(EAD).
B.Delayed after depolarization(DAD).Occur at near the very end of repolarization or just after full repolarization(phase4), its usually caused by digitalis toxicity which lead to increase intracellular calcium. Catecholamines can cause DADs by causing intracellular Ca2+ overload. Ischemia-induced DADs are thought to be mediated by the accumulation of lysophosphoglycerides in the ischemic tissue, with subsequent elevation in Na+ and Ca2+. Abnormal sarcoplasmic reticulum function (e.g. mutations in ryanodine receptor) can also lead to intracellular Ca2+ overload.
4.Disorders of Impulse Conduction Block
A. BlockConduction delay and block occurs when the propagating impulse fails to conduct. Many factors can alter the conduction, including rate, autonomic tone, drugs (eg, calcium channel blockers, beta blockers, digitalis, adenosine/adenosine triphosphate), or degenerative processes (by altering the physiology of the tissue and the capacity to conduct impulses).
B. Reentry
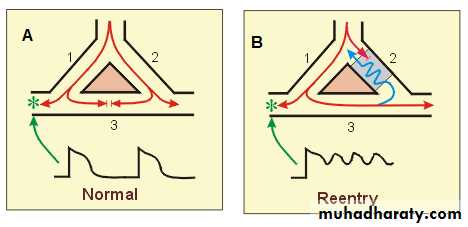
During normal electrical activity, the cardiac cycle begins in the sinoatrial node and continues to propagate until the entire heart is activated. This impulse dies out when all fibers have been depolarized and are completely refractory. However, if a group of isolated fibers is not activated during the initial wave of depolarization, they can recover excitability in time to be depolarized before the impulse dies out. They may then serve as a link to reexcite areas that were previously depolarized but have already recovered from the initial depolarization. Such a process is commonly denoted as reentry, reentrant excitation, circus movement, reciprocal or echo beats. Reentry has been divided in 2 main groups: anatomical or classic reentry, where the circuit is determined by anatomical structures, and functional reentry, which in turn includes different mechanisms. Reentry can take place within a small local region within the heart or it can occur, for example, between the atria and ventricles (global reentry). For reentry to occur, certain conditions must be met that are related to the following:
1.the presence of a unidirectional block within a conducting pathway
2.critical timing
3.the length of the effective refractory period of the normal tissue
A model for reentry
In normal tissue (figure 10. A), if a single Purkinje fiber forms two branches (1 & 2), the action potential will travel down both branches , finally the action potentials that travel into branch 3 will cancel each other out.Reentry (figure 10. B) can occur if branch 2, for example, has a unidirectional block. In such a block, an action potential will travel down the branch 1, into the common distal path (branch 3), and then travel retrograde through the unidirectional block in branch 2 (blue line). When the action potential exits the block(gray area), if it finds the tissue excitable, then the action potential will continue by traveling down (i.e., reenter) the branch 1. If the action potential exits the block in branch 2 and finds the tissue unexcitable (i.e., within its effective refractory period), then the action potential will die. Therefore, both timing and refractory state of the tissue are important for reentry to occur, alterations in timing (related to conduction velocity) and refractoriness (related to effective refractory period) can either precipitate reentry or abolish reentry. For this reason, changes in autonomic nerve function can significantly affect reentry mechanisms, either precipitating or terminating reentry. Many antiarrhythmic drugs alter effective refractory
Figure 10: Re-entry( Circus movements)
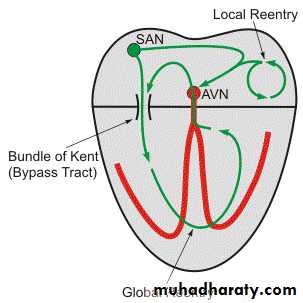
Global ReentryGlobal reentry between the atria and ventricles may involve accessory conduction pathways ("bypass tracts") such as the bundle of Kent. The AV node is normally the only electrical pathway connecting the atria and ventricles. When accessory pathways exist, impulses can travel between the atria and ventricles by multiple pathways. In the example shown to the right, the impulse is traveling through the accessory pathway (bundle of Kent), depolarizing ventricular tissue, then traveling backwards (retrograde) through the AV node to re-excite the atrial tissue and establishing a counter-clockwise global reentry. This type of reentry results in supraventricular tachyarrhythmias (e.g., Wolff-Parkinson-White syndrome, or WPW, found in 0.1% of the population).
figure: Global reentry
Examples of cardiac arrhythmias1.Tachycardia
tachycardia, defined as heart rate faster than 100 beats /min. ECG: is normal except the rate is fast. Causes:
1.increased body temperature.
2.stimulation of the heart by the sympathetic nerves.
2.Bradycardia
bradycardia, defined as heart rate fewer than 60 beats/ min. ECG: is normal except the rate is slow.Causes, Athlete’s heart or Vagal stimulation..3.Sinus arrhythmia
In healthy young individuals, the heart rate accelerates during inspiration and de-celerates during expiration,4.Atrioventricular block
Impairement of impulse conduction from atria to ventricleFirst degree block( Prolonged P-R Interval)
ECG: normal a part from increased P-R interval to greater than 0.20 S.
Second-degree heart block
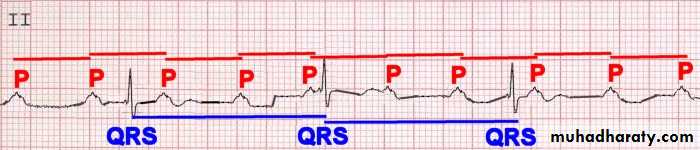
The ECG show a progressive lengthening of the PR interval and finally there is failure of impulse transmission to ventricle(P wave not followed by QRS complex).Complete A-V block (third degree block).
This condition characterized by complete block of the impuls transmission from the atria into the ventricles. The ventricles establish their own pulse rate, usually originating in the A-V node or A-V bundle. ECG: P waves become dissociated from the QRS-T complexes.6.Premature Contractions (extrasystole, ectopic beat)
A premature contraction is a contraction of the heart before the time that normal contraction would have been expected.Premature Atrial beat, this condition due to an abnormal beat originated in an ectopic foci in the atria. It occur frequently in otherwise healthy people, like athletes, or peoples with excess smoking, lack of sleep, ingestion of too much coffee, alcoholism.
ECG: the P wave has a different morphology because the atria activate from an abnormal site, the P-R interval is usually shortened, normal QRS complex, the interval between the premature contraction and the next succeeding contraction is slightly prolonged, which is called a compensatory pause.
Premature Ventricular Contractions(PVCs)
This condition due to an abnormal beat originated in an ectopic foci in the ventricle. PVCs may occur in ratio of one normal sinus beat to one PVC, the rhythm is called bigeminy. Trigeminy refers to two normal sinus beats for every one PVC, and so on. Isolated PVCs are common in normal hearts and they can result from factors as cigarettes, coffee, lack of sleep, various mild toxic states, and emotional irritability, and rarely require treatment. On the other hand, certain situations have been identified in which PVCs appear to pose an increased risk for triggering ventricular tachycardia, ventricular fibrillation, and death.
ECG: the ECG record of PVC characterized by
the QRS complex is usually considerably Prolonged.the QRS complex has a high voltage .
the T wave has polarity exactly opposite to that of the QRS complex.
7.Atrial Fibrillation
In atrial fibrillation, the atria beat very rapidly (300-500/min) in a completely irregular and disorganized fashion. The ventricles beat at a completely irregular rate, usually 80-160/min.The QRS-T complexes are usually normal.
Figure: atrial fibrillation.
8.Ventricular FibrillationVentricular fibrillation is a condition in which there is uncoordinated, totally irregular and ineffective contraction of the muscle of the ventricles. The fibrillating ventricles cannot pump blood effectively, and circulation of the blood stops. Therefore, in the absence of emergency treatment, ventricular fibrillation that lasts more than a few minutes is fatal. The most frequent cause of ventricular fibrillation is myocardial infarction , sudden electrical shock of the heart.
Figure: ventricular fibrillation.
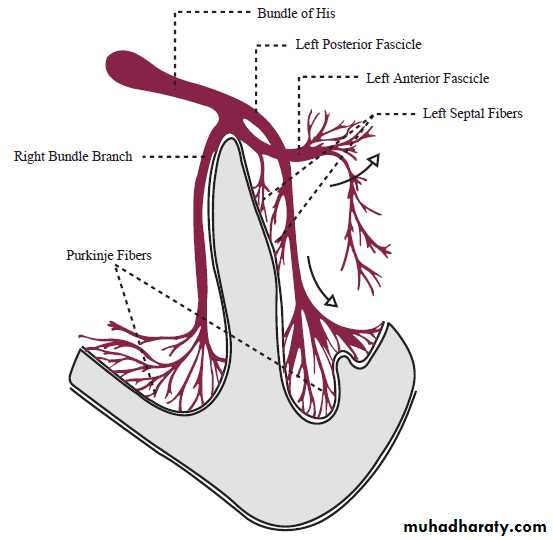
Bundle branch blockAfter leaving the AV node, electrical activity passes through the bundle of His. The conduction system then divides distally: the right ventricle is supplied by the right bundle branch, and the left ventricle is supplied by branches from the left bundle. A bundle branch block is an ECG abnormality resulting from failure to conduct in either the right bundle branch or the main division of the left bundle branch. A hemi-block is an ECG pattern which is associated with failure to conduct through one of the two fascicles of the left bundle branch.