PeriOrbital and orbital Infections
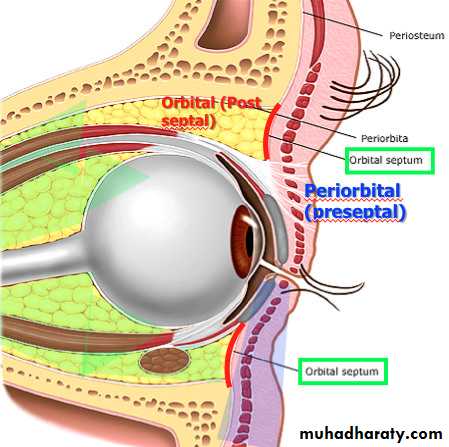
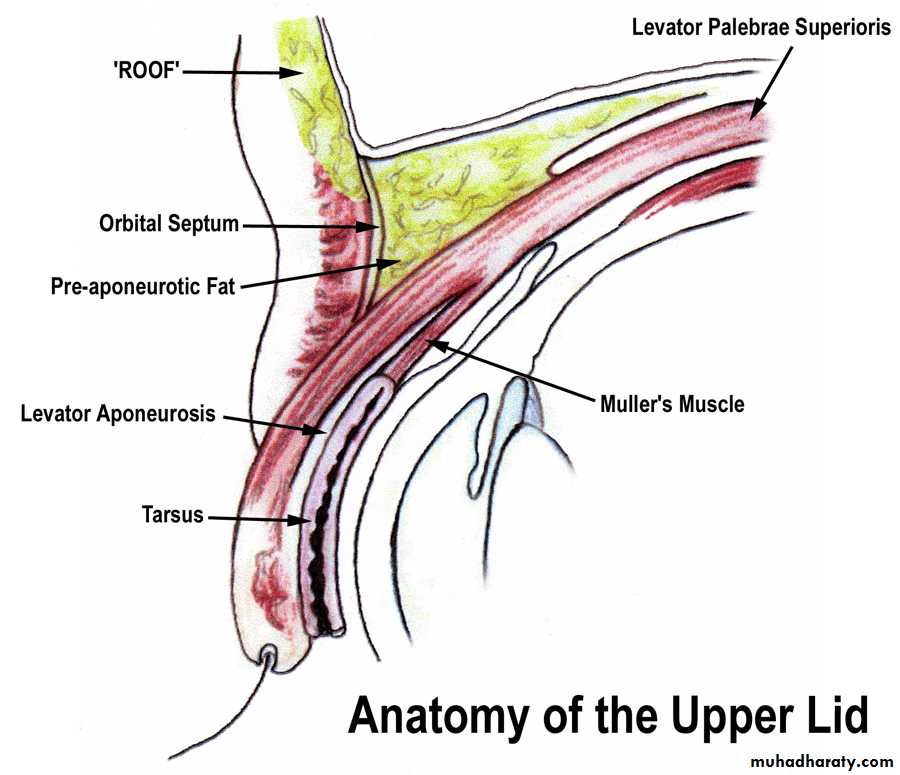
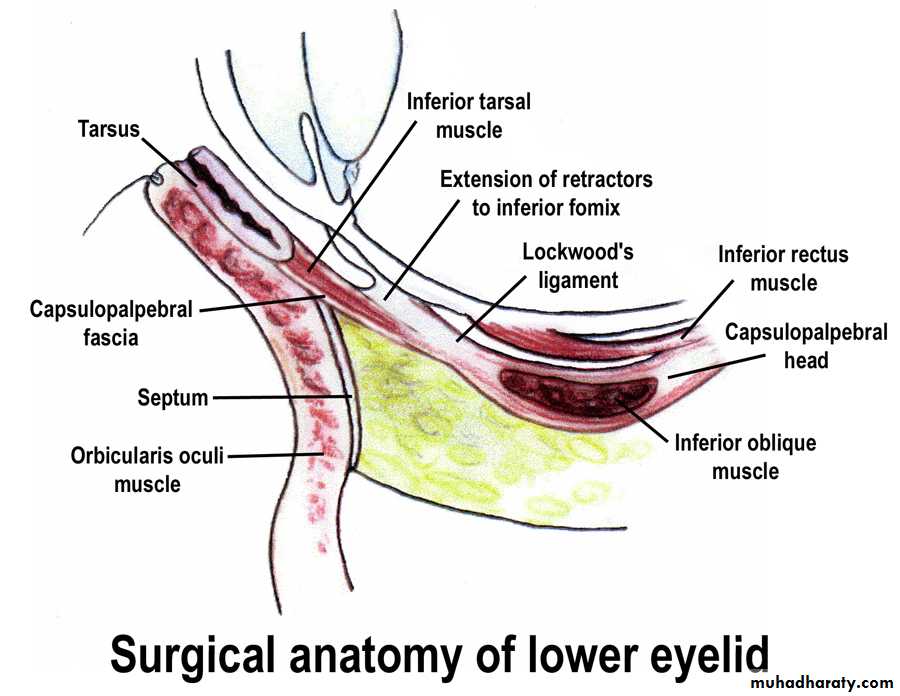
Orbital AnatomyOrbital Septum
Fibrous Membrane separating the orbital and preseptal compartmentUpper Eyelid
Extends from the periosteum of the orbital rim to the levator aponeurosisLower Eyelid
Extends from the periosteum of the orbital rim to the inferior border of the tarsal plateRoutes of Infection Extension to lids and orbit
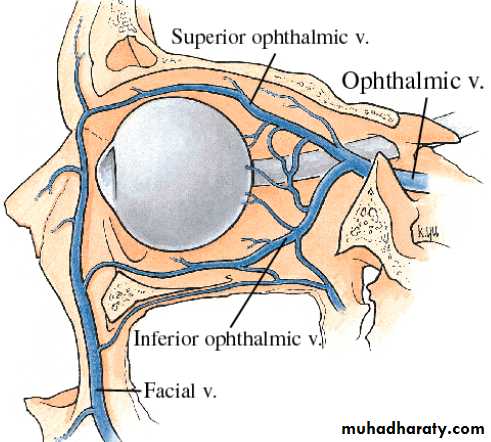
Indirect spread• venous drainage system shared by cranial and midface structures
• multiple anastomoses and valveless System
Routes of Infection Extension to lids and orbit
Direct spread• Ethmoid sinus through lamina papyracea - contained subpereosteal abscess or progressive orbital involvement
• frontal and maxillary sinus
• Orbital floor
• Odontogenic – maxillary sinus - orbit
Preseptal cellulitis
• An infection or inflammatory process of the eyelids and periorbital structures• Occurs anterior to and contained by the orbital septum
Orbital cellulitis
• Occurs posterior to the orbital septum
• Involves the soft tissue within the bony orbit
Cellulitis - Common Etiologies
• Spread from adjacent structures – Skin and Sinuses• Direct inoculation following Trauma
• Bacterial spread Upper Respiratory or Middle Ear
Preseptal – Associated factors
• Hordeola and Chalazia• Impetigo/Erysipelas
• Blepharitis
• Conjunctivitis
• Canaliculitis
• Dacryocystitis
• Viral dermatitis – herpes simplex & herpes zoster
Eyelid swelling both causes and results from impeded venous flow and lymphatic drainage – leading to self-propagating process
Chalazion
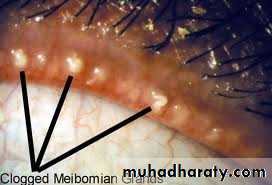
Most common inflammatory Lesion of eyelid
Blocked meibomian gland
Inflammatory nodule/cyst
Lipogranulomatous
Not infectious
Typically not painful
Chalazion
Managed by warm compresses and massageExcision/ Steroid Injection
Chalazion
PreventionRoutine use of warm compresses
Lid margin Cleansing
Low dose oral doxycycline
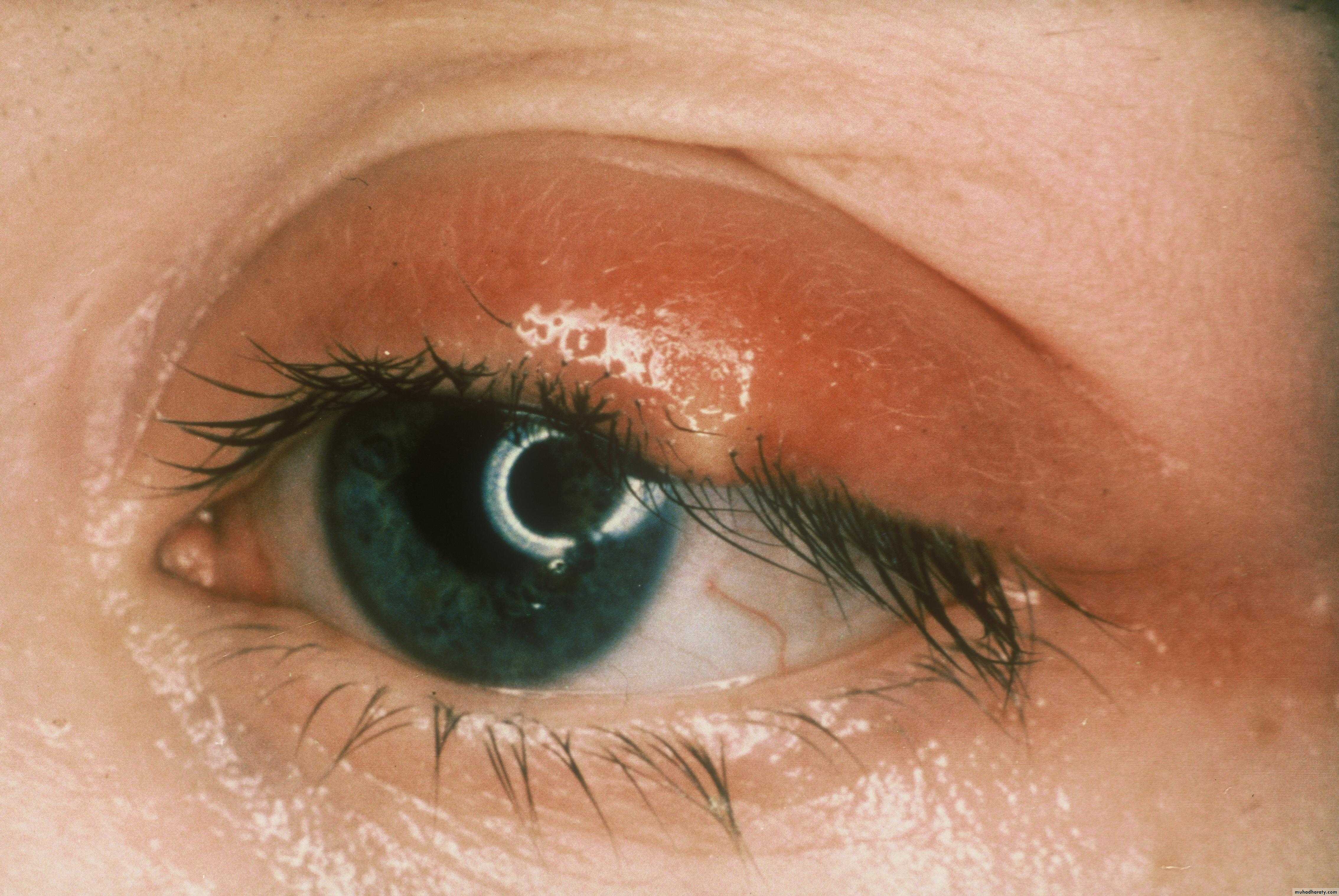
Erysipelas
Superficial cellulitisUsually group A Strep
Intensely erythematous with sharply demarcated border
hordeolum
Bacterial Infectionmebomian gland or ciliary glands (zeiss or moll)
Internal or external
Typically painful
May lead to preseptal cellulits
hordeolum
ManagementStaphylococcal - most common etiology
Systemic Antibiotics
Lance/Drain
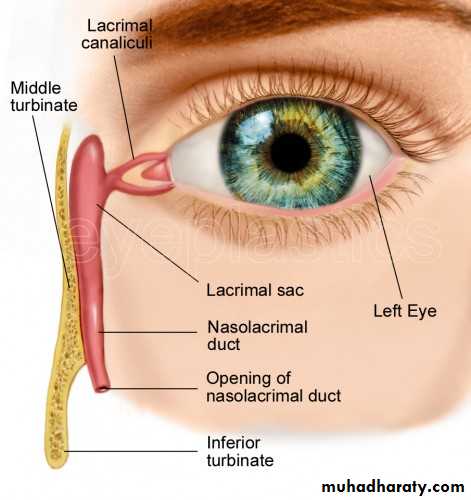
dacryocystitis
Pain, redness and swelling below the medial Canthal tendonTypically associated with blockage of the nasolacrimal System
Tear stasis and retention → secondary bacterial infection
dacryocystitis
ManagementAntibiotics – systemic
Warm compresses
Drainage
dacryocystitis
ManagementOral antibiotics
Gram Positive bacteria most common
Consider Gram neg in diabetics, immunocompromised patients
IV antibiotics when severe/associated with orbital cellulitis
drainage of abscess
Herpes Zoster Dermatoblepharitits
Recurrence or reactivation of Varicella Zoster virusBurning, Stabbing pain of forehead/scalp
Vesicular Rash in V1 distribution
Herpes Zoster Dermatoblepharitits
treat with antiviralsAcyclovir if identified within 72 hours of skin lesion onset
treat with antivirals
Acyclovir if identified within 72 hours of skin lesion onsetPreseptal Cellulitis
Other Causes of Eyelid Swellingcontact dermatitis
Insect bites
Thyroid Eye Disease
Dacryoadenitis
Preseptal Cellulitis
Other Causes of Eyelid Swelling
contact dermatitis
Thickened, Erythematous, scaly skin
•
Preseptal Cellulitis
Other Causes of Eyelid SwellingInsect bites
•
Preseptal Cellulitis
Other Causes of Eyelid SwellingThyroid Eye Disease
Periorbital edema
Preseptal Cellulitis
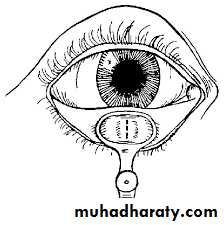
Other Causes of Eyelid SwellingDacryoadenitis
Inflammation of lacrimal gland
Superotmeporal pain, swelling, erythema
“S” shaped lid deformity
•
Preseptal management
Typically outpatient =oral antibioticsAll children < 1 year old should be hospitalized with IV antibiotics
Culture when able – more likely after traumatic insult
Most common bacteria involved for adults: Staph aurues and Strep pyogenes
Most common for children: h influenza type b and strep pneumonia
If abscess develops it should be incised and drained
Preseptal Management
• Teenagers and Adults
• Usually arises from superficial source (trauma, chalazion)
• Treated with oral antibiotics
• Commonly Penicillinase-resistant penicillin or Bactrim
• Image if:
• source of infection not determined
• not responding quickly to treatment
• orbital process suspected
Preseptal Management
• Children• The most common cause is underlying sinusitis
• Work up with CT quickly if no source of direct inoculation easily identified
• Hospitalize and IV antibiotics
Orbital Cellulitis
Ophthalmic SignsProptosis
Motility Disturbance
Pronounced edema and erythema
Impaired vision with afferent pupil defect
Conjunctival chemosis and hyperemia
Reduced corneal sensation
Orbital cellulitis
Sources of infection are similar to preseptalExtension of sinus disease
Penetrating trauma
Infected adjacent structures
Other uncommon sources
Scleral buckles, Aqueous drainage devices, endophthalmitis
Orbital Cellulitis
Noninfectious causes of orbital inflammatory diseaseInflammatory and Autoimmune
thyroid ophthalmopathyorbital pseudotumor
lymphoma
dermatomyositis-polymyositis
Wegener granulomatosis
Sjogren syndrome
Orbital Cellulitis
Noninfectious causes of orbital inflammatory diseaseVascular
orbital venous malformation
cavernous sinus thrombosis
Arteriovenous fistula
superior vena cava syndrome
Orbital Cellulitis
Noninfectious causes of orbital inflammatory diseaseNeoplasms of orbit and lacrimal gland
pediatric: rhabdomyosarcoma, leukemia, metastatic neuroblastoma, retinoblastoma
adult: lymphoma
Orbital Cellulitis
> 90% of all related to underlying sinus diseaseIn children usually single organism from sinus (s aureus or strep pneumonia)
Adolescents and adults have more complex bacteriology (often 2-5 organisms)
trauma – Gram - rods
Dental – mixed, aggressive aerobes and anaerobes
Immunocompromised/Diabetics - fungi
Orbital cellulitis
Laboratory studies
CBC
Nasal swab if purulent material
Blood cultures
Lumbar puncture if meningeal signs present
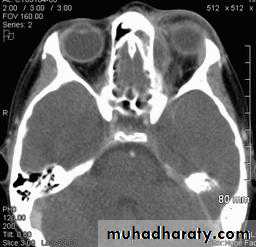
Orbital cellulitis
Imaging StudiesOrbital CT
Thin, axial and coronal, without contrast
Include orbits, paranasal sinuses, frontal lobes
If neurologic involvement include the head when imaging
Orbital Cellulitis
Significant morbidity if not appropriately treatedorbital apex syndrome
blindness
cavernous sinus thrombosis
cranial nerve palsies
meningitis
intracranial abscess
Orbital Cellulitis
Medical ManagementAdmit for IV antibiotics
cephalosporin – Ampicillin or Pipercillin
Vancomycin for MRSA
Clindamycin for anaerobic coverage
Nasal decongestants
Transition to outpatient oral antibiotics treatment for 1-3 weeksOrbital Cellulitis
Surgical ManagementIf orbital abscess present
Early drainage of involved sinus
if orbital signs progressing
Feature
PreseptalOrbital
Proptosis
Absent
Present
Motility
Normal - pain
Decreased + pain and double vision
Vision
Normal
Reduced – check vision and color vision
Pupillary Reaction
Normal
+/- APD – check swinging flashlight test
Chemosis
Rare
Common
Corneal Sensation
Normal
May be reduced
Systemic Signs
Absent/Mild
Commonly severe (Fever/Leukocytosis)
Differentiating features of cellulitis