
Topographic &Applied anatomy
of the anterior abdominal wall
&surgical incisions
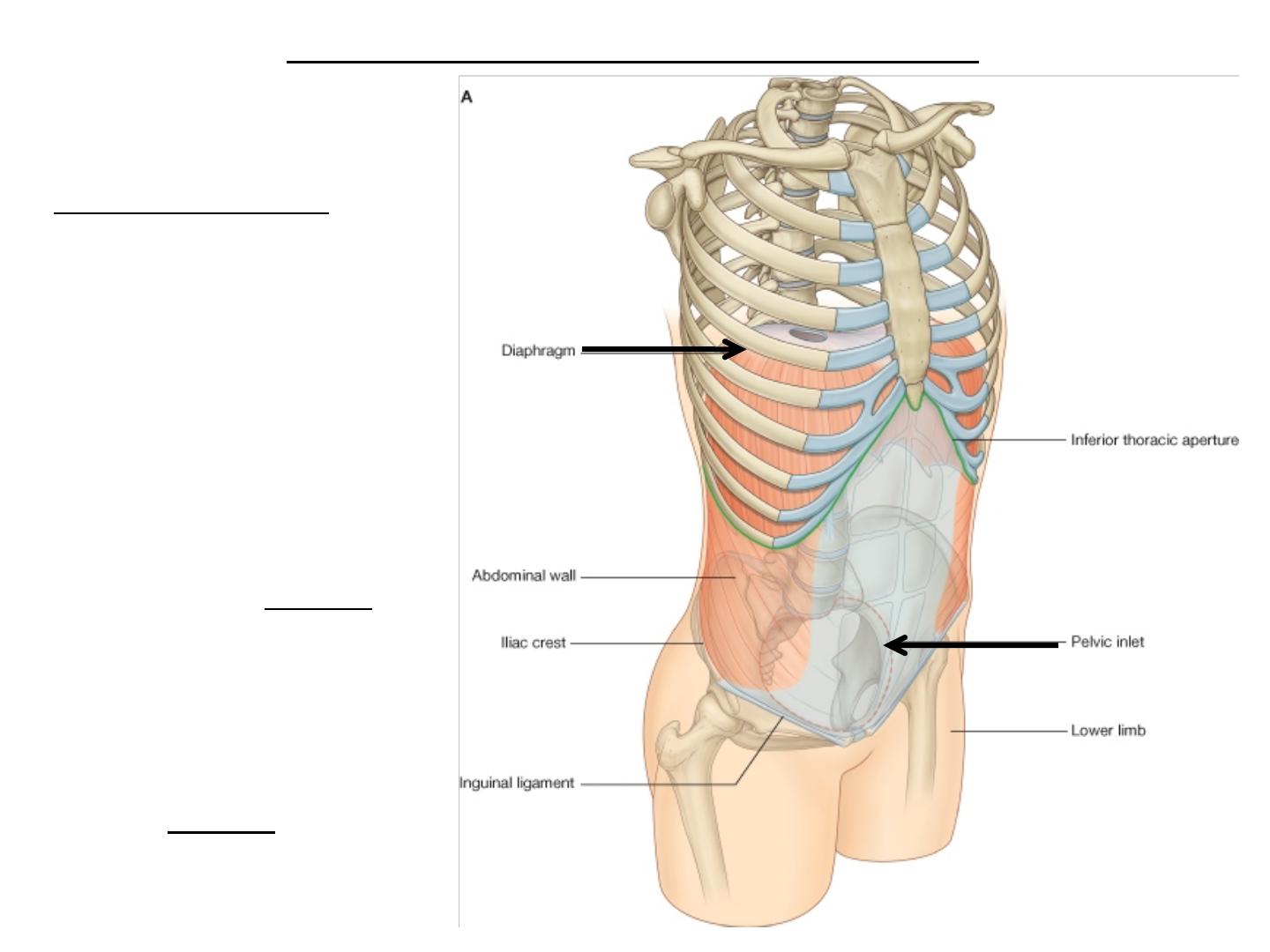
Basic Anatomy
The abdomen is
the region of the
trunk that lies
between the
diaphragm above
and
the inlet of the
pelvis below.
● Extent of the abdominal cavity
The cavity is
larger than the
wall so it extend
up
to the
thoracic cavity
and
down
to the
pelvis
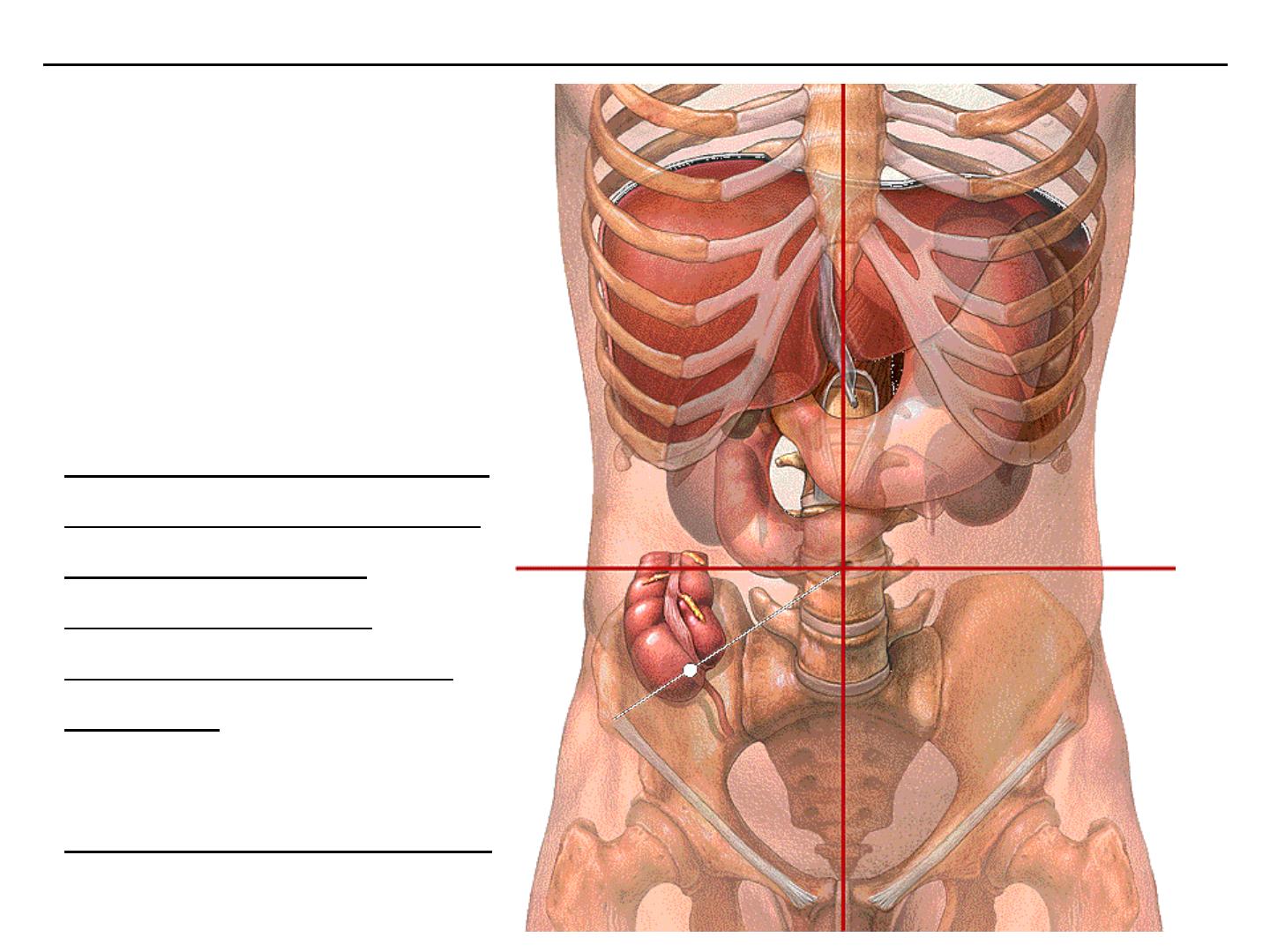
● Topography of the anterior abdominal wall; Planes and regions
Four-quadrant pattern
For the simple four-
quadrant topographical
pattern a
horizontal transumbilical
plane passes through the
umbilicus and the
intervertebral disc
between vertebrae LIII
and LIV,
intersects with
the vertical median plane
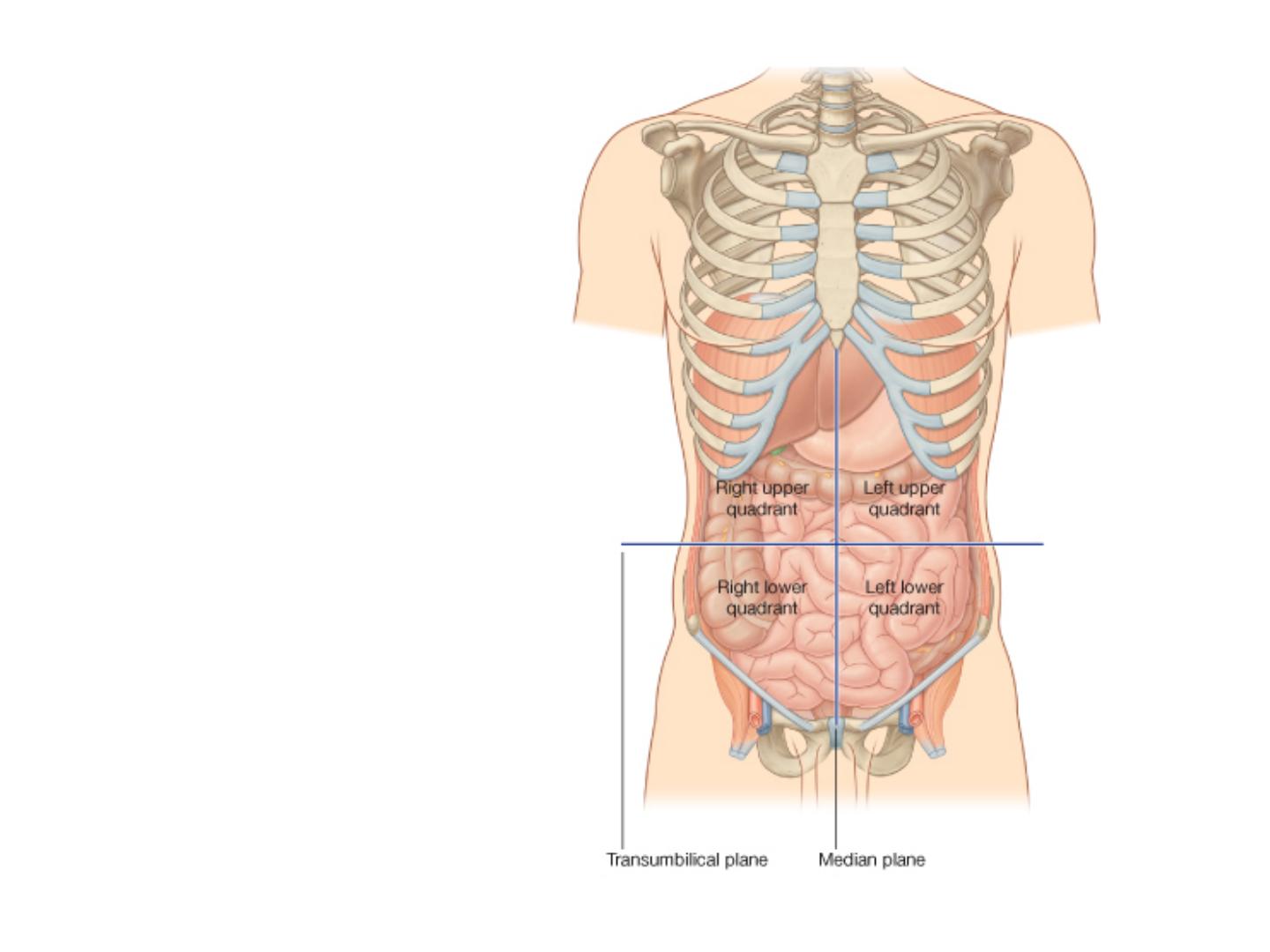
Four-quadrant pattern
to form four quadrants-
the
right upper
,
left
upper
,
right lower
, and
left
lower
quadrants.
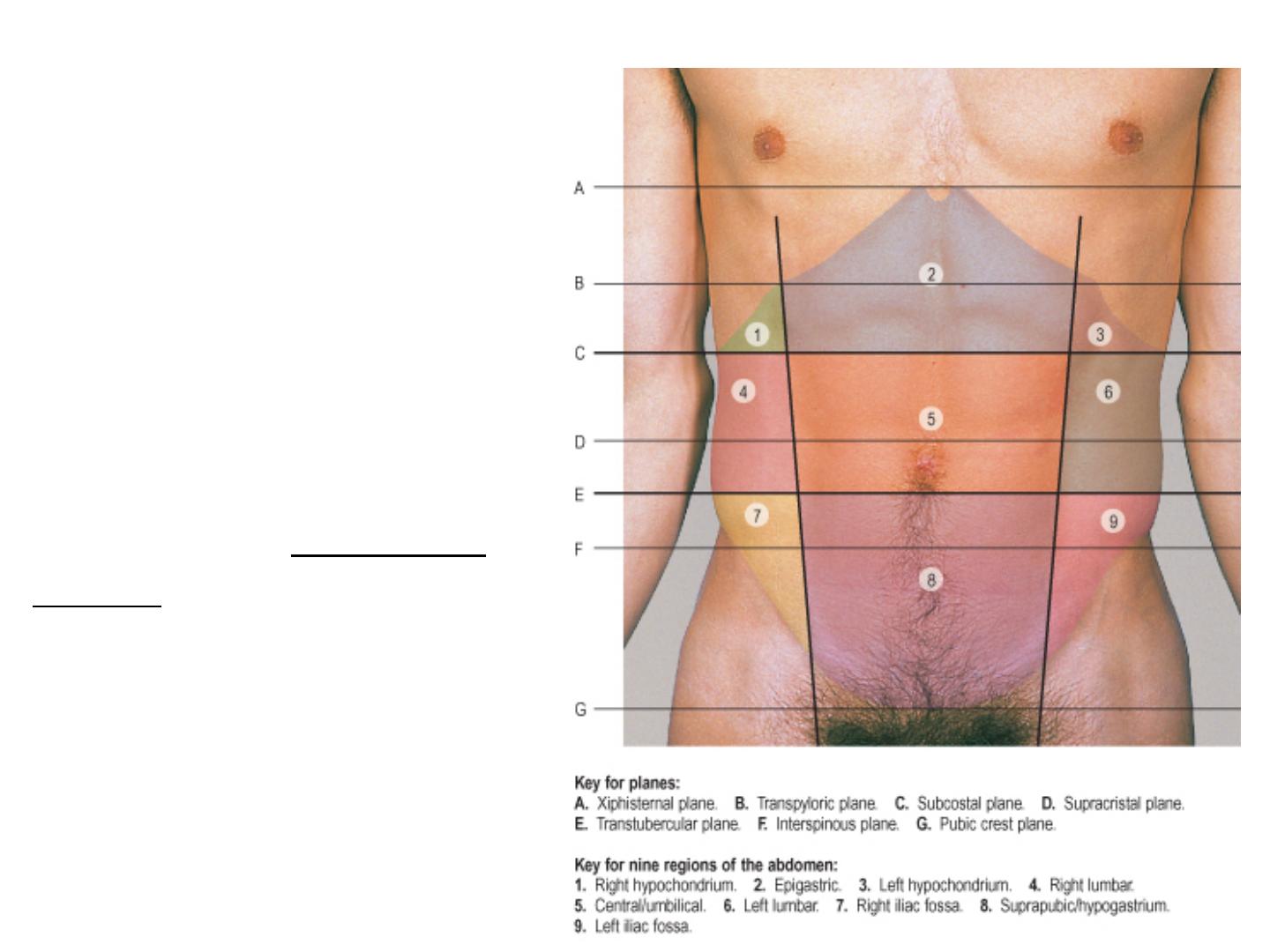
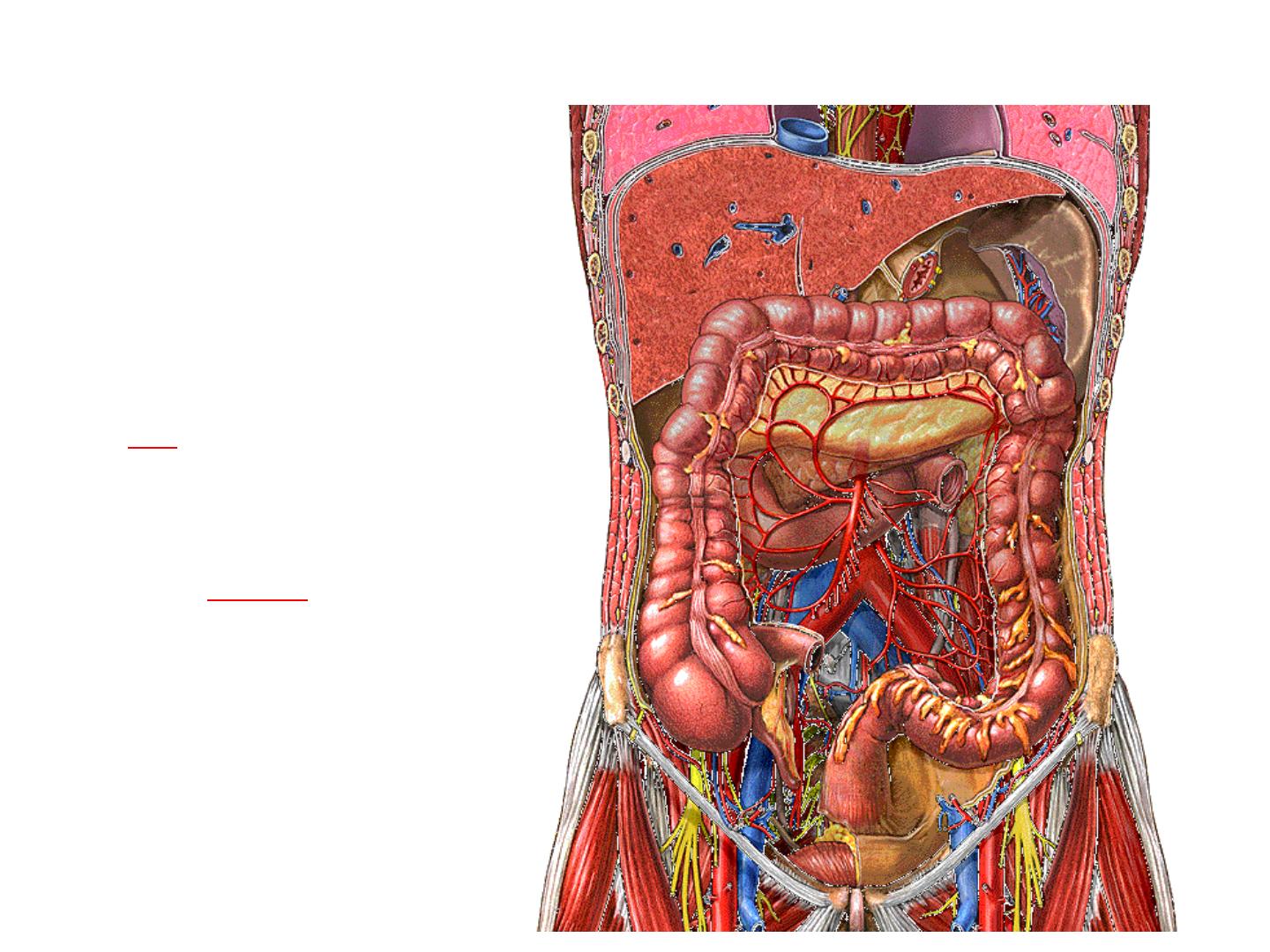
ABDOMINAL PLANES AND
REGIONS
The abdomen can be
divided by a number of
imaginary horizontal and
vertical lines drawn
using the skeletal
landmarks of the thorax
and abdomen. These
lines can be used to
define certain abdominal
'planes'. These planes are
of value in defining
approximate vertebral
levels and the positions of
some relatively fixed
intra-abdominal
structures.
VERTICAL PLANES
In addition to the midline,
which passes through the
xiphisternal process and the
pubic symphysis,
there are two paramedian
planes which are projected from
the midclavicular line. This line
passes through the midpoint of
the clavicle, crosses the costal
margin just lateral to the tip of
the ninth costal cartilage, and
passes through a point mid way
between the anterior superior
iliac spine and the symphysis
pubis.
HORIZONTAL PLANES
The xiphisternal plane
runs horizontally through the
xiphoid processes at the level of
the ninth thoracic vertebra.
The transpyloric plane
lies midway between the
suprasternal notch of the
manubrium and the upper border
of the pubic symphysis. It usually
lies at the level of the body of the
first lumbar vertebra near its lower
border and meets the costal
margins at the tips of the ninth
costal cartilages.
The linea semilunaris crosses
the costal margin on the
transpyloric plane.
The hilum of both kidneys,
the origin of the superior
mesenteric artery, the
termination of the spinal
cord, the neck, adjacent body
and head of the pancreas,
and the confluence of the
superior mesenteric and
splenic veins as they form the
hepatic portal vein may all lie
in this plane.
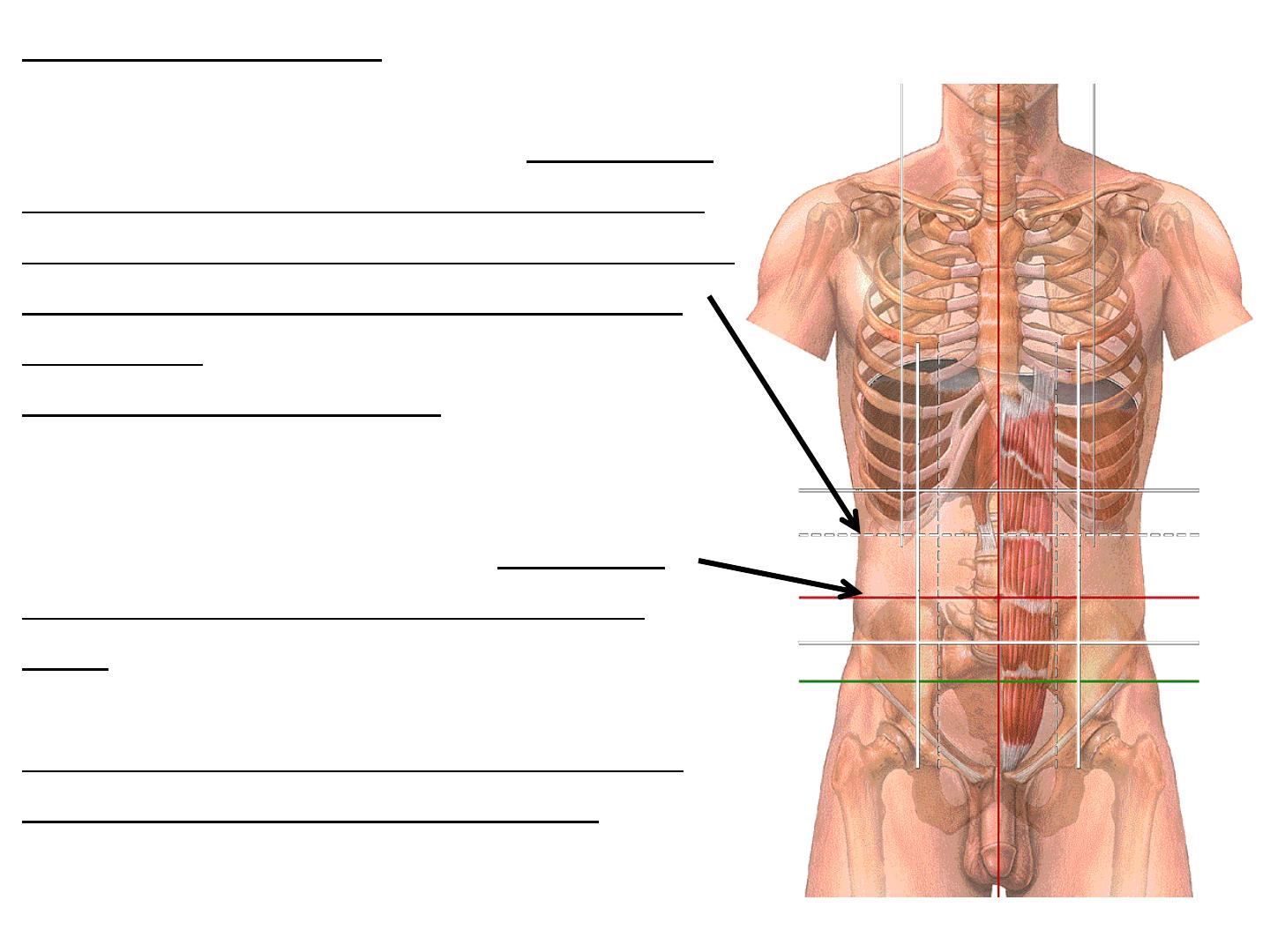
The subcostal plane
is a line joining the lowest point of the
costal margins. It usually lies at the level
of the body of the third lumbar vertebra,
the origin of the inferior mesenteric artery
from the aorta, and the third part of the
duodenum.
The supracristal plane joins the highest
point of the iliac crest on each side. It
usually lies at the level of the body of the
fourth lumbar vertebra, and marks the
level of bifurcation of the abdominal
aorta.
On the posterior abdominal surface, is
used to perform lumbar puncture at the
L4-5 or L5-S1 intervertebral level, which
is safely below the termination of the
spinal cord.
The transtubercular plane
joins the tubercles of the iliac crests
and usually lies at the level of the
body of the fifth lumbar vertebra
near its upper border. It indicates, or
is just above, the confluence of the
common iliac veins and marks the
origin of the inferior vena cava.
The interspinous plane
joins the centres of the anterior
superior spines of the iliac crests. It
passes through either the
lumbosacral disc, or the sacral
promontory, or just below them,
depending on the degree of lumbar
lordosis, sacral inclination and
curvature.
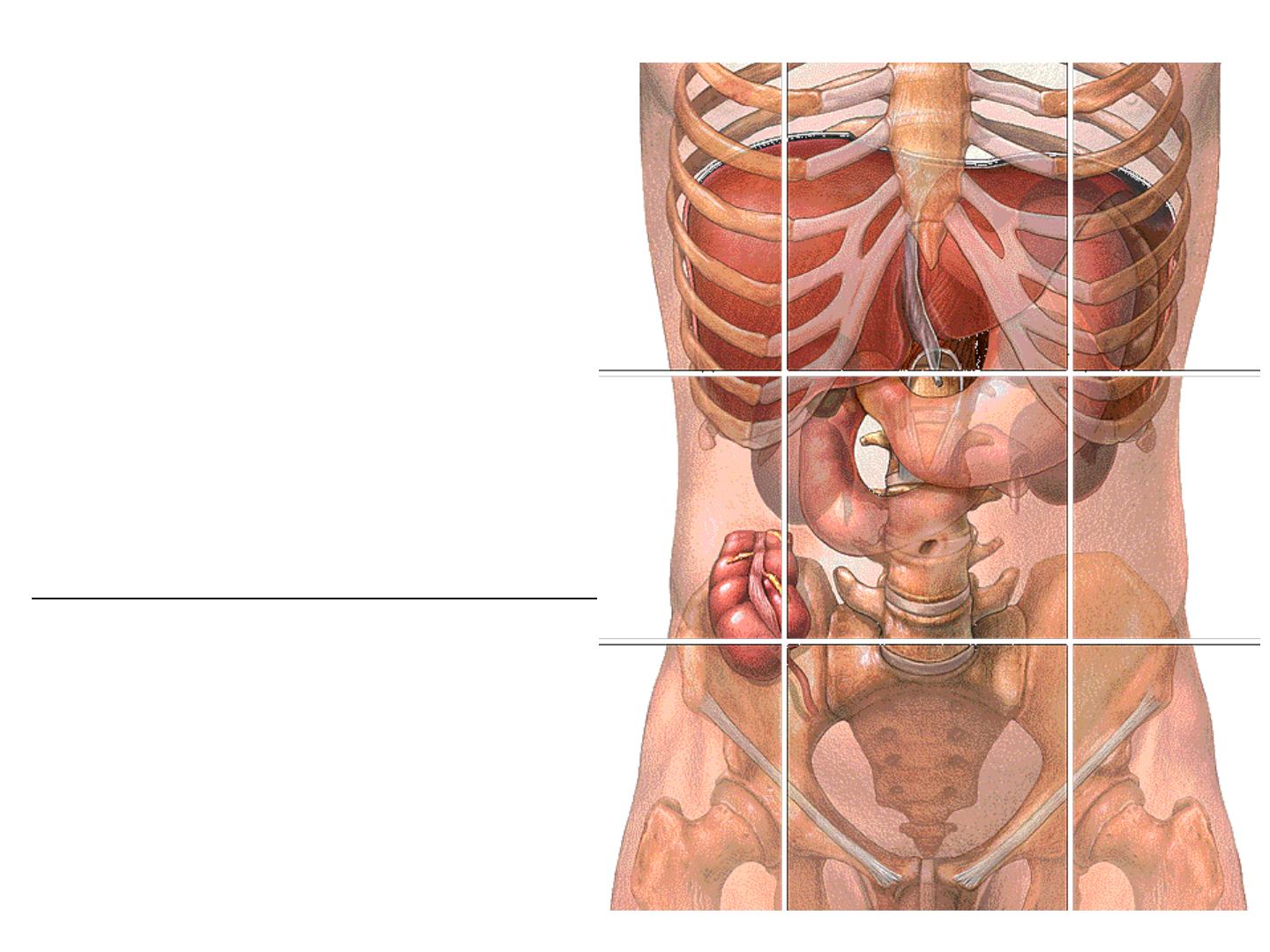
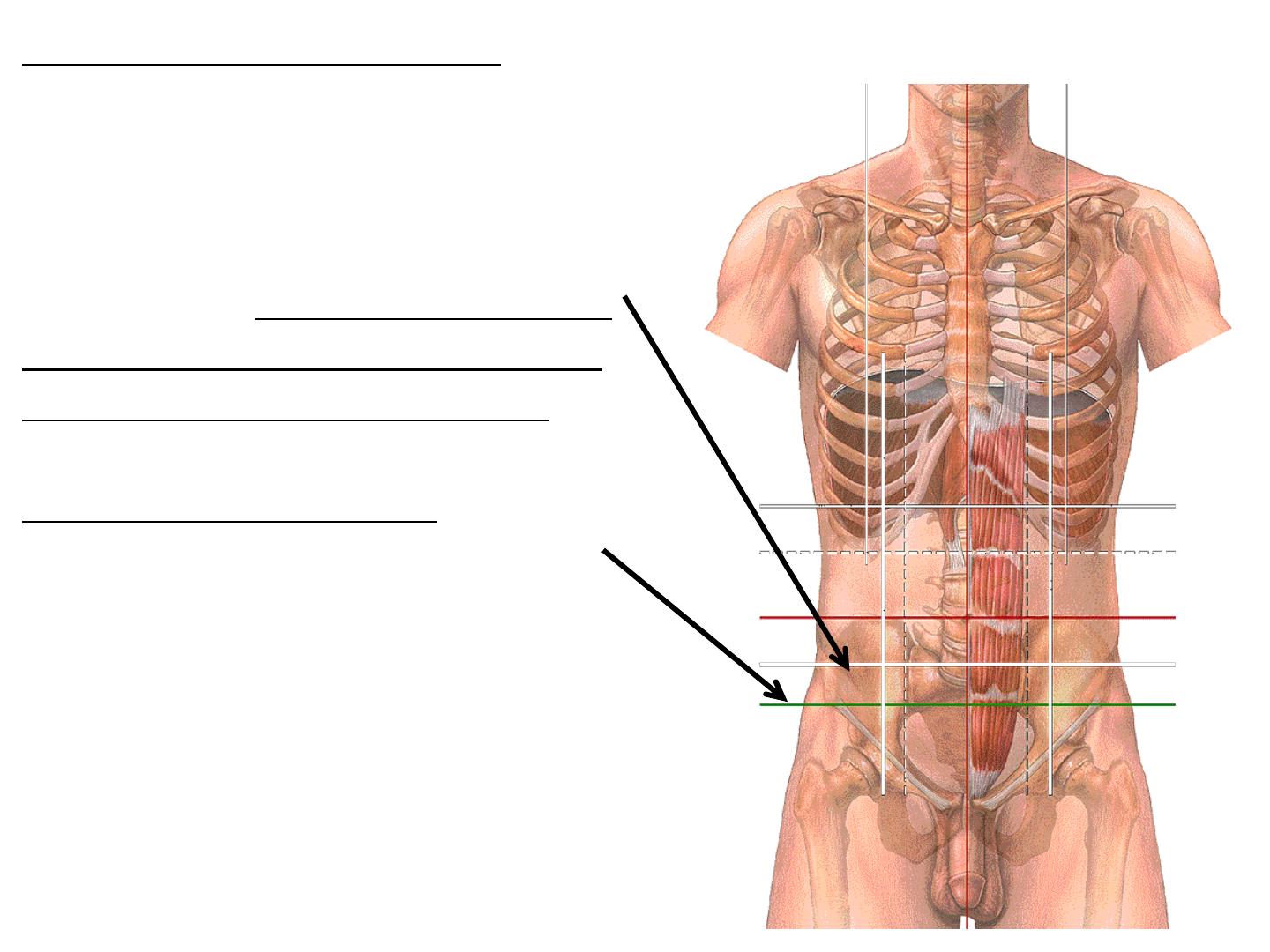
ABDOMINAL REGIONS
The abdomen can be divided into
nine regions by the subcostal and
transtubercular planes and the two
midclavicular planes. These regions
are used in practice for descriptive
localization of the position of a mass
or the localization of a patient's pain.
They may also be used in the
description of the location of the
abdominal viscera.
The nine regions thus formed are:
epigastrium;
right and left hypochondrium;
central or umbilical;
right and left lumbar;
hypogastrium or suprapubic;
right and left iliac fossa.
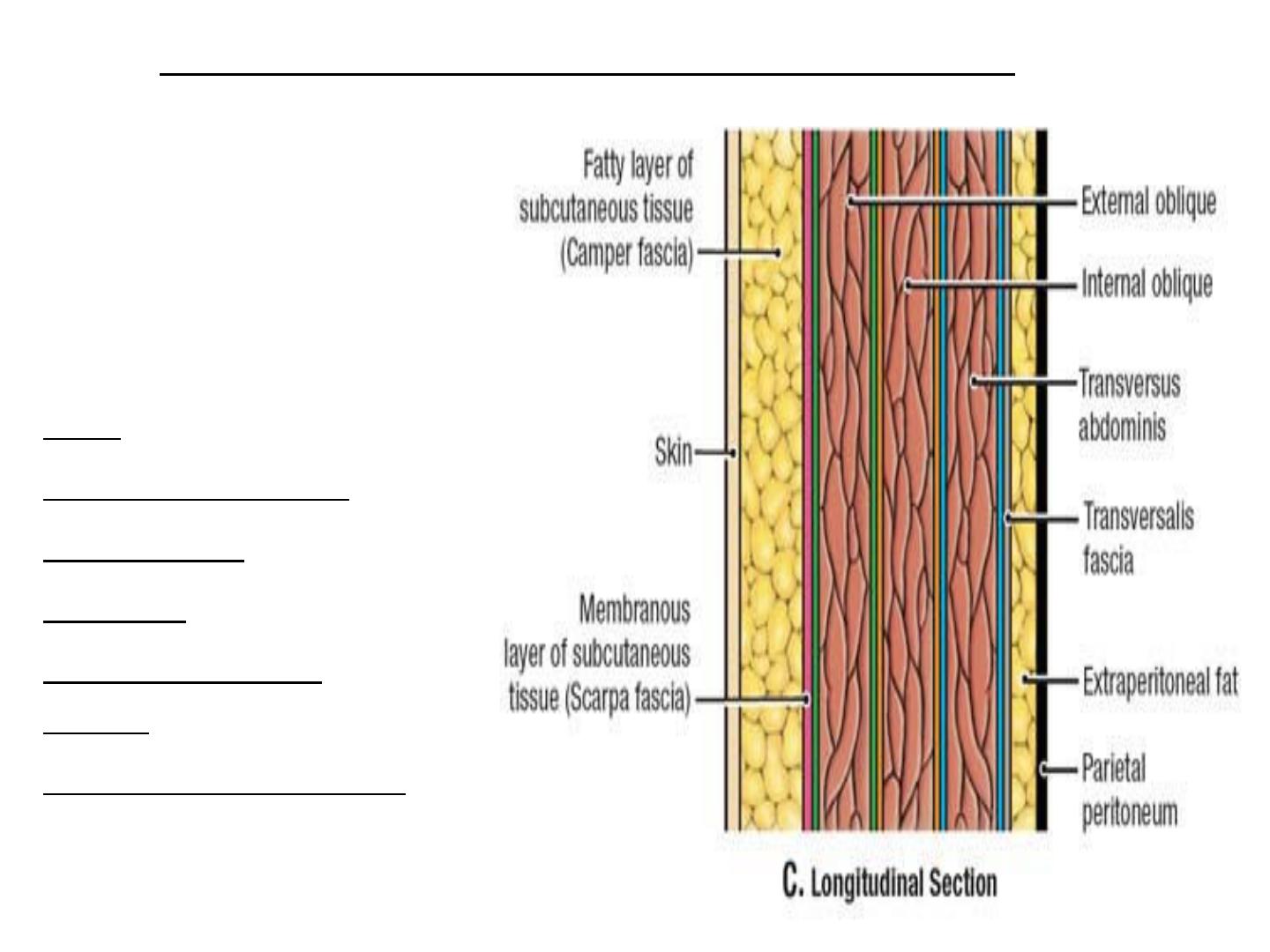
The anterior
abdominal wall is
made up of;
skin,
superficial fascia,
deep fascia,
muscles,
extraperitoneal
fascia, and
parietal peritoneum.
● Layers of the anterior abdominal wall.
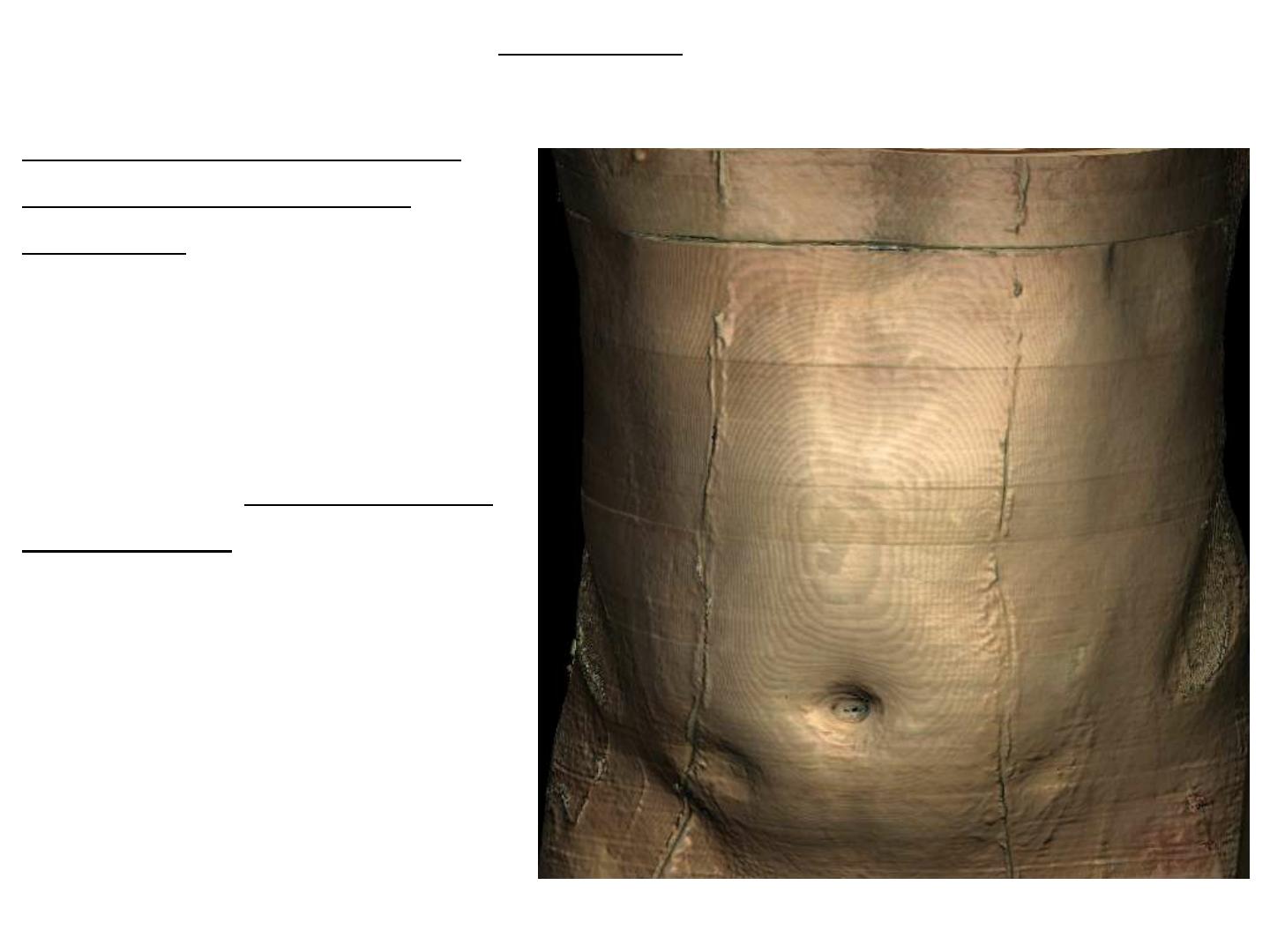
●The skin
۩The skin is loosely
attached to the underlying
structures except at the
umbilicus, where it is
tethered to the scar tissue.
۩The natural lines of
cleavage in the skin are
constant and run downward
and forward almost
horizontally around the
trunk.
۩The umbilicus is a scar
representing the site of
attachment of the umbilical
cord in the fetus; it is situated
in the linea alba.

Clinical Notes
Surgical Incisions
All surgical incisions should be made in the lines of cleavage where
the bundles of collagen fibers in the dermis run in parallel rows. An
incision along a cleavage line will heal as a narrow scar, whereas one
that crosses the lines will heal as wide scars.
Infection of the Umbilicus
In the adult, the umbilicus often receives scant attention in the shower
and is consequently a common site of infection.
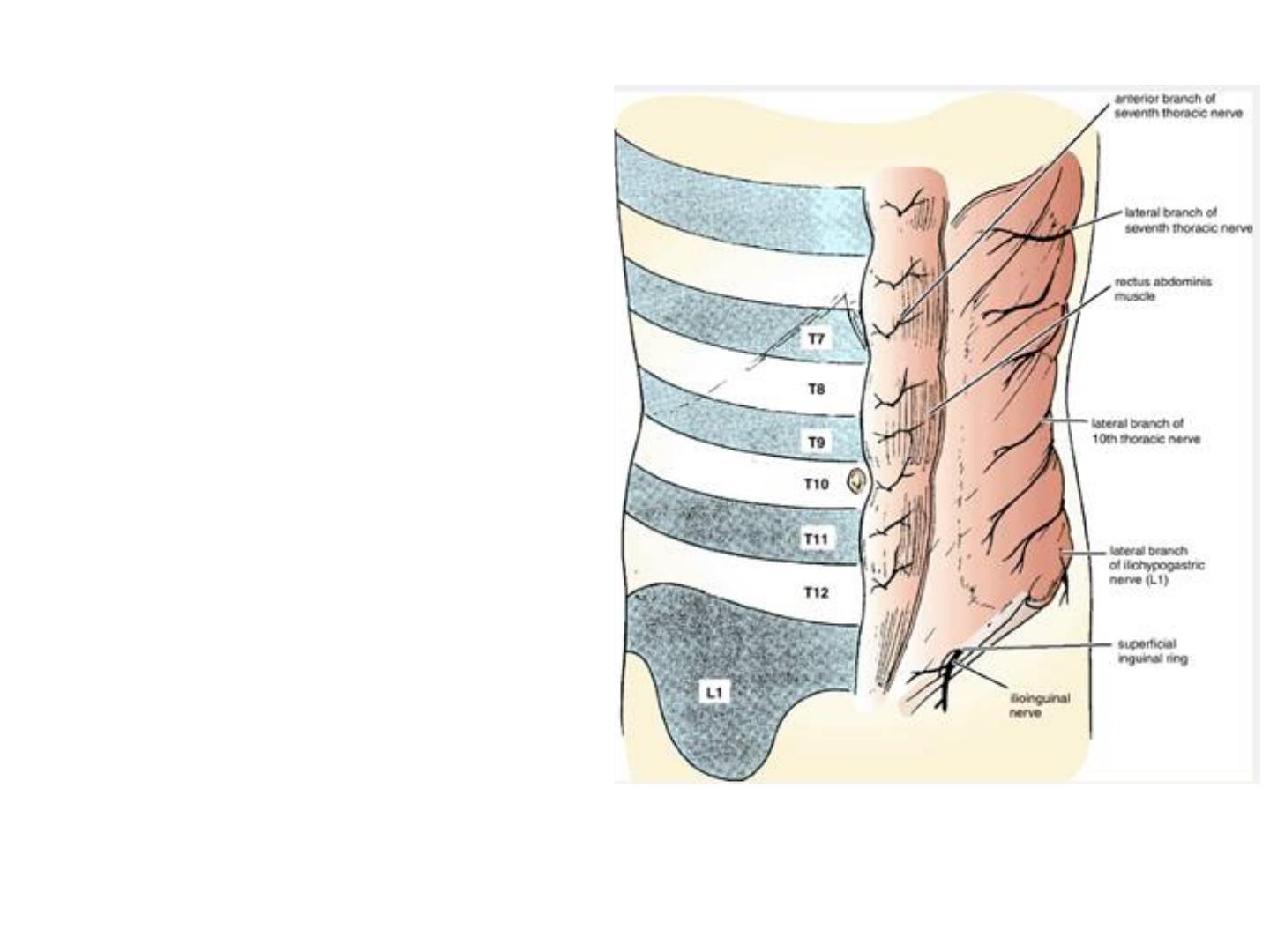
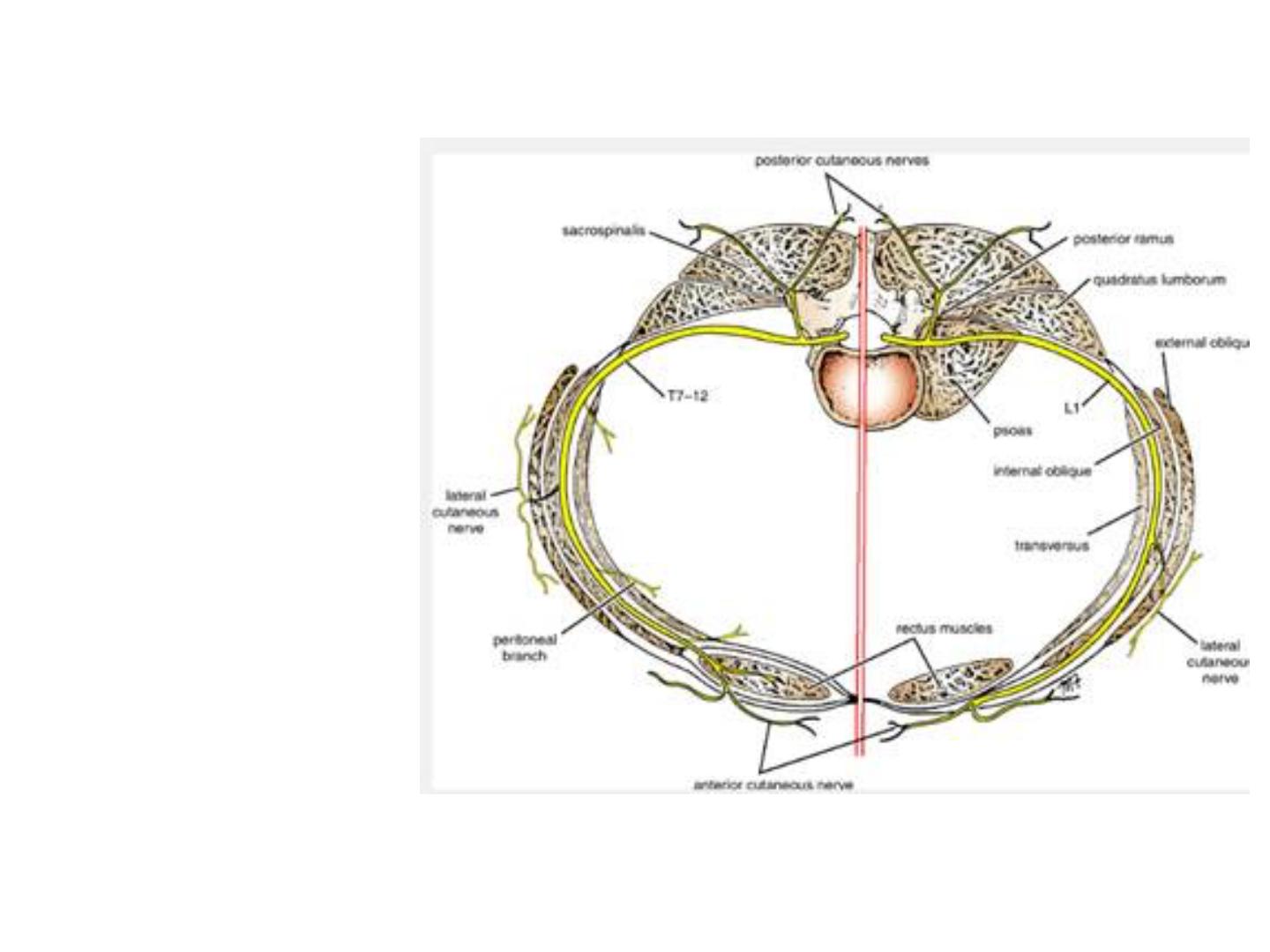
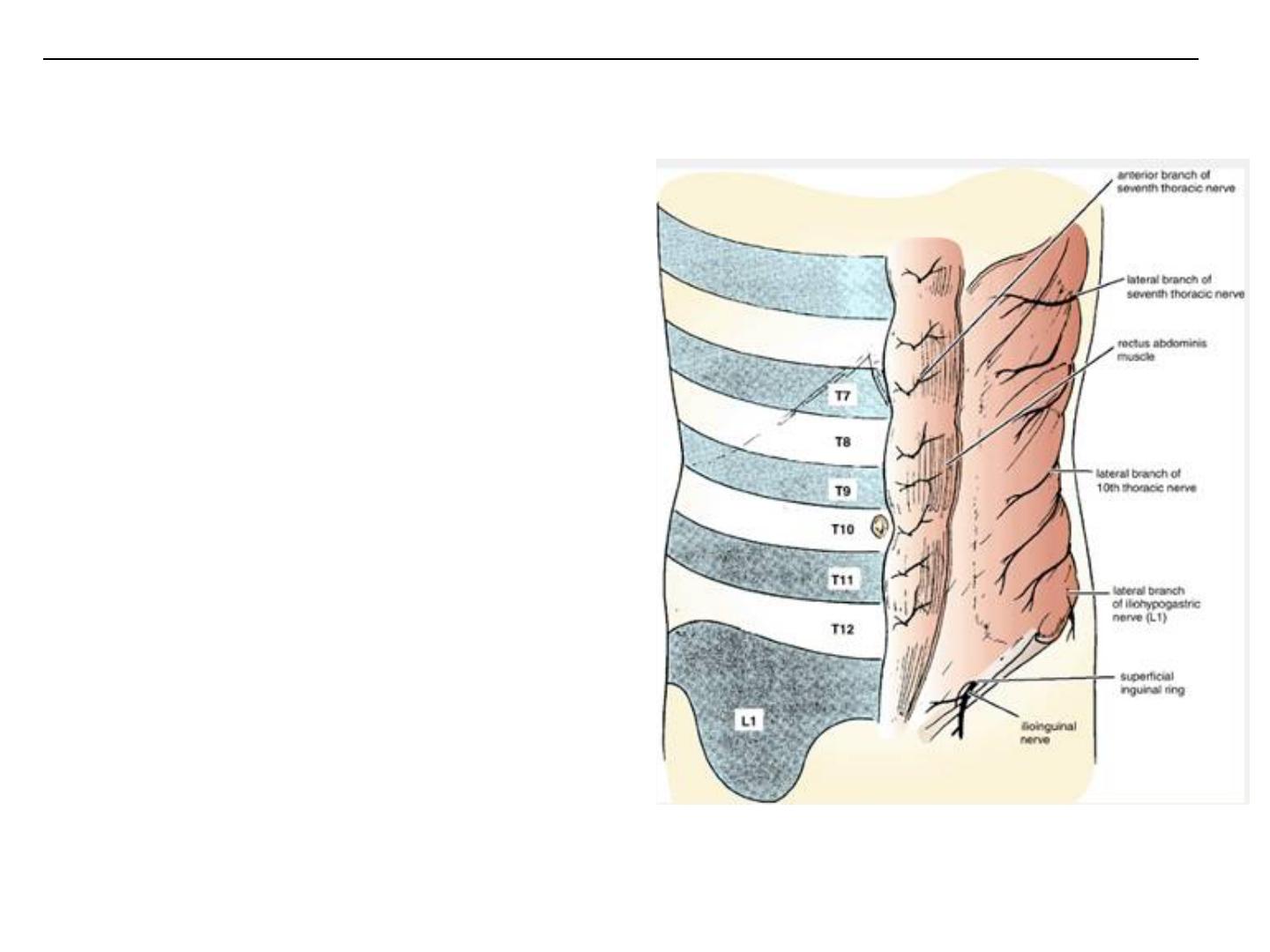
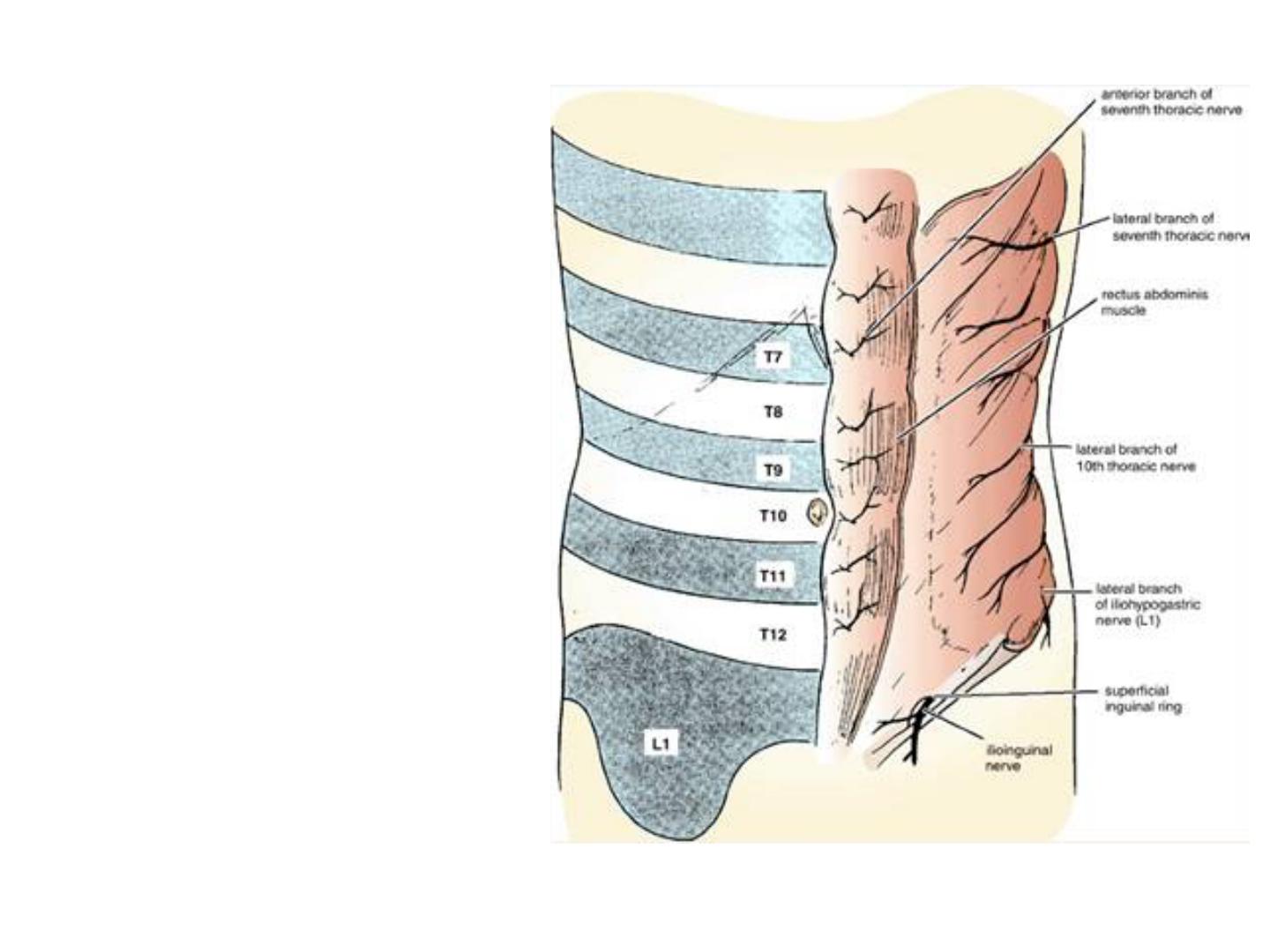
Nerve Supply
The cutaneous nerve supply to the
anterior abdominal wall is derived
from the anterior rami of the lower
six thoracic and the first lumbar
nerves .
The thoracic nerves are the lower
five intercostal and the subcostal
nerves;
the first lumbar nerve is
represented by the iliohypogastric
and the ilioinguinal nerves.
The dermatome of T7 is located in
the epigastrium over the xiphoid
process. The dermatome of T10
includes the umbilicus, and that of L1
lies just above the inguinal ligament
and the symphysis pubis.
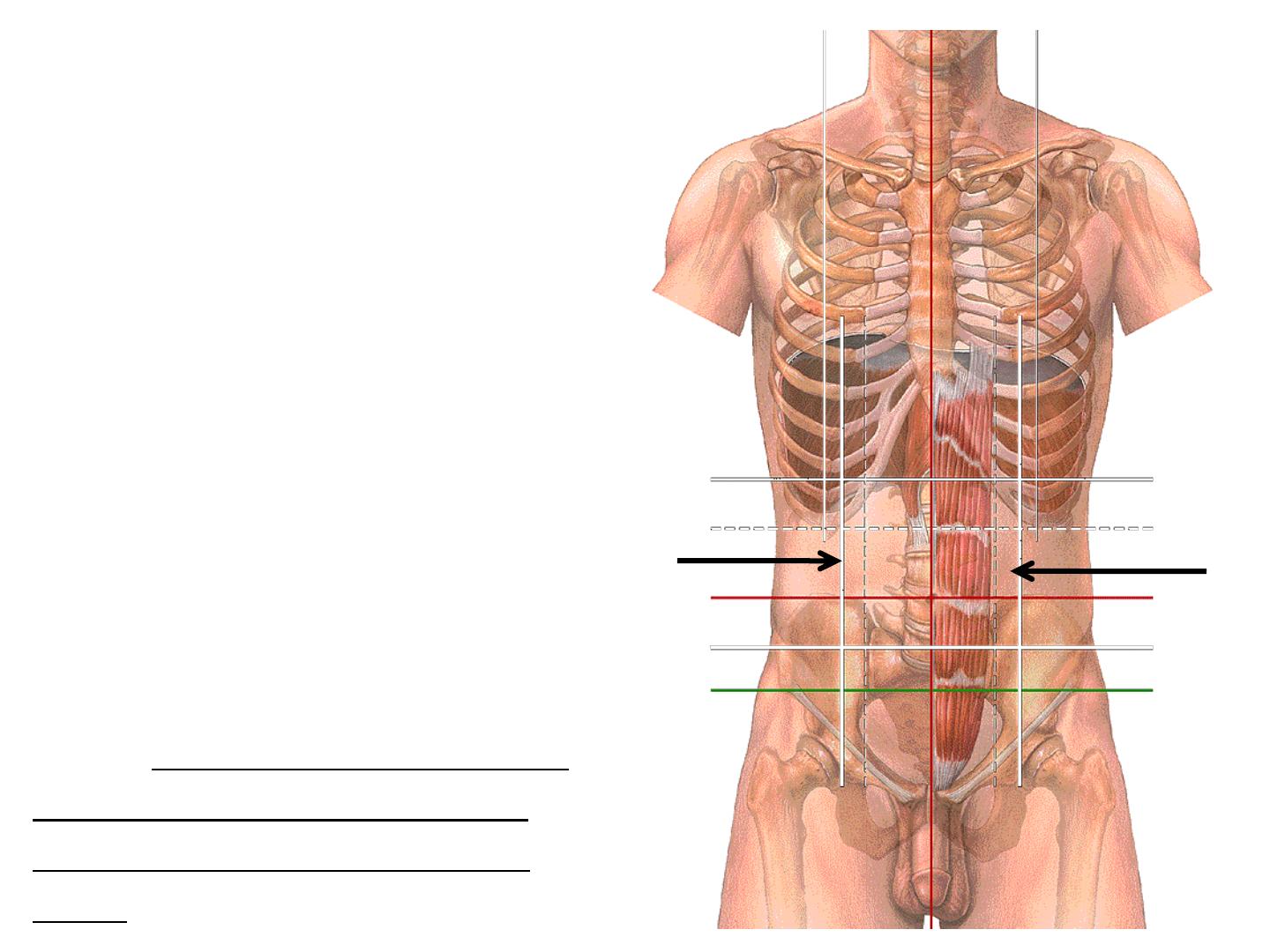
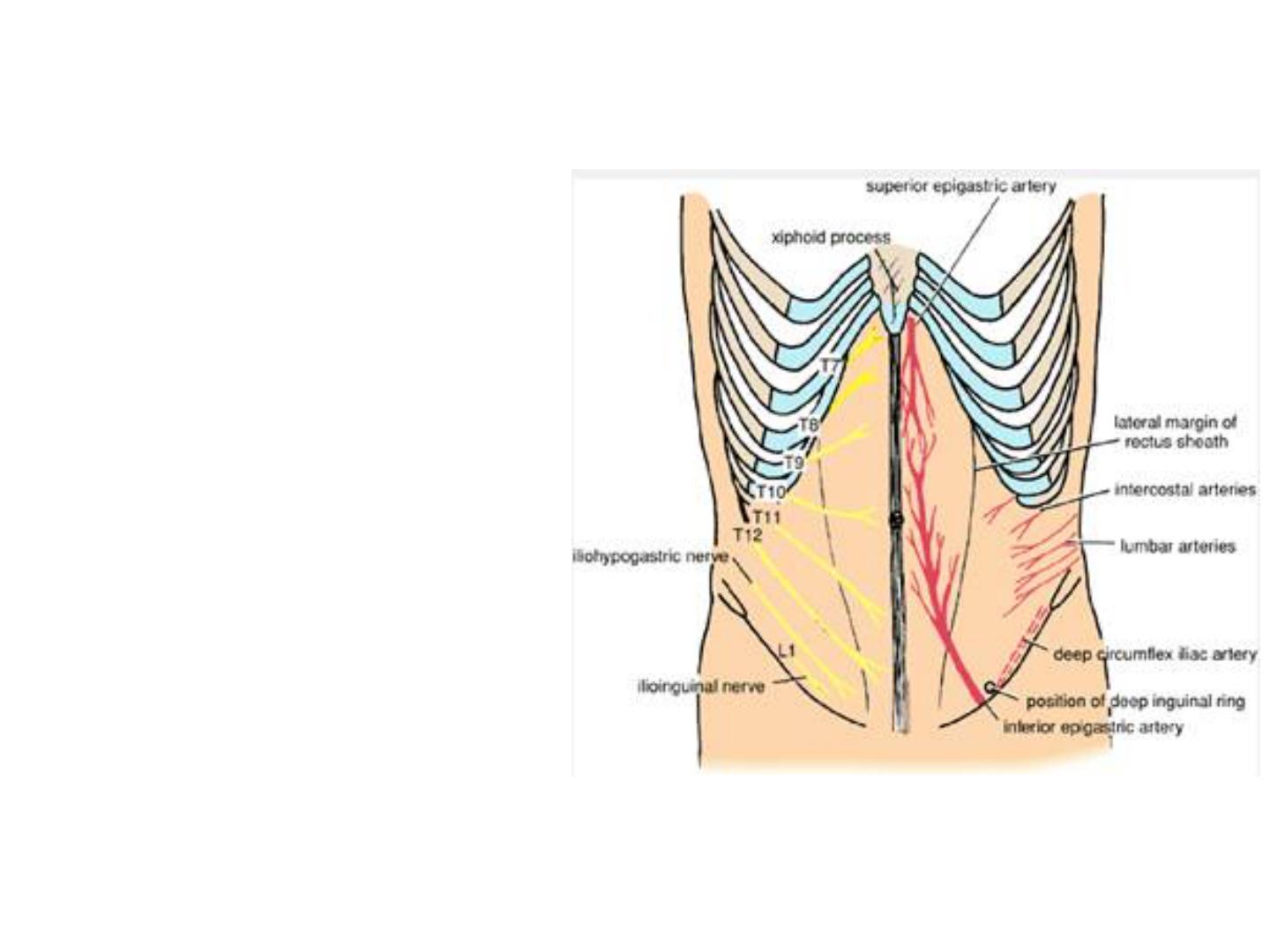
Dermatomes and distribution of
cutaneous nerves on the anterior
abdominal wall.
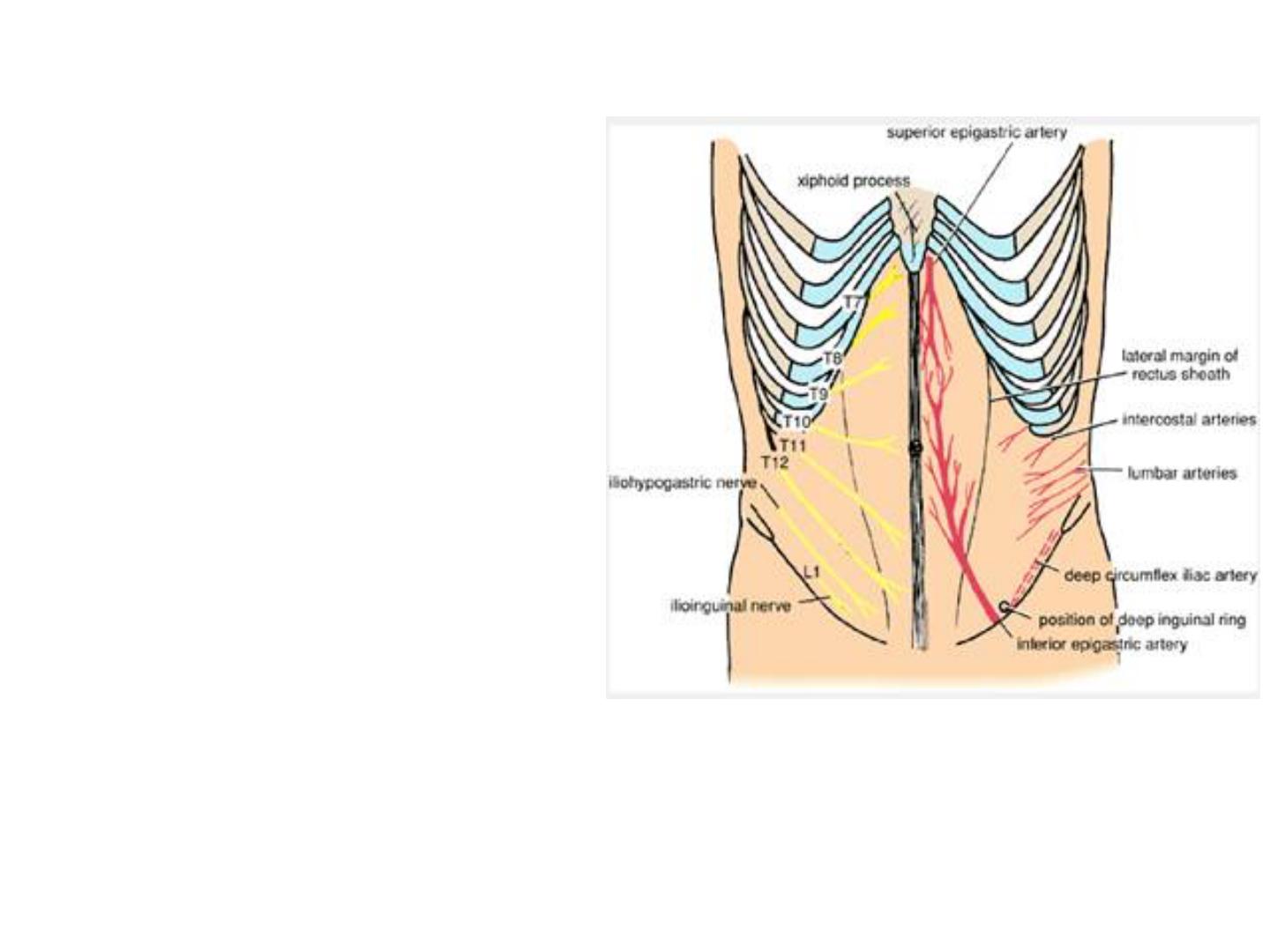
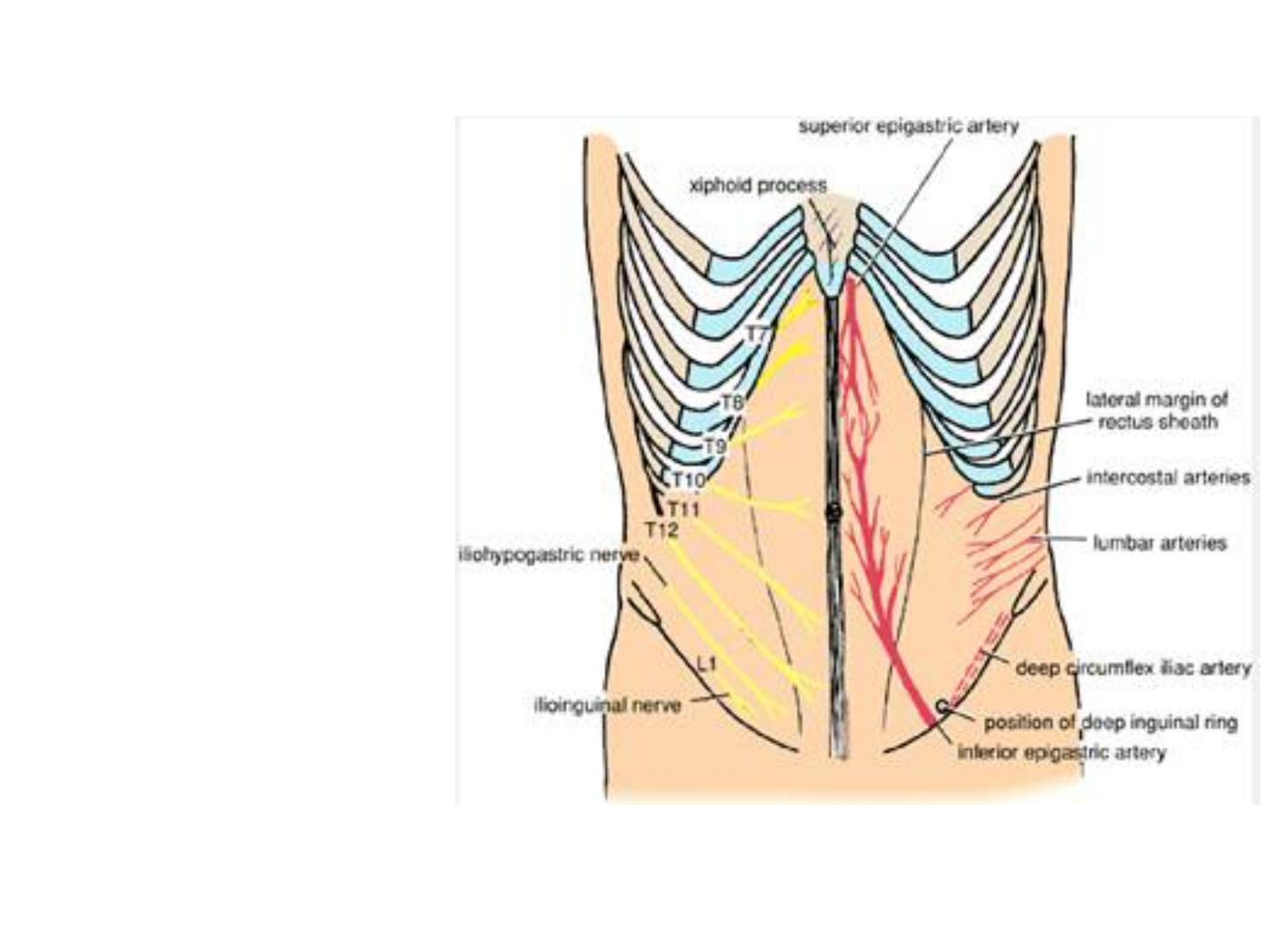
Blood Supply
Arteries
The skin near the midline is
supplied by branches of the
superior and the inferior
epigastric arteries.
The skin of the flanks is supplied
by branches of the intercostal,
the lumbar, and the deep
circumflex iliac arteries .
The skin in the inguinal region is
supplied by the superficial
epigastric, the superficial
circumflex iliac, and the
superficial external pudendal
arteries, branches of the femoral
artery.
segmental innervation of the anterior
abdominal wall (left) and arterial supply
to the anterior abdominal wall (right).
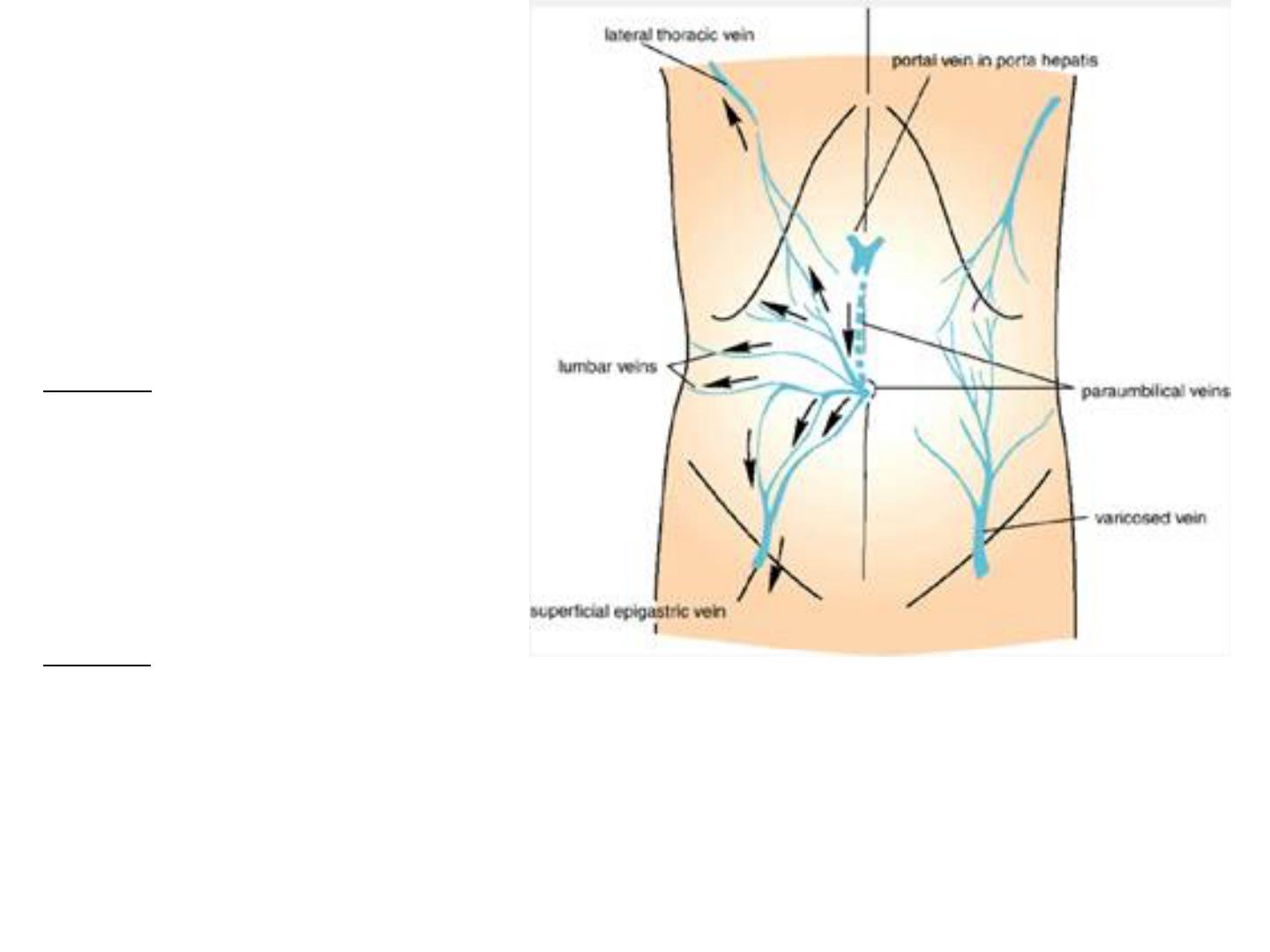
Blood Supply
Veins
The venous
drainage passes
above mainly into the
axillary vein via the
lateral thoracic vein
and
below into the femoral
vein via the superficial
epigastric and the
great saphenous veins.
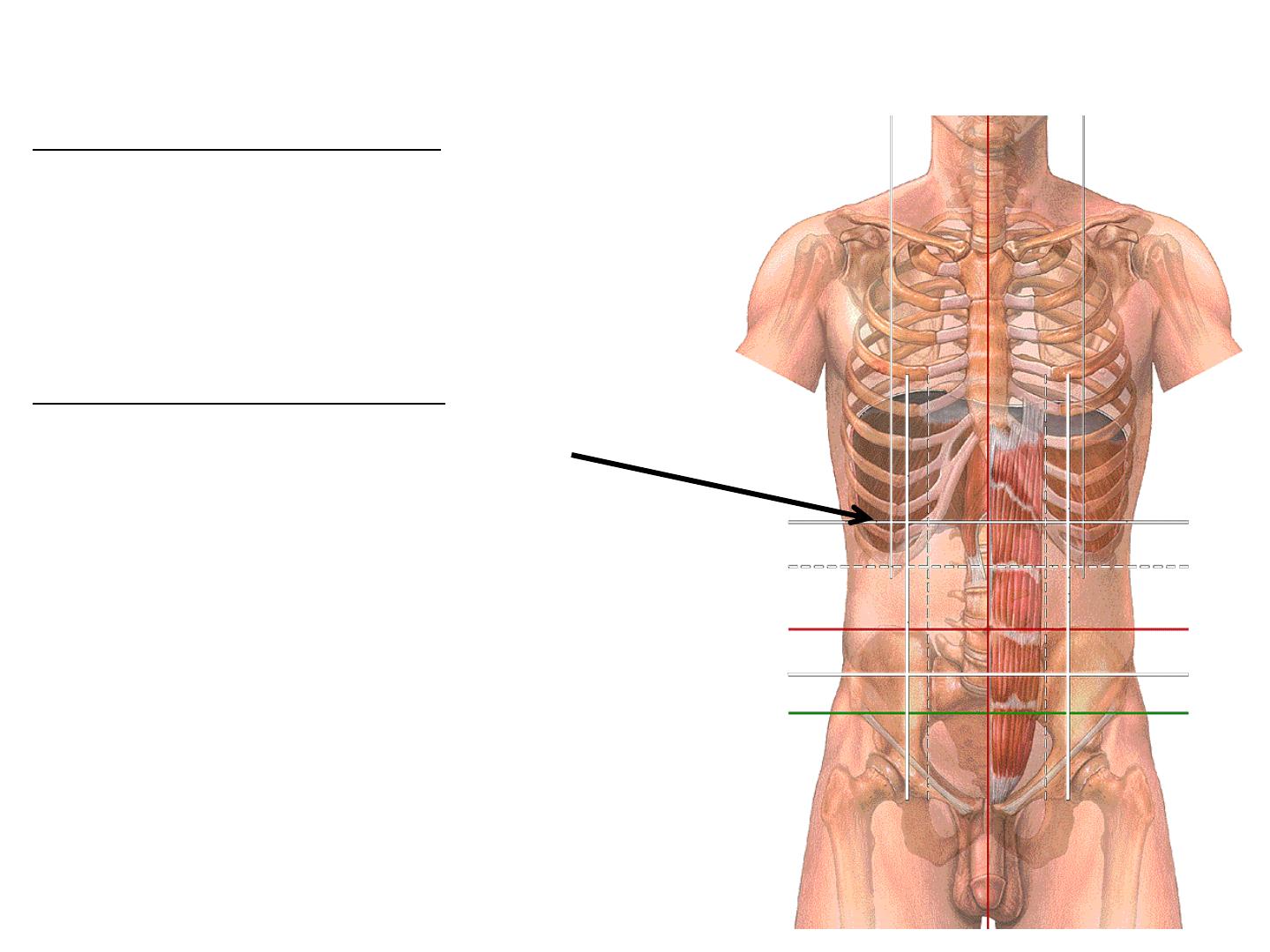
On the left are anastomoses between systemic veins
and the portal vein via paraumbilical veins. Arrows
indicate the direction taken by venous blood when the
portal vein is obstructed. On the right is an enlarged
anastomosis between the lateral thoracic vein and the
superficial epigastric vein. This occurs if either the
superior or the interior vena cava is obstructed.
● Applied anatomy of the anterior abdominal wall, and surgical incision
Incisions of the Abdominal Wall
Principles
Three requirements for a proper
abdominal incision:
●accessibility
●extensibility
●security
The following rules should be
observed where they apply:
●The incision should be adequate:
long enough for good exposure and
for room to work, but short enough
to avoid unnecessary complications.
●Skin incisions should follow
Langer's lines where possible.
●Incisions parallel with existing
scars should be avoided.
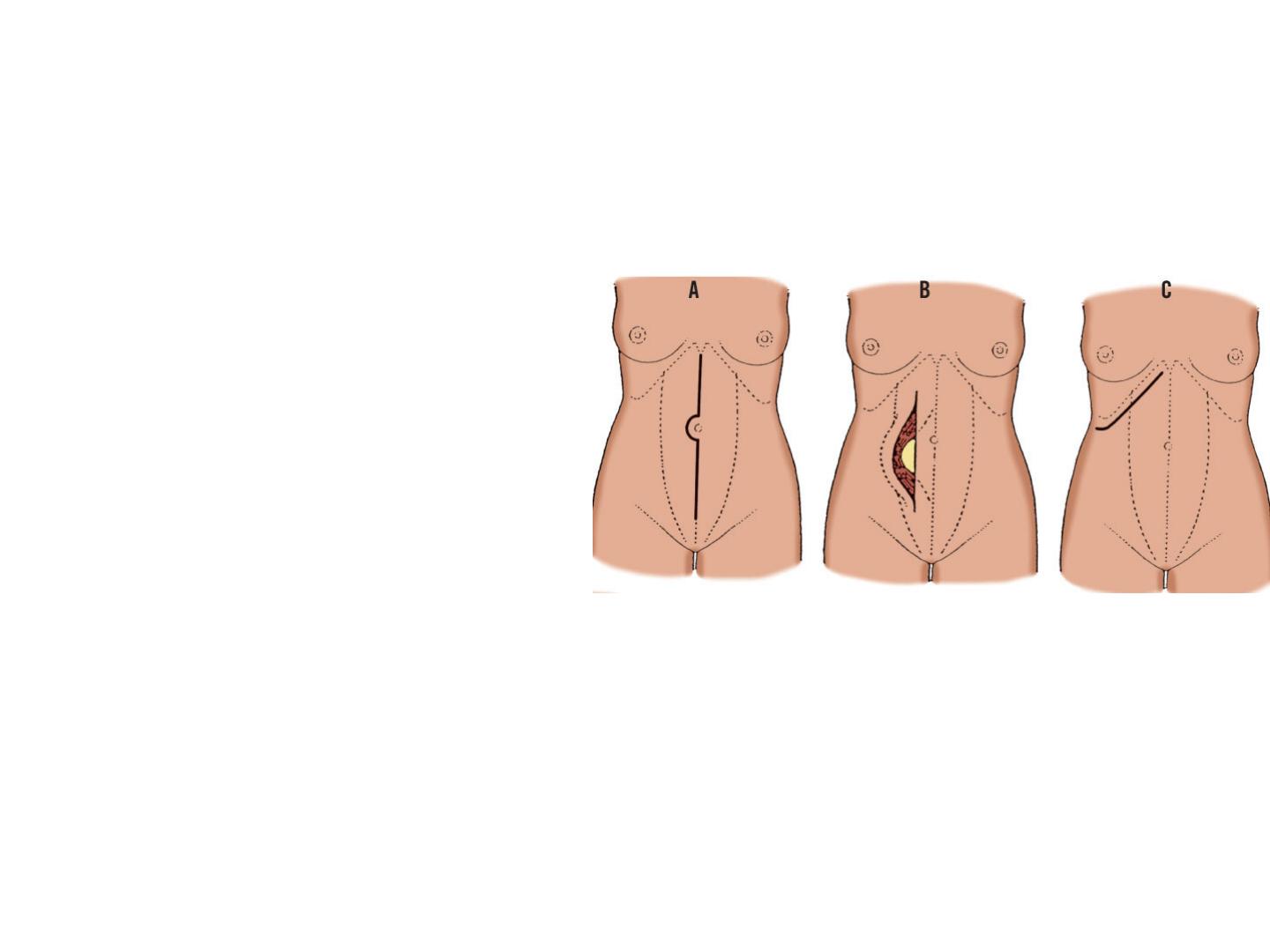
A, Midline (linea alba) incision. B,
Paramedian (rectus) incision with muscle
retraction. C, Subcostal incision.
●Muscles should be split
in the direction of their
fibers rather than
transected. An exception
is the rectus muscle,
which may be transected
because it has a
segmental nerve supply.
There is no risk of
denervation.
●The openings formed
through the different
layers of the abdominal
wall should not be
superimposed.
●Cutting of nerves should
be avoided wherever
possible.
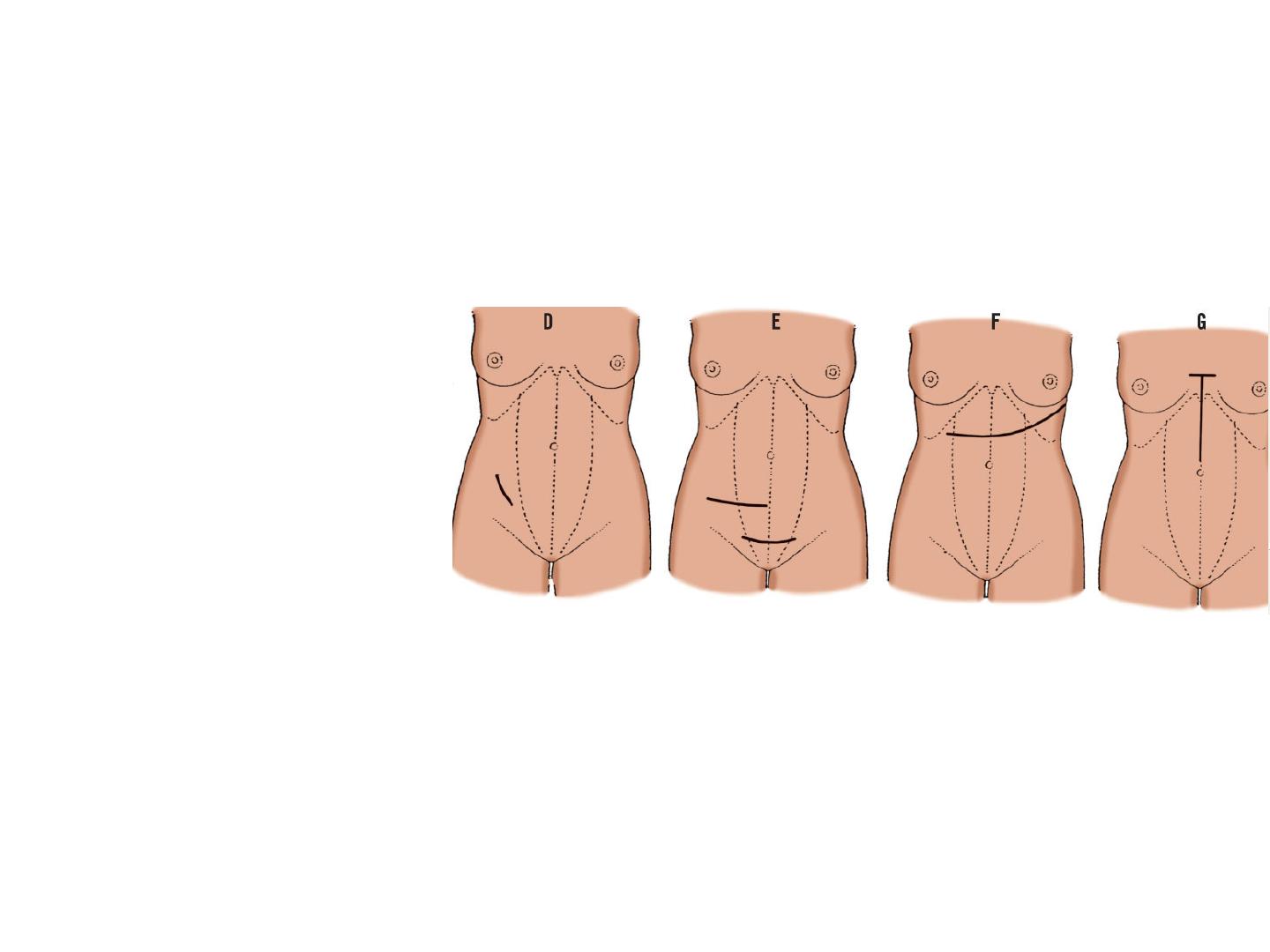
D, McBurney incision. E, Transverse abdominal
incision. F and G, Two types of thoracoabdominal
incisions.
●Muscles and
abdominal organs
should be retracted
toward, not away
from, their
neurovascular supply.
●Drainage tubes
should be inserted in
separate small
incisions, not in the
main incision. They
may weaken the
wound.
●Cosmetic
considerations must
be given close
attention.
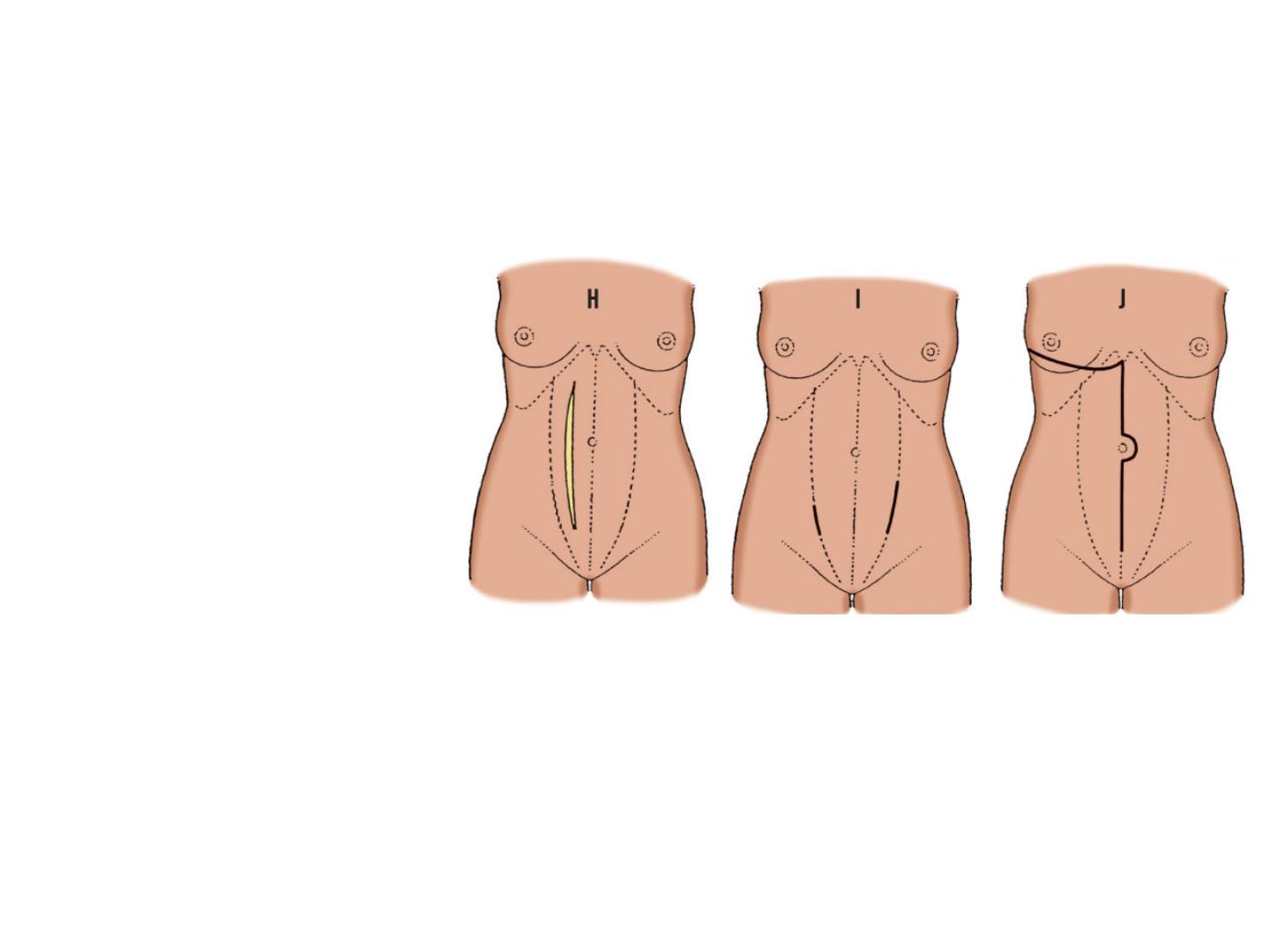
H, Paramedian (rectus) incision with muscle
splitting. I, Pararectus incision. J, "Hockey
stick" (thoracoabdominal) incision.
Vertical
Incisions
Upper midline incisions
of the linea alba and the
transversalis fascia may
reveal abundant and
well-vascularized fat in
the upper midline. We
suggest that incisions of
the peritoneum be made
slightly to the left of the
midline to avoid the
ligamentum teres in the
edge of the falciform
ligament. If the
ligamentum teres is
encountered, it may be
ligated and divided.
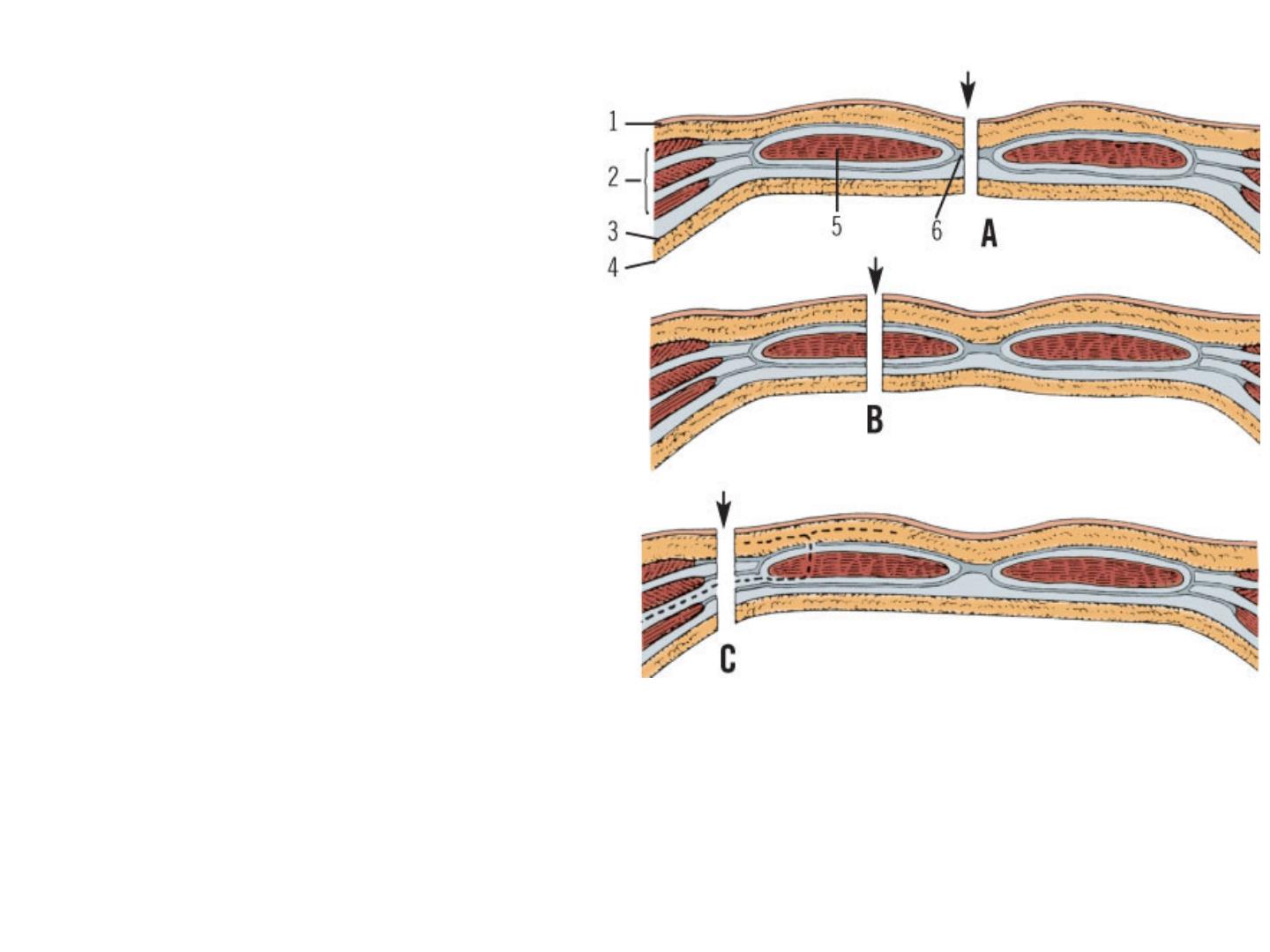
Vertical incisions. A, Incision through linea alba. B,
Incision through rectus muscle (paramedian), splitting
muscle. C, Incision lateral to rectus sheath (pararectus).
Segmental nerves to rectus muscle (dashed line) will be
cut. 1, Skin; 2, Three flat muscles and their aponeuroses;
3, Transversalis fascia; 4, Peritoneum; 5, Rectus
abdominis muscle; 6, Linea alba.
Upper Midline Incision
An upper midline
incision can be enlarged
upward by removal of the
xiphoid process and
upward extension of the
peritoneal opening.to
provide access to the
upper margin of the liver,
vena cava, and hepatic
veins, as well as the
gastroesophageal
junction.
A downward
continuation of an upper
midline incision is
always an available
option.
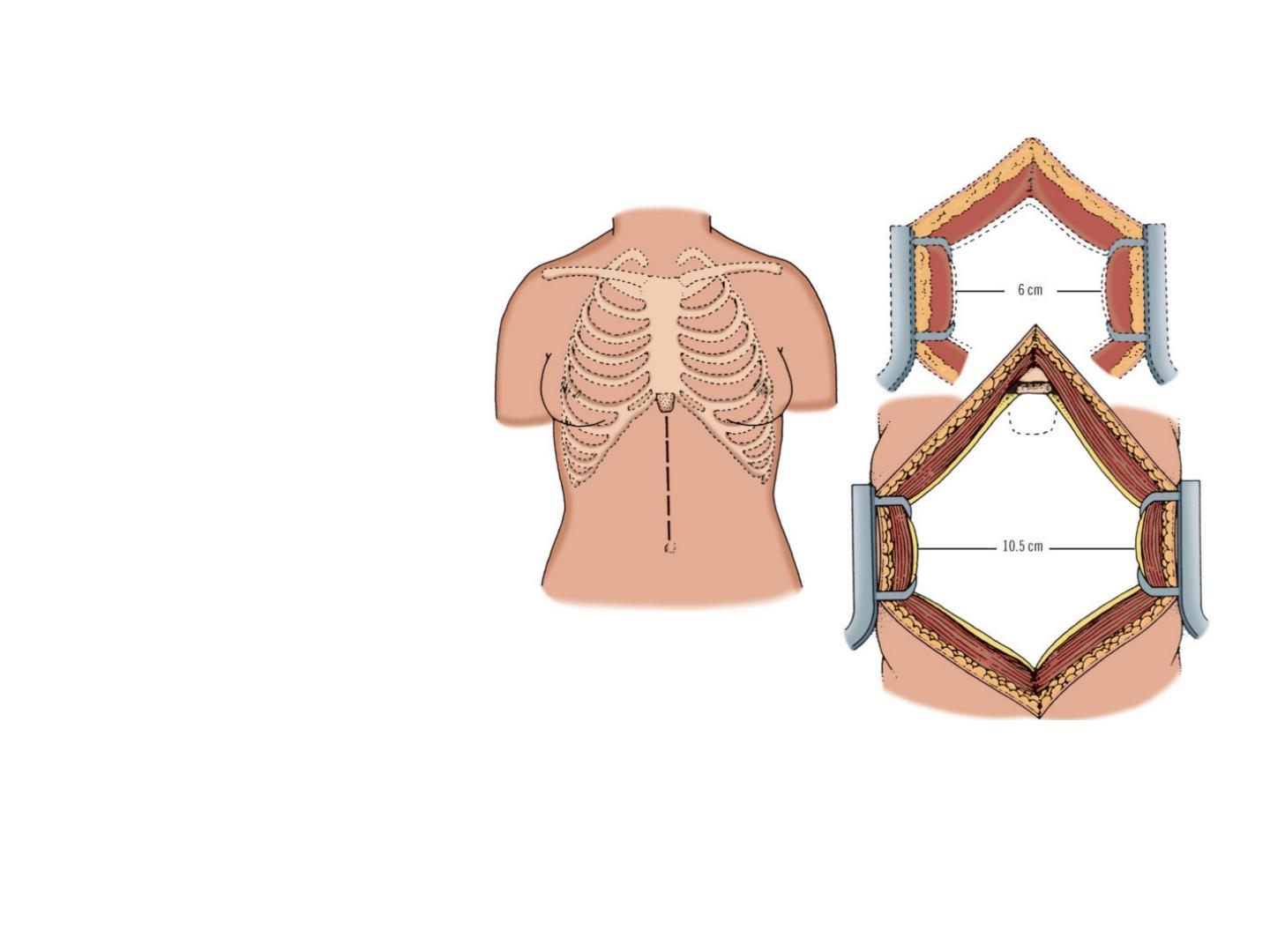
Increased abdominal exposure by excision of xiphoid
process. Left, Upper midline abdominal incision.
Right, Usual exposure of about 6 cm (broken lines),
and 10-11 cm exposure obtained after excision of
xiphoid process (solid lines).
Feasible extensions include the following:
Lower Midline Incision
The linea alba is
narrow and more difficult
to identify below.
Remember that the
bladder must always be
decompressed by
catheterization prior to
surgery.
Rectus (Paramedian)
Incision
It does not destroy muscle
tissue or nerves. The
rectus muscle should be
retracted laterally to
prevent tension on vessels
and nerves.
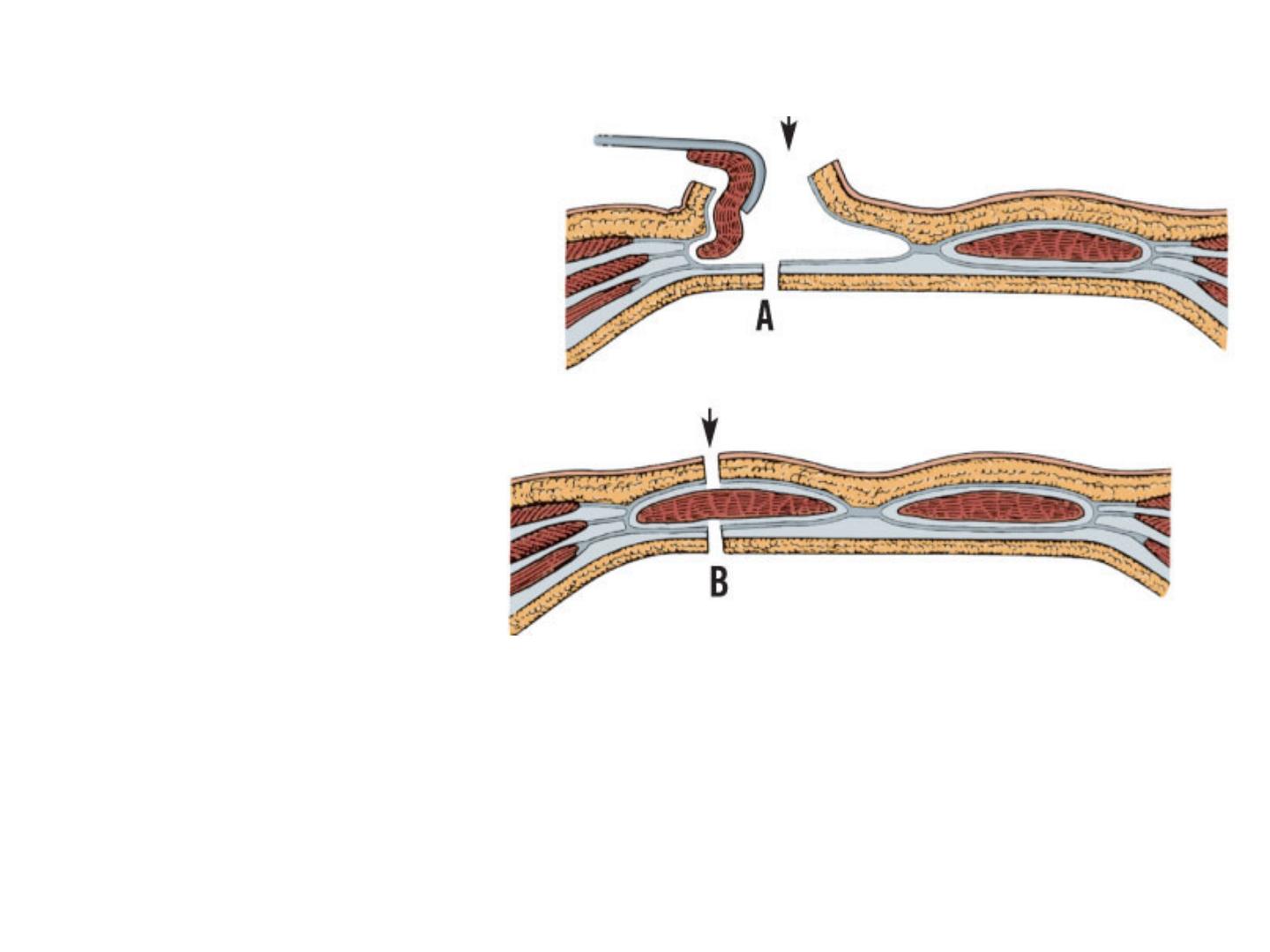
Incision through the rectus sheath without muscle
splitting. A, Lateral retraction of rectus muscle
following incision of anterior layer of sheath. B,
Release of traction allows intact muscle to bridge
incision through sheath
Transverse Incisions
In transverse incision, both
the rectus sheath and
muscle are incised.
Upper Abdominal
Transverse Incision
The rectus muscle is
transected during an upper
abdominal transverse
incision.
Lower Abdominal
Transverse Incision
Both rectus abdominis
muscles are incised, and
perhaps also right or left
flat muscles.
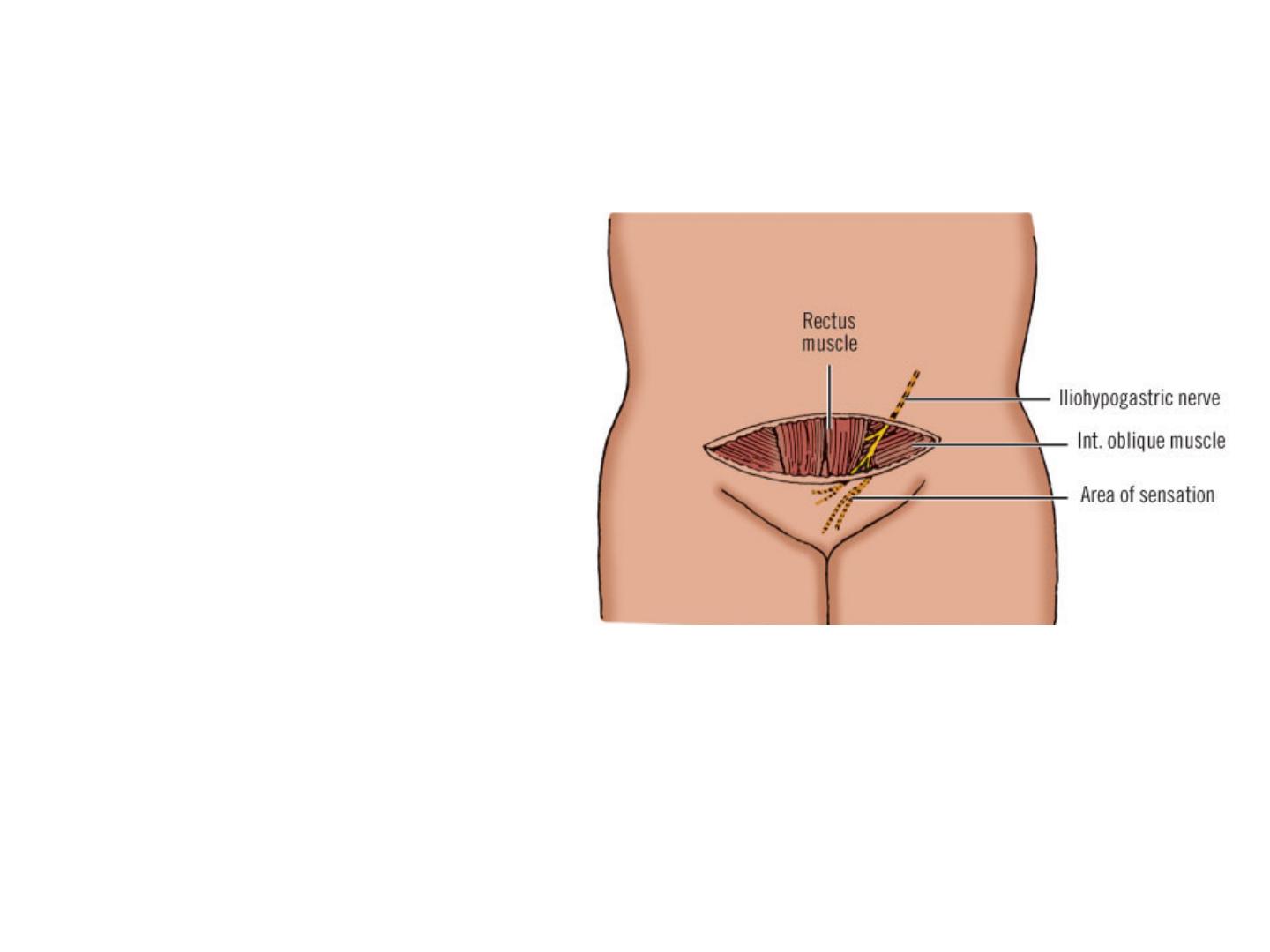
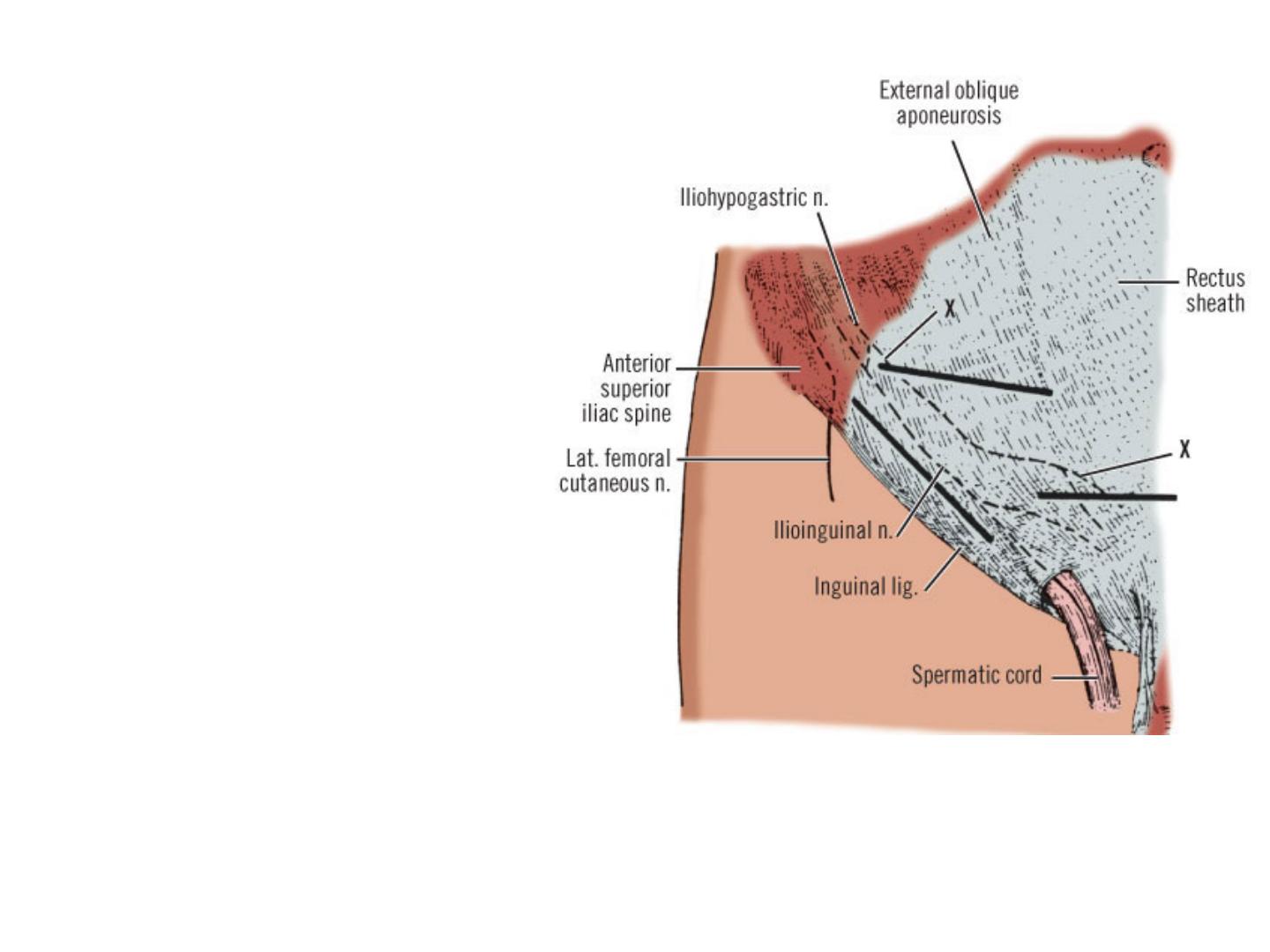
Pfannenstiel transverse abdominal incision
showing iliohypogastric nerve between internal
oblique muscle and external oblique
aponeurosis just lateral to border of rectus
muscle
Pfannenstiel Incision
The Pfannenstiel
transverse abdominal
incision is made
horizontally just above
the pubis. The
iliohypogastric nerve
must be identified and
protected.
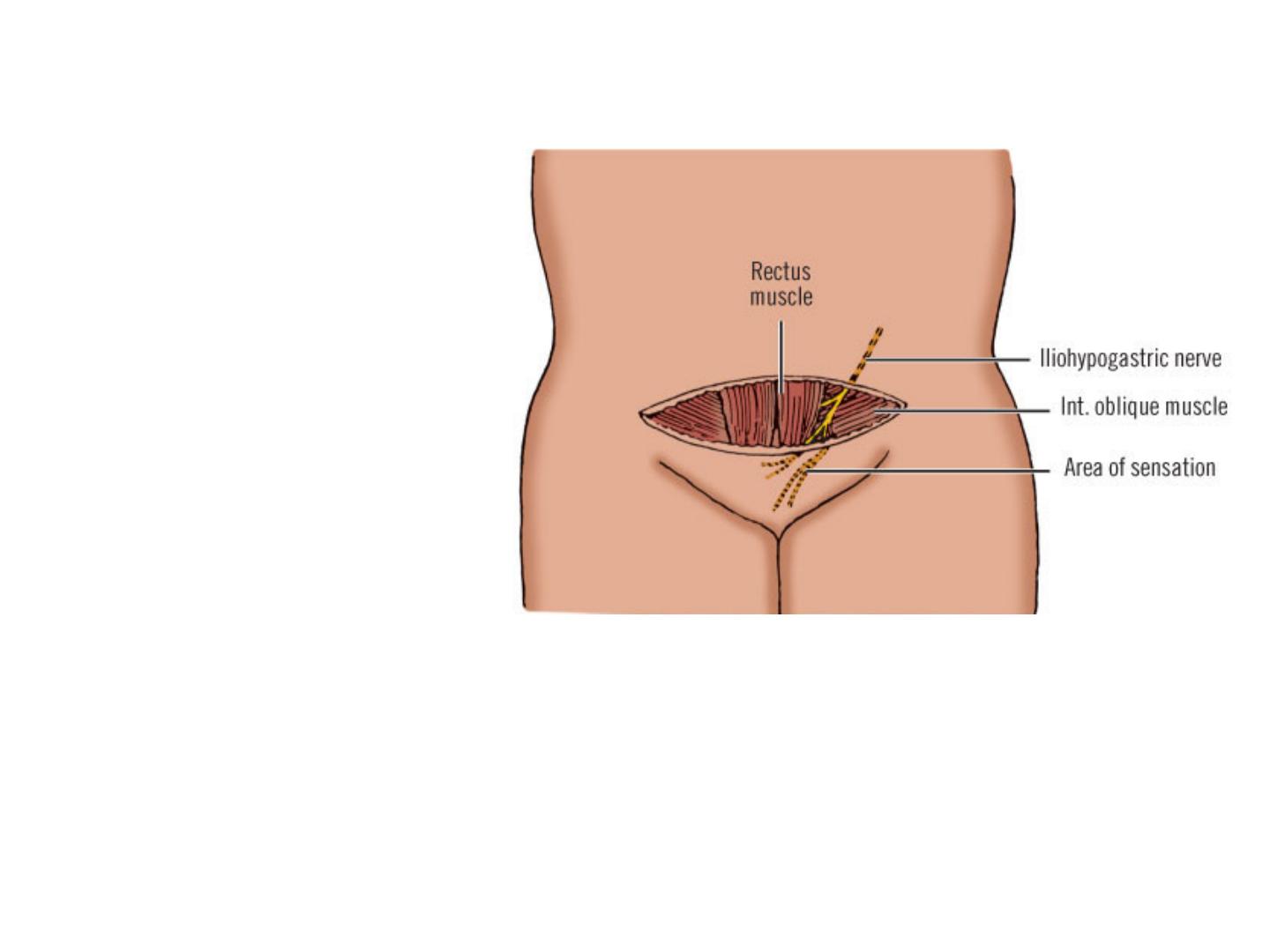
Pfannenstiel transverse abdominal incision
showing iliohypogastric nerve between internal
oblique muscle and external oblique aponeurosis
just lateral to border of rectus muscle.
Oblique Incisions
Subcostal Incision
The incision should extend
laterally no farther than necessary
in order to avoid cutting
intercostal nerves.
McBurney (Gridiron) Incision
The McBurney (gridiron)
incision starting 4 cm medial to
the right anterosuperior spine and
extending downward on a line
from the spine to the umbilicus.
The iliohypogastric nerve, deep to
the internal oblique muscle, must
be identified and preserved.
Right or Left Lateral Oblique
(Kocher)
This is an oblique incision from
the tip of the right or left 10th rib
to the pubic crest.
Courses of the iliohypogastric and ilioinguinal
nerves.
Oblique Incision
The oblique incision
is the one most
frequently used by
urologists.
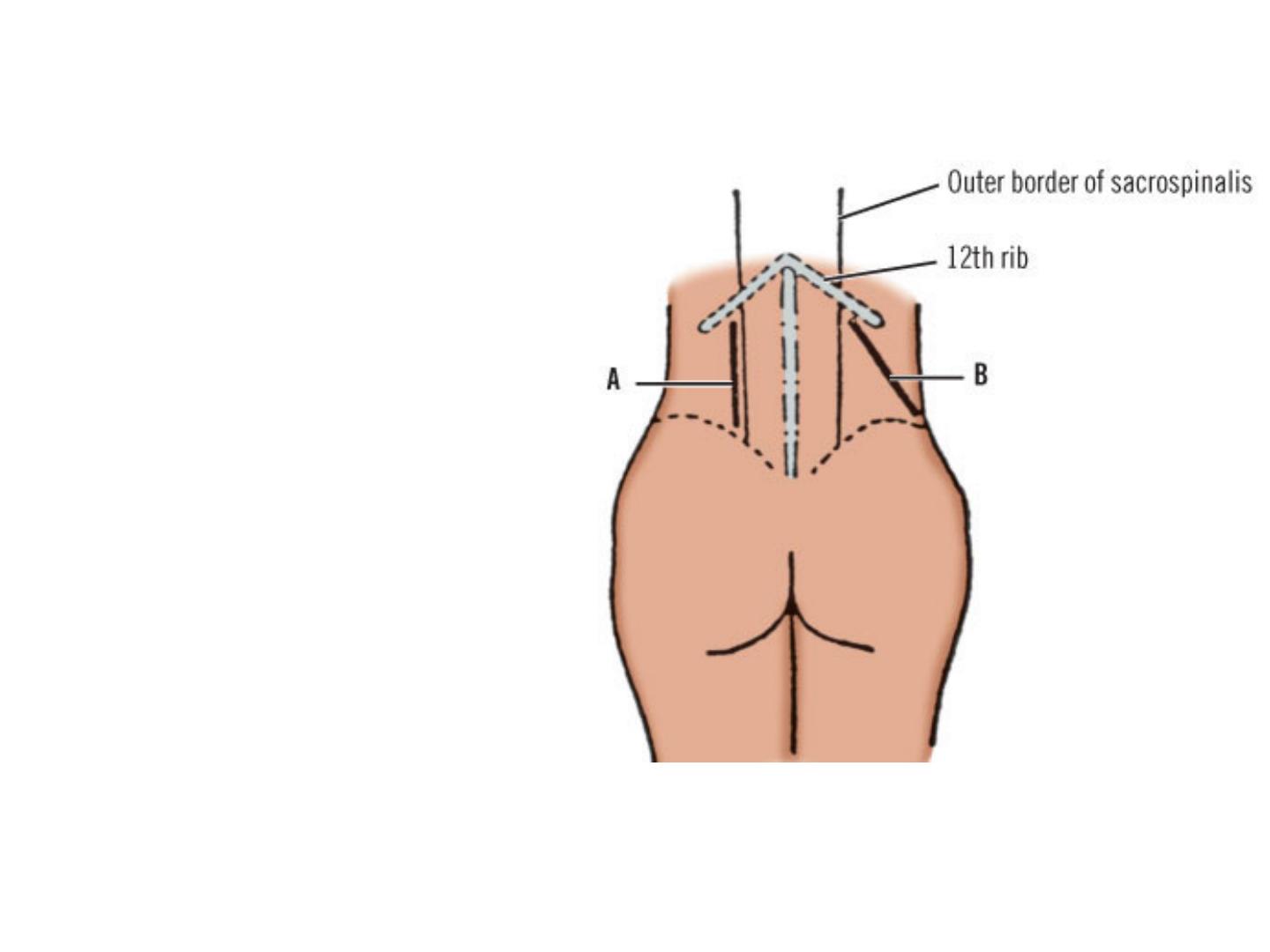
Posterior approaches to kidney. A, Vertical
incision. B, Oblique incision.
•Incisions of the Posterior (Lumbar) Abdominal Wall
Vertical Incision
The vertical incision
proceeds along the
lateral border of the
sacrospinalis from the
12th rib to the iliac
crest in a
perpendicular
orientation.
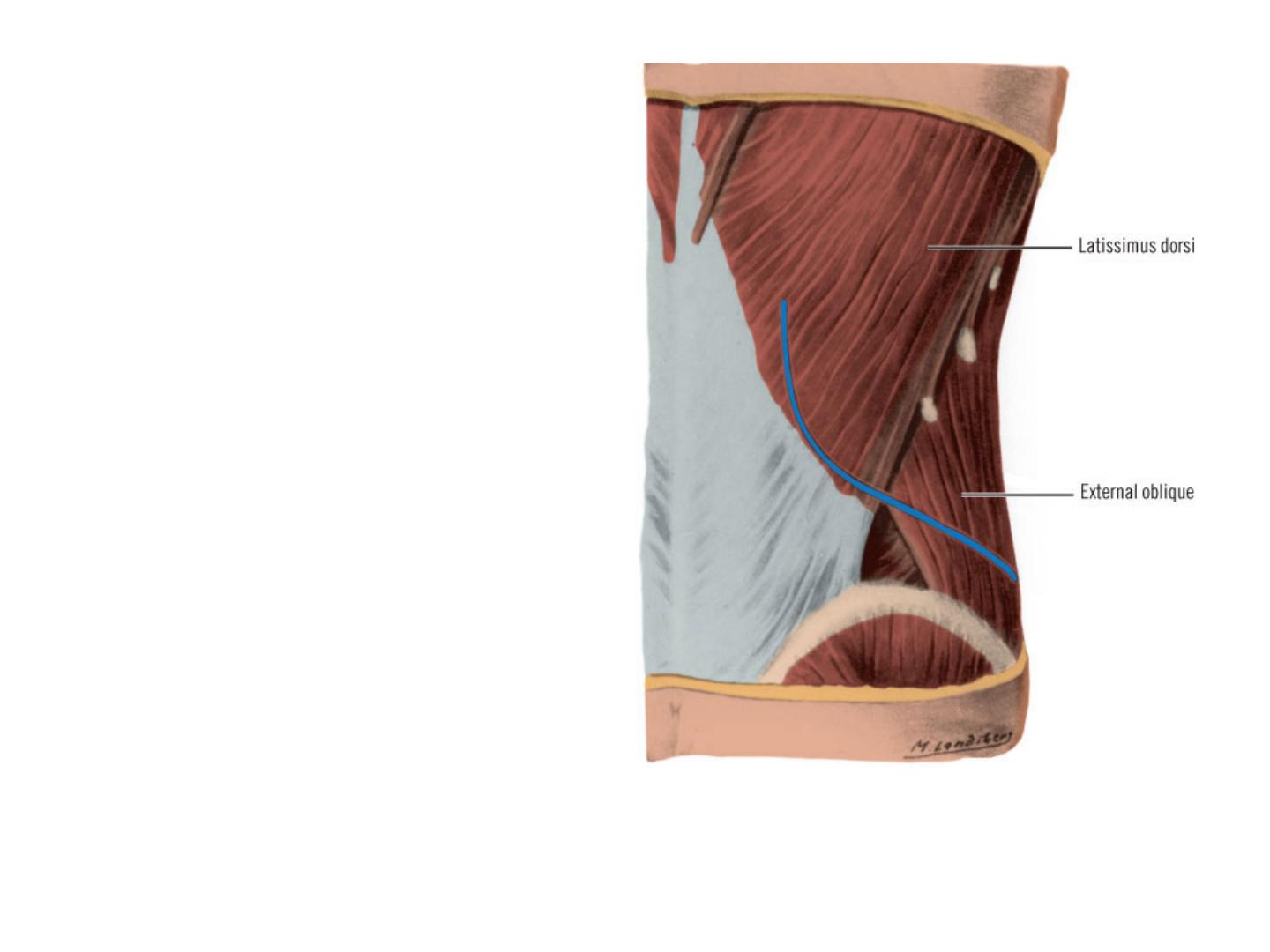
First layer of muscles to divide in lumbar
approach to kidney. Incision shown in blue.
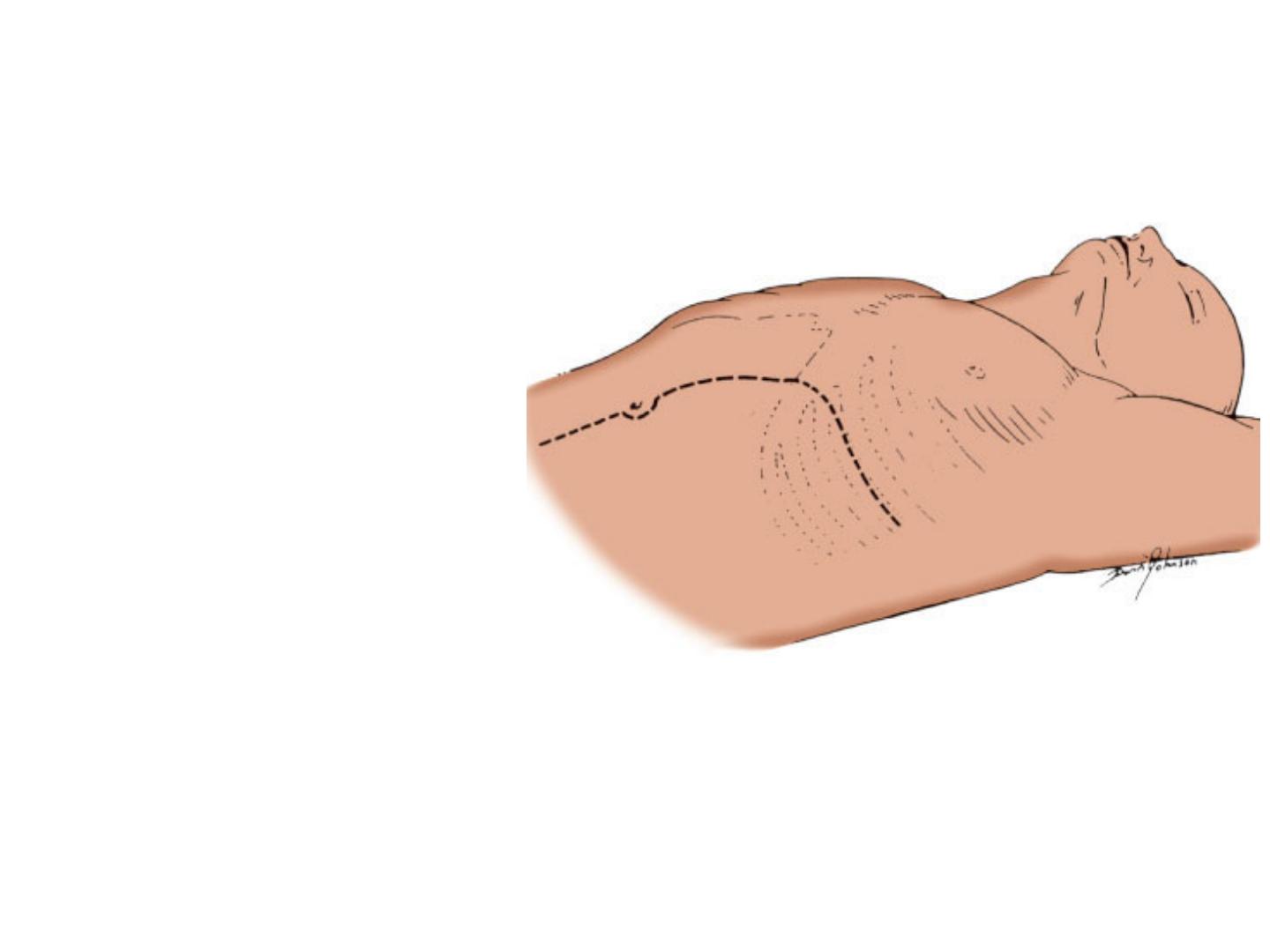
Thoracoabdominal
Incisions
In the more commonly
used left thoracoabdominal
approach, the incision
extends from a point on the
posterior axillary line near
the inferior angle of the
scapula and runs in the
seventh or eighth
intercostal space. It then
crosses the costal margin
and rectus muscle
obliquely in a line toward
the umbilicus. The incision
then continues down the
linea alba toward the pubis.
Seventh or eighth intercostal space incision
crosses costal margin obliquely and extends
down midline to the pubis.
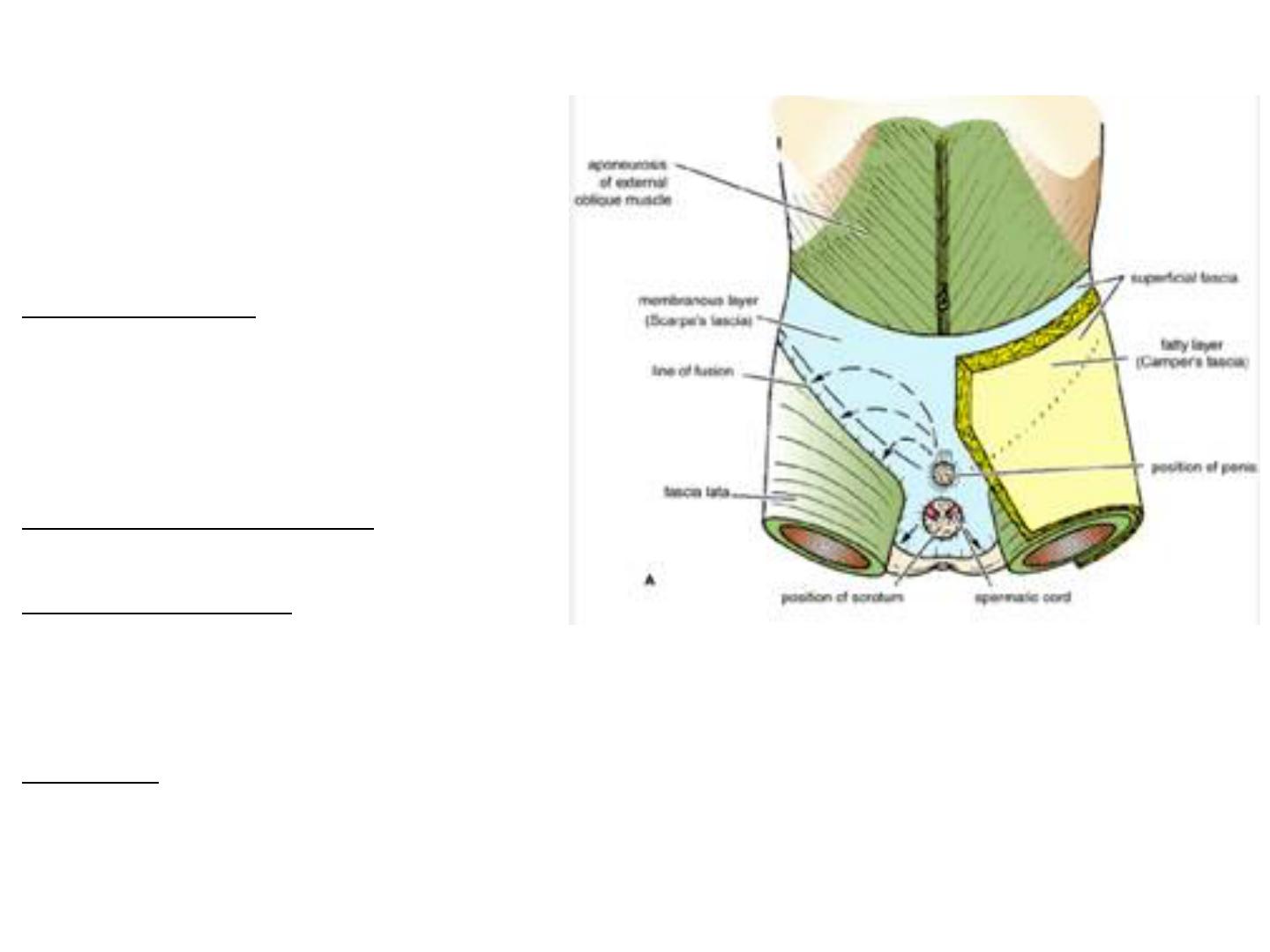
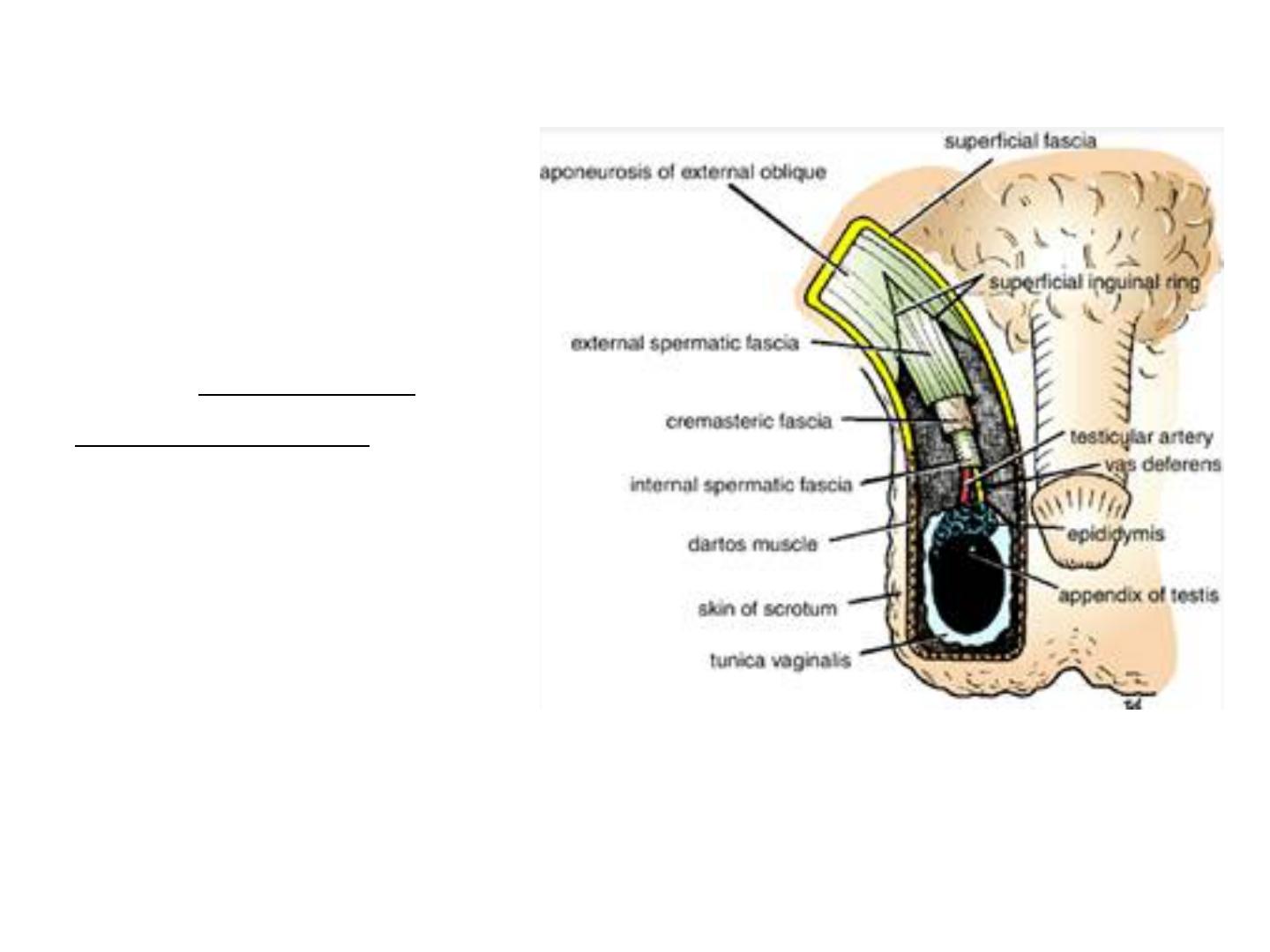
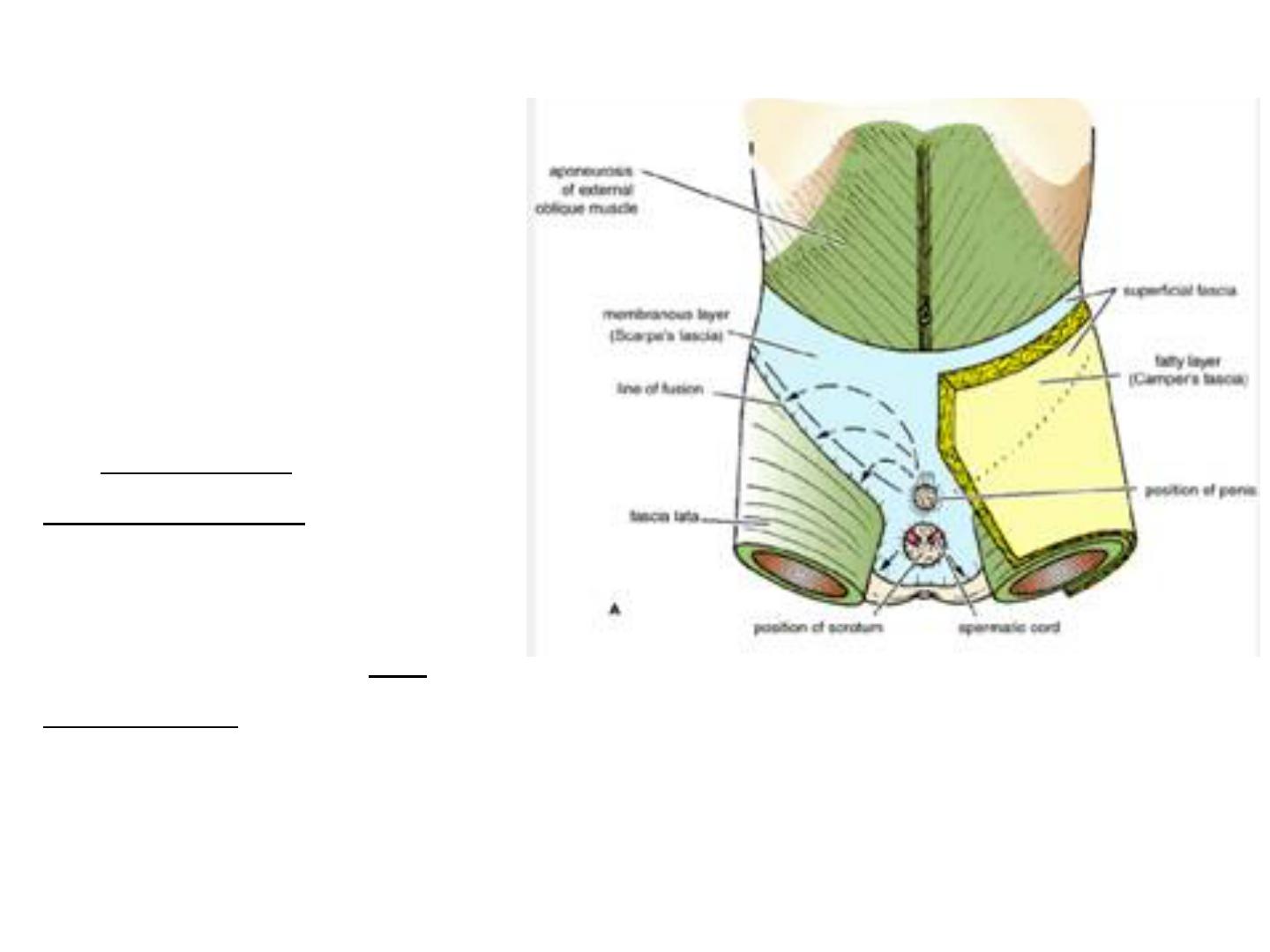
Superficial Fascia
The superficial fascia is divided
into a superficial fatty layer
(fascia of Camper) and a deep
membranous layer (Scarpa's
fascia).
The fatty layer is continuous with
the superficial fat over the rest of
the body and may be extremely
thick (3 in. [8 cm] or more in obese
patients).
The membranous layer is thin
and fades out
laterally and above, where it
becomes continuous with the
superficial fascia of the back and
the thorax, respectively.
Inferiorly, the membranous layer
passes onto the front of the thigh,
where it fuses with the deep fascia
one fingerbreadth below the
inguinal ligament.
Arrangement of the fatty layer and the
membranous layer of the superficial fascia
in the lower part of the anterior abdominal
wall. Note the line of fusion between the
membranous layer and the deep fascia of the
thigh (fascia lata).
In the midline inferiorly, the
membranous layer of fascia is not
attached to the pubis but forms a
tubular sheath for the penis (or
clitoris). Below in the perineum, it
enters the wall of the scrotum (or
labia majora). From there it passes to
be attached on each side to the
margins of the pubic arch; it is here
referred to as Colles' fascia.
Posteriorly, it fuses with the perineal
body and the posterior margin of the
perineal membrane.
In the scrotum, the fatty layer of
the superficial fascia is represented
as a thin layer of smooth muscle, the
dartos muscle. The membranous
layer of the superficial fascia persists
as a separate layer.
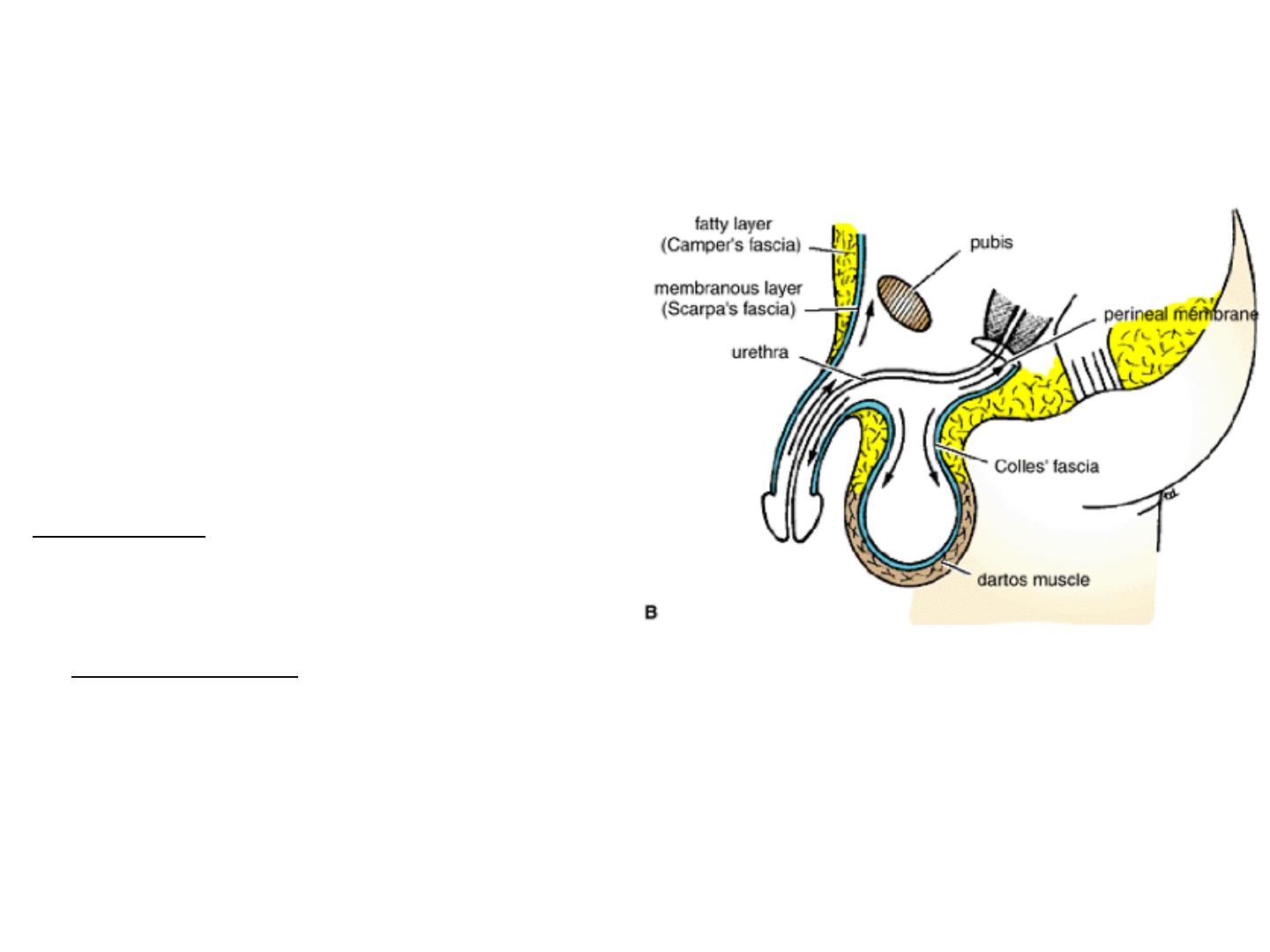
Note the attachment of the
membranous layer to the posterior
margin of the perineal membrane.
Arrows indicate paths taken by
urine in cases of ruptured urethra.
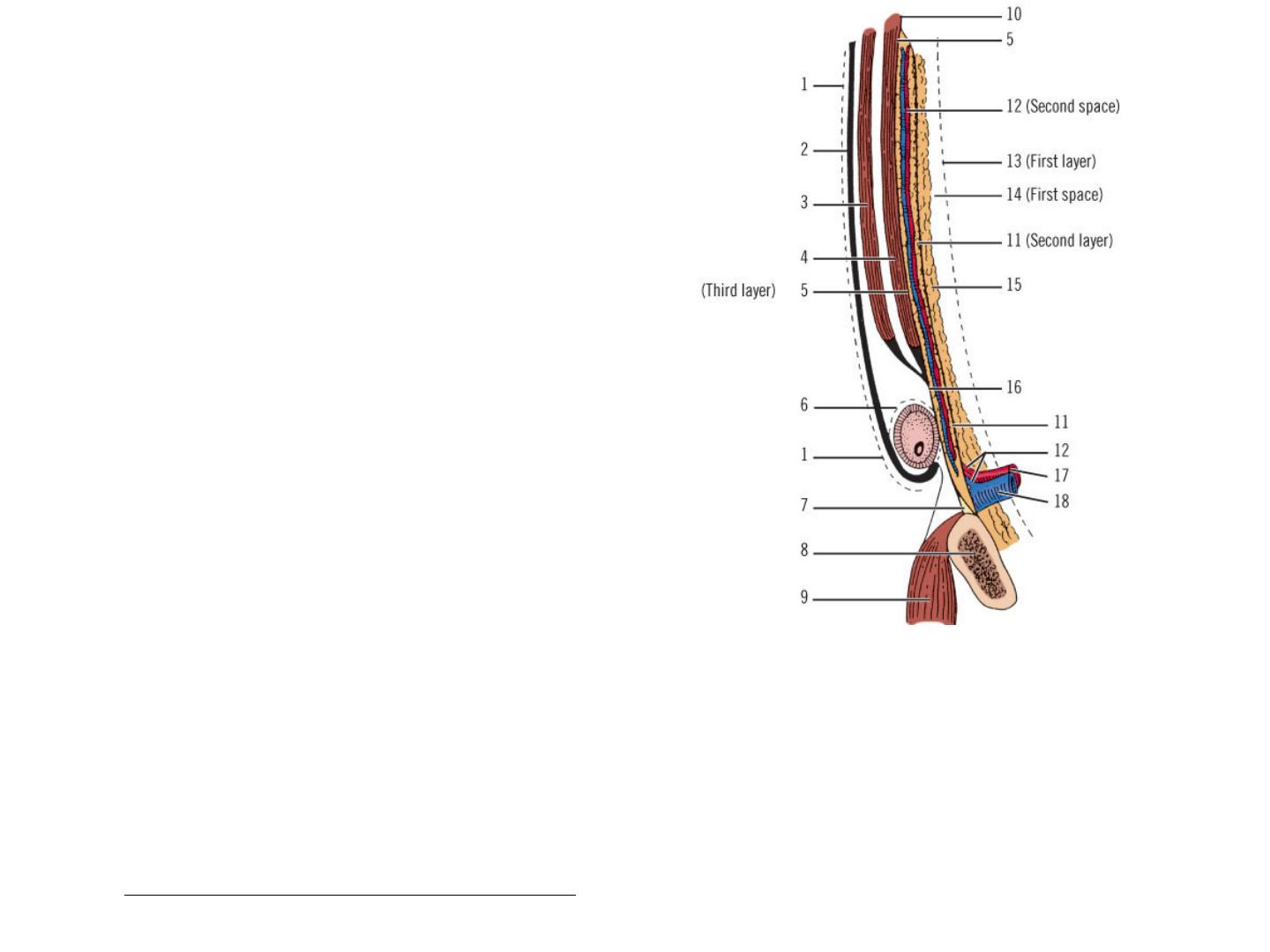
Spaces and Fossae
Space of Bogros
Fat and other connective tissue, either
thick or thin, lies within a space between
the peritoneum and the posterior lamina
of the transversalis fascia that is called the
space of Bogros. A triangular space with
the following boundaries:
Lateral: Iliac fascia
Anterior: Transversalis fascia
Medial: Parietal peritoneum
Highly diagrammatic representation of the layers of the abdominal wall and inguinal area. 1,
External oblique fascia (fascia of Gallaudet); 2, External oblique aponeurosis; 3, Internal
oblique muscle; 4, Transversus abdominis muscle and its aponeurosis; 5, Transversalis fascia
anterior lamina (third layer); 6, External spermatic fascia; 7, Cooper's ligament; 8, Pubic bone;
9, Pectineus muscle; 10, Possible union of transversalis fascia laminae; 11, Transversalis
fascia posterior lamina (second layer); 12, Vessels (second space); 13, Peritoneum (first
layer); 14, Space of Bogros (first space); 15, Preperitoneal fat; 16, Transversus abdominis
aponeurosis and anterior lamina of transversalis fascia; 17, Femoral artery; 18, Femoral vein.

Superficial Perineal Cleft
This potential space lies between Colles' membranous fascia of
the perineum and the muscle fascia of the superficial perineal
pouch. The superficial pouch contains the ischiocavernosus
and bulbospongiosus muscles and erectile bodies, etc. The
superficial pouch covers the more deeply situated urogenital
diaphragm. The superficial perineal cleft is present in the
scrotum or the labia majora and is continuous with the
potential space deep to the fascia of Scarpa of the anterior
abdominal wall.
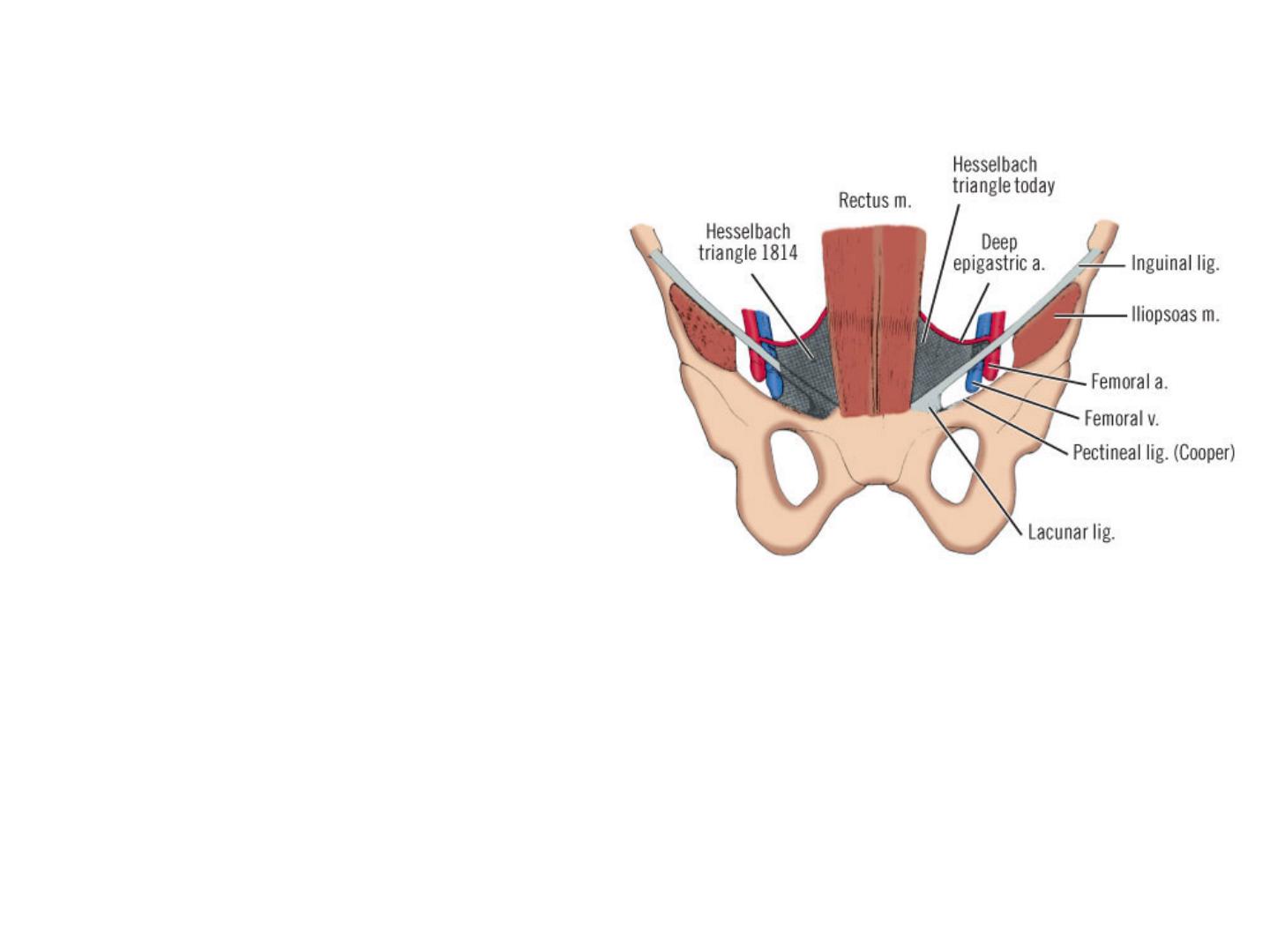
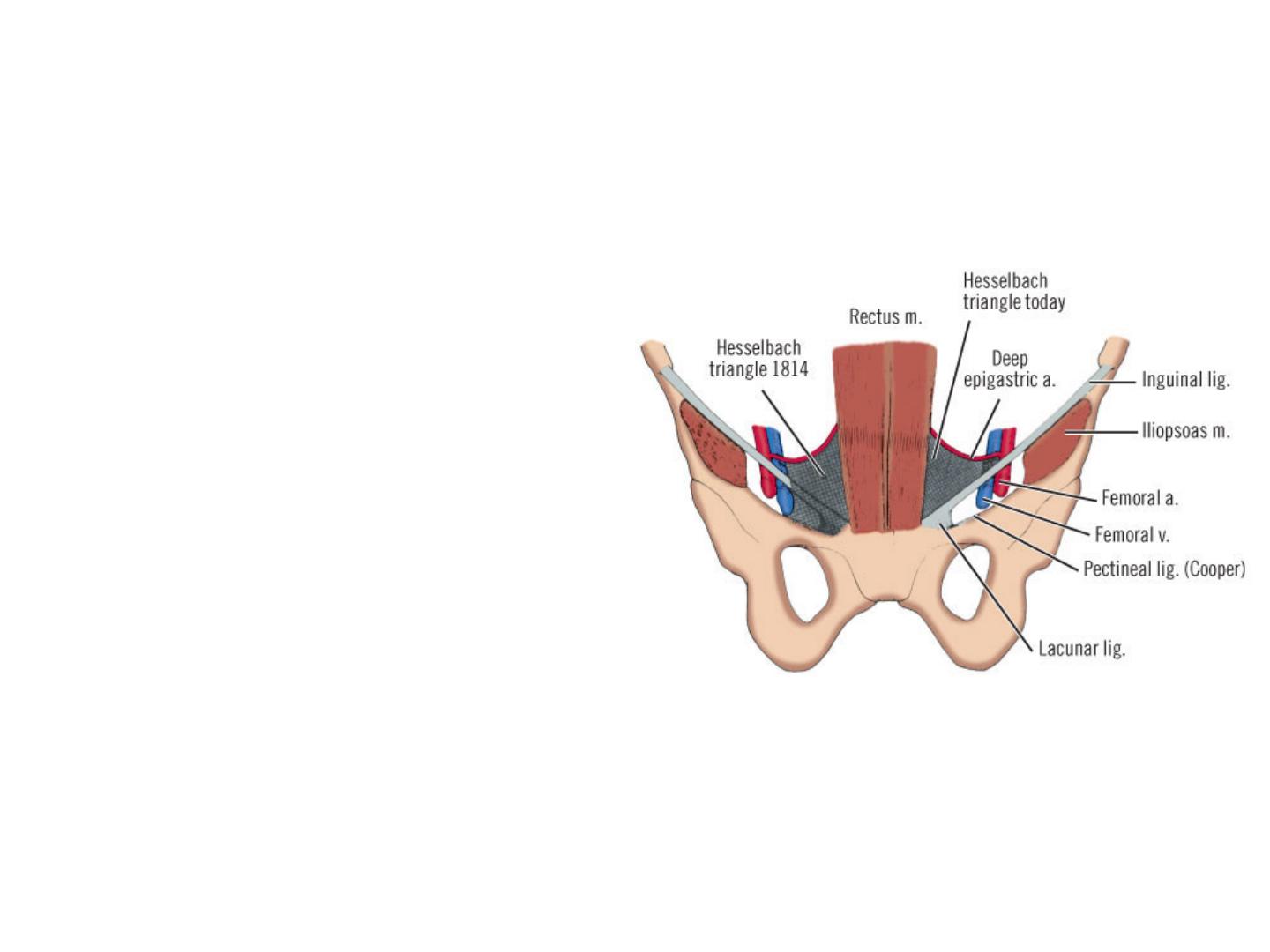
Hesselbach's Triangle
Hesselbach's triangle is
defined as having the
inferior (deep) epigastric
vessels as its superior or
lateral border, the lateral
edge of the rectus
abdominis muscle as its
medial border, and the
inguinal ligament as its
inferolateral border.
Most direct inguinal
hernias and external
supravesical inguinal
hernias occur in this area.
Hesselbach triangle as originally described
(left) and as accepted today (right). Note
that part of supravesical fossa lies within
triangle.
Fossae of the Lower Anterior
Abdominal Wall
The posterior surface of the
anterior abdominal wall above
the inguinal ligament is divided
into three shallow fossae.
Located on either side of the
midline, these fossae are
marked by the obliterated
embryonic urachus, extending
from the dome of the bladder to
the umbilicus (median
umbilical ligament). Laterally,
the fossae are separated by the
medial umbilical ligaments
(obliterated umbilical arteries)
and the lateral umbilical
ligaments (inferior or deep
epigastric arteries).
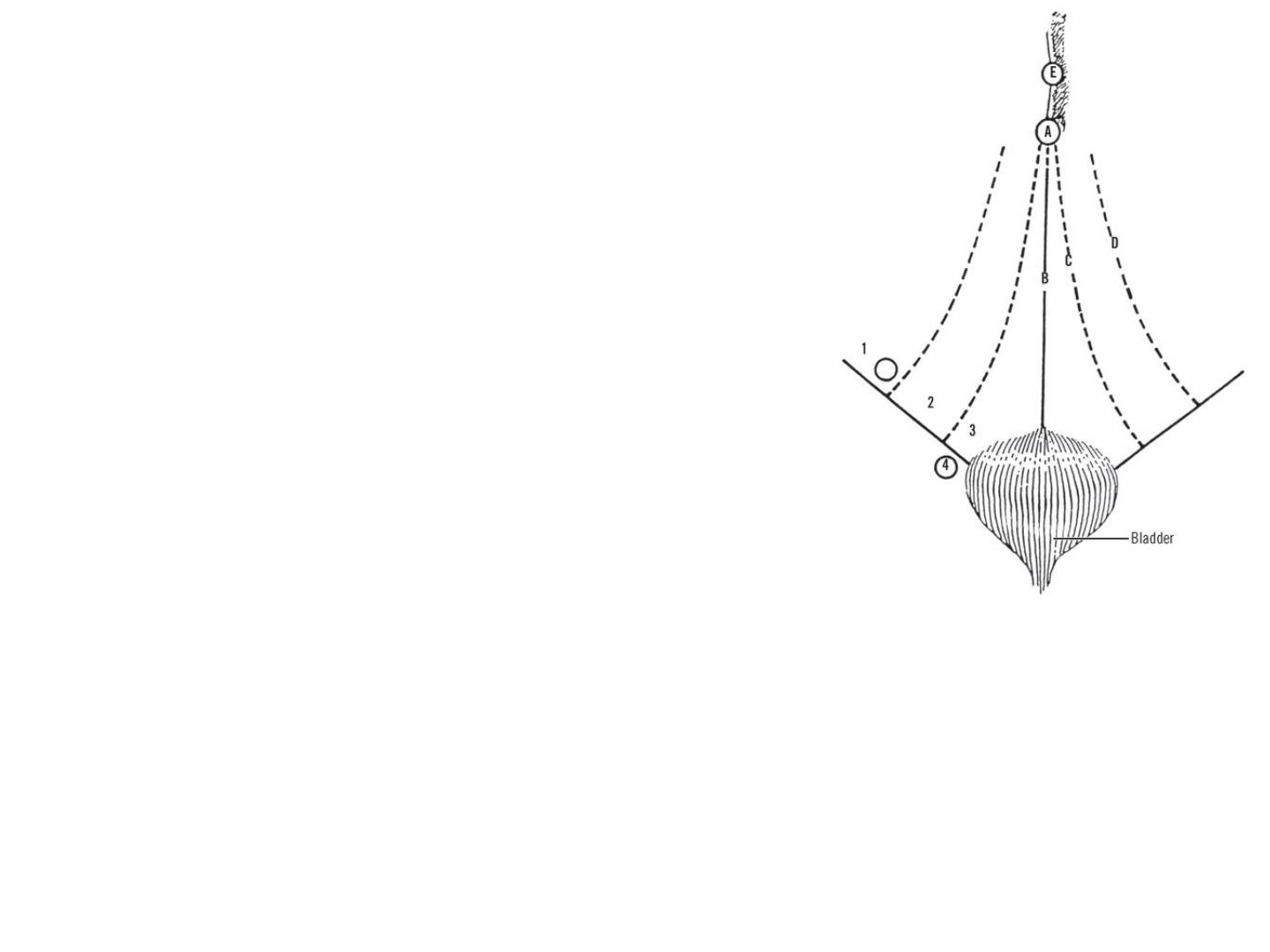
Fossae of anterior abdominal wall and their
relation to sites of groin hernias. A, Umbilicus.
B, Median umbilical ligament (obliterated
urachus). C, Medial umbilical ligament
(obliterated umbilical arteries). D, Lateral
umbilical ligament containing inferior (deep)
epigastric arteries. E, Falciform ligament.
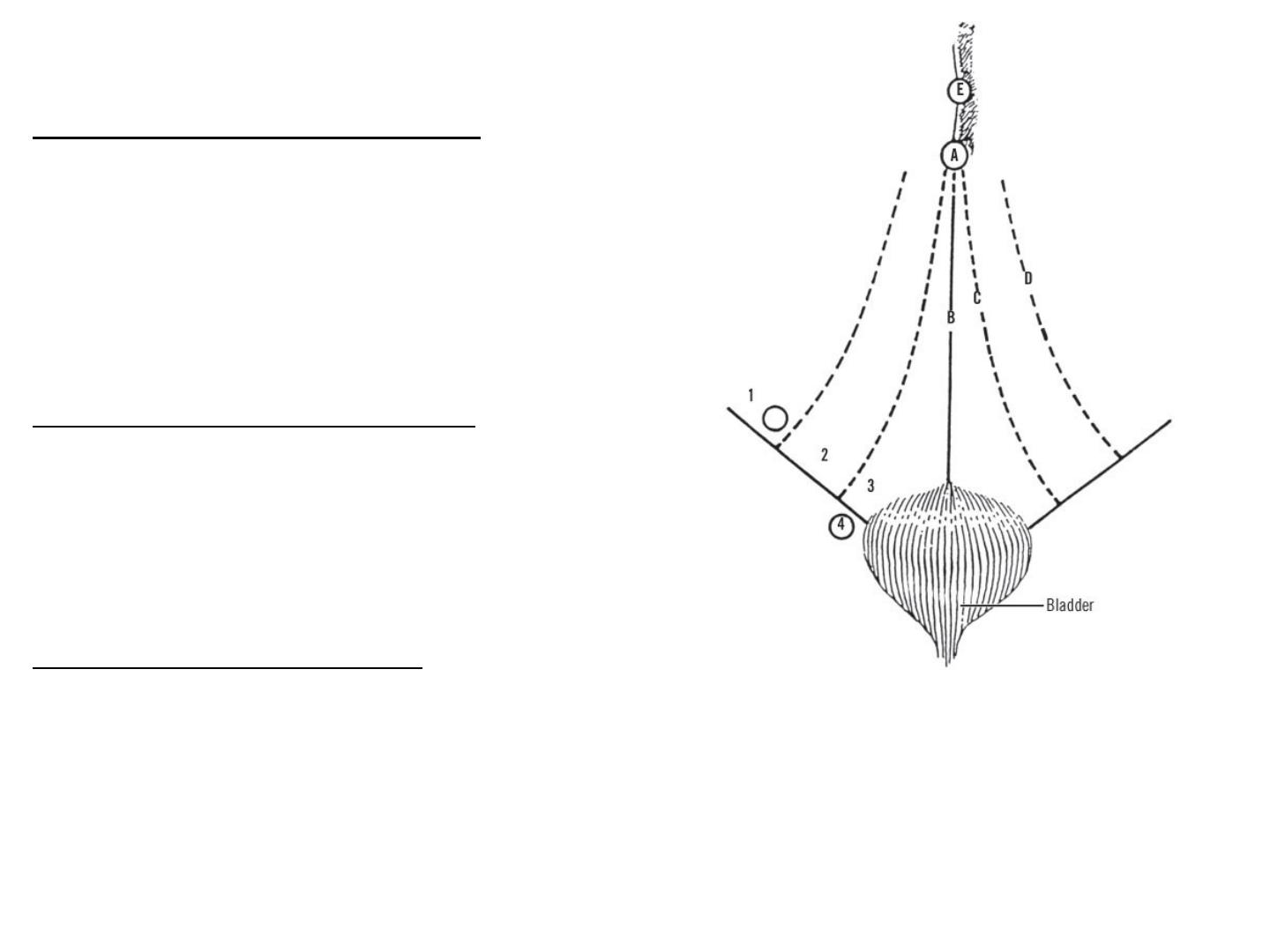
The fossae are as follows:
The lateral inguinal fossae ,
lateral to the inferior epigastric
arteries, contain the internal
inguinal rings. They are the
site of indirect inguinal
hernias.
The medial inguinal fossae,
between the inferior epigastric
arteries and the medial
umbilical ligaments, are the
site of direct inguinal hernias.
The supravesical fossae,
between the medial and
median umbilical ligaments,
are the site of external
supravesical hernias.
Sites of possible hernias: 1, Lateral fossa
(indirect inguinal hernia); 2, Medial fossa
(direct inguinal hernia); 3, Supravesical fossa
(supravesical hernia); 4, Femoral ring (femoral
hernia).
Spaces between the Inguinal Ligament and the Iliopectineal Line
Between the inguinal ligament and the
superior pubic ramus is a space organized
into three compartments: neuromuscular,
vascular, and femoral canal. The most
lateral of these is the neuromuscular. This
area contains the iliopsoas muscle, the
femoral nerve, and the lateral femoral
cutaneous nerve.
The femoral nerve may pierce the iliacus
muscle. It may be found between the
femoral artery and vein. Part of the nerve
may be a fellow traveler with the superior
gluteal nerve to supply the rectus femoris
and vastus lateralis. Or the femoral nerve
may be found deep in the iliacus muscle.
Medial to the area containing the iliopsoas
muscle, the femoral nerve, and the lateral
femoral cutaneous nerve is the vascular
compartment which contains the femoral
artery and vein.
Clinical Notes
Membranous Layer of Superficial Fascia and the Extravasation of
Urine
The membranous layer of the superficial fascia is important clinically because
beneath it is a potential closed space that does not open into the thigh but is
continuous with the superficial perineal pouch via the penis and scrotum. Rupture
of the penile urethra may be followed by extravasation of urine into the scrotum,
perineum, and penis and then up into the lower part of the anterior abdominal
wall deep to the membranous layer of fascia. The urine is excluded from the thigh
because of the attachment of the fascia to the fascia lata.
Deep Fascia
The deep fascia in the anterior abdominal wall is merely a thin layer of
connective tissue covering the muscles; it lies immediately deep to the
membranous layer of superficial fascia.
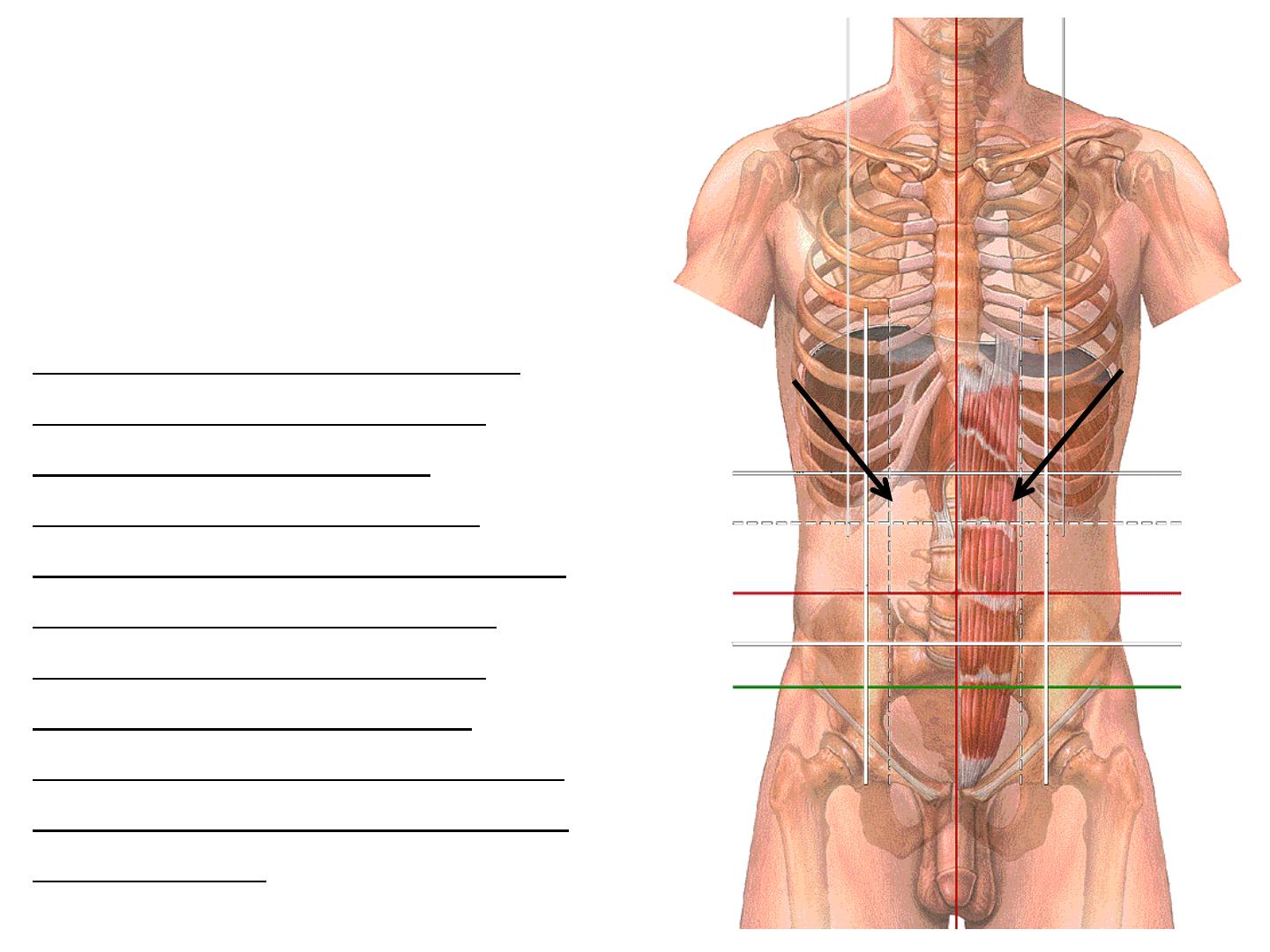
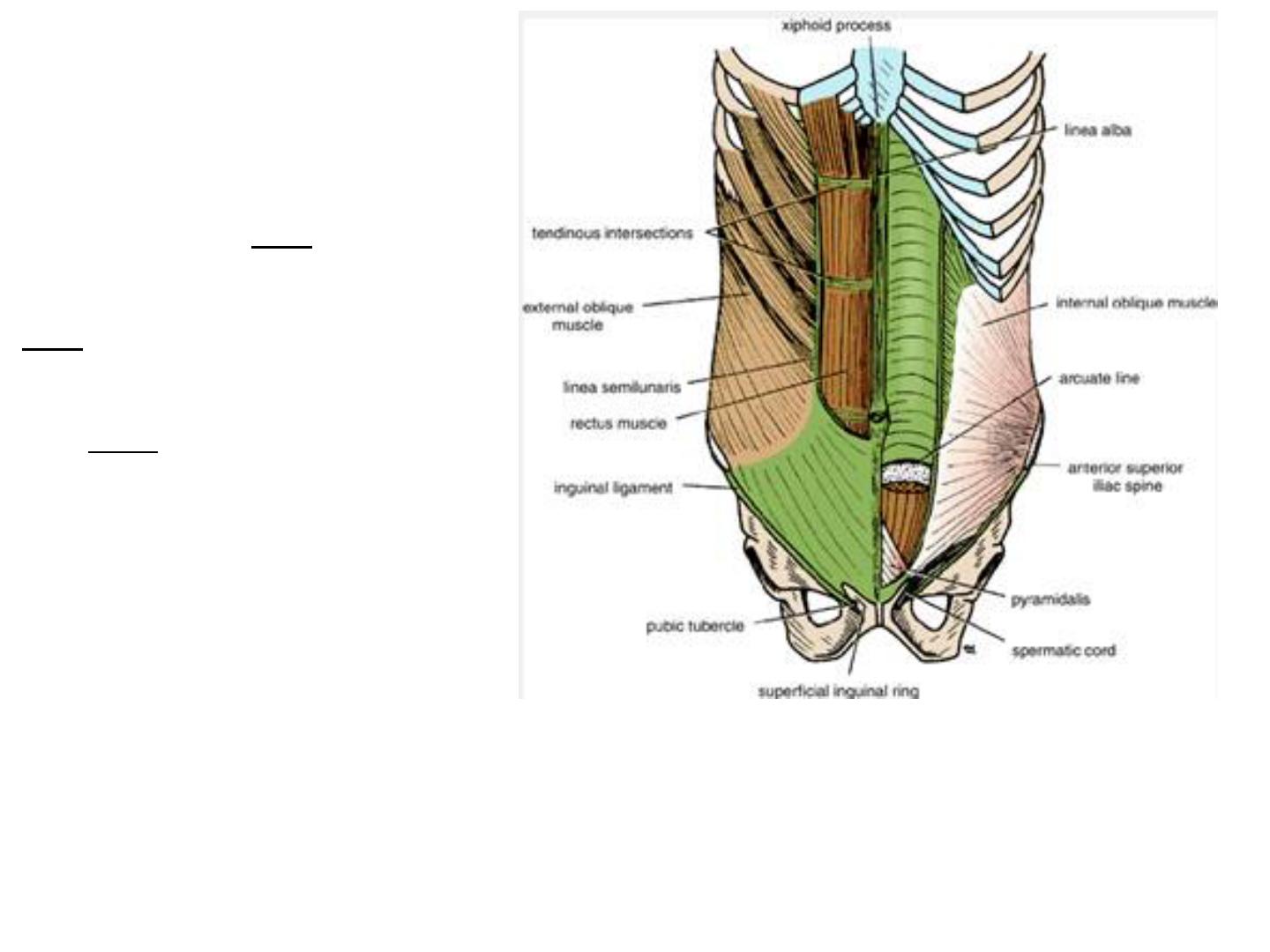
● Muscle arrangements
Muscles of the Anterior
Abdominal Wall
The muscles of the
anterior abdominal wall
consist of three broad thin
sheets that are aponeurotic
in front; from exterior to
interior they are
the external oblique,
internal oblique, and
transversus.
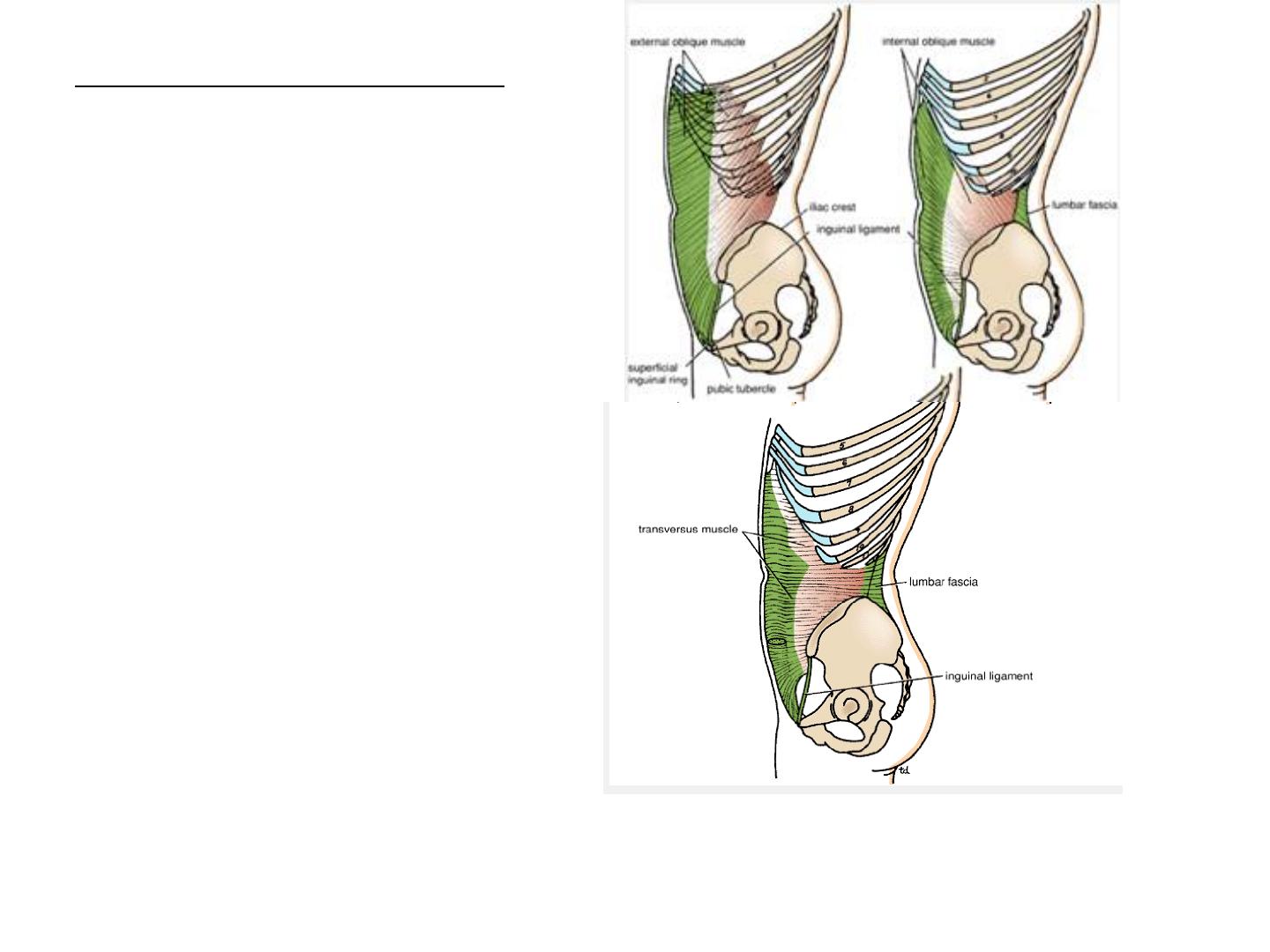
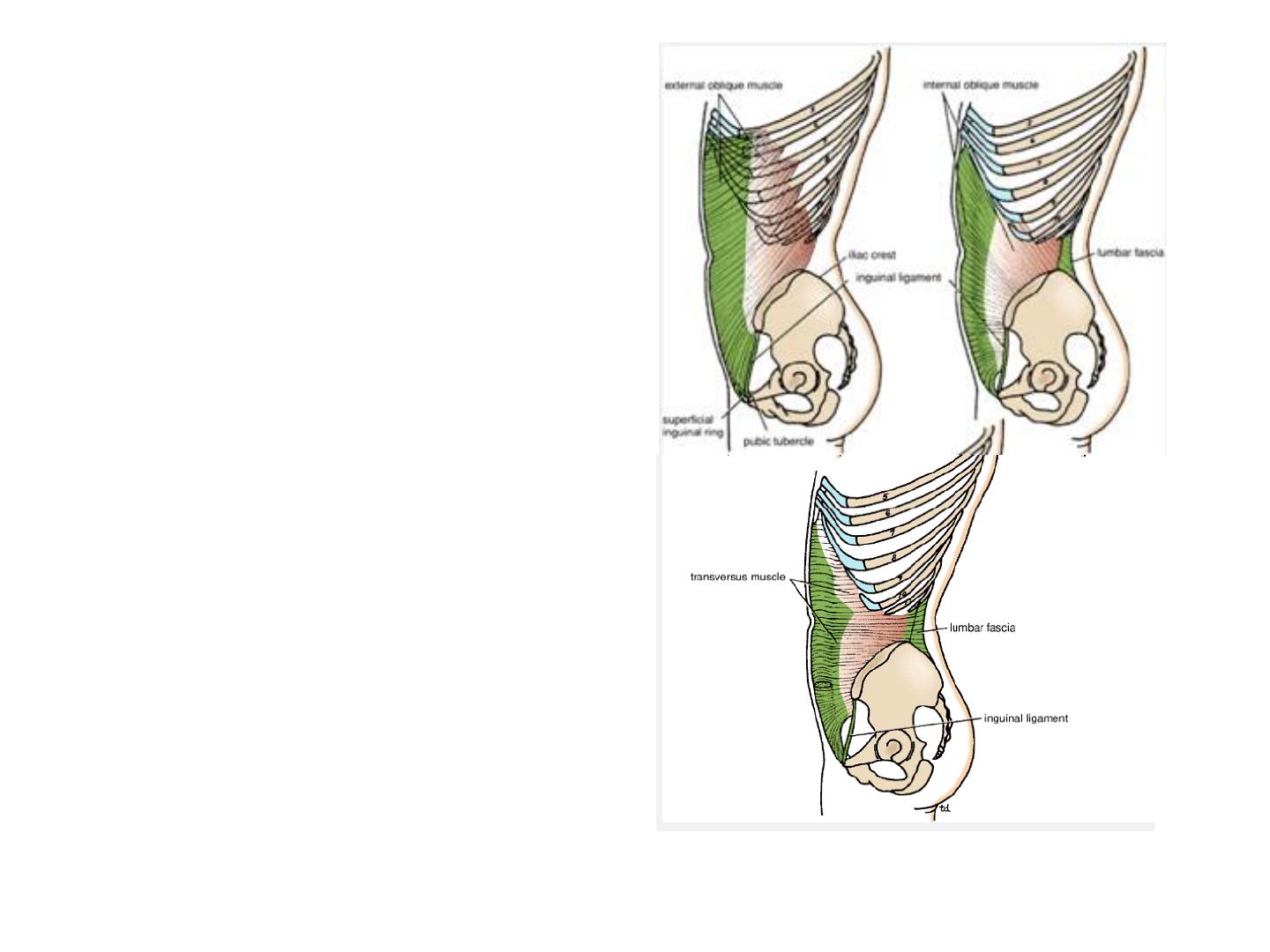
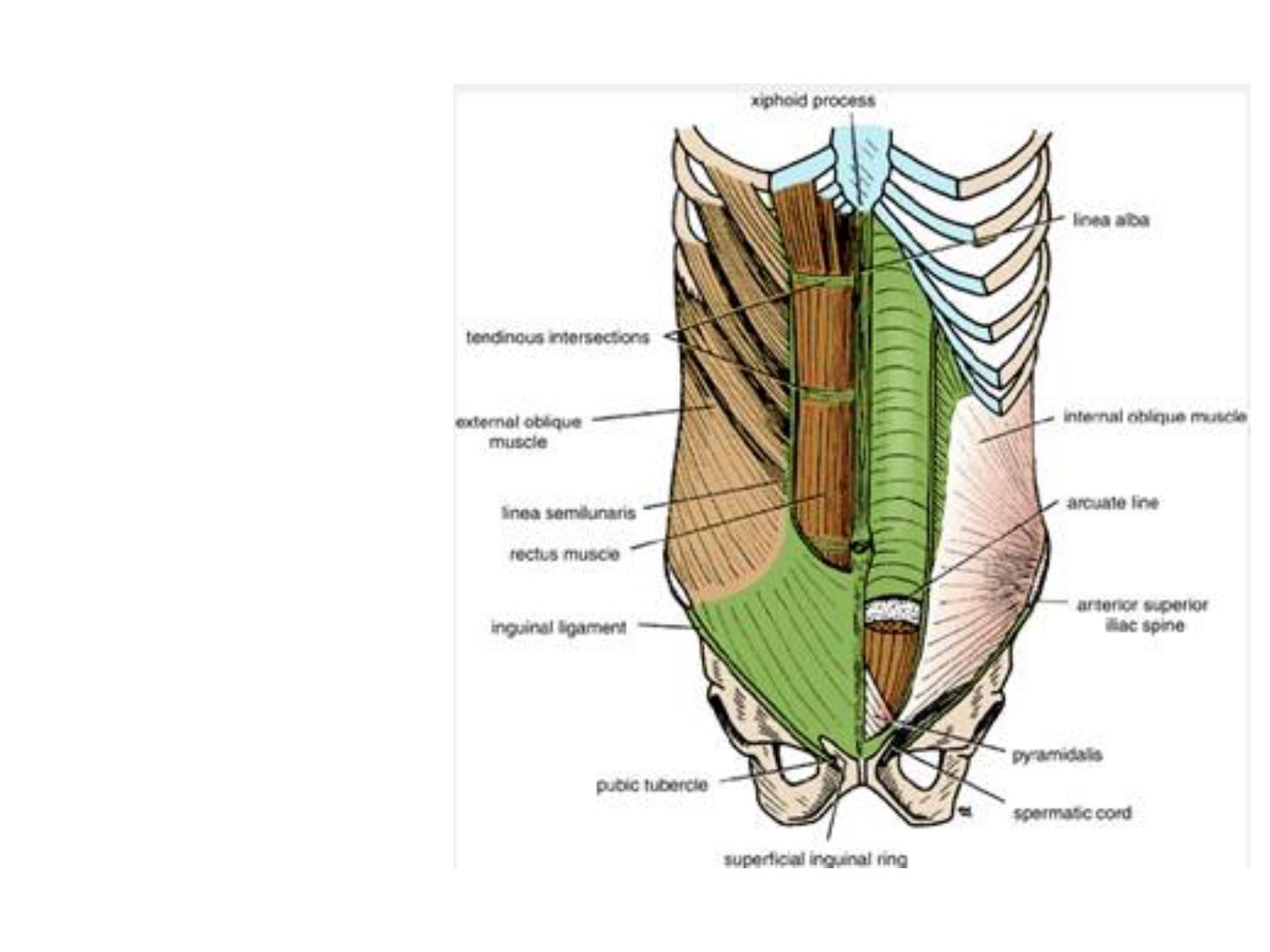
External oblique, internal oblique, and transversus
muscles of the anterior abdominal wall.
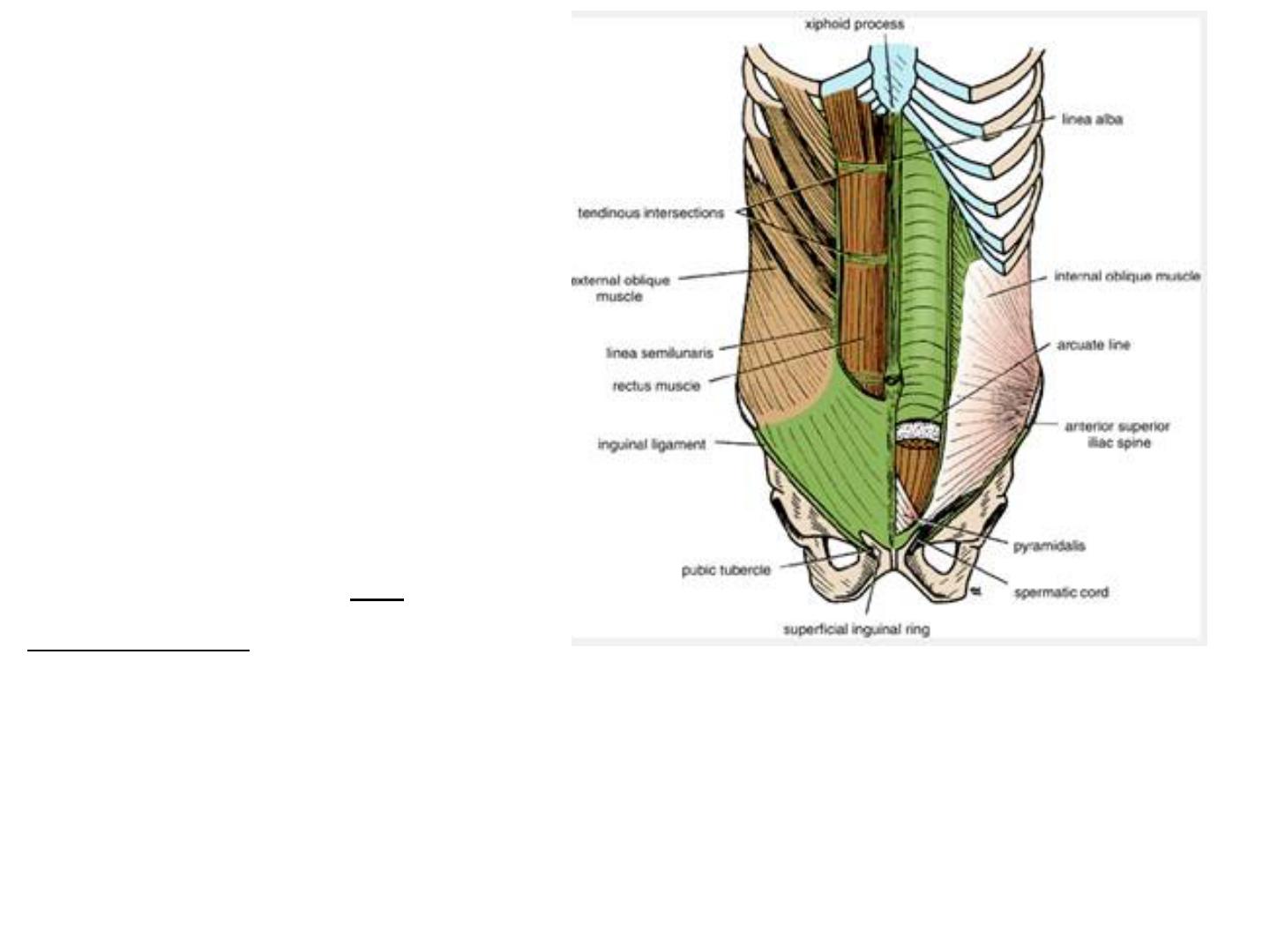
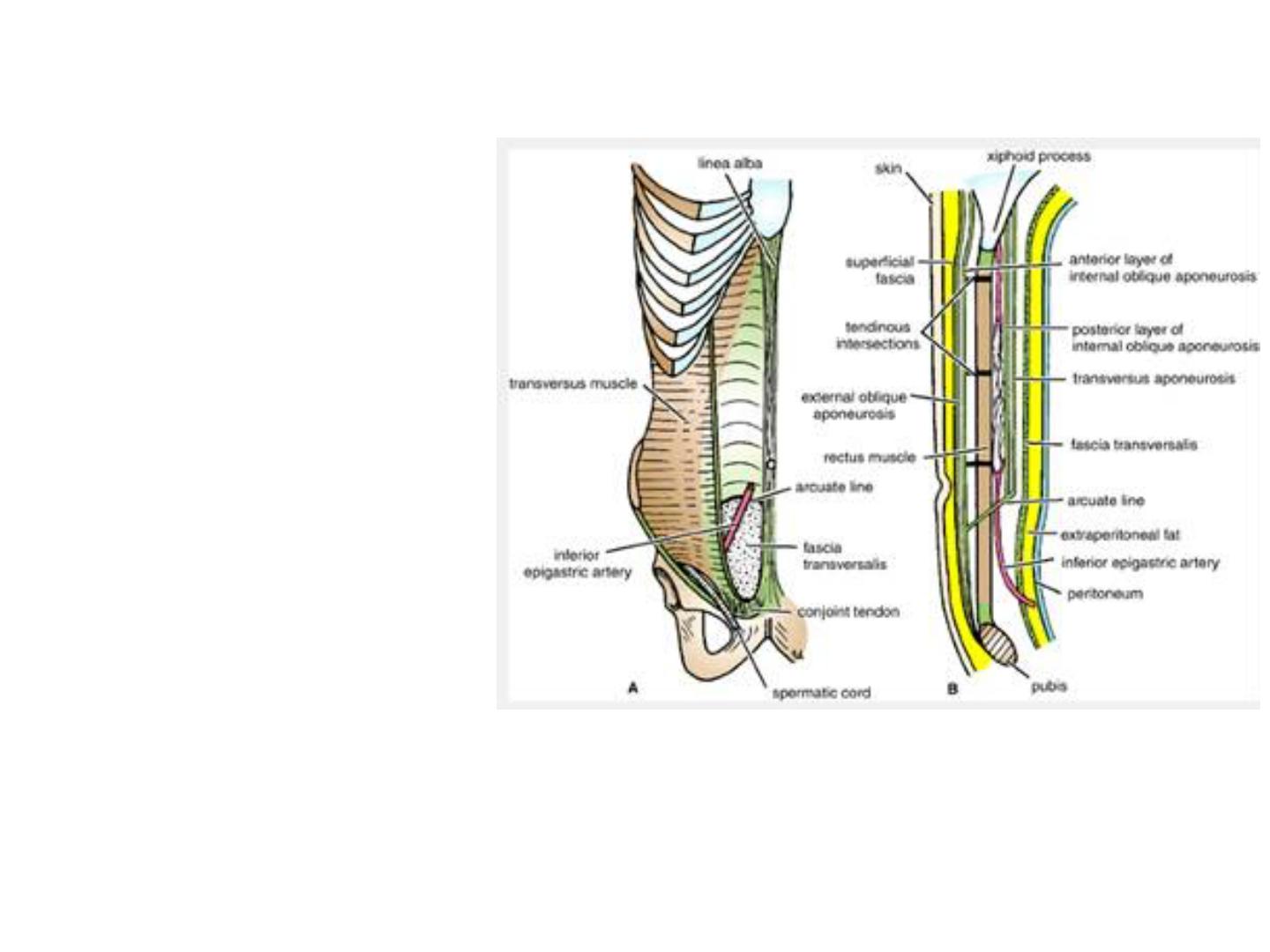
Muscles of the Anterior
Abdominal Wall
On either side of the
midline anteriorly is, in
addition, a wide vertical
muscle, the rectus
abdominis. As the
aponeuroses of the three
sheets pass forward, they
enclose the rectus
abdominis to form the
rectus sheath. The lower
part of the rectus sheath
might contain a small
muscle called the
pyramidalis.
Anterior view of the rectus abdominis muscle and
the rectus sheath. Left: The anterior wall of the
sheath has been partly removed, revealing the
rectus muscle with its tendinous intersections.
Right: The posterior wall of the rectus sheath is
shown. The edge of the arcuate line is shown at
the level of the anterior superior iliac spine.
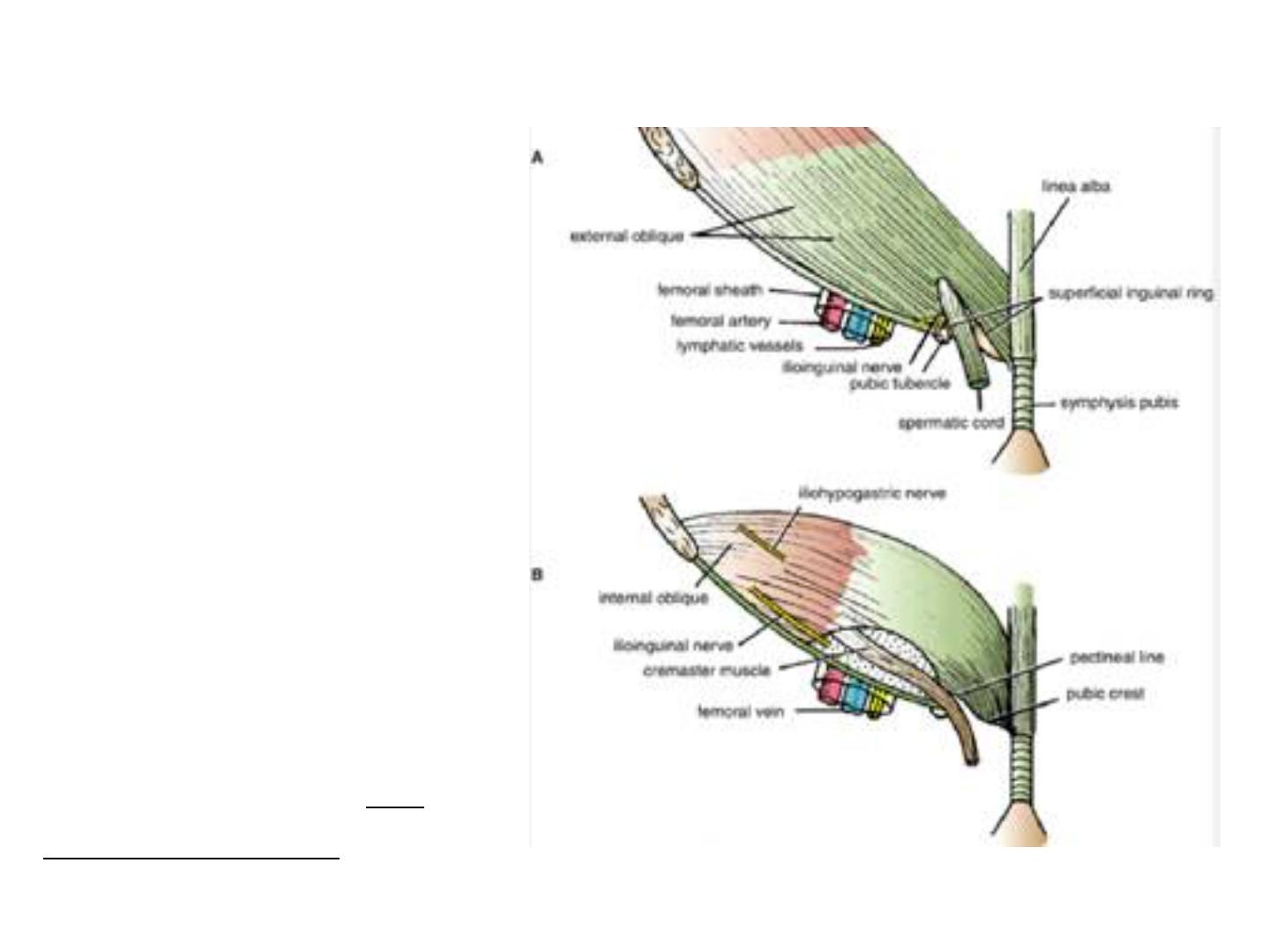
External Oblique
The external oblique
muscle is a broad,
thin, muscular sheet
that arises from the
outer surfaces of
the lower eight ribs
and fans out to be
inserted into the
xiphoid process, the
linea alba, the pubic
crest, the pubic
tubercle, and the
anterior half of the
iliac crest.
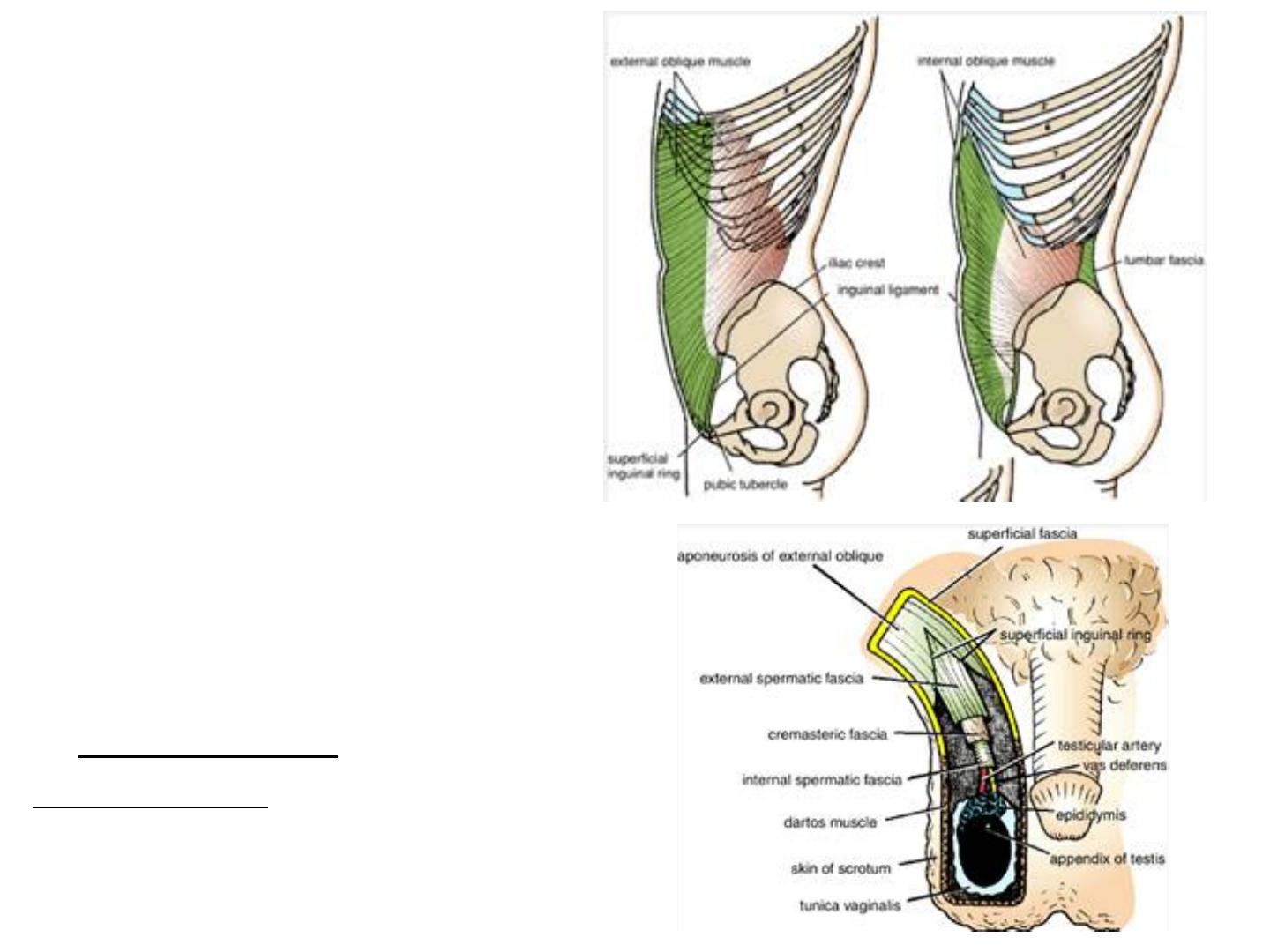
•
Double click to add text
Most of the fibers are
inserted by means of a
broad aponeurosis. Note
that the most posterior
fibers passing down to
the iliac crest form a
posterior free border.
A triangular-shaped
defect in the external
oblique aponeurosis lies
immediately above and
medial to the pubic
tubercle. This is known
as the superficial
inguinal ring.
The spermatic cord (or
round ligament of the
uterus) passes through
this opening and
carries the external
spermatic fascia (or
the external covering
of the round ligament
of the uterus) from the
margins of the ring.
Between the anterior
superior iliac spine
and the pubic tubercle,
the lower border of the
aponeurosis is folded
backward on itself,
forming the inguinal
ligament.
From the medial end of
the ligament, the lacunar
ligament extends
backward and upward to
the pectineal line on the
superior ramus of the
pubis.
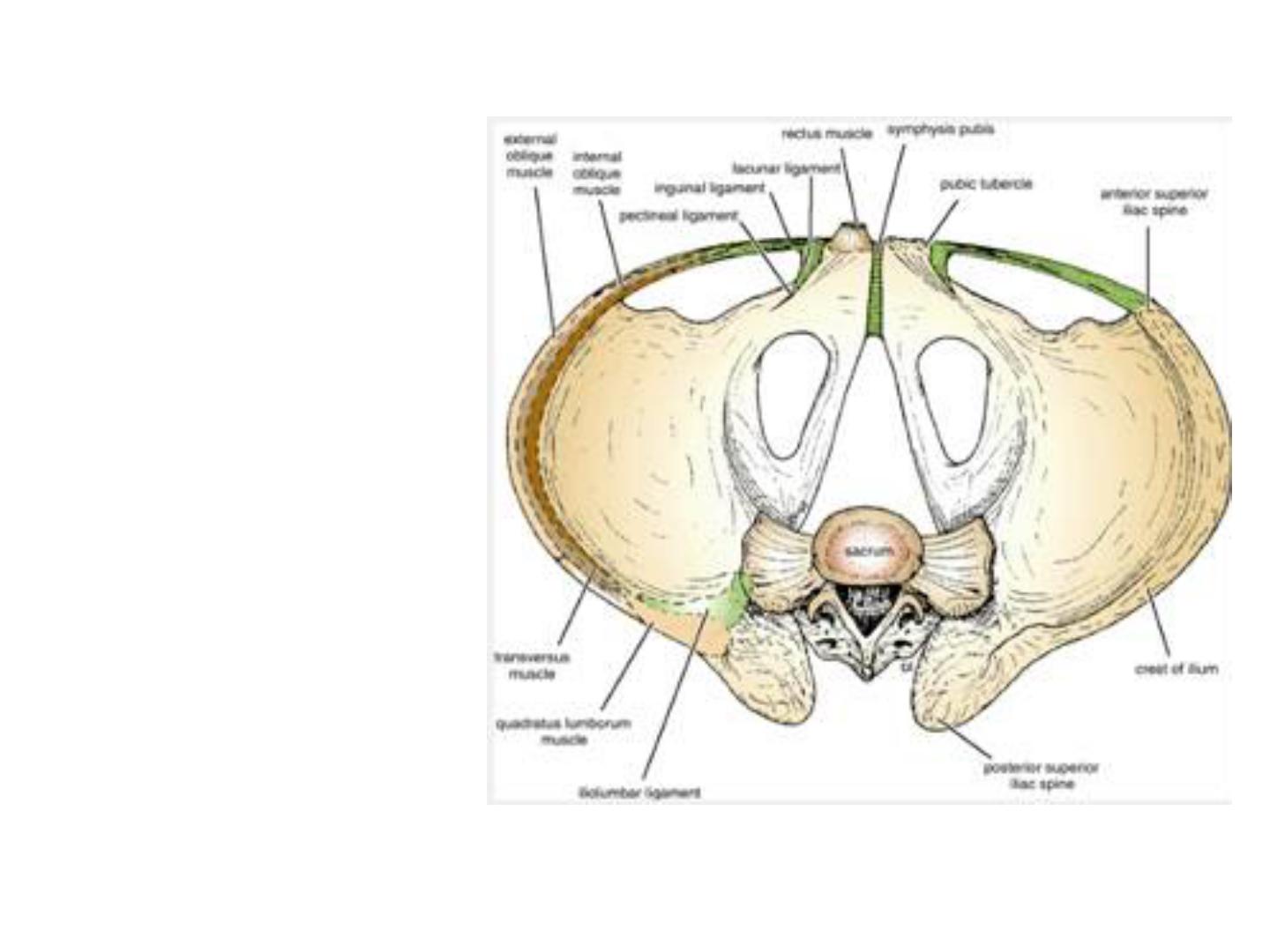
Its sharp, free
crescentic edge
forms the medial
margin of the
femoral ring. On
reaching the
pectineal line, the
lacunar ligament
becomes
continuous with a
thickening of the
periosteum called
the pectineal
ligament.
The lateral part of the
posterior edge of the
inguinal ligament
gives origin to part of
the internal oblique
and transversus
abdominis muscles.
To the inferior
rounded border of the
inguinal ligament is
attached the deep
fascia of the thigh, the
fascia lata.
A. Arrangement of the fatty layer and the
membranous layer of the superficial fascia
in the lower part of the anterior abdominal
wall. Note the line of fusion between the
membranous layer and the deep fascia of the
thigh (fascia lata).
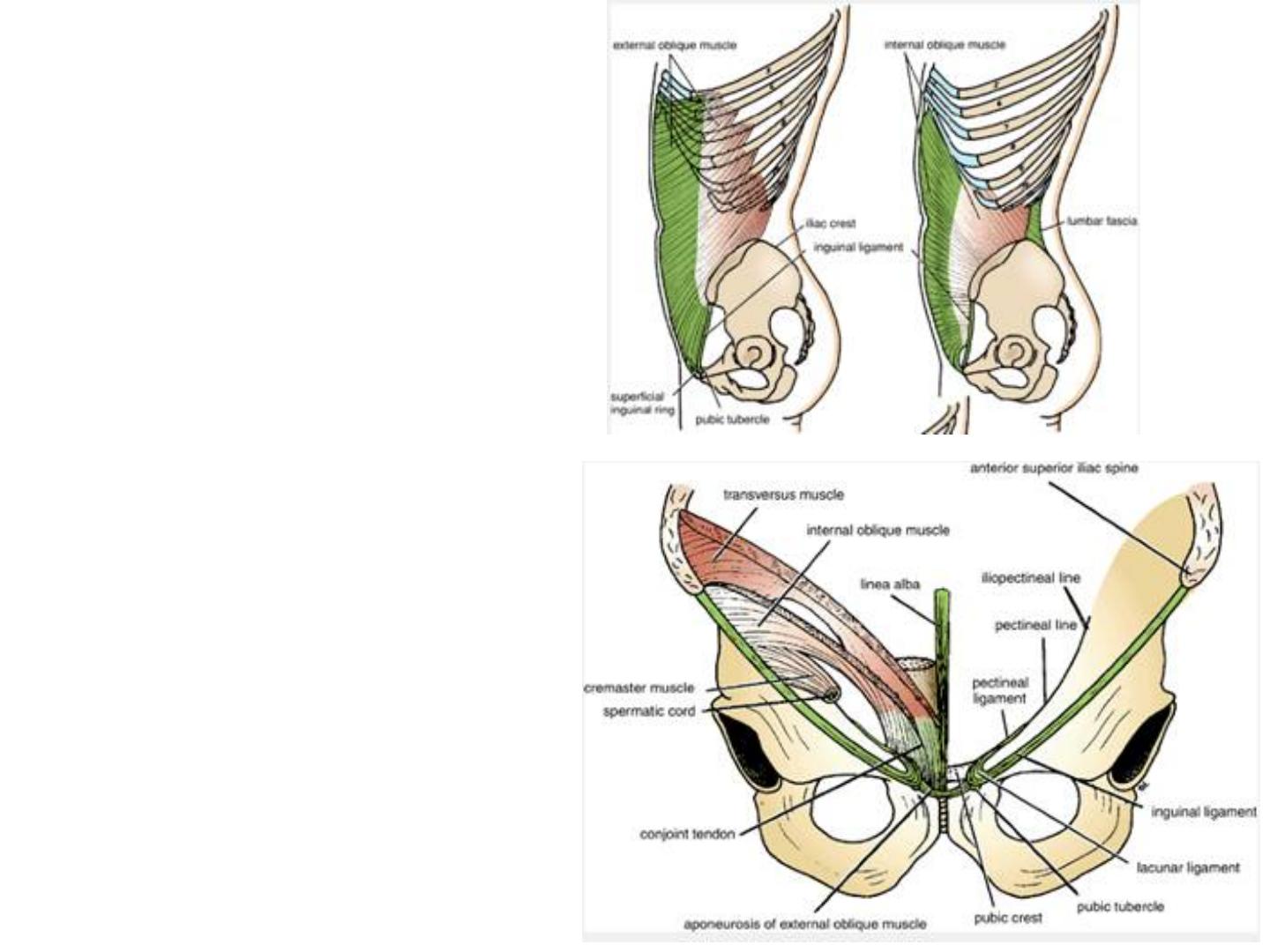
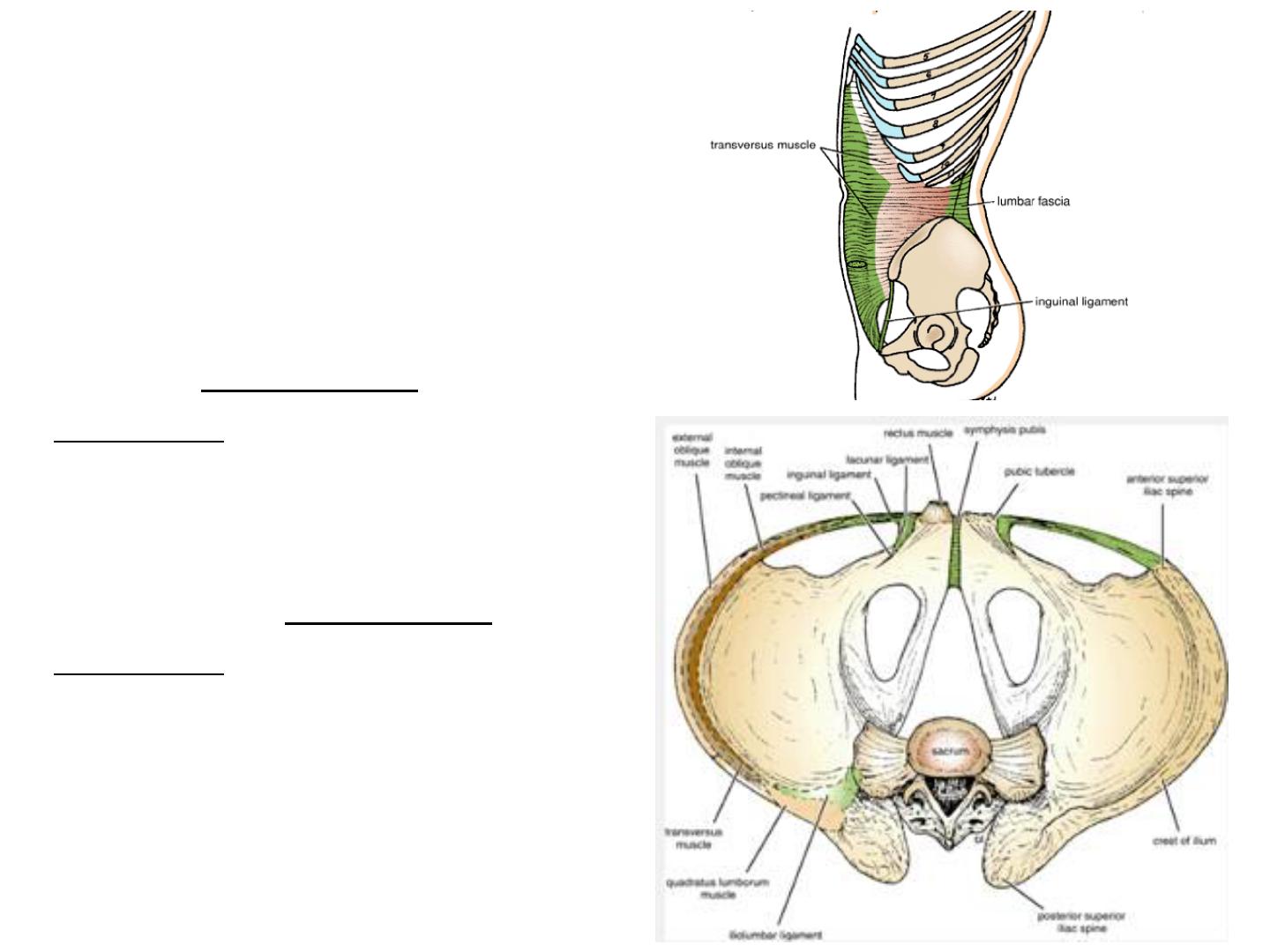
Internal Oblique
The internal oblique muscle is
also a broad, thin, muscular sheet
that lies deep to the external
oblique; most of its fibers run at
right angles to those of the
external oblique.
It arises from the lumbar fascia,
the anterior two thirds of the
iliac crest, and the lateral two
thirds of the inguinal ligament.
The muscle fibers radiate as they
pass upward and forward. The
muscle is inserted into the lower
borders of the lower three ribs
and their costal cartilages, the
xiphoid process, the linea alba,
and the symphysis pubis.
The internal oblique
has a lower free border
that arches over the
spermatic cord (or
round ligament of the
uterus) and then
descends behind it to be
attached to the pubic
crest and the pectineal
line. Near their
insertion, the lowest
tendinous fibers are
joined by similar fibers
from the transversus
abdominis to form the
conjoint tendon.
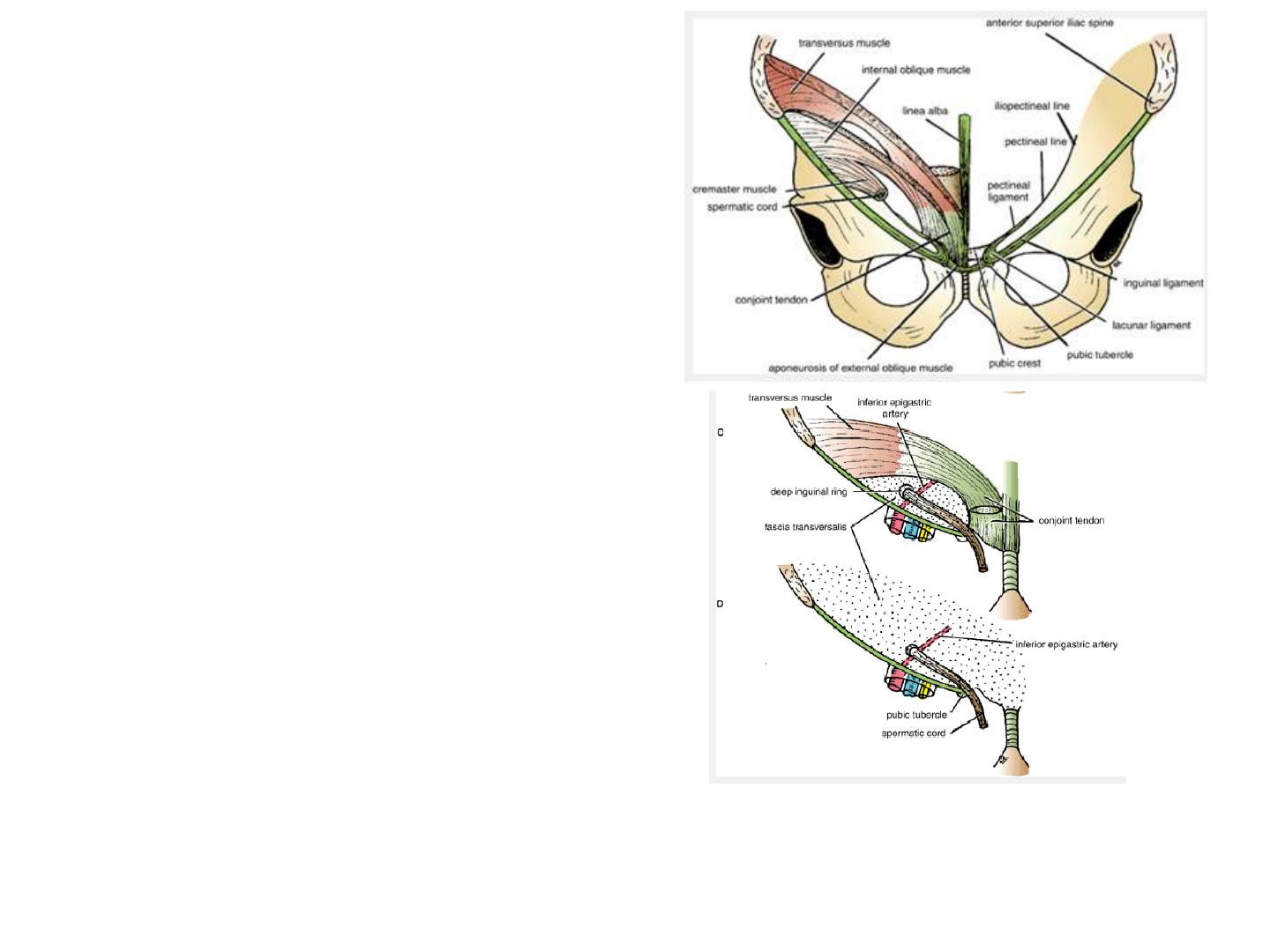
The conjoint tendon is attached
medially to the linea alba, but it
has a lateral free border.
As the spermatic cord (or
round ligament of the uterus)
passes under the lower border of
the internal oblique, it carries
with it some of the muscle fibers
that are called the cremaster
muscle. The cremasteric fascia
is the term used to describe the
cremaster muscle and its fascia.
(D). Note that the anterior wall of the canal is formed by the
external oblique and the internal oblique and the posterior wall is
formed by the fascia transversalis and the conjoint tendon. The
deep inguinal ring lies lateral to the inferior epigastric artery.
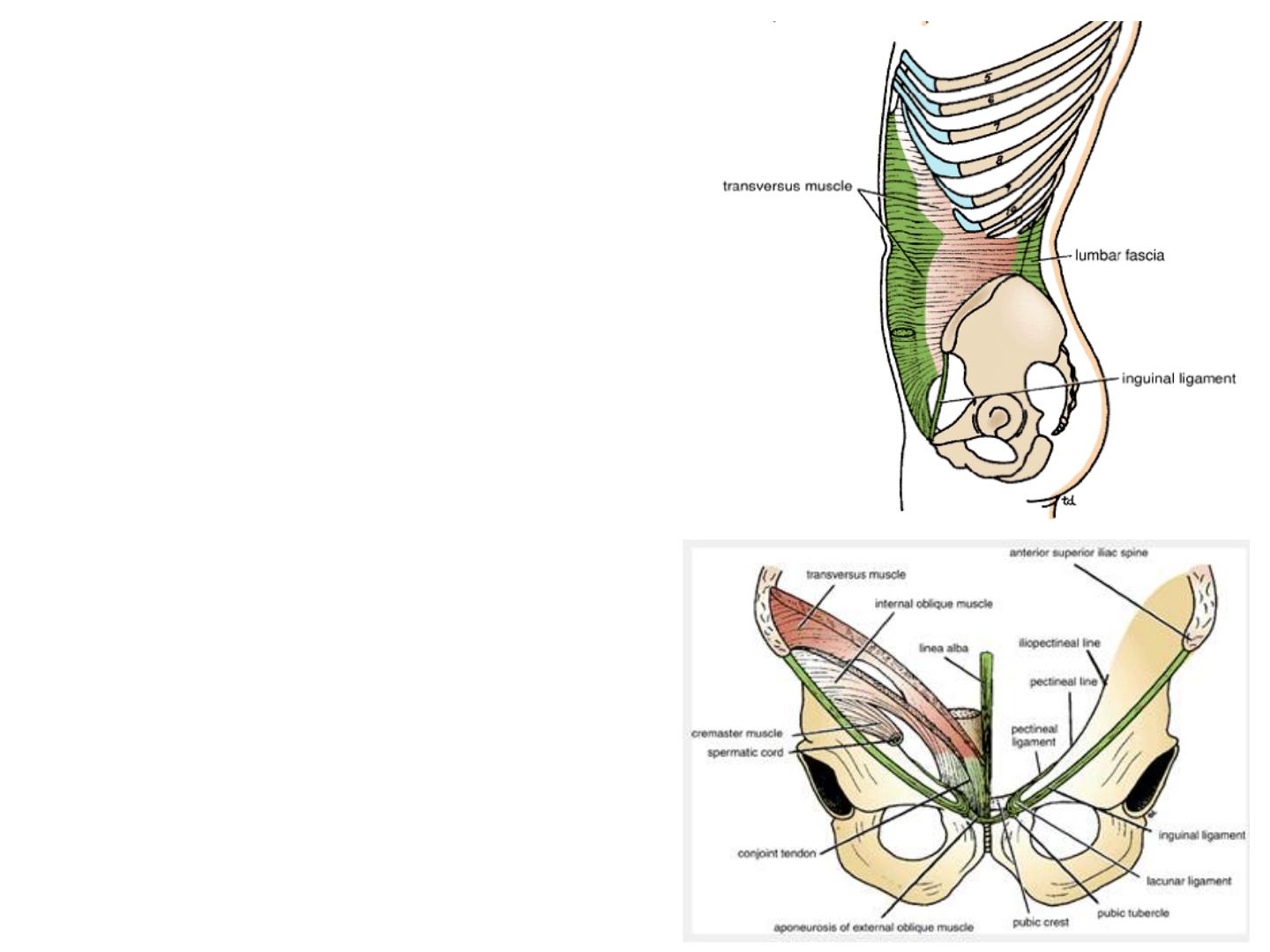
Transversus
The transversus muscle is a thin
sheet of muscle that lies deep to the
internal oblique, and its fibers run
horizontally forward.
It arises from the deep surface of
the lower six costal cartilages
(interdigitating with the
diaphragm), the lumbar fascia,
the anterior two thirds of the
iliac crest, and the lateral third of
the inguinal ligament. It is
inserted into the xiphoid process,
the linea alba, and the symphysis
pubis. The lowest tendinous fibers
join similar fibers from the internal
oblique to form the conjoint
tendon, which is fixed to the pubic
crest and the pectineal line.
Note that the
posterior border
of the external
oblique muscle
is free, whereas
the posterior
borders of the
internal oblique
and transversus
muscles are
attached to the
lumbar
vertebrae by the
lumbar fascia.
Rectus Abdominis
The rectus abdominis is a
long strap muscle that
extends along the whole
length of the anterior
abdominal wall. It is
broader above and lies
close to the midline, being
separated from its fellow
by the linea alba. The
rectus abdominis muscle
arises by two heads, from
the front of the symphysis
pubis and from the pubic
crest.
It is inserted into the fifth,
sixth, and seventh costal
cartilages and the xiphoid
process.
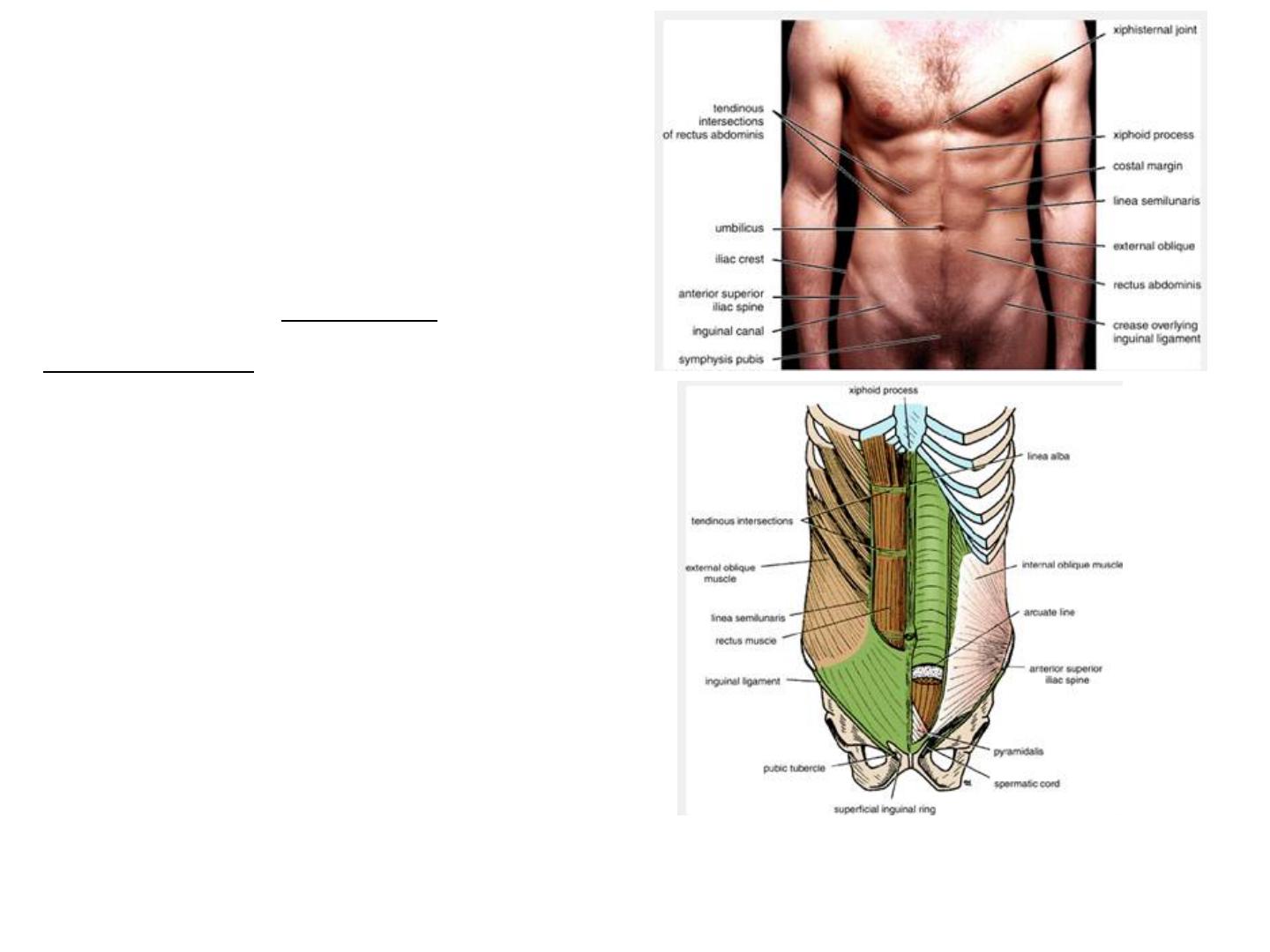
When it contracts, its
lateral margin forms a
curved ridge that can be
palpated and often seen
and is termed the linea
semilunaris. This extends
from the tip of the ninth
costal cartilage to the
pubic tubercle.
Anterior view of the rectus abdominis muscle and the rectus sheath. Left: The anterior wall of
the sheath has been partly removed, revealing the rectus muscle with its tendinous intersections.
Right: The posterior wall of the rectus sheath is shown. The edge of the arcuate line is shown at
the level of the anterior superior iliac spine.
The rectus abdominis
muscle is divided into
distinct segments by three
transverse tendinous
intersections: one at the
level of the xiphoid process,
one at the level of the
umbilicus,
and one halfway between
these two. These
intersections are strongly
attached to the anterior wall
of the rectus sheath. The
rectus abdominis is
enclosed between the
aponeuroses of the external
oblique, internal oblique,
and transversus, which form
the rectus sheath.
Anterior view of the rectus abdominis muscle and the
rectus sheath. Left: The anterior wall of the sheath has
been partly removed, revealing the rectus muscle with
its tendinous intersections. Right: The posterior wall of
the rectus sheath is shown. The edge of the arcuate line
is shown at the level of the anterior superior iliac spine.
Pyramidalis
The pyramidalis
muscle is often
absent. It arises by its
base from the
anterior surface of
the pubis and is
inserted into the linea
alba. It lies in front
of the lower part of
the rectus abdominis.
Nerve Supply of Anterior Abdominal Wall Muscles
The oblique and transversus
abdominis muscles are
supplied by the lower six
thoracic nerves and the
iliohypogastric and
ilioinguinal nerves (L1).
The rectus muscle is
supplied by the lower six
thoracic nerves.
The pyramidalis is supplied
by the 12th thoracic nerve.
Name of Muscle
Origin
Insertion
Nerve Supply
Action
External oblique
Lower eight ribs
Xiphoid process, linea
alba, pubic crest, pubic
tubercle, iliac crest
Lower six thoracic
nerves and
iliohypogastric and
ilioinguinal nerves (L1)
Supports abdominal
contents; compresses
abdominal contents;
assists in flexing and
rotation of trunk; assists
inforced expiration,
micturition, defecation,
parturition, and
vomiting
Internal oblique
Lumbar fascia, iliac crest,
lateral two thirds of
inguinal ligament
Lower three ribs and
costal cartilages, xiphoid
process, linea alba,
symphysis pubis
Lower six thoracic
nerves and
iliohypogastric and
ilioinguinal nerves (L1)
As above
Transversus
Lower six costal
cartilages, lumbar fascia,
iliac crest, lateral third of
inguinal ligament
Xiphoid process linea
alba, symphysis pubis
Lower six thoracic
nerves and
iliohypogastric and
ilioinguinal nerves (L1)
Compresses abdominal
contents
Rectus abdominis
Symphysis pubis and
pubic crest
Fifth, sixth, and seventh
costal cartilages and
xiphoid process
Lower six thoracic
nerves
Compresses abdominal
contents and flexes
vertebral column;
accessory muscle of
expiration
Pyramidalis (if present) Anterior surface of pubis Linea alba
12th thoracic nerve
Tenses the linea alba
Table 4-1 Muscles of the Anterior Abdominal Wall
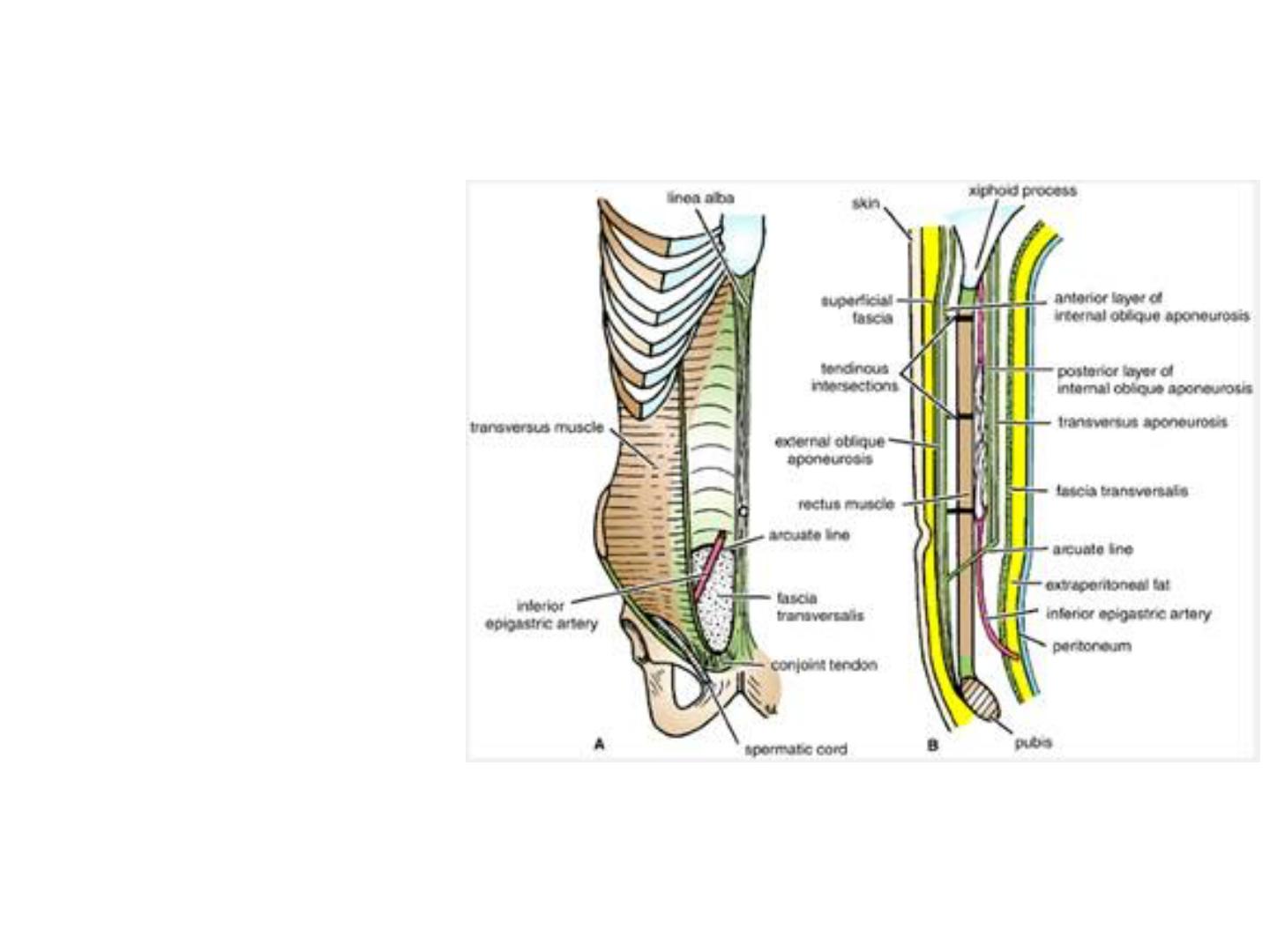
Fascia Transversalis
The fascia transversalis
is a thin layer of fascia
that lines the transversus
abdominis muscle and is
continuous with a
similar layer lining the
diaphragm and the
iliacus muscle.
The femoral sheath
for the femoral vessels
in the lower limbs is
formed from the fascia
transversalis and the
fascia iliaca that covers
the iliacus muscle.
Clinical Notes
Abdominal Muscles, Abdominothoracic Rhythm, and Visceroptosis
The abdominal muscles contract and relax with respiration, and the
abdominal wall conforms to the volume of the abdominal viscera. There
is an abdominothoracic rhythm. Normally, during inspiration, when the
sternum moves forward and the chest expand, the anterior abdominal
wall also moves forward. If, when the chest expands, the anterior
abdominal wall remains stationary or contracts inward, it is highly
probable that the parietal peritoneum is inflamed and has caused a
reflex contraction of the abdominal muscles.
The shape of the anterior abdominal wall depends on the tone of its
muscles. A middle-aged woman with poor abdominal muscles who has
had multiple pregnancies is often incapable of supporting her abdominal
viscera. The lower part of the anterior abdominal wall protrudes
forward, a condition known as visceroptosis. This should not be confused
with an abdominal tumor such as an ovarian cyst or with the excessive
accumulation of fat in the fatty layer of the superficial fascia.
Extraperitoneal Fat
The extraperitoneal
fat is a thin layer of
connective tissue
that contains a
variable amount of
fat and lies
between the fascia
transversalis and
the parietal
peritoneum.
Parietal Peritoneum
The walls of the
abdomen are
lined with
parietal
peritoneum. This
is a thin serous
membrane and is
continuous below
with the parietal
peritoneum lining
the pelvis.
Clinical Notes
Abdominal Pain
Muscle Rigidity and Referred Pain
Sometimes it is difficult for a physician to decide whether the muscles of the
anterior abdominal wall of a patient are rigid because of underlying
inflammation of the parietal peritoneum or whether the patient is voluntarily
contracting the muscles because he or she resents being examined or because
the physician's hand is cold. This problem is usually easily solved by asking the
patient, who is lying supine on the examination table, to rest the arms by the
sides and draw up the knees to flex the hip joints.
A pleurisy involving the lower costal parietal pleura causes pain in the
overlying skin that may radiate down into the abdomen. Although it is unlikely
to cause rigidity of the abdominal muscles, it may cause confusion in making a
diagnosis unless these anatomic facts are remembered.
It is useful to remember the following:
Dermatomes over:
•The xiphoid process: T7
•The umbilicus: T10
•The pubis: L1

Anterior Abdominal Nerve Block
Area of Anesthesia
The area of anesthesia is the skin of the anterior abdominal wall. The nerves of the
anterior and lateral abdominal walls are the anterior rami of the 7th through the 12th
thoracic nerves and the first lumbar nerve (ilioinguinal and iliohypogastric nerves).
Indications
An anterior abdominal nerve block is performed to repair lacerations of the anterior
abdominal wall.
Procedure
The anterior ends of intercostal nerves T7 through T11 enter the abdominal wall by
passing posterior to the costal cartilages. An abdominal field block is most easily
carried out along the lower border of the costal margin and then infiltrating the nerves
as they emerge between the xiphoid process and the 10th or 11th rib along the costal
margin.
The ilioinguinal nerve passes forward in the inguinal canal and emerges through the
superficial inguinal ring. The iliohypogastric nerve passes forward around the
abdominal wall and pierces the external oblique aponeurosis above the superficial
inguinal ring. The two nerves are easily blocked by inserting the anesthetic needle 1 in.
(2.5 cm) above the anterior superior iliac spine on the spinoumbilical line.
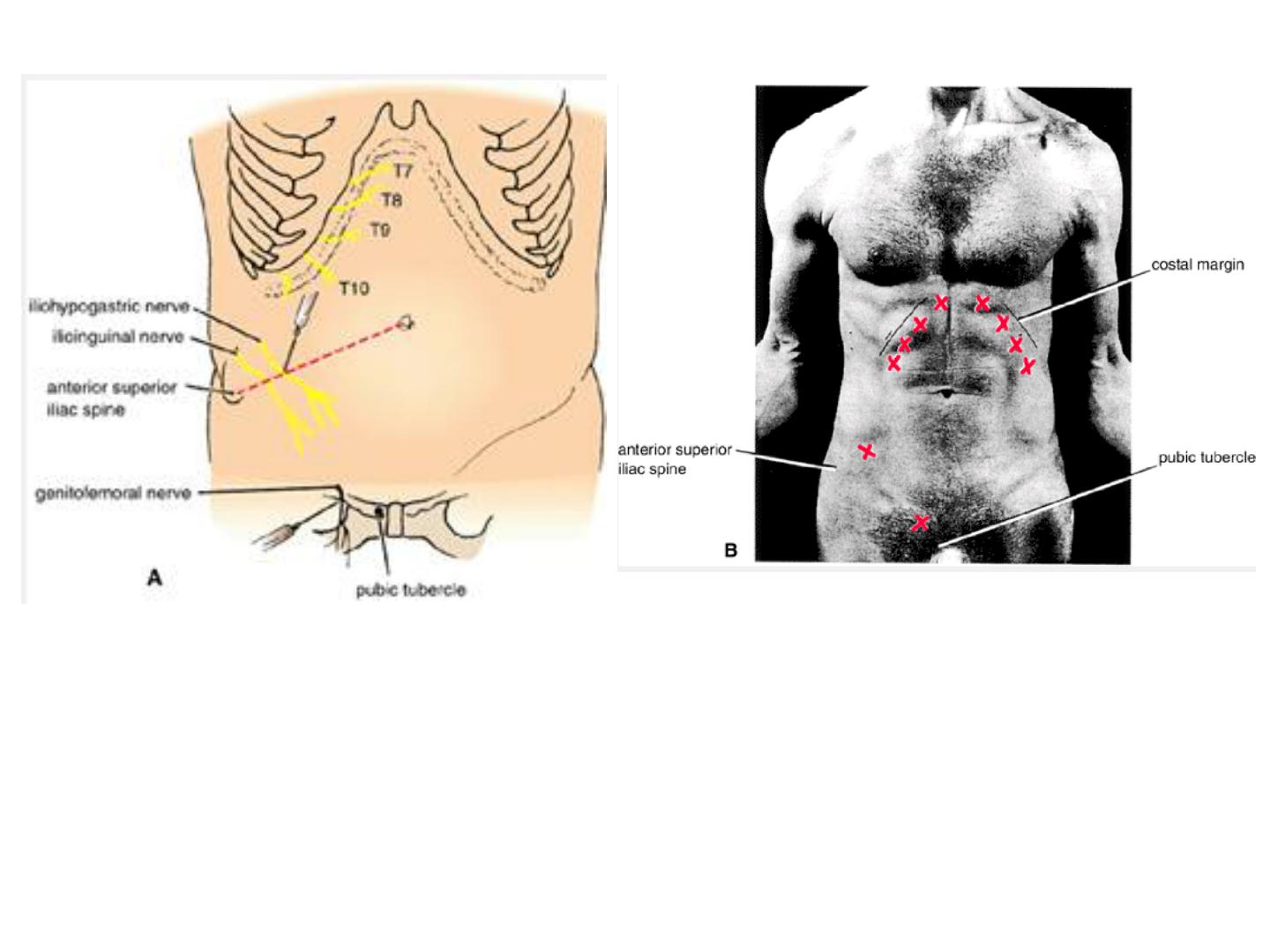
Anterior abdominal wall nerve blocks. T7 though T11 are blocked (X) as they emerge
from beneath the costal margin. The iliohypogastric ilioinguinal nerves are blocked by
inserting the needle about 1 in. (2.5 cm) above the anterior superior iliac spine on the
spinoumbilical line (X). The terminal branches of the genitofemoral nerve are blocked
by inserting the needle through the skin just lateral to the pubic tubercle and infiltrating
the subcutaneous tissue with anesthetic solution (X).
● The neurovascular supply of the anterolateral abdominal wall
The nerves of the anterior
abdominal wall are the anterior
rami of the lower six thoracic
and the first lumbar nerves.
They pass forward in the interval
between the internal oblique and
the transversus muscles. The
thoracic nerves are the lower five
intercostal nerves and the
subcostal nerves, and the first
lumbar nerve is represented by
the iliohypogastric and
ilioinguinal nerves, branches of
the lumbar plexus. They supply
the skin of the anterior
abdominal wall, the muscles, and
the parietal peritoneum.
Dermatomes and distribution of cutaneous
nerves on the anterior abdominal wall.
Nerves of the Anterior Abdominal Wall
The lower six thoracic
nerves pierce the
posterior wall of the
rectus sheath to supply
the rectus muscle and
the pyramidalis (T12
only). They terminate
by piercing the
anterior wall of the
sheath and supplying
the skin.
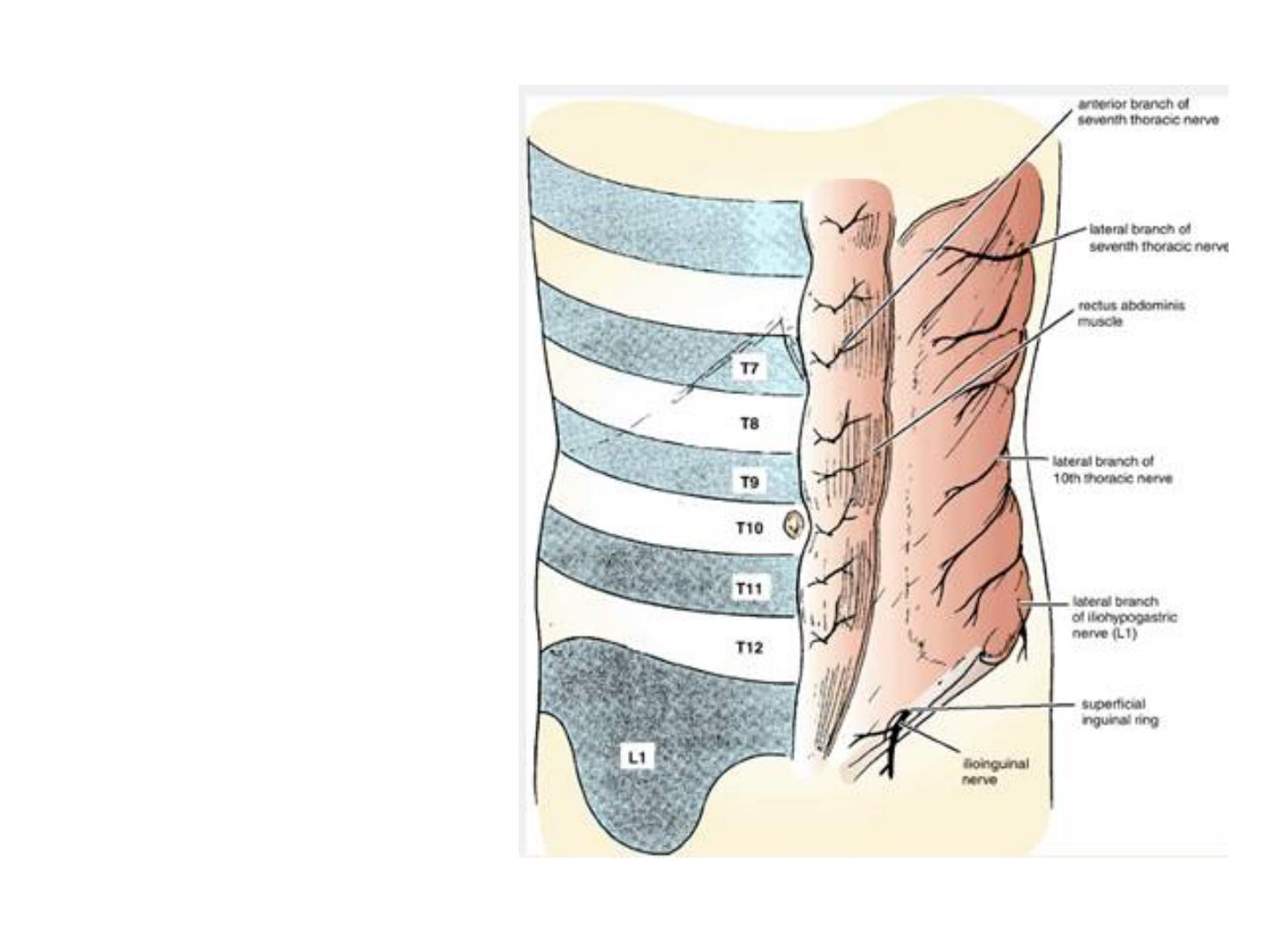
first lumbar nerve has a
similar course, but it does
not enter the rectus
sheath. It is represented
by the iliohypogastric
nerve, which pierces the
external oblique
aponeurosis above the
superficial inguinal
ring,
and by the ilioinguinal
nerve, which emerges
through the ring. They
end by supplying the skin
just above the inguinal
ligament and symphysis
pubis.
The dermatome of
T7 is located in
the epigastrium
over the xiphoid
process that of
T10 includes the
umbilicus, and that
of L1 lies just
above the inguinal
ligament and the
symphysis pubis.
For the
dermatomes of the
anterior abdominal
wall.
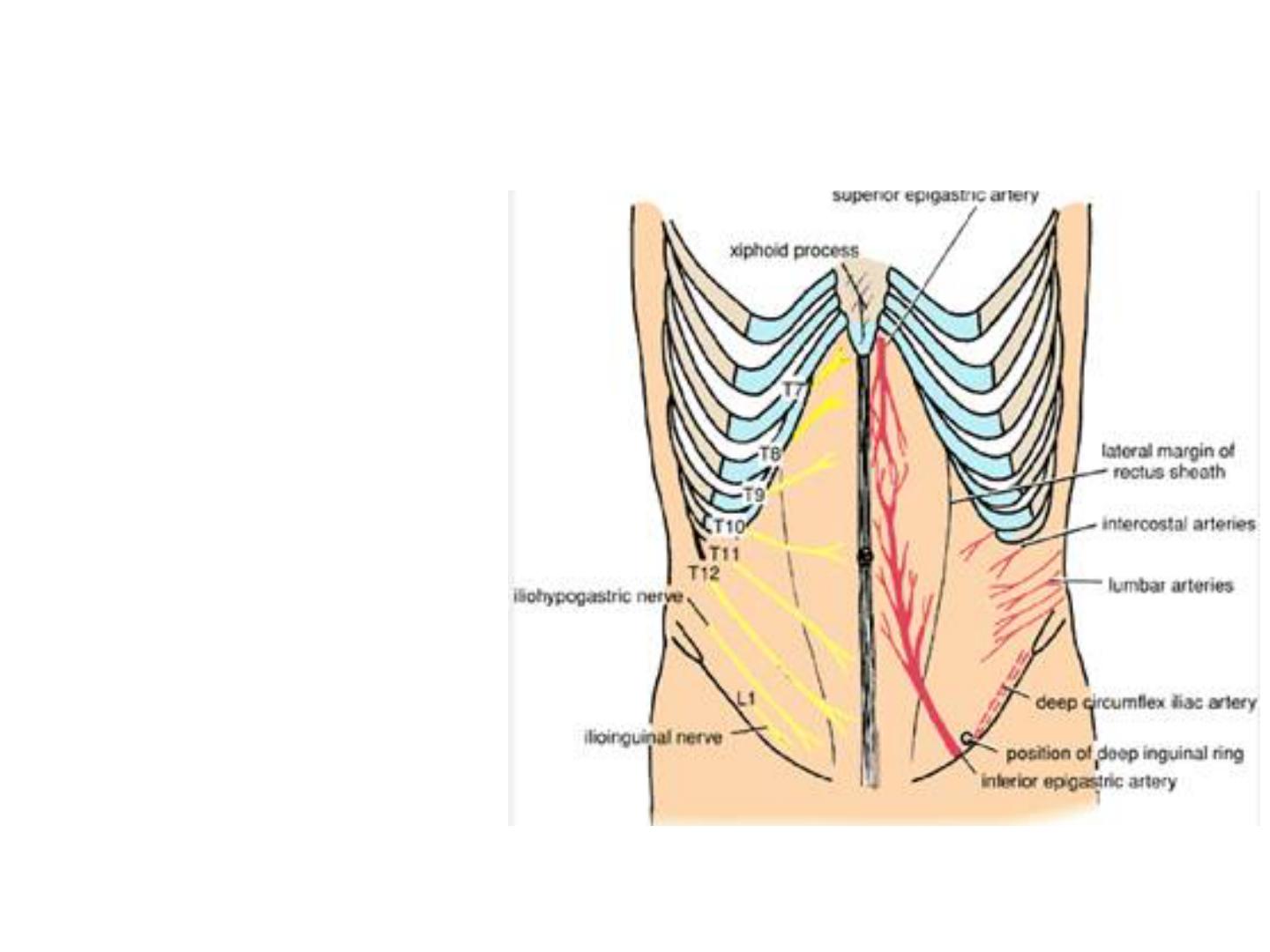
Arteries of the Anterior Abdominal Wall
The superior epigastric
artery, one of the
terminal branches of the
internal thoracic artery,
enters the upper part of
the rectus sheath between
the sternal and costal
origins of the diaphragm.
It descends behind the
rectus muscle, supplying
the upper central part of
the anterior abdominal
wall, and anastomoses
with the inferior
epigastric artery.
The inferior epigastric
artery is a branch of the
external iliac artery just
above the inguinal
ligament. It runs upward
and medially along the
medial side of the deep
inguinal ring. It pierces
the fascia transversalis to
enter the rectus sheath
anterior to the arcuate
line. It ascends behind the
rectus muscle, supplying
the lower central part of
the anterior abdominal
wall, and anastomoses
with the superior
epigastric artery.
The deep circumflex iliac
artery is a branch of the external
iliac artery just above the
inguinal ligament. It runs upward
and laterally toward the
anterosuperior iliac spine and
then continues along the iliac
crest. It supplies the lower lateral
part of the abdominal wall.
The lower two posterior
intercostal arteries, branches of
the descending thoracic aorta,
and the four lumbar arteries,
branches of the abdominal aorta,
pass forward between the muscle
layers and supply the lateral part
of the abdominal wall.
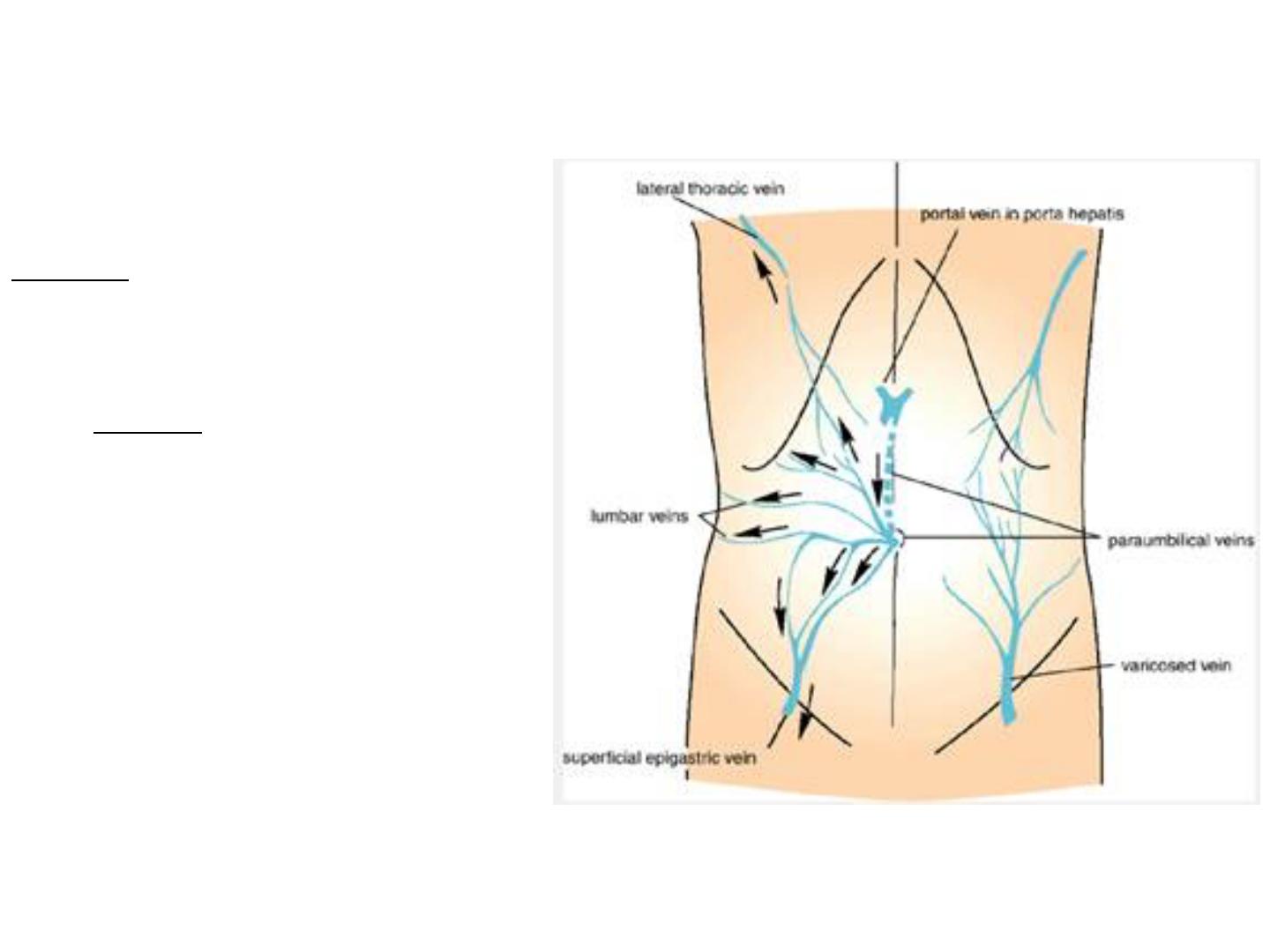
Veins of the Anterior Abdominal Wall Superficial
Veins
The superficial veins form a
network that radiates out
from the umbilicus.
Above, the network is
drained into the axillary vein
via the lateral thoracic vein
and, below, into the femoral
vein via the superficial
epigastric and great
saphenous veins. A few
small veins, the
paraumbilical veins, connect
the network through the
umbilicus and along the
ligamentum teres to the
portal vein. This forms an
important portal/systemic
venous anastomosis.

Clinical Notes
Portal Vein Obstruction
In cases of portal vein obstruction, the superficial veins around
the umbilicus and the paraumbilical veins become grossly
distended. The distended subcutaneous veins radiate out from the
umbilicus, producing in severe cases the clinical picture referred
to as caput medusae.

Deep Veins
The deep veins of the abdominal wall, the superior epigastric,
inferior epigastric, and deep circumflex iliac veins, follow the
arteries of the same name and drain into the internal thoracic
and external iliac veins. The posterior intercostal veins drain
into the azygos veins, and the lumbar veins drain into the
inferior vena cava.

Clinical Notes
Caval Obstruction
If the superior or inferior vena cava is obstructed, the venous
blood causes distention of the veins running from the anterior chest
wall to the thigh. The lateral thoracic vein anastomoses with the
superficial epigastric vein, a tributary of the great saphenous vein
of the leg. In these circumstances, a tortuous varicose vein may
extend from the axilla to the lower abdomen.
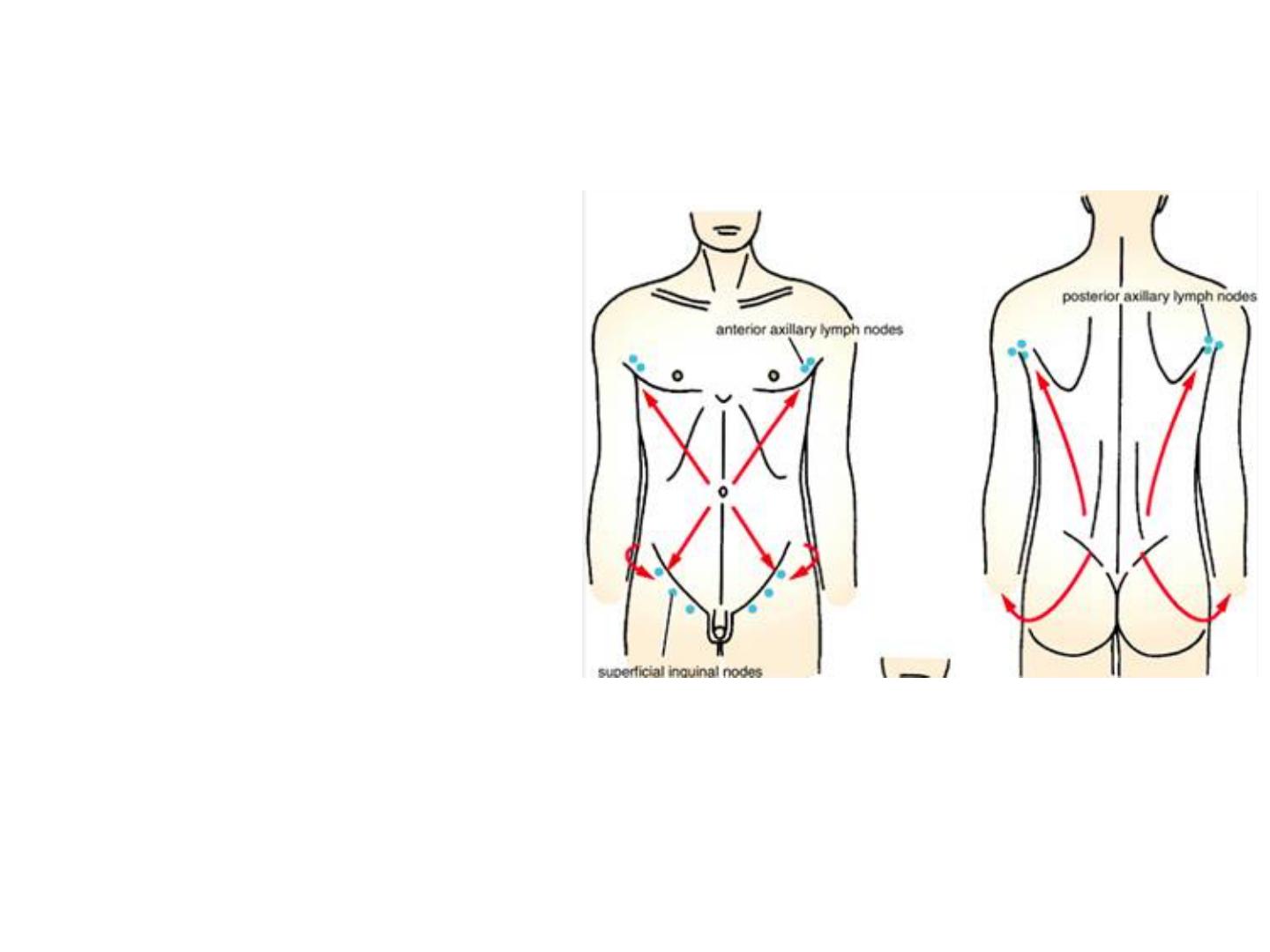
Lymph Drainage of the Anterior Abdominal Wall
Superficial Lymph Vessels
The lymph drainage of the skin of
the anterior abdominal wall above
the level of the umbilicus is upward
to the anterior axillary (pectoral)
group of nodes, which can be
palpated just beneath the lower
border of the pectoralis major
muscle. Below the level of the
umbilicus, the lymph drains
downward and laterally to the
superficial inguinal nodes. The
lymph of the skin of the back above
the level of the iliac crests is
drained upward to the posterior
axillary group of nodes, palpated on
the posterior wall of the axilla;
below the level of the iliac crests, it
drains downward to the superficial
inguinal nodes.
Lymph drainage of the skin of the
anterior and posterior abdominal walls.

Clinical Notes
Skin and Its Regional Lymph Nodes
For example, it is possible to find a swelling in the groin (enlarged
superficial inguinal node) caused by an infection or malignant
tumor of the skin of the lower part of the anterior abdominal wall or
that of the buttock.
Deep Lymph Vessels
The deep lymph vessels follow the arteries and drain into the
internal thoracic, external iliac, posterior mediastinal, and para-
aortic (lumbar) nodes.
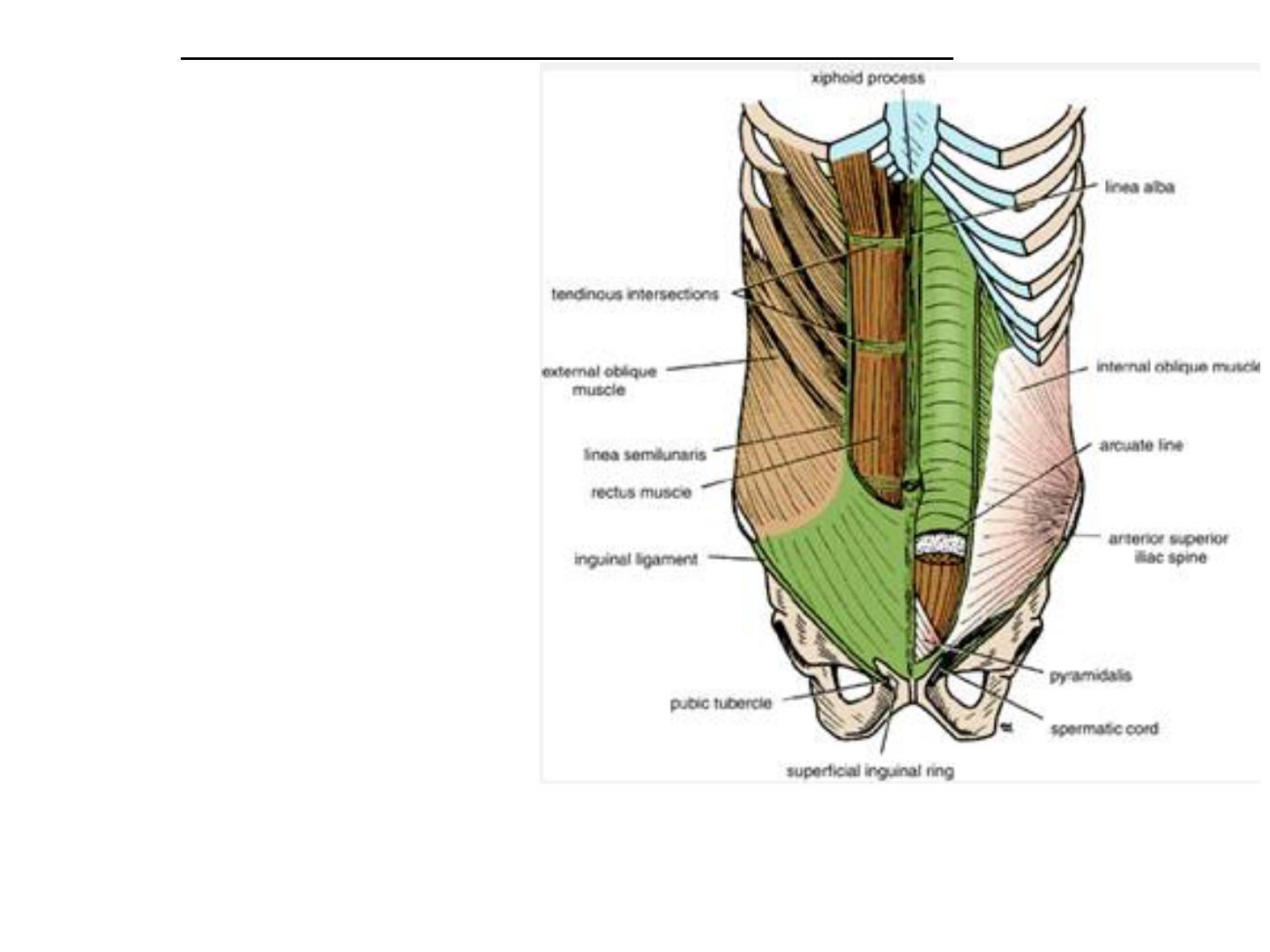
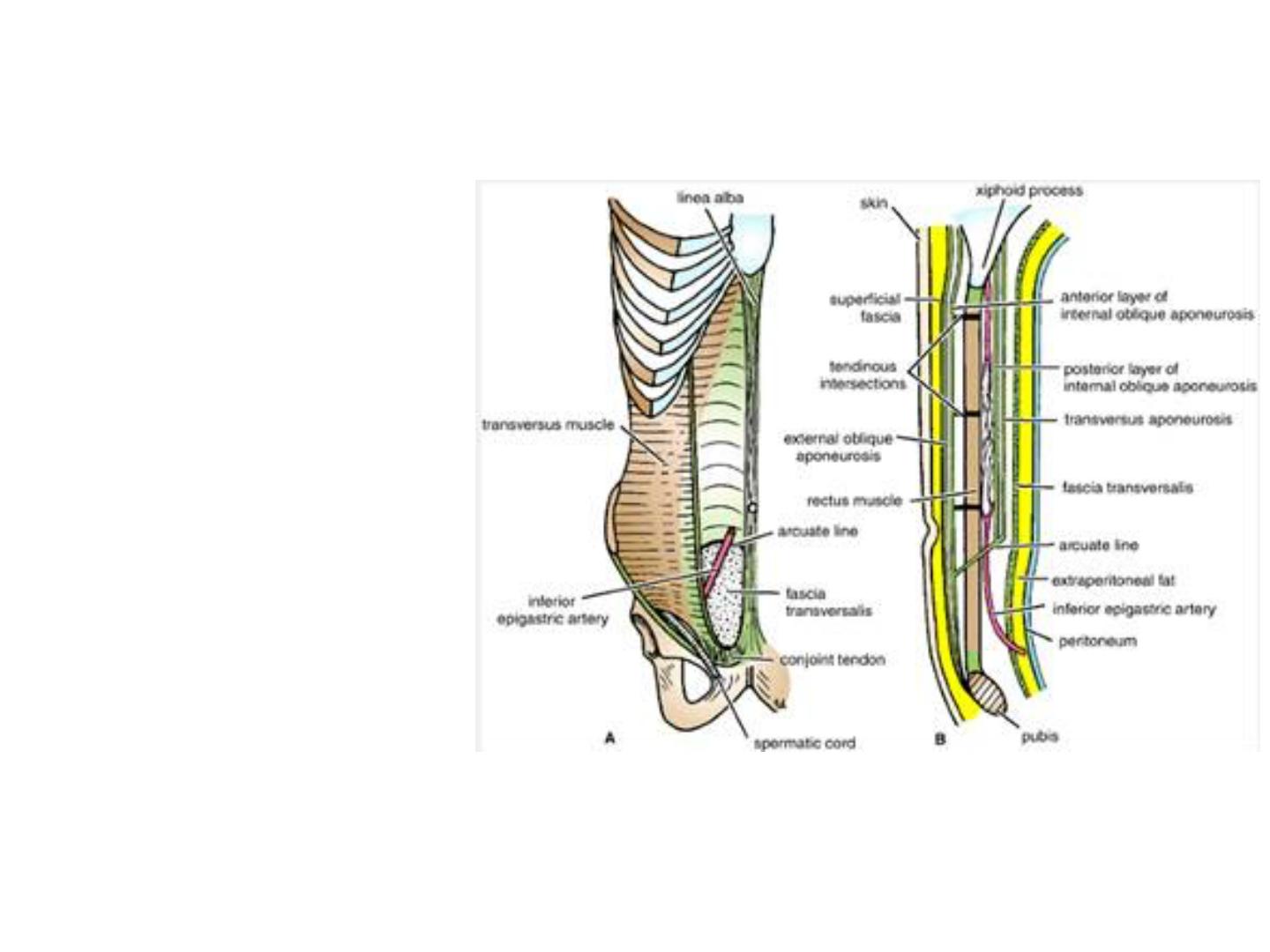
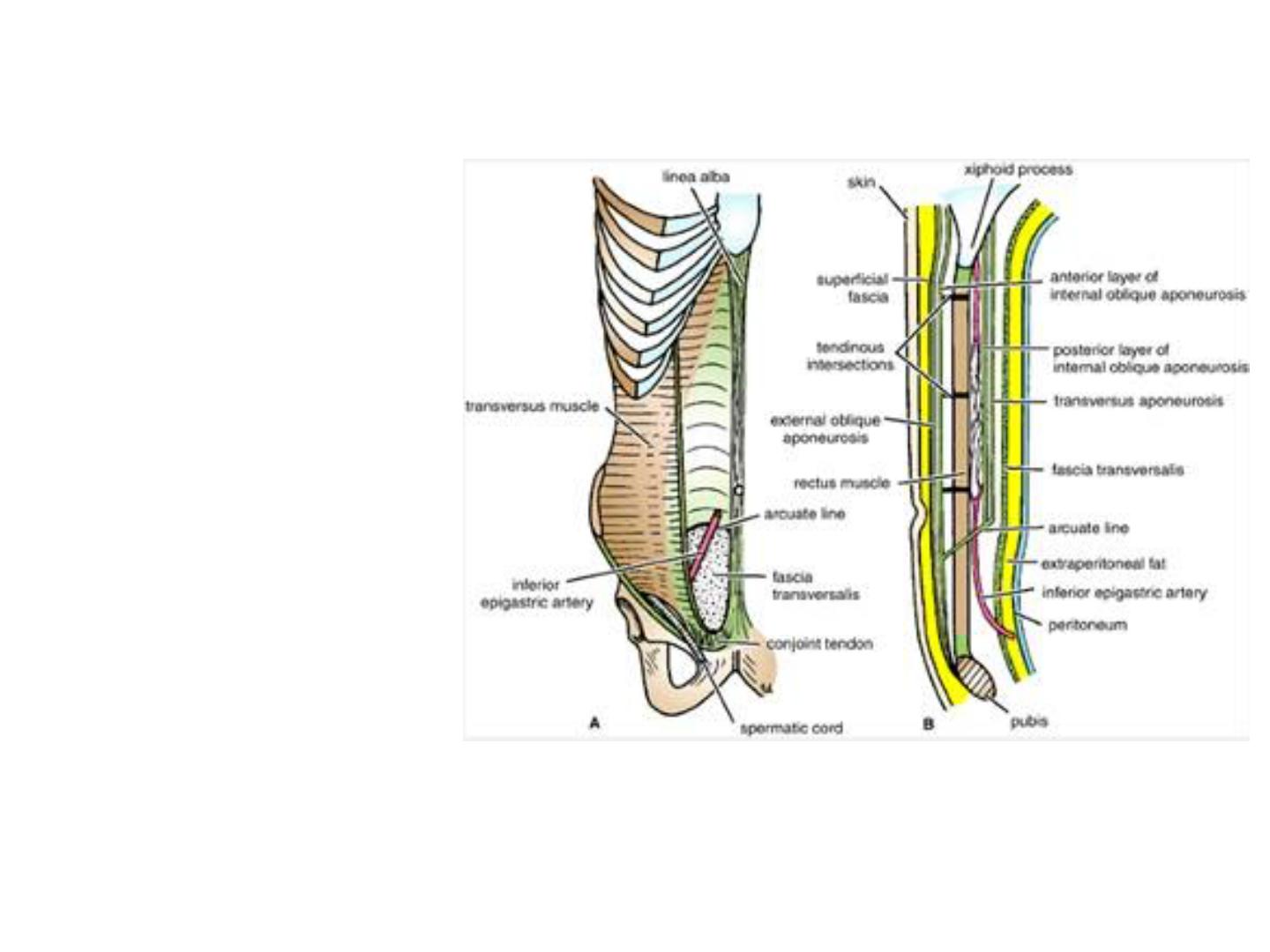
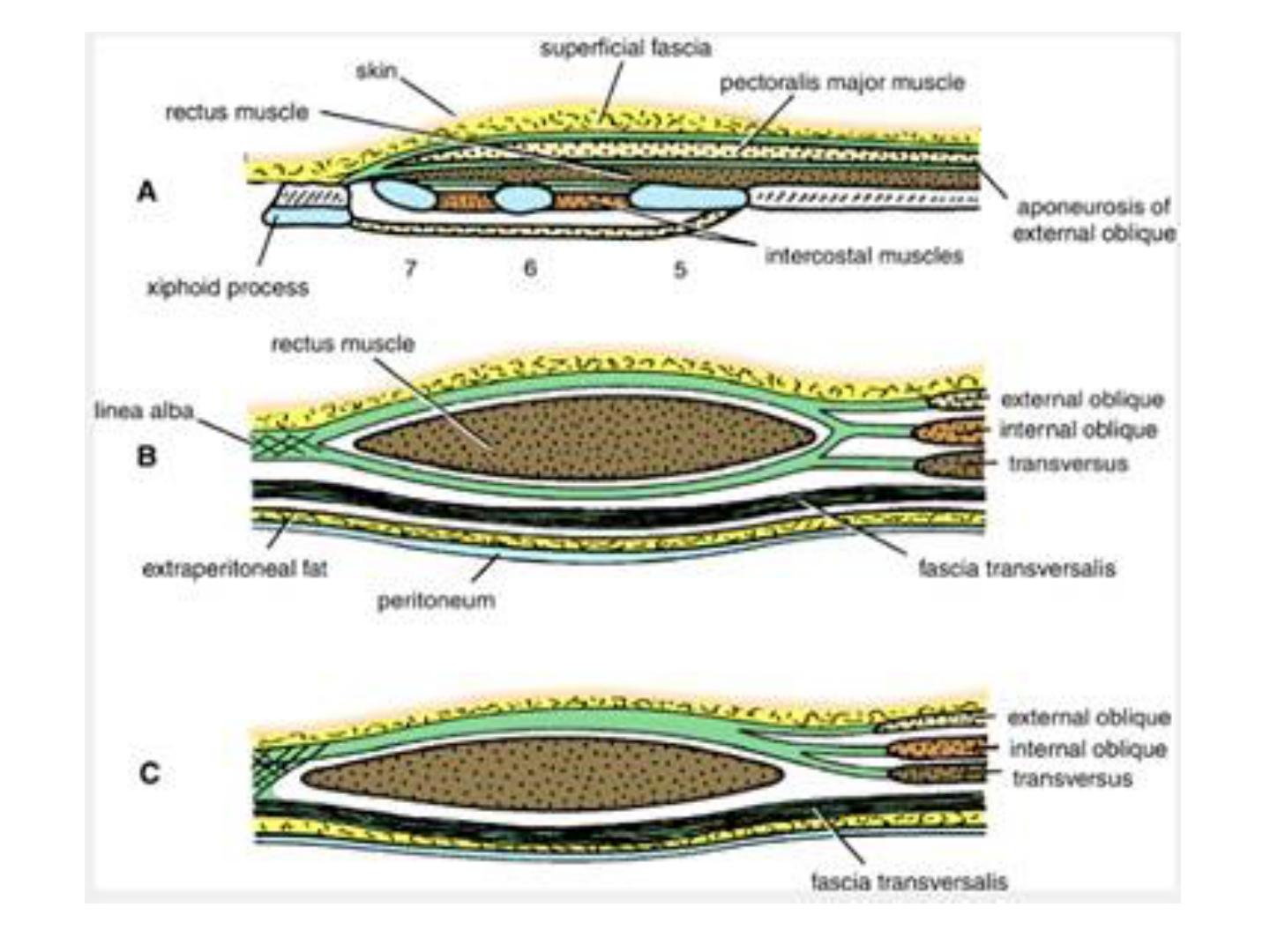
●The formation of the rectus sheath.
Anterior view of the rectus abdominis muscle and the rectus sheath. Left: The anterior
wall of the sheath has been partly removed, revealing the rectus muscle with its
tendinous intersections. Right: The posterior wall of the rectus sheath is shown. The
edge of the arcuate line is shown at the level of the anterior superior iliac spine.
Rectus Sheath
The rectus sheath is a long
fibrous sheath that encloses the
rectus abdominis muscle and
pyramidalis muscle (if present)
and contains the anterior rami
of the lower six thoracic nerves
and the superior and inferior
epigastric vessels and lymph
vessels. It is formed mainly by
the aponeuroses of the three
lateral abdominal muscles.
For ease of description the rectus sheath is considered at three levels
•Above the costal margin, the anterior wall is formed by the aponeurosis of the external
oblique. The posterior wall is formed by the thoracic wall that is, the fifth, sixth, and seventh
costal cartilages and the intercostal spaces.
•Between the costal margin and the level of the anterior superior iliac spine, the
aponeurosis of the internal oblique splits to enclose the rectus muscle; the external oblique
aponeurosis is directed in front of the muscle, and the transversus aponeurosis is directed
behind the muscle.
•Between the level of the anterosuperior iliac spine and the pubis, the aponeuroses of all
three muscles form the anterior wall. The posterior wall is absent, and the rectus muscle lies
in contact with the fascia transversalis.
The posterior wall has a free, curved lower border called the arcuate line. At this site, the
inferior epigastric vessels enter the rectus sheath and pass upward to anastomose with the
superior epigastric vessels.
The rectus sheath is separated from its fellow on the opposite side by a fibrous band
called the linea alba. This extends from the xiphoid process down to the symphysis pubis
and is formed by the fusion of the aponeuroses of the lateral muscles of the two sides. Wider
above the umbilicus, it narrows down below the umbilicus to be attached to the symphysis
pubis.
The posterior wall of the rectus sheath is not attached to the rectus abdominis muscle. The
anterior wall is firmly attached to it by the muscle's tendinous intersections.

Clinical Notes
Hematoma of the Rectus Sheath
Hematoma of the rectus sheath is uncommon but important. It
occurs most often on the right side below the level of the
umbilicus. The source of the bleeding is the inferior epigastric
vein or, more rarely, the inferior epigastric artery. These vessels
may be stretched during a severe bout of coughing or in the
later months of pregnancy, which may predispose to the
condition. The cause is usually blunt trauma to the abdominal
wall, such as a fall or a kick.
● The “new” description of the anterior abdominal wall.
The arrangement of aponeuroses of the flat muscles of the anterolateral abdominal
wall:
1. The aponeurosis of each flat abdominal muscle is bilaminar.
2.Six laminae are formed, three pass anterior and three pass posterior to the rectus
abdominis down to the level of the umbilicus.
3. There are intramuscular and intermuscular fiber exchanges within the bilaminar
aponeurosis of the external and internal oblique muscles.
4. Intramuscular exchange of superficial and deep fibers within the aponeurosis of
conralateral external oblique muscle. Fibers of right external oblique aponeurosis
which run deep on the right side, running superficially on the left side.
5. Intermuscular exchange of fibers between aponeuroses of contralateral external
and inernal oblique muscles. Fibers of the right external oblique aponeurosis
blending with fibers of the left internal oblique aponeurosis.
6. Below the umbilicus there is gradual transition of the fibers from the posterior to
the anterior layer of the rectus sheath, rather than a sudden posterior to anterior
transition of the fibers at the arcuate line.
7. The formation of digastrics muscles.
8. The linea alba is a line of decussation rather than a line of insertion of the fibers
of the aponeuroses.
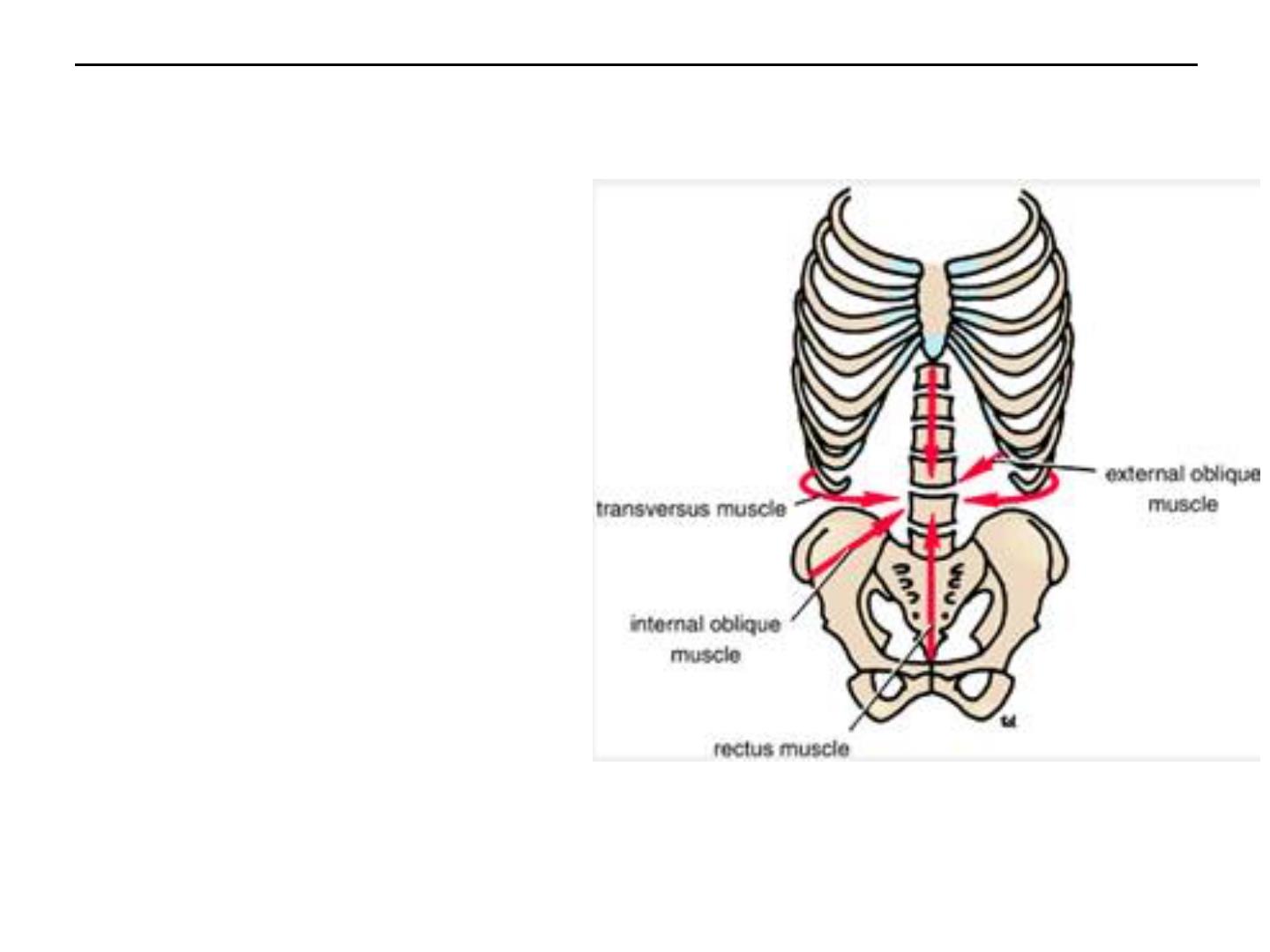
● Functional anatomy of the anterior abdominal wall
The oblique muscles laterally flex and
rotate the trunk. The rectus abdominis
flexes the trunk and stabilizes the
pelvis, and the pyramidalis keeps the
linea alba taut during the process.
The muscles of the anterior and
lateral abdominal walls assist the
diaphragm during inspiration by
relaxing as the diaphragm descends so
that the abdominal viscera can be
accommodated.
The muscles assist in the act of
forced expiration that occurs during
coughing and sneezing by pulling down
the ribs and sternum. By contracting
simultaneously with the diaphragm,
with the glottis of the larynx closed,
they increase the intra-abdominal
pressure and help in micturition,
defecation, vomiting, and parturition.
