
BENIGN PROSTATIC HYPERPLASIA
BPH
BPH
Dr. AMMAR FADIL

•
BPH is the most common benign disease in older
men
•
Is a common cause of lower urinary tract symptoms
(LUTS)-
(prostatism)
in men
•
Occurs in men over 50 years of age;
•
Occurs in men over 50 years of age;
•
The principle cause of BOO in men is BPH
•
Less common causes are urethral stricture &
malignant enlargement of the prostate.
2

•
Histologic changes of prostatic enlargement
are evident in 50% of men by the age of 60 y,
Although not all patients have “luts”
•
Prostate size : 20g (4.4x3.4x2.6cm (wxlxA-P)
•
Prostatic functions:
–
sperm nutrition
–
seminal anticoagulation
3
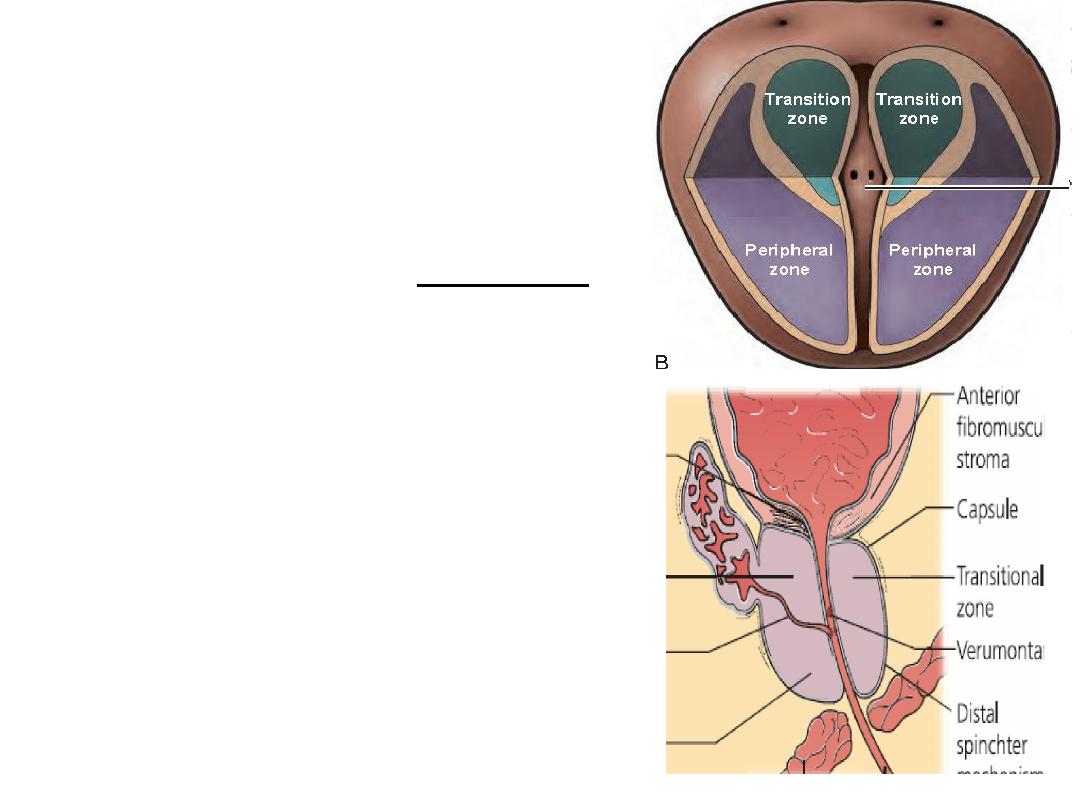
PROSTATE ZONES
•
Transitional zone,
surrounds upper urethra,
sphincter 5% of prostate
glandular elements, site of BPH
•
Peripheral zone,
70% of prostate glandular
70% of prostate glandular
elements, site of prostatic CA
•
Central zone
25% of prostate glandular
elements; surrounds ejaculatory
ducts
4
•
Another prostate
classification is
often referred to the “3
lobes” of the prostate,
namely, the median and
the 2 lateral lobes
5
Etiology
•
BPH is believed due to a
–
Hormonal imbalance :
Serum testosterone levels slowly but
significantly decrease with advancing age;
however, levels of oestrogenic steroids are
however, levels of oestrogenic steroids are
not decreased equally. According to this
theory, the prostate enlargement because of
increased estrogenic effects
–
aging
6

pathology
•
BPH is characterized by an increased number of epithelial
& stromal cells in the periurethral area of the prostate
and thus correctly referred to as hyperplasia and not
hypertrophy
The main hormone acting on the prostate is
Testosterone, which is secreted by the Leydig cells of the testes
Testosterone, which is secreted by the Leydig cells of the testes
•
Testosterone is converted to DHT by the enzyme 5a-reductase
, which is found in high concentration in prostate.
•
DHT has five times the potency of testosterone
•
Castration results in the regression of established BPH and
improvement in urinary symptoms.
7
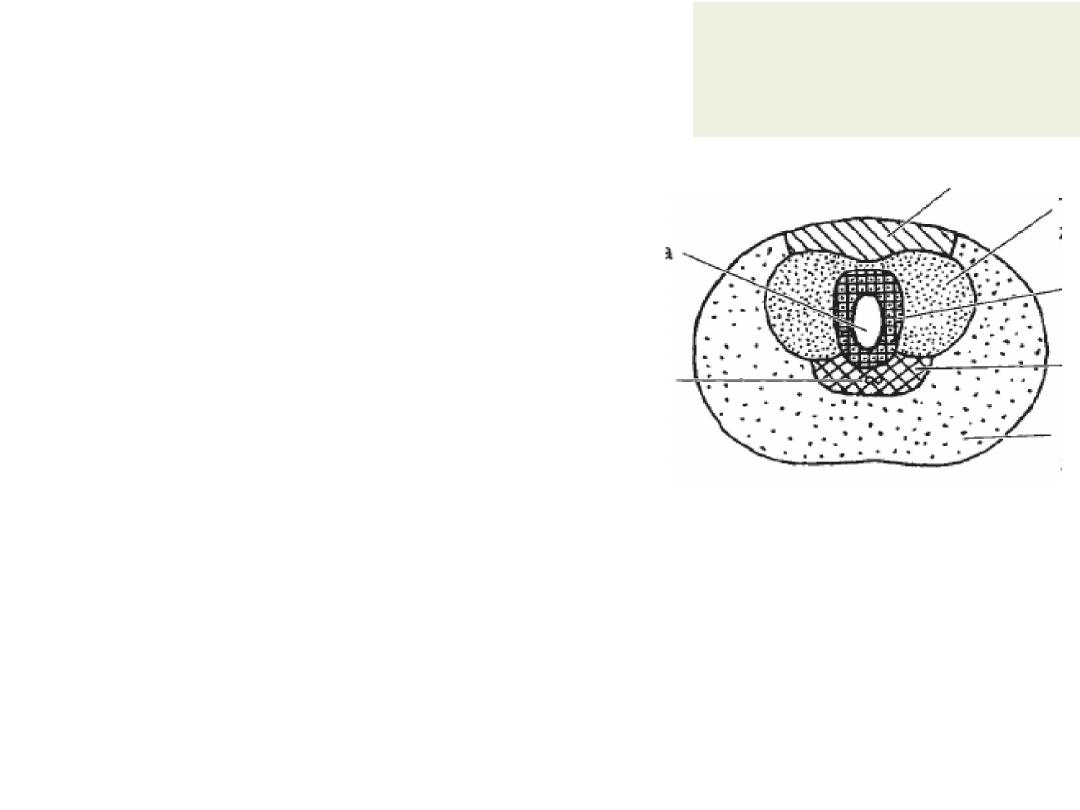
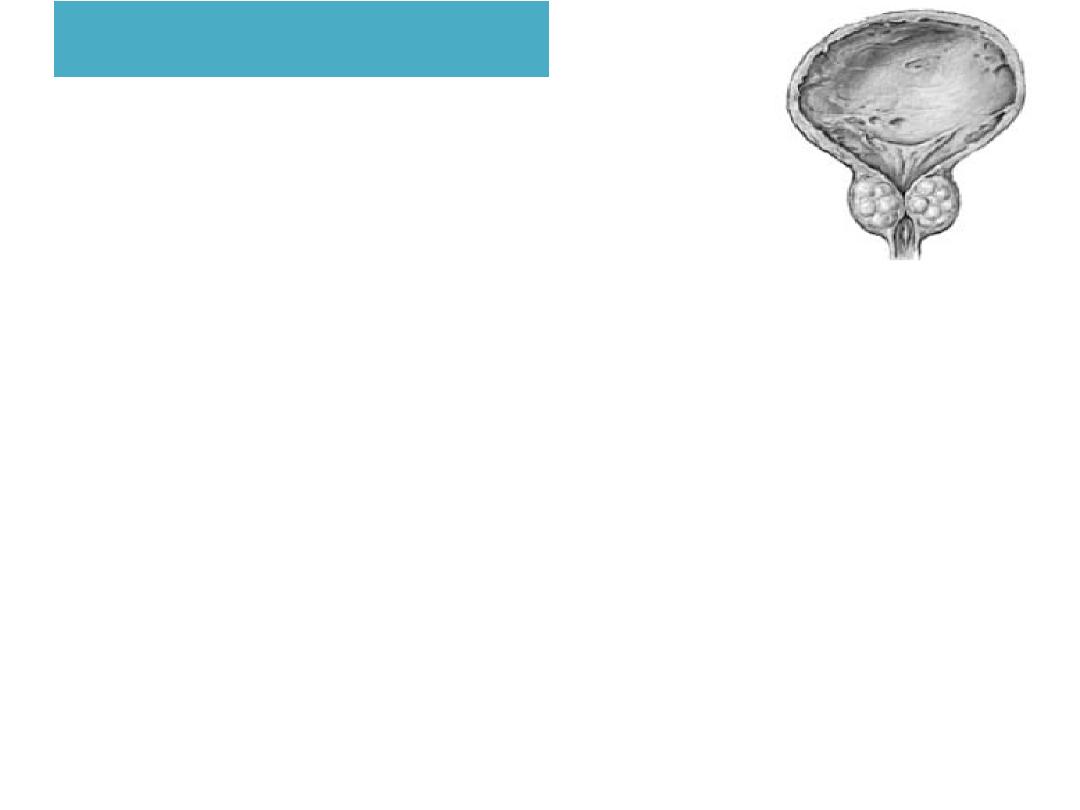
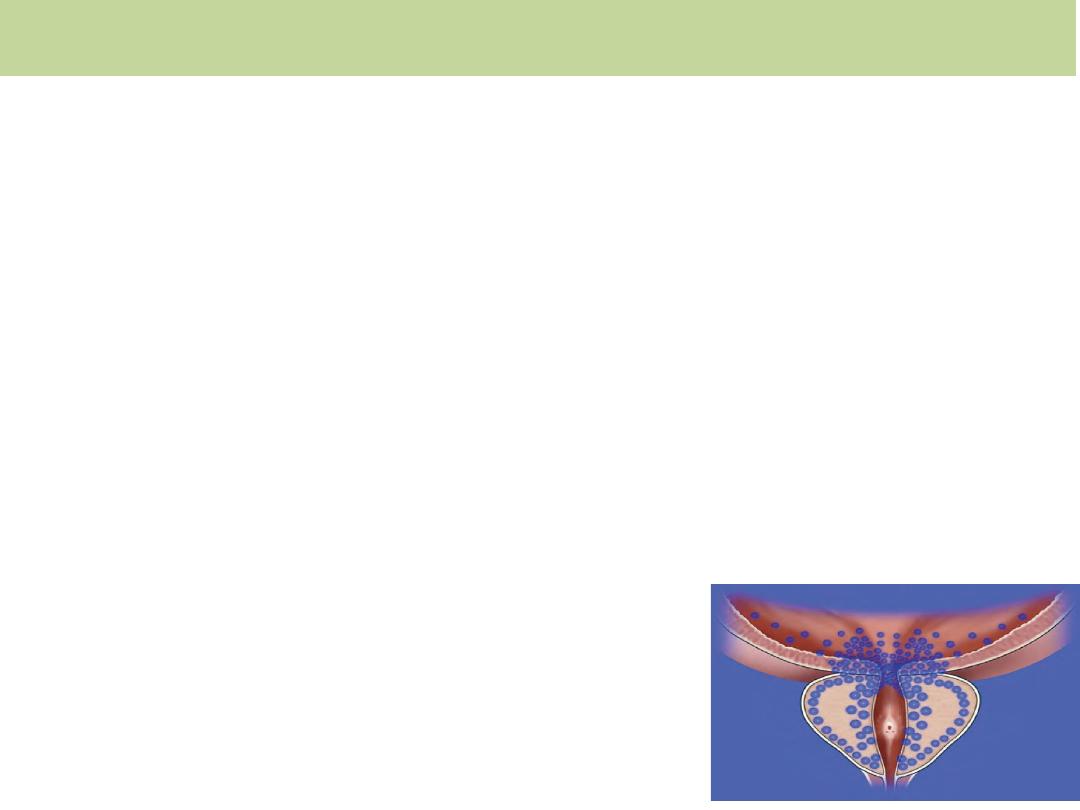
Pathology
As BPH nodules in the transition
zone enlarge, they compress the
outer zones of the prostate,
resulting in the formation of a
so-called surgical capsule.
•
This boundary separates the transition zone from the peripheral zone and
•
This boundary separates the transition zone from the peripheral zone and
serves as a cleavage plane for open enucleation of the prostate during open
simple prostatectomies
8
Pathophysiology
•
can be subdivided into
the static & the dynamic component
static component
mediated by the volume effect of
mediated by the volume effect of
BPH. intrusion into the urethral lumen leading to a
(bladder outlet obstruction) BOO
9
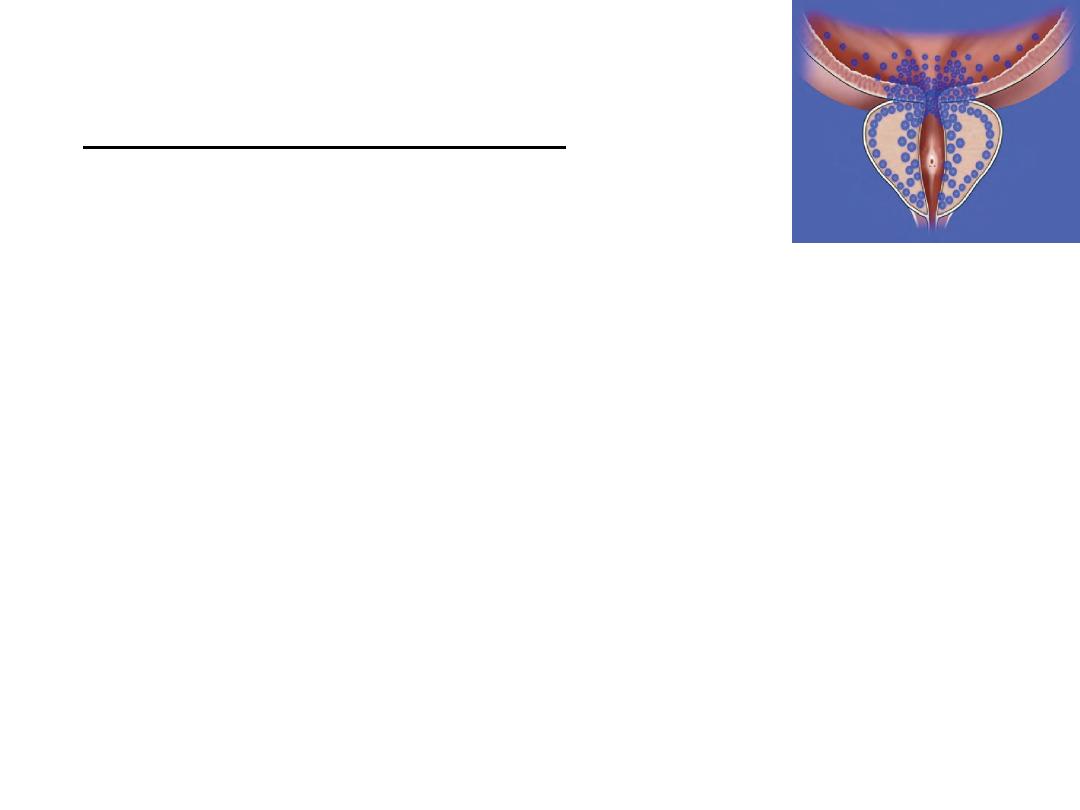
The dynamic component
•
A1-adrenoceptor-mediated prostatic
smooth muscle contraction.
•
Smooth muscle accounts for 40% of the
•
Smooth muscle accounts for 40% of the
hyperplastic prostate.
•
This effect is the rationale for A-
adrenoceptor blocker treatment for
symptomatic BPH.
10
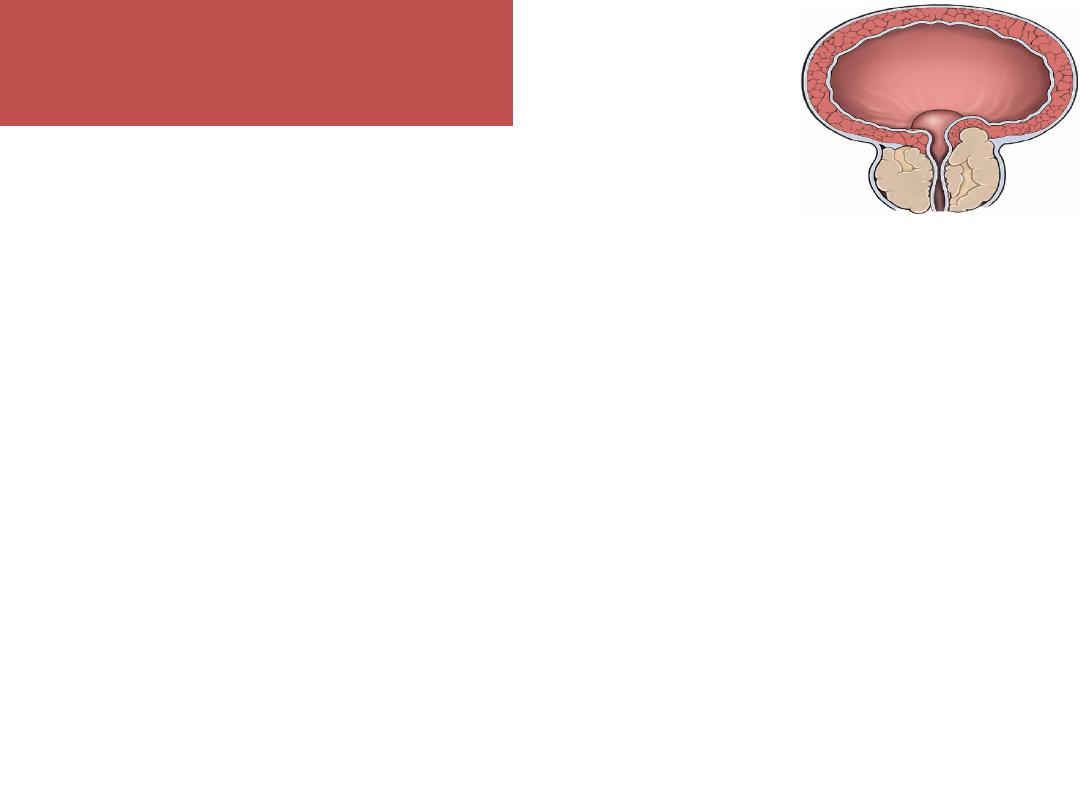
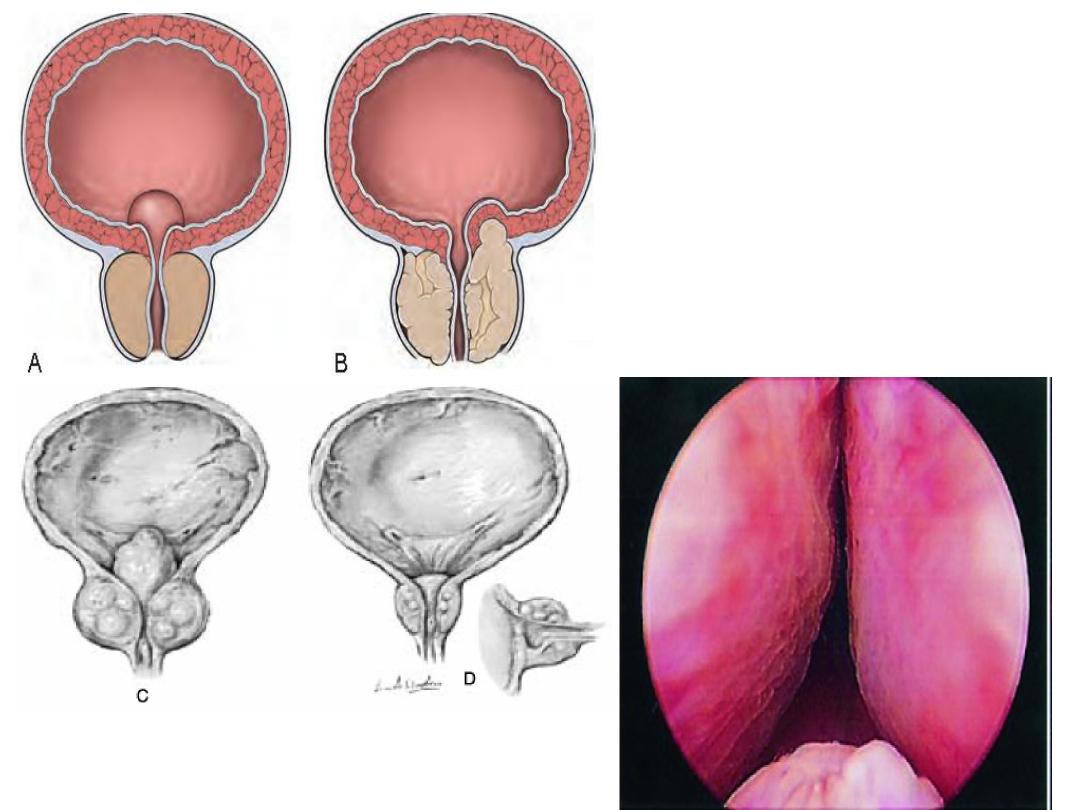
Effects of BPH ON
Bladder.
•
BOO causes thickening of the wall of the bladder, the
musculature of the bladder hypertrophies to overcome
the obstruction and appears trabeculated (cystoscopy).
If left untreated, mucosal herniation between detrusor
If left untreated, mucosal herniation between detrusor
muscle bundles ensues, causing diverticula formation
•
Significant BPH is associated with increased blood flow,
and the resultant veins at the base of the bladder are
liable to rupture to cause haematuria
11
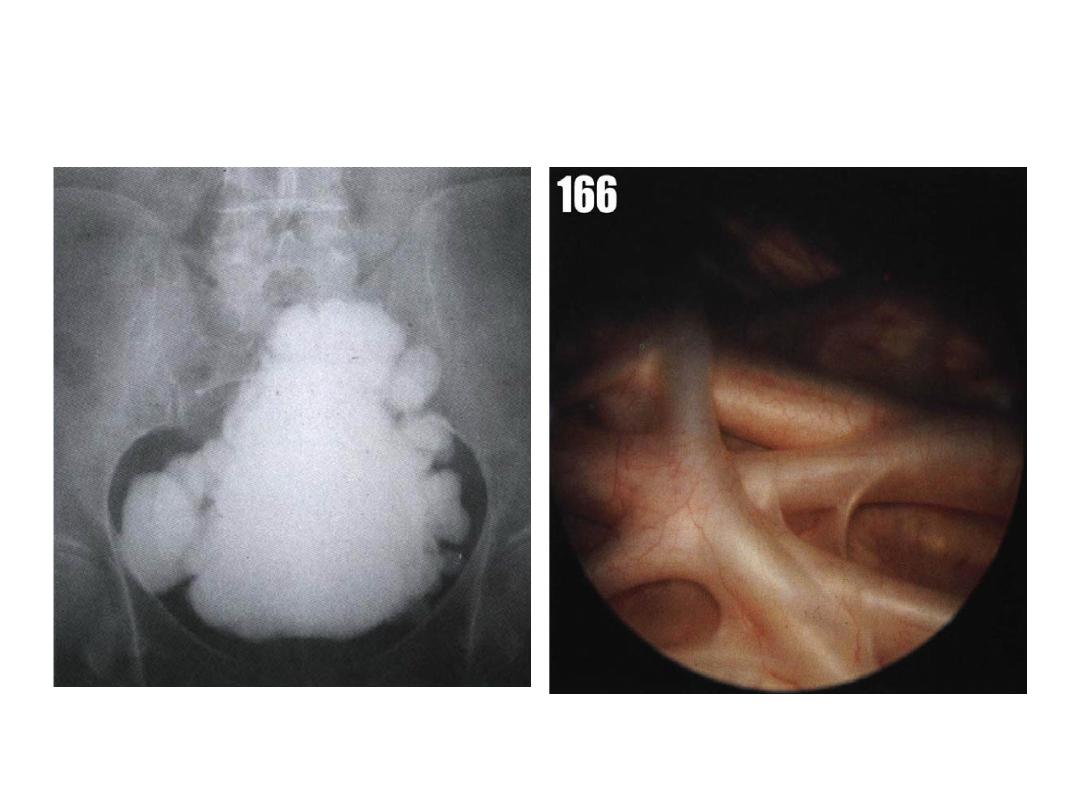
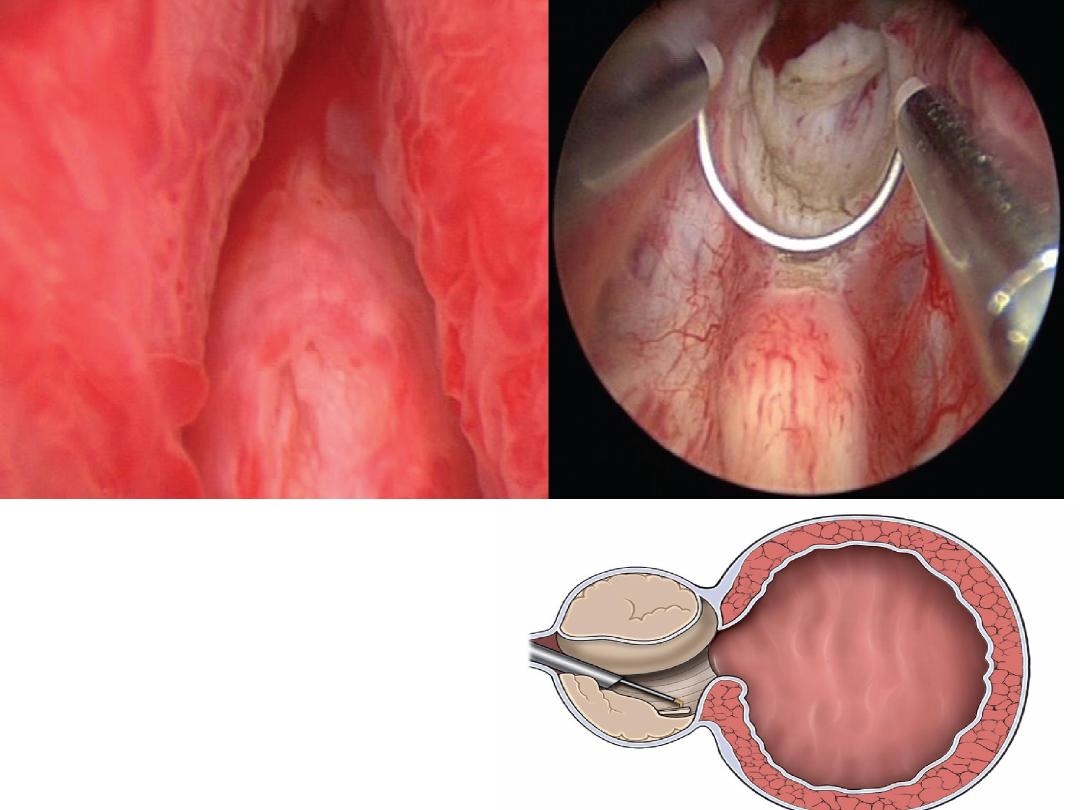
Cystogram
cystoscopy
12
Presentation and Symptoms
1
.
No symptoms (silent prostate)
2.Lower urinary tract symptoms (LUTS)
3. Urine retention acute or chronic
4. Hematuria
4. Hematuria
5. UTI
6. vesical stone
7. bilateral hydronephrosis and renal failure
13
Lower urinary tract symptoms LUTS
• storage
– frequency;
– nocturia;
– urgency (urge incontinence)
• voiding
• voiding
– hesitancy
– poor flow
– intermittent stream – stops and starts;
– terminal dribbling
– sensation of incomplete bladder emptying;
14

AUR\ Precipitating factors
o
Drugs
anticholinergics e.g……
sympathomimetic agents such as ephedrine
(nasal
decongestants)
diuretics
.
o
Intercurrent surgery
o
Intercurrent surgery
o
Intercurrent illness MI
o
Postponement of urination
o
Cold weather
15
Presentation and Symptoms
•
The severity of urinary symptoms do not
correlate with prostate size.
Small prostates can cause severe symptoms.
Small prostates can cause severe symptoms.
Large prostates can be asymptomatic
16

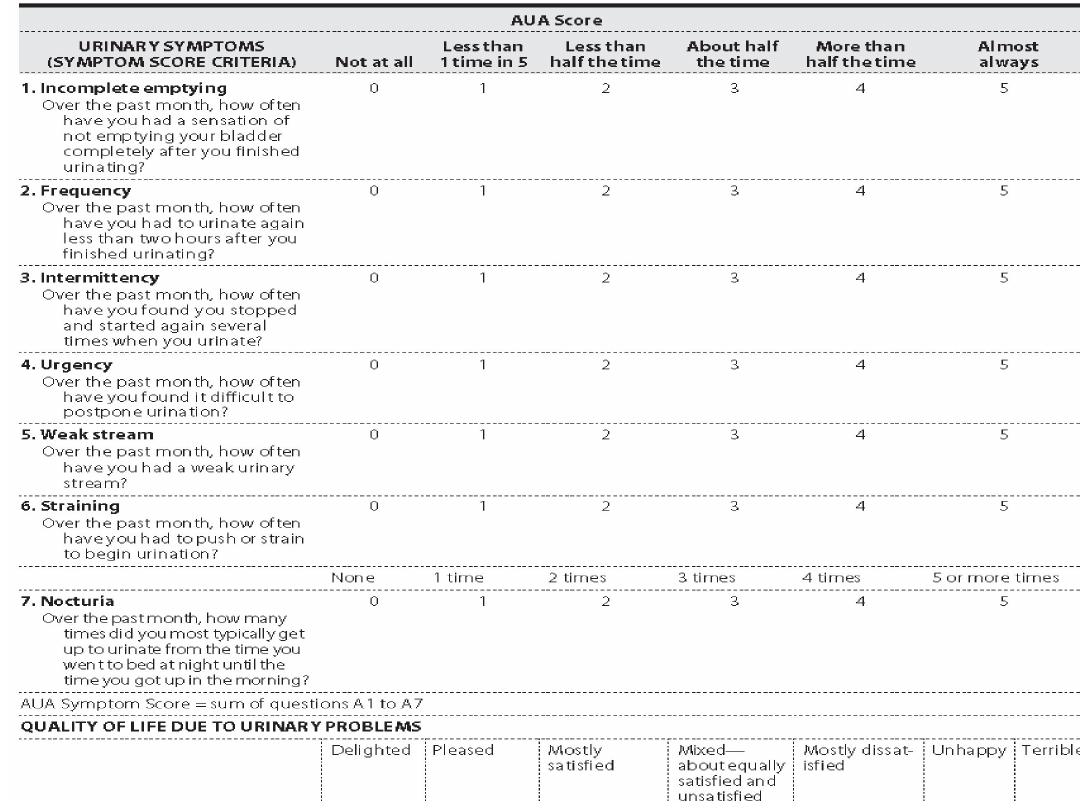
Assessment of Symptoms
International Prostate Symptom Score (IPSS) The AUA
Symptom Score questionnaire is perhaps the single
most
important tool used in the evaluation of patients with BPH
and is recommended for all patients before the initiation of
therapy.
We ask patients to quantify the severity of their complaints on
We ask patients to quantify the severity of their complaints on
a scale of 0–5. Thus, the score can range from 0 to 35.
A symptom score of 0–7 is mild,
8–19 is moderate ,&
20–35 is severe
The IPSS assessment should include an assessment of quality of life, which is a
reflection of the degree of ‘bother’ caused by a patient’s symptoms
17
18

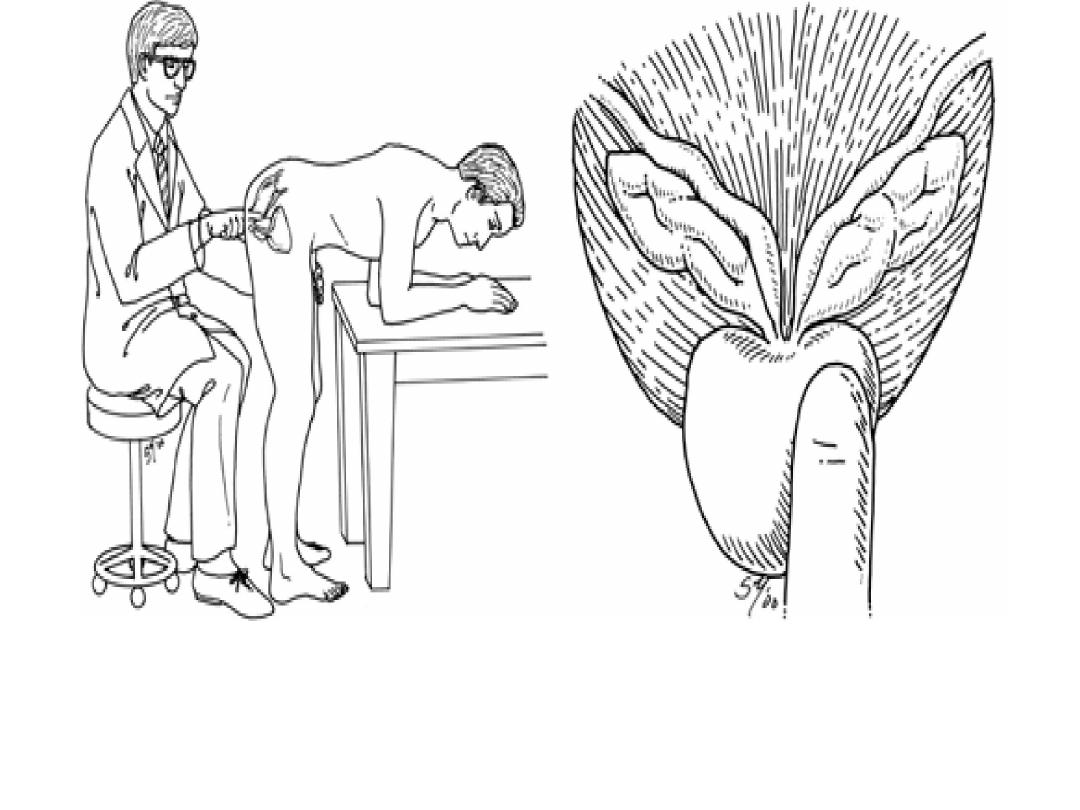
Sign
DRE, & focused neurologic examination are
performed on all patients.
DRE:
The size & consistency of the prostate & to assess
The size & consistency of the prostate & to assess
anal tone, faecal impaction.
BPH usually is a smooth, firm, elastic enlargement
of the prostate
CA stony hard
19
20

Investigations of men with BPH\LUTS
Essential investigations
1.A urinalysis to exclude infection or hematuria
2. Renal function
S. Creatinine & B. urea
(renal insufficiency may be observed in 10% of BPH)
(renal insufficiency may be observed in 10% of BPH)
3. Prostatic specific antigen (PSA)
4. Ultrasound assess prostatic size, PVR, UUT
5. Urinary flow rate (flowmetry)
ADDITIONAL TESTS
–
urodynamic study are reserved for patients with
suspected neurologic disease
21
Flowmetry
Flowmetry
•The simplest & most useful test in
the assessment LUTS
• Normal Q max 20-25ml/s in men
•
voided volume > 150 ml
•The simplest & most useful test in
the assessment LUTS
• Normal Q max 20-25ml/s in men
•
voided volume > 150 ml
< 10 ml \ s indicate obstruction
< 10 ml \ s indicate obstruction
22
Differential Diagnosis
•
urethral stricture,
•
CaP (may be detected by abnormalities on
the DRE or an elevated PSA)
•
neurologic disease, stroke, diabetes mellitus
neurologic disease, stroke, diabetes mellitus
23

Complications
•
UTI
•
Urine retention
•
Vesical stones,
•
Hematuria ,
•
urinary incontinence,
•
upper urinary tract deterioration with renal
insufficiency
24

Modality of therapy
1. watchful waiting
2. Pharmacological therapy
alpha blocker
5 alpha reductase inhibitor
combination therapy
combination therapy
5 PDI
3.Phytotherapy
4. Surgery
5. Minimal invasive therapy
25

1.Conservative treatment
Watchful waiting
Is suitable for LUTS cause little or no bother.
It includes education, re-assurance
•
decreasing total fluid intake especially before
•
decreasing total fluid intake especially before
bedtime
•
periodic monitoring.
26
2. Pharmacological management
1. α-ADRENERGIC BLOCKERS
The α receptors are most abundant in the fibromuscular
stroma of the bladder neck and prostatic urethra.
α blocking agents inhibit the contraction of smooth muscle
that is found in the prostate. causes an improvement in flow
rates and symptom scores
rates and symptom scores
•
SE:
dizziness , orthostatic hypotension & retrograde
ejaculation
27

2. 5α –reductase inhibitors
–
which inhibit the conversion of testosterone to
DHT, the most active form of androgen in prostate.
–
causes a reduction in prostatic volume up to 20 %
over 6 months.
–
It is only appropriate in larger prostates (>30g)
–
It is only appropriate in larger prostates (>30g)
•
SE:
sexual problems (e.g., loss of libido)
•
Both groups of drugs are effective; however, α-
blockers work more quickly
28

Alpha-blockers
–
Doxazosin
–
Alfuzosin 10 mg daily
–
Tamsulosin 0.4 or 0.8
mg daily
5-alpha-reductase
inhibitors
–
Finasteride 5 mg
–
Dutasteride 0.5 mg
mg daily
–
Recently silodosin
29

3. Combination therapy
Combination alpha-blocker and 5-alpha-
reductase inhibitor therapy
30

4. Tadalafil 5 mg
once daily 5mg.
is the only Type 5 Phosphodiesterase (PDE5)
inhibitor that is FDA approved for the treatment
of BPH related voiding symptoms.
5. Muscarinic receptor antagonist
LUTS who have mainly bladder storage
symptoms.
31

3.Phytotherapy
These agents are derived from plants
African plum (Pygeum africanum) &
saw palmetto
32

surgical indications
•
Recurrent or refractory retention (failing at least one
attempt at catheter removal) or any of the following
clearly related to BPH
severe symptoms not responding to medical therapy
• Bladder stones
• Bladder stones
• Recurrent UTIs
•
Recurrent gross hematuria
• diltation of the upper urinary tract due to BOO, w or
wo renal insufficiency
33

Counselling men undergoing prostatectomy
1. Retrograde ejaculation
This occurs in about 65% of men after
prostatectomy.
2. Erectile dysfunction
2. Erectile dysfunction
This occurs in about 5% of men
34

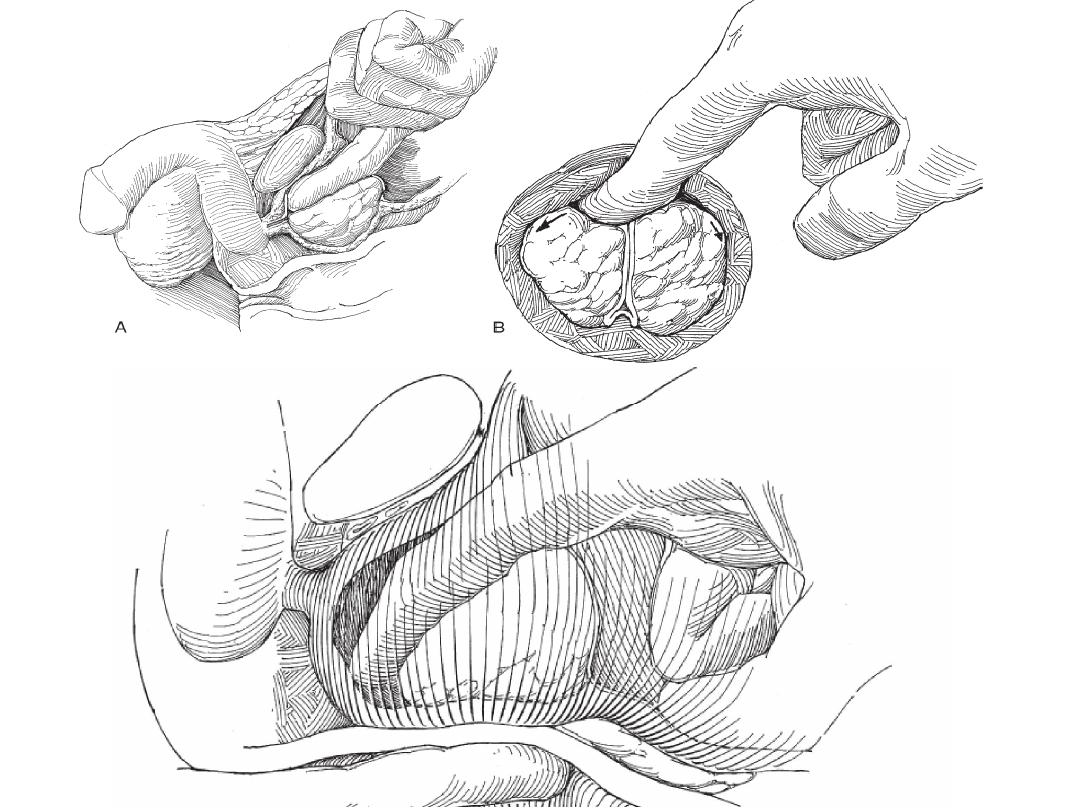
Operative treatment
1.TURP Transurethral resection of the prostate
TURP is most suitable for prostates < 80 cc
.
2. Open prostatectomy
–
Transvesical prostatectomy
–
Retropubic prostatectomy (Millin)
–
Retropubic prostatectomy (Millin)
•
When the prostate is too large to be removed
endoscopically, an open enucleation is necessary.
Prostate glands > 80 g
•
Open prostatectomy may also be initiated when
concomitant bladder stone is present
35
36
37

LASER
Therapy
Laser
Vaporization
Enucleation
Laser Advantages
(1) minimal blood loss
(1) minimal blood loss
(2) ability to treat patients receiving anticoagulation therapy
Disadvantages
(1) lack of availability of tissue for pathologic Examination
(2) more irritative voiding complaints &
(3) High cost
38
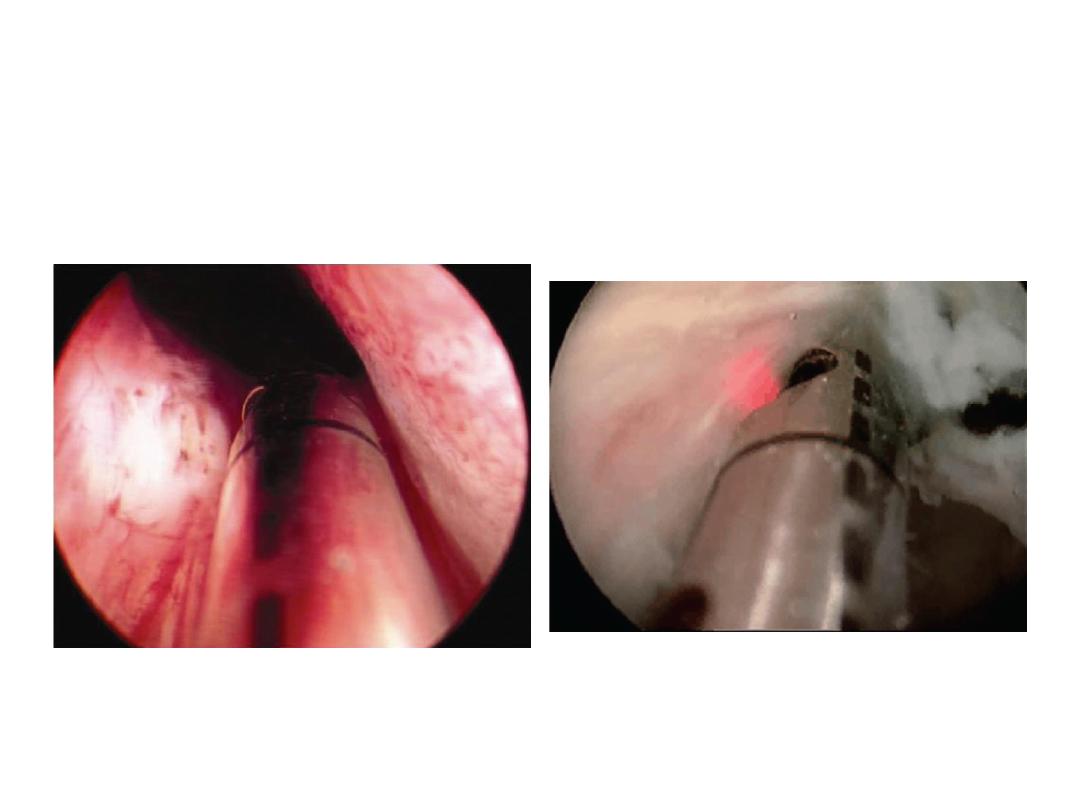
LASER
39
