The Blood
General InformationHematology—study of blood, blood-forming tissues, and disorders
Description:
Average Volume 5-6 liters men & 5 women (7-8% TBW)
pH 7.35-7.45 slightly alkaline
Connective Tissue
Makes up 25% of ECF
Color ranges from scarlet (oxygen-rich) to dark red (oxygen poor).
Viscosity is 5x that of water, due primarily to the presence of formed elements.
Temperature is typically 37.7°C.
Functions of Blood
A. Transportation/Distribution of Essential Substances1. Respiratory
Carries O2
CO2
Nutritive from GI tract and body stores
Excretory
Metabolic wastes, excess water and ions, other molecules not needed by body carried to kidneys for excretion in urine
B. Regulation/Maintenance
Hormonal; Carries hormones (chemical signals) from endocrine organs to target tissues.
Temperature—when ambient temp is high, diverts blood from deep vessels to superficial vessels/when ambient temp low, diverts blood from superficial to deeper vessels to help keep body warm
Maintains normal pH
maintains adequate fluid volume
C. Protection/Prevention
1. Prevents blood loss
2. Prevents infection via WBCs and plasma immune proteins.
Plasma and Formed Elements
General Information
Plasma=48-58% of blood volume in ♂ and 53-63% of blood volume in ♀.
Formed elements= Erythrocytes, Leukocytes, Platelets
Plasma— straw-colored liquid portion (55%) Composition:
Water – 92%
Proteins - ~7%, 4 Types:
Albumins
Most abundant plasma protein (60-80 %)
Contributes to viscosity & osmotic pressure
Produced by liver
Act as carriers for various molecules— steroids, fatty acids, bile salts, penicillin, etc.
2. Globulins
25-35% of the proteins
Multiple subtypes, designated; alpha, beta, and gamma globulins, play various roles;
Some bind specific molecules that are poorly water soluble such as cholesterol, fat-soluble vitamins also thyroid hormone, iron
(immunoglobins) function in immunity
regulating salt balance
3. Clotting proteins; prothrombin and fibrinogen.
Accounts for about 4%Produced in liver & help with clotting process
4. Various regulatory proteins (peptide hormones, TSH, LH, FSH) whose levels vary widely
Note: The presence of proteins in plasma makes the osmotic pressure of blood higher than that of the interstitial fluid (pulls water from interstitial fluid into capillaries)
Miscellaneous~1% Includes:
nutrients and hormonesWastes such as creatinine, bilirubin, urea.
dissolved gases
electrolytes (ions) & organic molecules (glucose, amino acids, lipids, vitamins)
Formed Elements (45% of volume of blood)—specialized for special functions:
ErythrocytesLeukocytes
Platelets
IV. Hematopoiesis (or Hemopoiesis)
The process of blood cell production, it occurs in the hematopoitic tissue.Stem Cells—after birth are the source of aLL blood cells, reside in the red marrow (fills internal cavities of ribs, sternum, pelvis, vertebrae, portions of skull) and continuously divide and differentiate to give rise to each types of blood cells
Hematopoiesis occurs in liver of fetus, and after birth liver ceases to be course of blood cell production.
Stem cells migrate to bone marrow, Red myloid tissue
Lymphoid tissue produces lymphocytes derived from cells that originated in bone marrow.
Erythropoiesis = RBC formation:
Mechanism for regulating RBC production is called Erythropoisisa. Number of RBCs in blood is remarkably constant and maintained via negative feedback.
b. The daily production of new R.B.Cs compensates for the daily destruction of old R.B.Cs .
c. Erythropoietin (EPO) a hormone released from the kidney, controls the rate of erythropoiesis.
d. The kidneys always release EPO. whenever blood oxygen levels are decreased or R.B.Cs count decreased.
e. Erythropoietin acts by binding membrane receptors on cells that will become erythroblasts and this will undergo cell division & differentiation leading to the production of erythroblast Normoblast which lose their nuclei to became Reticulocytes (This process takes 3 days).
f. Most of the iron contained in the hemoglobin molecules of the destroyed cells is recycled back to new R.B.Cs .
g. Requires the supply of iron , vitB12 & folic acid.
Stimulus of erythropoiesis
1) Hypoxia or hypoxemia(low oxygen amounts in the blood)Happens naturally in change from low to high altitude
Helps maintain gas levels in areas with low O2
2) Artificial Means of Influencing number of erythrocytes:
Blood doping—transfusion of more blood into systemIllegal in airy-fairy and Olympic competition (no lab test available)
Injection of EPO into blood stream
Both processes artificially induce excess of RBC—increases viscosity
Done to increase amount of O2 tissues get, hence greater endurance and speed
Risks—increased viscosity of blood may cause temporary high blood pressure or reduced blood delivery to body tissues—heart must work harder to pump blood through circulatory system
No test currently available to detect erythropoietin so is widely used among competitors in cycling, skiing, and long distance running
Leukopoiesis ; production of white blood cells
White blood cells are produced at varying rates depending on changing defense needs of the body/different types are selectively producedSpecific chemical messengers analogous to EPO direct differentiation and proliferation of each white blood cell type
Some messengers have been identified and can be produced in lab (granulocyte colony-stimulating factor) marketed as powerful therapeutic agent to decrease infection in chemotherapy patients
Thrombopoietin (TPO); produced by liver, stimulates proliferation of megakaryocytes and their growth and development into platelets.
V. Erythrocytes, Red blood cells (RBCs);
A. Structure is well suited to their main function of O2 transport in blood
Most abundant cell type in blood
Women average about 4.8 million of these cells per cubic millimeter (mm3; which is the same as a microliter [µl]) of blood. Men average about 5.4 x 106 per µl.
These values can vary over quite a range depending on such factors as; health and height above sea level. (Peoples living at 18,000 feet may have as many as 8.3 x 106 RBCs per µl.)
Primary function is O2 transport. Play a minor role in CO2 transport.
Disc shaped cell with thick rim and thin sunken center, Biconcave shape gives them a high surface area to volume ration (good for O2 entry/exit) and increased flexibility (good for squeezing thru tight capillaries).
Plasma membrane of mature RBC has glycoproteins and glycolipids that determine blood type
Inner surface has two peripheral proteins that give membrane elasticity and durability so RBC can stretch, bend, fold to squeeze through small capillaries and they spring back into shape.
Mature cells have no organelles and cannot respire aerobically. Prevents them from consuming the O2 they are transporting; also can't repair cell damage if it occurs
Hemoglobin
Abundant within RBCs. Small amount is also dissolved in plasma. reversibly binds and releases O2.Hemoglobin consists of:
4 protein chains called globins: 2 alpha and 2 beta globins
Each chain is bound to a heme group (red pigmented molecule that contains iron)
heme group binds O2 to an iron ion at its center
Each heme group can carry one molecule of O2 so each hemoglobin molecule as a whole can transport up to 4 O2. (because there are 4 hemes)
CO2 transported by binding to the globins rather than the heme
B. Quantities of Erythrocytes and Hemoglobin
RBC count and hemoglobin concentration important clinical data—amount of O2 blood can carryThree common measurements:
1) hematocrit-(men=average 45%women=average 42%)
2) hemoglobin concentration of whole blood
3) RBC count
Typically, values lower in women due to:
androgens stimulate RBC production in men
women of reproductive age have menstrual losses
Men have fewer vessels in skin and blood clots faster.
hematocrit is inversely proportional to % body fat
C. Erythrocyte Destruction
Circulating erythrocytes stay in blood for 120 days
Must be replaced at average rate of 2-3 million cells/second
As RBC ages membrane proteins deteriorate and membrane grows increasingly fragile. (No DNA or RNA so cannot synthesize proteins for cellular growth, repair, division)
Hemolysis
RBCs Eventually ruptures as it tries to squeeze through narrow capillaries
Spleen “erythrocyte graveyard”—very difficult to pass through its narrow, twisting channels. Old RBCs get trapped here (some in liver), get broken down (enlarged spleen may indicate diseases in which RBCs are rapidly breaking down)
Cell fragments are phagocytized by macrophages in spleen, liver.
Hemoglobin decomposes into:
Globin portion—hydrolyzed to amino acids which is reused
Heme portion—further decomposed into:
Iron portion—transported to liver and bone marrow and some is used to make new hemoglobin in bone marrow.
Rest of the heme is converted into biliverdin (greenish pigment) bilirubin (yellowish green pigment) in the liver contributes to the formation of bile.
(high level of bilirubin in blood causes jaundice—yellowish color—may be sign of liver disease that interferes with bilirubin disposal or rapid hemolysis)
VI. Erythrocyte disorders
Polycythemia
Dangerous excess of RBCs
Caused by factors that stimulate states of chronic hypoxemia which stimulates erythropoietin secretion
Cancer, emphysema, smoking, air pollution, etc.
Excess # of RBCs make the blood stream packed full of RBCs; hard to get all of them through capillaries poor circulation, clogged capillaries, which strains heart—heart failure, stroke, embolism.
Anemia
Refers to any condition that compromises the O2 carrying capacity of blood/ there is an abnormally low hemoglobin concentration/low RBC count
Various causes:
Nutrional anemia—dietary deficiency of factor needed for erythropoeisis, (iron).
Pernicious anemia—inability to absorb enough ingested Vitamin B12—need for normal RBCs development and maturation
Hemorrhagic anemia—due to excessive bleeding
Renal anemia from kidney disease
Aplastic anemia—failure of bone marrow to produce enough RBCs—may be due to toxic chemicals, exposure to readiation, cancer, chemotherapy
Hemolytic anemia—caused by rupture of too many RBCs.
Example: Sickle Cell Anemia—due to hereditary hemoglobin defects—occur mostly among people of African, Mediterranean descent. RBCs are sickle-shaped due to problem in one of the hemoglobin chains tend to clump together and shape of cell causes it to block small blood vessels. Can lead to heart failure, kidney failure, paralysis, strokes, etc.
VI. Platelets (thrombocytes);
General info
Fragments of cells—smallest of formed elements(2-4 m diam.)
Start with a hematocytoblast megakaryocyte bits of megakaryocyte break off become platelets
150,000-400,000 platelets per L of blood
Typical life span of about 10 days
Always present in blood, but not active unless damage has occurred to walls of circulatory system
Important in blood clotting—attach together
Platelets reside in bone marrow, blood, spleen
B. Hemostasis = the stoppage of bleeding. Consists of 3 events: vascular spasm, platelet plug formation, and coagulation.
1.Vascular spasm (vasoconstriction) prompt constriction of the broken vessel
Triggered by several things.Platelets release serotonin, a chemical vasoconstrictor.
Pain receptors innervate nearby blood vessels and cause them to constrict.
Injury to smooth muscle also causes some vasoconstriction
2. Platelet plug formation—mechanical blockage of a hole
When a vessel breaks, platelets stick to exposed collagen (platelet adhesion)Activated platelets release chemical messengers that work to activate more platelets
Mass of platelets = platelet plug—may reduce or stop minor bleeding
As platelets continue to aggregate into growing platelet plug release more platelet-attracting chemicals, RBCs also aggregates with Platelets giving red color to the clot.
Thus, positive feedback cycle is activated that can quickly seal a small break in blood vessel
Uninjured endothelial tissue releases chemicals that inhibit platelet aggregation so plug is confined to site of injury
3. Blood clotting - the coagulation cascade;
last but most effective defense against larger tears in vessels
Very complex process involving over 30 chemical reactions—delicate balance between clotting and absence of vessel damage.
Ultimate step is conversion of fibrinogen, a large plasma protein produced by liver, into fibrin, an insoluble threadlike molecule
Enzyme thrombin converts fibrinogen into fibrin fibers that intertwine with and reinforce the platelet plug. Reinforced plug is called a clot.
Various pathways are important but the important thing is that fibrinogen is converted to fibrin needed to form the clot
Preventing Inappropriate clot formation:
Anti-coagulants inhibit clotting. Body produces two anticoagulants which work together to inhibit inappropriate clotting.Anticoagulant drugs use various mechanisms & are prescribed when needed, such as heparin (inactivation of thrombin) , Coumadin (interferes with Vit K, which is required for functioning of several clotting factors, several others.
(Aspirin—prevents platelet plug formation—does not thin blood but prevent platelets from aggregating)
Clot restriction
Clots are restricted from growing too large by the removal of clotting factors as well as the presence of normal anticoagulant chemicals.Clot retraction
a. Following clot formation the actin/myosin in platelets contract, compacting the clot and pulling the vessel edges together (facilitating repair).b. Squeezes serum (plasma minus clotting factors) from the clot.
Fibrinolysis
a. Breakdown of the clotb. Following vessel repair the inactive plasma protein plasminogen is converted to plasmin by tissue plasminogen activator.
Plasmin digests fibrin once repairs have taken place.
Coagulation disorders
a. Hemophilia—family of hereditary diseases characterized by deficiencies of one factor or another (clotting factor VIII)Sex-linked recessive mechanism of heredity (carried on the X chromosome) occurs predominantly in males as they carry this gene.
Varies in severity; If severe, physical effort causes bleeding in muscles and joints.
Managed clinically by transfusions of fresh plasma or injections of appropriate clotting factor
b. Thrombosis—hemostasis in wrong place
Abnormal clotting in an unbroken vessel called thrombus
Can be caused by several factors—roughened vessel surfaces associated with atherosclerosis, imbalances in clotting factors, slow moving blood such as pooled in DVTs (deep vein thrombosis), bacteria or toxins
If the clot breaks free and travels in the blood system, may lodge in dangerous areas (lungs, heart, brain)—called embolus
Vitamin K Deficiency—inadequate formation of clotting factors
VII. Leukocytes , White blood cells(WBCs)General information
Account for far less than 1% of total blood volume.
Normal range is 5000-10,000 per L of blood.
Protect the body from pathogens, toxins, and cancerous cells.
Differences between RBCs and WBCs
Have nuclei and mitochondria
Lack hemoglobin
Far less numerous in blood than RBC
Immune function (not gas transport)
Five different types—each vary in structure, function, number
Don't circulate in the blood as much spend most time in tissues-have ability to migrate through tissues—very important for their function as defense corps of the body—attack foreign invaders, and destroy abnormal cells (precancerous, cancer) that arise in body and clean up cellular debris
Categories of WBCs (2 categories, 5 major types):
A. Granulocytes; Stay in transit in blood for less than a day before leaving blood to enter tissues, where it survives another 3-4 days unless it dies sooner in line of dutyNeutrophils
Most numerous of WBC—50-70% of all
Phagocytic specialists that engulf debris and bacteria
First to arrive at an scene of bacterial invasion
can release additional chemicals to attract other neutrophils & help in inflammatory response
Can also act like “suicide bombers”
Eosinophils
Associated with allergic conditions such as asthma, hay fever and with internal parasitic infestations
Main contribution is attacking parasitic invaders to large to be engulfed. Attach to invader and secretes substances that kills it
Can sometimes be harmful because toxic molecules they release can trigger allergic reactions.
Basophils
Non-phagocytic cells that synthesize, store, and release on appropriate stimulation.
May release histamine that triggers allergic reactions
Also synthesize and release heparin—anticoagulant
Speeds up removal of fat from blood after fatty meal
Release chemicals to help with blood vessel dilation, attracts other WBCs to the injured site.
Agranulocytes;
Monocytes
A non-specific defense
Largest of all formed elements
Become large tissue macrophages that phagocytize items that are non-self
Lifespan ranges from months to years unless destroyed sooner while performing phagocytosis
Found in GI tract, alveoli of lungs
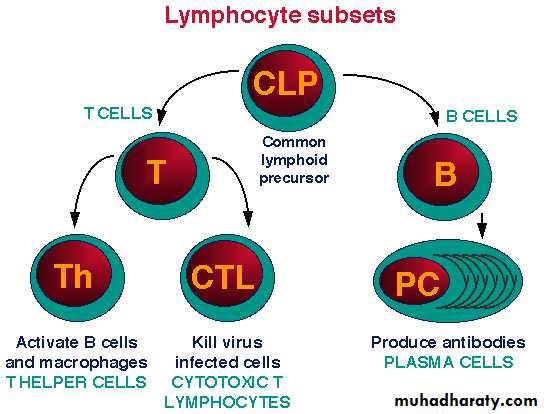
Lymphocytes
2nd most numerous type of leukocyte
Provide specific defense against particular bacteria, viruses, and other targets for which they are specifically programmed.
Live for about 100-300 days continuously recycling through lymphoid tissues, lymph, and blood.
2 functional types of lymphocytes
T-cellsmigrate to the Thymus & develop into T-cells.
recognize & destroy body cells gone awry, including virus-infected cells & cancer cells.
Coordinate cell-mediated attack—directly destroy specific target cells by releasing chemicals that punch holes in victim cell
B-cells
remain in the Bone marrow & develop into B-cells
are most effective against bacteria & their toxins plus a few viruses
Produce antibodies, which circulate in blood
Antibodies bind with and mark specific invaders
VIII. Blood types
Blood types classified by the ABO systemWithin major blood group system, the ABO system, erythrocytes have specific surface antigens.
ABO classification
Hereditary presence or absence of RBC surface antigens A and B determines a person’s ABO blood type. Antibodies react against any AB antigen except those present on a person’s own RBCs.
Each person inherits two genes (one from each parent) that control production of the ABO antigens.
Genes for A and B are dominant to the gene for O since O means absence of A or B.
Type A
Type B
Type AB
Type O
Antigen on RBCs
A
B
A and B
None
Antibody in plasma
Anti B
Anti ANeither anti-A nor anti-B (none)
Anti-A and Anti-B
Compatible donor blood
A, O
B, O
A, B, AB, O
O
Incompatible
B, AB
A, AB
None
A, B, AB
Antibodies against erythrocyte antigens not present on body’s own RBCs begin to appear in human plasma at about age six months.
The antibodies in plasma may not be made specifically against RBC antigens but are produced in response to some intestinal bacteria that share same characteristics
Transfusions
Agglutination is the adhesion of RBCs to each other block small vessels causing hemolysis kidney blockage
When mismatched blood is infused, transfusion reaction occurs
Reaction occurs when donor’s RBCs are attacked by recipient’s plasma antibodies.
Initial event is agglutination of foreign RBCs (adhesion of RBCs to each other). This clumping obstructs blood flow through small vessels so oxygen and nutrient flow to cells and tissues is reduced.
Clumped blood cells begin to rupture and circulating hemoglobin passes into kidney tubules leading to blockage and may cause renal shutdown or even acute renal failure resulting in death.
RH factor
DefinitionRH factor
A group of antigens found on the RBC membranes
Antigens first found in rhesus monkeys
No naturally occurring antibodies develop against the Rh factor
Importance
If you have the Rh antigen Rh+If you don’t have the Rh antigen Rh-
However, anti-Rh agglutinins are not normally present, they form only in Rh- individuals who are exposed to Rh+ blood.
Rh- individuals should be given only Rh- blood whereas Rh+ people can safely receive both
Rh- person receiving Rh+ transfusion, recipient’s antibody producing cells are stimulated to produce anti Rh. Presents little danger in first mismatched transfusion but later mismatched transfusion recipient’s plasma agglutinins would agglutinate donor’s RBCs.
If an Rh- mother gives birth to an Rh+ baby, there is no problem with the pregnancy, but during birth, blood may mix and the mother may be exposed to Rh+ cells and produce antibodies against Rh+ cells
If a second child is Rh+, the mother’s body may view the second child as an “invader” and antibodies against the Rh factor could cross placenta and destruct fetal erythrocytes.
erythroblastosis fetalis—hemolytic disease of the newborn baby—severe anemia.
Can be prevented by treating with Rh immunoglobulin
(RhoGAM) during birthing process or during pregnancy. (Injected antibodies inactivate the Rh antigens and thus prevent mother from becoming actively immunized to them)
Other Blood Groups: At least 300 other detectable blood groups, in addition to ABO and Rh have been identified.
Rarely have transfusion reactions from these groups but are useful for legal purposes, in paternity and criminal cases and for research in anthropology and population genetics.
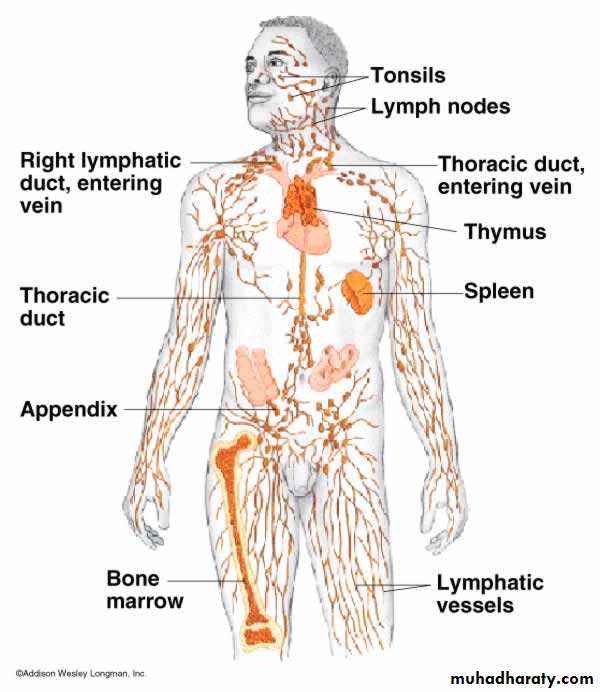
Lymph
Lymph is similar to plasma except it contains fewer proteins. It contains water, nutrients, ions, gases, wastes, and hormones.
Lymph within lacteals is known as chyle ,it Pass thru lymph nodes, where lymph is “cleaned” of pathogens and cancer cells
The lymphatic system represents an accessory route through which fluid can flow from the interstitial spaces into the blood.
The lymphatics can carry proteins and large particulate matter away from the tissue spaces, neither of which can be removed by absorption directly into the blood capillaries.
This return of proteins to the blood from the interstitial spaces is an essential function without which we would die within about 24 hours.
Formation of Lymph;
Most of the fluid filtering from the arterial ends of blood capillaries flows among the cells and finally is reabsorbed back into the venous ends of the blood capillaries; but on the average, about 1/10 of the fluid instead enters the lymphatic capillaries and returns to the blood through the lymphatic system rather than through the venous capillaries.
The total quantity of all this lymph is normally only 2 to 3 liters each day.
The fluid that returns to the circulation by way of the lymphatics is extremely important because substances of high molecular weight, such as proteins, cannot be absorbed from the tissues in any other way.
Lymph is derived from interstitial fluid that flows into the lymphatics. Therefore, lymph as it first enters the terminal lymphatics has almost the same composition as the interstitial fluid.
The protein concentration in the interstitial fluid of most tissues averages about 2 g/dl, and the protein concentration of lymph flowing from these tissues is near this value.
Conversely, lymph formed in the liver has a protein concentration as high as 6 g/dl, and lymph formed in the intestines has a protein concentration as high as 3 to 4 g/dl.
Because about two thirds of all lymph normally is derived from the liver and intestines, the thoracic duct lymph, which is a mixture of lymph from all areas of the body, usually has a protein concentration of 3 to 5 g/dl.
The lymphatic system is also one of the major routes for absorption of nutrients from the gastrointestinal tract, especially for absorption of all fats in food. Indeed, after a fatty meal, thoracic duct lymph sometimes contains as much as 1 to 2 per cent fat.
Finally, even large particles, such as bacteria, can push their way between the endothelial cells of the
lymphatic capillaries and in this way enter the lymph.
As the lymph passes through the lymph nodes, these particles are almost entirely removed and destroyed.
lymph flow of about 120 ml/hr or 2 to 3 liters per day.
Effect of Interstitial Fluid Pressure on Lymph Flow.
Any factor that increases interstitial fluid pressure also increases lymph flow if the lymph
vessels are functioning normally. Such factors include the following:
Elevated capillary pressure
Decreased plasma colloid osmotic pressure
Increased interstitial fluid colloid osmotic pressure
Increased permeability of the capillaries
Increasing tissue pressure not only increases entry of fluid into the lymphatic capillaries but also compresses the outside surfaces of the larger lymphatics, thus delay lymph flow.
Factors responsible for lymph flow:
Skeletal muscle pumpRespiratory pump
Lymphatic Pump; Contraction of smooth muscle in the lymphatic vessel walls, Valves exist in all lymph channels. each segment of the lymph vessel between successive valves functions as a separate automatic pump.
Compression of lymphatic vessels by pulsations of nearby arteries.
Inability to move lymph (perhaps due to blockage of a lymphatic vessel) can result in an excess of ISF accumulation, i.e., edema.