Infectious diseaseMosul medical college2016-2017
Dr. Athl HumoCASES
Q1/ A 8 years old child is presented with fever for 24 hours followed by appearance of pruritic maculopapular rash that rapidly changes to vesicles with maximum distribution over the trunk. The child is generally well.
• What is the most probable diagnosis?
• What is the causative agent?
• Mention three important complication?
Q2/ A 10-year-old patient presented to you with fever, muscular pain (especially in the neck),headache, and malaise. He describes the area from the back of his mandible toward the mastoid space as being full and tender and that his earlobe on the affected side appears to be sticking upward and outward. Drinking sour liquids causes much pain in the affected area.
• What is the diagnosis?
• What are the complications?
• How can prevent such disease?
Q3/An 8-year-old sickle-cell patient arrives at the emergency room (ER) in respiratory distress. Over the previous several days, the child has become feverish, progressively tired and pale. The child’s hemoglobin concentration in the ER is 3.1 mg/dL.
• What is the most likely diagnosis?
• What are others hematological abnormalities could be seen?
• How can confirm the diagnosis?
• Outline the treatment?
Q4/ A previously healthy 8-year-old boy has a 3-week history of low-grade fever of unknown source, fatigue, weight loss, myalgia, and headaches. On repeated examinations during this time, he is found to have developed a heart murmur, petechiae, and mild splenomegaly.
• What is the likely diagnosis?
• What are the investigation needed to done?
• What is the treatment?
LABORATORY
• Positive blood culture• Elevated ESR; may be low with HF or RF.
• Elevated CRP
• Anemia
• Leukocytosis
• Immune complexes
• Hypergammaglobulinemia
• Hypocomplementemia
• Cryoglobulinemia
• Rheumatoid factor
• Hematuria
• Renal failure: azotemia, high creatinine (glomerulonephritis)
• CXR: bilateral infiltrates, nodules, pleural effusions
• Echocardiographic evidence of valve vegetations, prosthetic valve dysfunction or leak, myocardial abscess, new-onset valve insufficiency
Treatment of ie
• stabilized with supportive therapies.
• High doses of bactericidal antibiotics are required for an extended period of treatment (4 to 8 weeks).Vancomycin or a β-lactam antibiotic, with or without gentamicin, for a 6-week course is the most common regimen.
Q5/ A 14-year-old boy is seen in the ER because of a 3-week history of fever between 38.3°C and 38.9°C, lethargy, and a 2.7-kg weight loss. Physical examination reveals marked cervical and inguinal adenopathy, enlarged tonsils with exudate, small hemorrhages on the soft palate, a WBC differential that has 50% lymphocytes (10% atypical), and a palpable spleen 2 cm below the left costal margin.
• What is the diagnosis?
• What are the complications?
• What is the prognosis?
• What is the treatment?
Q 6/ two years old child presents with a 3-day history of malaise, fever to 41.1°C, cough, coryza, and conjunctivitis. He then develops the erythematous, maculopapular rash pictured. He is noted to have white pinpoint lesions on a bright red buccal mucosa in the area opposite his lower molars.
• What is the most likely diagnosis?
• What are the lab. investigations help in diagnosis?
• What are the complications?
• How can prevent the disease?
Lab for measle
The diagnosis of measles is almost always based on clinical and epidemiologic findings.Laboratory findings in the acute phase include Leukopenia.
Serologic confirmation is most conveniently made by:
identification of immunoglobulin IgM antibody in serum. IgM antibody appears 1-2 days after the onset of the rash and remains detectable for about 1 mo.
demonstration of a 4-fold rise in IgG antibodies in acute and convalescent specimens.
Viral isolation from blood, urine, or respiratory secretions can be accomplished by culture.
PCR
Complications of measle
Otitis media is the most common complication of measles infection.
Interstitial (measles) pneumonia or may result from secondary bacterial infection. Persons with impaired cell-mediated immunity may develop giant cell (Hecht) pneumonia, which is usually fatal.
Myocarditis and mesenteric lymphadenitis are infrequent complications.
Encephalomyelitis (1 to 2 per 1000 cases) usually occurs 2 to 5 days after the onset of the rash. Early encephalitis probably is caused by direct viral infection of brain tissue, whereas later onset encephalitis is a demyelinating and probably an immunopathologic phenomenon.
Subacute sclerosing panencephalitis is a late (after 8 to 10 years) neurologic complication of slow measles infection that is characterized by progressive behavioral and intellectual deterioration and eventual death.There is no effective treatment.
prevention
Exposure of susceptible individuals to patients with measles should be avoided during this period.In hospitals, standard and airborne precautions should be observed for this period.
Live measles vaccine prevents infection and is recommended as measles, mumps, and rubella (MMR) for children at 12 to 15 months and 4 to 6 years of age.
Susceptible household contacts with a chronic disease or who are immunocompromised should receive postexposure prophylaxis with measles vaccine within 72 hours of measles exposure or immunoglobulin within 6 days of exposure.
Q7/ A newly delivered infant is noted to be microcephalic, has cataracts, a heart murmur, and hepatosplenomegaly. An echocardiogram reveals, patent ductus arteriosus and peripheral pulmonary artery stenosis. The mother had no antenatal care.
• What is the most likely diagnosis?
• What is the treatment?
Q8 /A 14-year-old girl awakens with a mild sore throat, low-grade fever, and a diffuse maculopapular rash. During the next 24 hours, she develops tender swelling of her wrists and redness of her eyes. In addition, her physician notes mild tenderness and marked swelling of her posterior cervical and occipital lymph nodes. Four days after the onset of her illness, the rash has vanished.
• What is the most likely diagnosis?
Q9 / patient presents to the emergency center with a 6-hour history of fever to 38.9°C (102°F). Her mother reports that the patient appeared to be feeling poorly, that she had been eating less than normal, and that she vomited once. About 2 hours prior to arrival at the ER, the mother states that she noted a few purple spots scattered about the body on the patient, especially on the buttocks and legs. On the 30-minute ride to the ER, the purple areas spread rapidly and became coalesced in areas, and the patient is now obtunded.
• What is the most likely diagnosis?
• How confirm the diagnosis?
• What is the treatment?
Q10/ A 2-month-old infant comes to the emergency center with fever for 2 days, emesis, a petechial rash, and increasing lethargy. In the ambulance he had a 3-minute generalized tonic/clonic seizure that was aborted with lorazepam. He does not respond when blood is drawn or when an IV is placed, but he continues to ooze blood from the skin puncture sites. On examination, his anterior fontanelle is open and bulging. His CBC shows a WBC of 30,000 cells/μL with 20% band forms. Which of the infant’s problems listed below is a contraindication to lumbar puncture?
• Uncorrected bleeding diathesis
• Bulging fontanelle
• Dehydration
• History of recent seizure
• Significantly elevated WBC count consistent with bacteremia
Q 11/ A 2-year-old child is admitted to your hospital team. The child’s primary care doctor has been following the child for several days and has noted her to have had high fever, peeling skin, abdominal pain, and a bright red throat. You are concerned because two common pediatric problems that could explain this child’s condition have overlapping presenting signs and symptoms. Which of the following statements comparing these two diseases in your differential is true?
• Neither has cardiac complications.
• Serologic tests are helpful in diagnosing both.
• Only one of the diseases has mucocutaneous and lymph node involvement.
• Pharyngeal culture aids in the diagnosis of one of the conditions.
• A specific antibiotic therapy is recommended for one of the conditions, but only supportive care is recommended for the other.
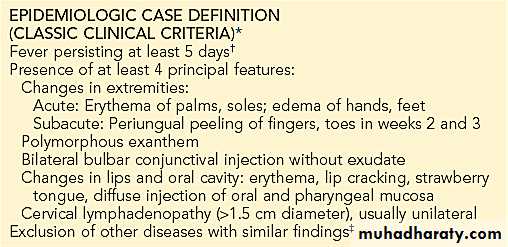
The two conditions in consideration are Kawasaki disease and scarlet fever caused by a group A β-hemolytic streptococci.
Kawasaki disease is an acute febrile illness of unknown etiology and shares many of its clinical manifestations with scarlet fever. Scarlatiniform rash, desquamation, erythema of the mucous membranes that produces an injected pharynx and strawberry tongue, and cervical lymphadenopathy are prominent findings in both.
Erythrogenic toxin-producing group A β-hemolytic streptococci is the agent responsible for scarlet fever. Isolation of the organism from the nasopharynx and a rise in antistreptolysin titers will confirm the diagnosis. Serologic tests for a variety of infectious agents, both viral and bacterial, have been negative in Kawasaki disease.
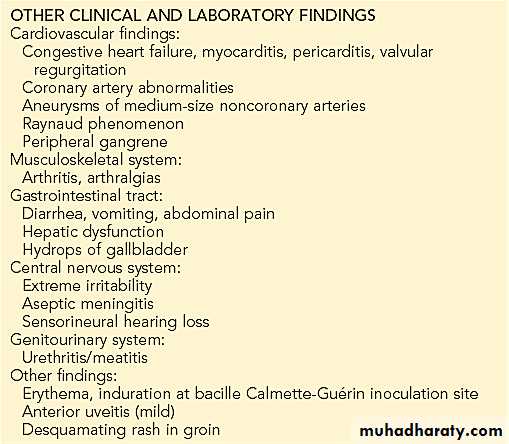
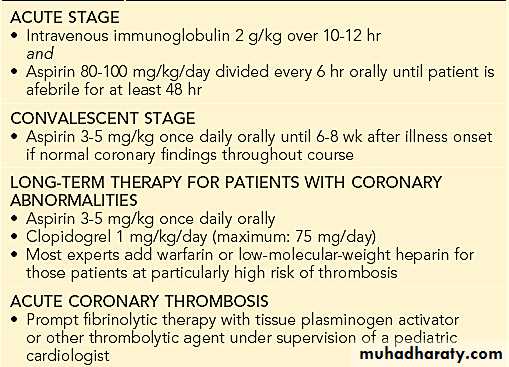
The most serious complication of Kawasaki disease and scarlet fever is cardiac involvement. Rheumatic heart disease is a serious sequela of streptococcal pharyngitis, which can be prevented by appropriate treatment with penicillin. Coronary artery aneurysm and thrombosis are the most serious complications of Kawasaki disease.
The current approach to treatment of Kawasaki disease, which includes specific therapy with aspirin and IV γ-globulin administered within a week of the onset of fever, appears to lower the prevalence of coronary artery dilatation and aneurysm and to shorten the acute phase of the illness.
Kawasaki Disease
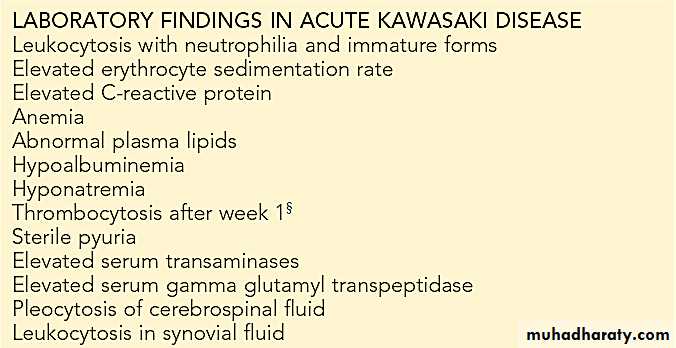
Kawasaki disease (KD), formerly known as mucocutaneous lymph node syndrome and infantile polyarteritis nodosa, is an acute febrile illness of childhood seen worldwide with the highest incidence occurring in Asian children. KD is a vasculitis (predominantly affects the medium-size arteries) with a predilection for the coronary arteries, although other arteries, such as the popliteal and brachial arteries, can also develop dilation.Clinical and Laboratory Features of Kawasaki Disease
*Patients with fever at least 5 days and <4 principal criteria can be diagnosed with Kawasaki disease when coronary artery abnormalities are detected by 2-dimensional echocardiography or angiography.
†In the presence of ≥4 principal criteria, Kawasaki disease diagnosis can be made on day 4 of illness. Experienced clinicians who have treated many patients with Kawasaki disease may establish diagnosis before day 4.
§ Some infants present with thrombocytopenia and DIC.
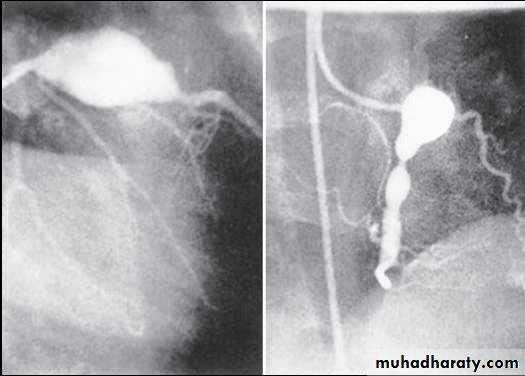
Coronary angiogram demonstrating giant aneurysm of the left anterior descending coronary artery (LAD) with obstruction and giant aneurysm of the right coronary artery (RCA) with an area of severe narrowing in 6 yr old boy.
Treatment of Kawasaki Disease
Q12/ An 18-month-old child presents to the emergency center having had a brief, generalized tonic-clonic seizure. He is now postictal and has a temperature of 40°C (104°F). During the lumbar puncture (which ultimately proves to be normal), he has a large, watery stool that has both blood and mucus in it.
• What is the most likely diagnosis in this patient?
• How can confirm the diagnosis?
• What is the treatment?