Chronic Rhinosinusitis
Dr. Abdullah AlkhalilMRCS-ENT(UK), DOHNS(London)
Higher specialty(JUST),
Jordanian Board.
1
Introduction
Chronic inflammation of the sinuses usually follows recurrent acute sinusitis, but in some cases the onset is more insidious.Considered when sinusitis symptoms persist after 12 week.
Chronic sinusitis accounts for over 85% of all clinic visits for sinusitis in adults.
Incidence is increasing worldwide.
2
Pathophysiology
There is an increase in vascularity and vascular permeability. This leads to oedema and hypertrophy of the mucosa which may become polypoidal. Goblet cell hyperplasia and a chronic cellular infiltrate will occur. Ulceration of the epithelium will result in the formation of granulation tissue.3
Pathophysiology
Multiple small abscesses occur in the thickened mucosa and fibrosis of the submucosal stroma supervenes. The changes in the mucosa over this time may be irreversible, and when the original cause of infection has been treated the lining will not revert to normal.
4
Microbiology
Anaerobesgm+ cocci, bacteroides, corynebacteria
Staphylococcus aureus
Streptococcus
H. Influenzae
M. catarrhalis
5
Symptoms
nasal obstruction 94%postnasal drainage 92%
facial pain & headache 90%
rhinorrhea 61%
hyposmia / anosmia
6
Clinical Features
The cardinal symptoms are nasal congestion, nasal or postnasal discharge and pain. A headache over the forehead, the bridge of the nose and the face is common. The patient may also suffer with hyposmia, anosmia, or even cacosmia (unpleasant smell), especially in infections of dental origin.7
Clinical Features
Chronic irritation of the nasal airway and repeated rubbing may lead to a vestibulitis and epistaxis. Chronic pharyngitis and laryngitis with the patient complaining of a productive cough are often encountered. Clinical examination will usually show nasal inflammation or perhaps another obvious intranasal predisposing factor.8
Differential diagnosis
It is not uncommon for general practitioners and those in other specialties to ascribe facial pain and headaches to sinus disease, often when it is not. It has been suggested that chronic paranasal sinus pain alone should not constitute chronic sinusitis.The ENT surgeon is confronted as a rule with three different groups of headache patients:
9
Differential diagnosis
• Those with headaches clearly connected to a sinus problem, such as inflammatory disease, neoplasm, barotrauma or another readily identifiable cause.10
Differential diagnosis
(b) Those with headaches clearly traceable tonon-sinus causes such as migraine,
neuralgias, cervical spine disorders,
temporomandibular joint diseases,
glaucoma, hypertension.
11
Differential diagnosis
(c) Those whose problems are not clear and in
whom there seems to be no overt indication
of sinus disease. In this group of patients
nasendoscopic examination with a high-
definition coronal section CT scan may
confirm that the symptoms are indeed sinus
related.
12
Investigations
Only the combination of diagnostic endoscopy and high-definition coronal section CT scanning will provide the maximum information. One modality is said to enhance the accuracy of the other. Furthermore, some patients with sinogenic headaches may present with an atypical history and have negative findings on examination and plain sinus radiographs. This does not rule out a sinus cause for their problem.13
14
Treatment
The principal aims of treatment are to correct the predisposing cause, to ventilate the sinus and to restore normal mucosal lining in the sinus.
Medical treatment should continue for at least three months before considering surgery.
15
Medical treatment
• Intranasal steroids.• Oral antibiotics:
- Amoxcillin + clavulanic acid
- Cefuroxime
- Macrolide
3. Treatment of underlying cause.
16
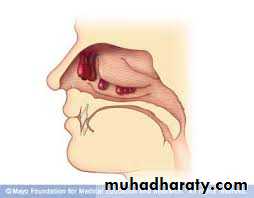
Surgery
• Functional endonasal(endoscopic) sinus surgery.Functional endoscopic sinus surgery is now
the preferred alternative to the classical open
surgical approaches to chronic sinusitis.
Those who advocate this procedure claim
that more accurate surgery can now be
undertaken and that injury to the eye, optic
nerve or dura is less likely.
17
Surgery
Step-wise removal of the ethmoidal cells extending to the posterior ethmoid and sphenoid sinus can be undertaken. The natural ostium of the maxillary sinus in the middle meatus can be cleared, opened and enlarged, as can any disease of the frontonasal duct.
18
Surgery
(b) Open sinus surgery procedures.If irreversible changes have occurred to the
sinus mucosa then some surgeons would
consider it necessary to remove it. A wide
range of procedures are available, so the
choice of operation should be tailored to the
requirements of the individual patient.
19
Surgery
Each procedure has its own limitations and specific complications. However, the more radical open procedures are still used and asked about in the examinations.20
Surgery
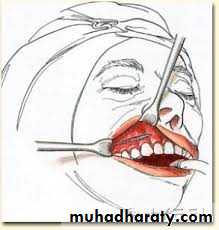
• Chronic maxillary sinusitis: Caldwell-Lucprocedure.
21
Surgery
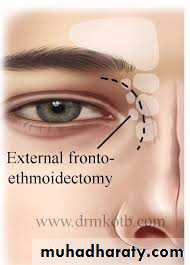
Chronic ethmoid sinusitis: external ethmoidectomy (Patterson’s operation).22
Surgery
Chronic frontal sinusitis: external frontoethmoidectomy (Howarth’s operation), osteoplastic flap procedure (MacBeth’s operation).Chronic sphenoiditis: via an intranasal ethmoidectomy, transantral to the posterior ethmoids then to the sphenoid sinus
23
Fungal sinusitis
24
Overview
This is now being recognized more frequently, because of advances in diagnostic techniques (nasal endoscopy and CT scans) and increasing numbers of immunocompromised individuals.Fungal infections have recently been implicated in the majority of cases of chronic rhinosinusitis.
25
Overview
• Mycetoma(Fungal ball). These are masses of fungal debris that usually occur in the maxillary or ethmoid sinuses. Patients are typically immunocompetent and non-atopic. Aspergillus fumigatus is the most common organism isolated. Treatment is by endoscopic removal of debris and ventilation of the sinus. There is usually no requirement for antifungal or any other systemic therapy.26
Mycetoma
27
Overview
2. Allergic fungal sinusitis. Typically occurs inatopic immunocompetent young adults.
Usually associated with nasal polyps and
asthma. Associated fungi include Aspergillus,
Bipolaris and Curvularia. Because of the
potential for orbital and intracranial
complications, appropriate treatment needs
to be rapidly instituted.
28
Overview
2. Allergic fungal sinusitis.
The mainstay of therapy is polypectomy and aeration of the sinuses. Systemic steroids and
antifungal therapy (itraconazole), may also be useful.
29
Overview
3. Chronic indolent sinusitis. This should besuspected in a healthy patient presenting with
chronic sinusitis resistant to conventional
therapy. This is a slow progressive disease
characterized by granulomatous infection.
Aspergillus fumigatus is the most common
organism isolated. Surgical debridement with
removal of all debris from the sinuses is required.
Amphotericin B is the drug of choice.
30
Overview
4. Acute invasive (fulminant) sinusitis.A rare entity that occurs in
immunocompromised individuals (diabetic
ketoacidosis, chemotherapy patients, AIDS,
leukaemia and lymphoma). Aspergillus, Mucor
and Rhizopus are the associated organisms.
31
Overview
4. Acute invasive (fulminant) sinusitis.
Immediate treatment consists of intravenous
antifungal therapy (amphotericin B) and
radical surgical debridement, which can
extend to a total maxillectomy and orbital
exenteration. The earlier the treatment is
started, the better the prognosis. The disease
still carries a mortality rate of 50–80%.
32
Investigation
1. Blood tests may show elevated fungus-specific IgE levels in patients with allergic
fungal sinusitis.
2. Microbiology of any secretions and tissue to
identify fungus and direct antimicrobial
therapy.
3. Biopsy.
33
Investigation
4. CT- scan of the sinuses may show
microcalcification of opaque fungal mass in the
non-invasive form due to accumulated heavy
metals, e.g. calcium, manganese. There may be
evidence of bone expansion. The invasive type,
however, will show evidence of bone destruction
with spread of disease outside the sinuses. MRI
scanning may further help delineate fungal mucin
from reactive inflammation .
34
Fungal Rhinosinusitis
35
Fungal Rhinosinusitis
36
NASAL POLYPS
37
Aetiology
In certain predisposed individuals, any inflammatory nasal condition can lead to marked swelling of the sinus and nasal mucosa. This seems particularly to affect the mucosa in the region of the middle turbinate and middle meatus. When this swelling becomes sufficiently pronounced, polyp formation may result. The initiator of this inflammatory response may be chronic infection, allergy or intrinsic rhinitis, but in some cases the cause is unknown.38
Pathology
Pathologically, polyps demonstrate marked oedema of the connective tissue stroma, which also contains a variety of inflammatory mediators such as histamine, prostaglandins and leukotrienes. There is a marked eosinophilic and histiocytic infiltrate and the epithelium displays goblet cell hyperplasia and in some areas a squamous cell metaplasia. A polyp forms when the oedematous stroma ruptures and herniates through the basement membrane.39
Pathology
Nasal polyps are rare in childhood, and if they occur one should suspect cystic fibrosis or immune deficiency. Recurrence is common after surgical removal, although it may often be delayed for many years. It is more likely and tends to occur sooner in those patients with coexistent asthma and aspirin hypersensitivity.40
Clinical features
Nasal polyps may be asymptomatic, but even when small most patients complain of a feeling of congestion or obstruction high in the nose and a hyponasal quality to their speech. As the polyps enlarge there is associated worsening of nasal obstruction and usually a profuse watery nasal discharge causing rhinorrhoea or a postnasal space drip. At the same time patients frequently complain of loss of taste and smell.
41
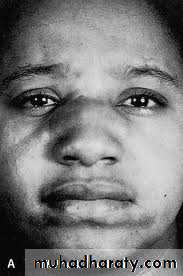
Clinical features
Headaches, pressure sensation in the face and sinusitis may occur. In severe cases the polyps may be visible at the external nares and widening of the intercanthal distance may occur. The polyps are insensitive. A history of epistaxis or contact bleeding should raise suspicion of the possibility of a neoplastic polyp. Clinical examination of the nose is not complete without an endoscopic examination (rigid or flexible), as without it small polyps in the middle meatus may be missed.42
43
Investigations
RAST test.CT Scan
44
Management
Medical. In patients with small polyps it is worth trying medical therapy. This consists of intranasal steroids, as either drops or spray, with the addition of oral antihistamines if there is an allergic element. Short courses of low-dose oral steroids may be extremely useful in those patients with particularly aggressive polyposis.45
Management
Surgical. If sufficiently troublesome surgical clearance can provide marked symptomatic improvement. The majority of surgeons would now probably undertake this procedure endoscopically. With appropriate preparation of the operative field and the excellent vision afforded by the endoscope, an exceptionally thorough clearance can be undertaken. This is now often augmented with the aid of powered suction and microdebriders.
46
47
Prognosis ?
48
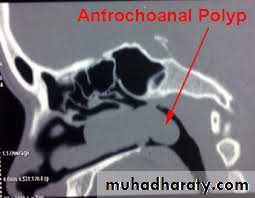
Antrochoanal polyp
The antrochoanal polyp is uncommon. It is typically unilateral and commences as oedematous lining from the maxillary sinus. This lining prolapses through the ostium into the nasal cavity and enlarges towards the posterior choana and nasopharynx.49
Antrochoanal polyp
50
Antrochoanal polyp
The patient, commonly a young adult, complains of unilateral nasal obstruction, which is worse on expiration owing to the ball valve-like effect of the polyp in the posterior choana. If sufficiently large, it may produce bilateral obstruction and cause otological symptoms as a result of blockage of the Eustachian tube orifice.51
Antrochoanal polyp
52
Antrochoanal polyp
Diagnosis :Endoscope + CT scan
53
Antrochoanal polyp
Treatment is by complete nasal avulsion with removal of the antral portion. This can usually be achieved endoscopically. An intranasal antrostomy is the usual approach. Failure to remove the antral lining may result in a recurrence. With recurrence a Caldwell-Luc procedure may be required to clear the sinus.54
Antrochoanal polyp
55