1
PATHOGENICITY OF MICROORGANISMS
Some microorganisms are :
1- Harmless microorganism, as normal flora
2- Harmfull microorganism, as pa
t
hogenic.
A pathogenic microorganism is defined as
one that causes or is capable of causing disease by
production of toxic, or by colonization on the skin
or mucous membrane, or by being introduced into
a normally sterile body site, or by infection of an
immunocompromised host.
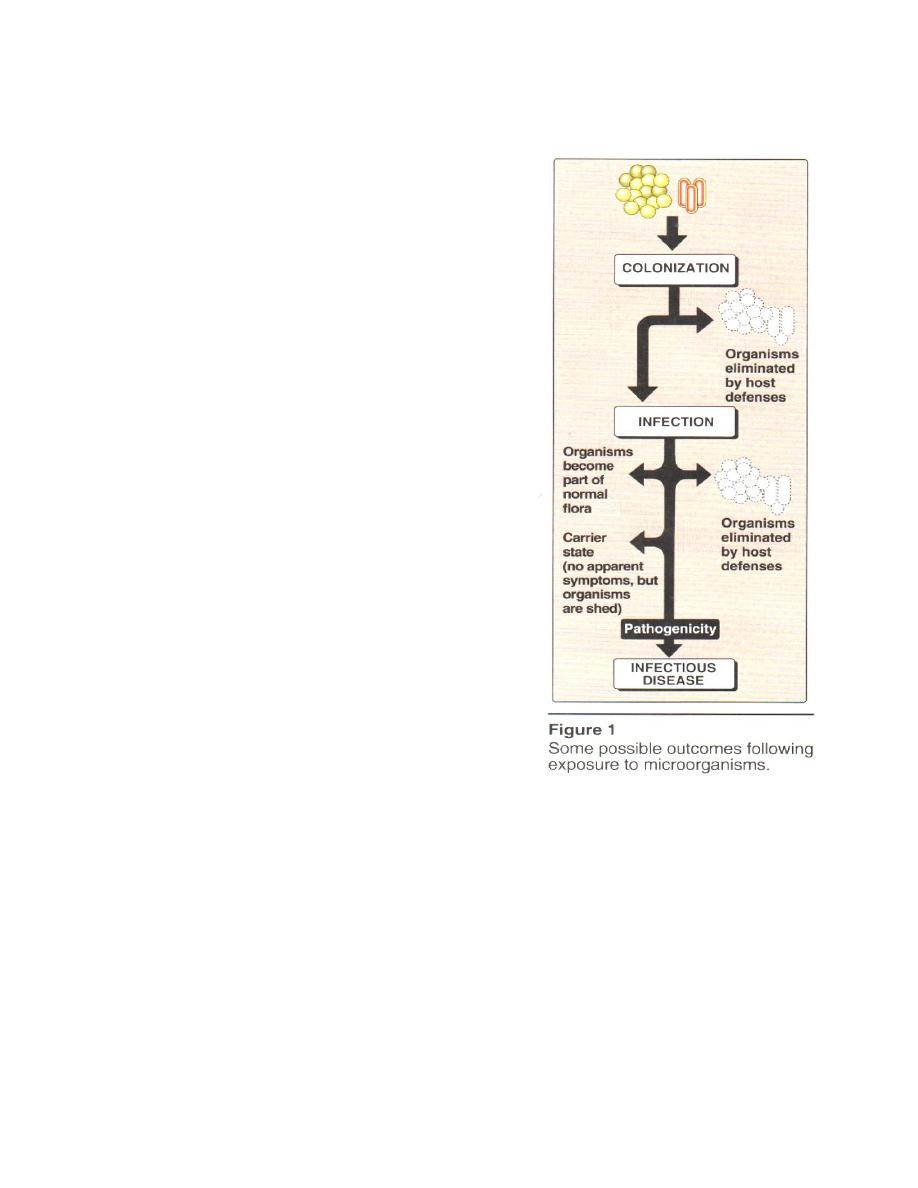
Microbial colonization may result in;-
1- elimination of the microorganisms without
affecting the host.
2- infection in which the organisms multiply
and causes the host to react by making an
immune or other type of response.
3- Infectious
diseases
occurs
when
the
organism causes tissue damage and impaired
of the body function.
BACTERIAL PATHOGENESIS
The in
f
ec
t
ious process can be divided in
t
o several
stages:
1- Entry into the host, with evasion of host primary defenses
2- Adhesion of the microorganism to host cells
3- Propagation of the organism
4- Damage to host cells by bacterial toxins or an inflammatory response of
'
the host
5- Evasion of host secondary defenses
Pathogenicity of a microorganism depends on its success in completing some
or all of these stages.
The characteristics of pathogenic microorganism are virulence factors , antigenic
switching and infections in human populations.
2
A. Virulence factors
Virulence factors are those characteristics of a
bacterium
t
hat enhance its pathogenicity, that is, the ability to
cause disease. The more important classes of virulence factors
are:
1- Entry into the host
2- Adherence to host cells
3- Invasiveness
4- Bacterial toxins
1- Entry into the host:
By one of several parts: the respiratory tract,
gastrointestinal tract (GI), urogenital tract, or skin that has
been cut, punctured, or burned. Once entry is achieved, the
pathogen must overcome a diversity of host defenses before it
can establish itself, include primary host defenses:
1- phagocytosis,
2- the acidic environments of the stomach and urogenital
tract.
3- various hydrolytic and proteolytic enzymes found in the
saliva, stomach, and small intestine.
Bacteria that have an outer polysaccharide capsule (
for example Streptococcus pneumonia and
Neisseria meningitidis) have a better chance of
surviving these primary host defenses.
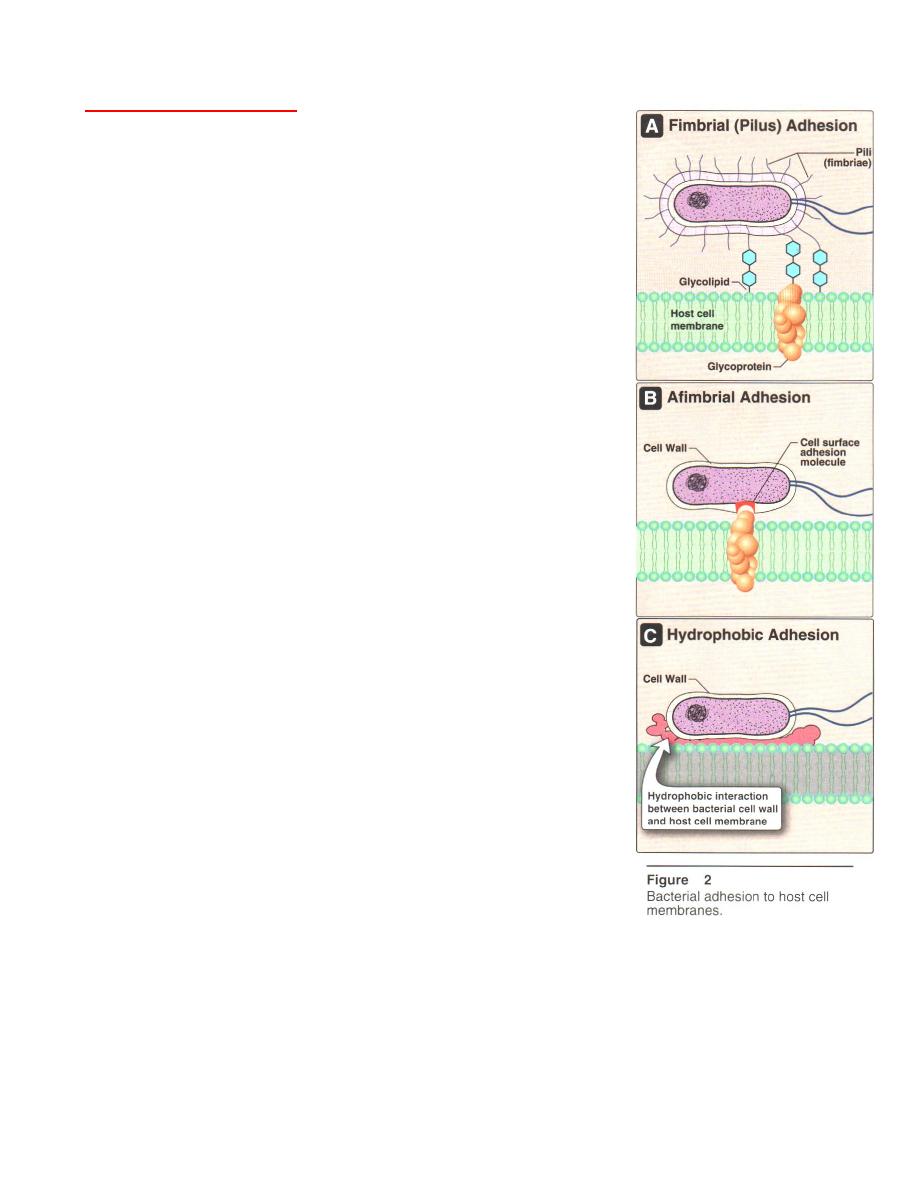
2- Adherence to host cells:
This done by: 1 pili like Escherichia coli, or fimbriae
like group A Streptococcus , 2 cell surface adhesion
molecules , 3 particularly hydrophobia cell walls (Figure 2).
In each case, adherence enhances virulence by preventing the bacteria from being
carried away by mucus, or washed from organs with fluid flow (the urinary and the GI
tracts) and allows each attached bacterial cell to form a microcolony.
Neisseria gonorrhoea in which strains that lack pili are not pathogenic .
3
3- Invasiveness:
Invasive bacteria are those that can enter host
cells or penetrate mucosal surfaces, spreading from
the initial site of infection, by several bacterial
enzymes, like collagenase and hyaluronidase,
which degrade components of the extracellular
matrix, providing the bacteria with easier access to
host cell surfaces. Invasion is followed by
inflammation, depending on the organism, which can
be either :
- pyogenic (involving pus formation contains
neutrophils) .
- granulomatous (having nodular lesions
contain
fibroblasts,
lymphocytes,
and
macrophages).
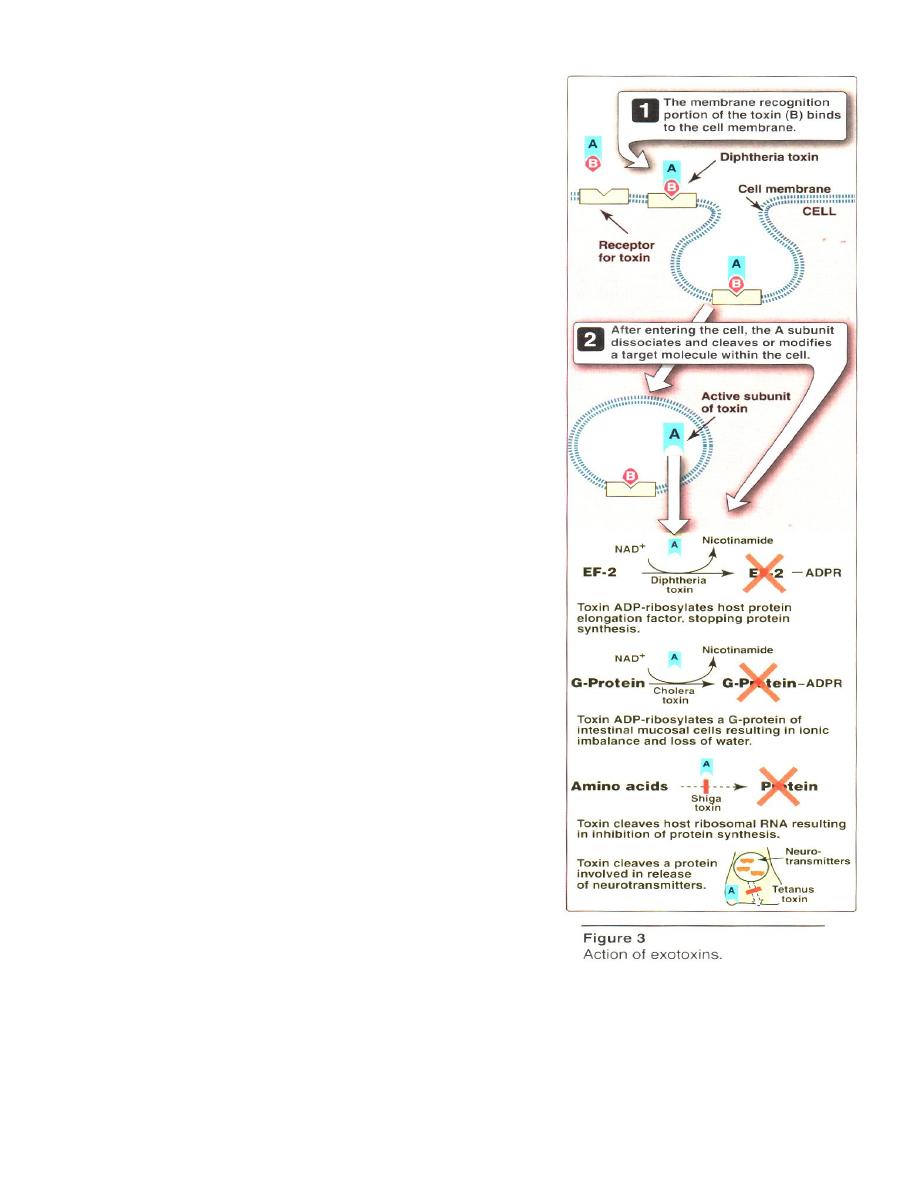
4- Bacterial toxins:
Some bacteria cause disease by producing
toxins, the exotoxins and the endotoxins.
a. Exotoxins:
are proteins , are secreted by both G+ and
G –bacteria, are heat labile or heat stable, find in
G+ or G- bacteria , caused septic shock syndrome
but not severe ,e.g. diphtheria, shigella, cholera, ,
tetanus exotoxin . one microgram of tetanus
exotoxin (produced by Clostridium tetani) can kill an
adult human.
Exotoxin. proteins have two polypeptide
components (Figure 3) ; one is responsible for
binding to the host cell, and one is responsible for the
toxic effect. Diphtheria toxin (produced by Corynebacterum diphtheria) is an enzyme
that blocks protein synthesis.
Most exotoxins are inactivated by heating (60°C), heat labile toxin (LT),
Staphylococcal enterotoxin and E. coli are heat-stable toxin (ST).

4
Treatment with dilute formaldehyde destroys the toxic activity of most exotoxins
but not their antigenicity. Formaldehyde-inactivated toxins, called toxoids, are useful in
preparing vaccines.
Exotoxin proteins are encoded by genes carried on plasmids or temperate
bacteriophages.
b. Endotoxins:
are lipopolysaccharides, are not secreted, but are integral components in the
outer membranes of the cell walls of G- bacteria released into the host's circulation
following bacterial cell lysis , are heat-stable , find in of G- but not G+ bacteria,
caused severe septic shock syndrome. The outer membranes consist of LPS:
- Polysaccharide O (somatic antigen), which its from the exterior cell surface.
- lipid A that faces the cell interior, responsible for the toxicity of this molecule.
The main physiologic effects of LPS endotoxins are fever, shock, hypotension,
and thrombosis, called as septic shock. These effects are produced indirectly by
activation of macrophages ,complement and coagulation cascade, with the release
of cytokines. Death can result from multiple organ failure.
In G+ bacteria their cell wall, peptidoglycan, can cause a shock syndrome similar
to that caused by LPS, but usually not as severe. Because the peptidoglycan fragments of
G+ bacteria are chemically so different from LPS, and are also less potent.
B. Antigenic switching
A successful pathogen must evade the host's immune system (that recognizes
bacterial surface antigens) change its surface antigens by several mechanisms:
1- Phase Variation,
is the ability of certain bacteria to turn off and turn on the
expression of genes coding for surface antigens.
2- Antigenic Variation,
is the modification of the gene for an expressed surface
antigen, by genetic recombination with one of many variable unexpressed DNA
sequences, so the expressed surface antigen can assume many different antigenic
structures.
5
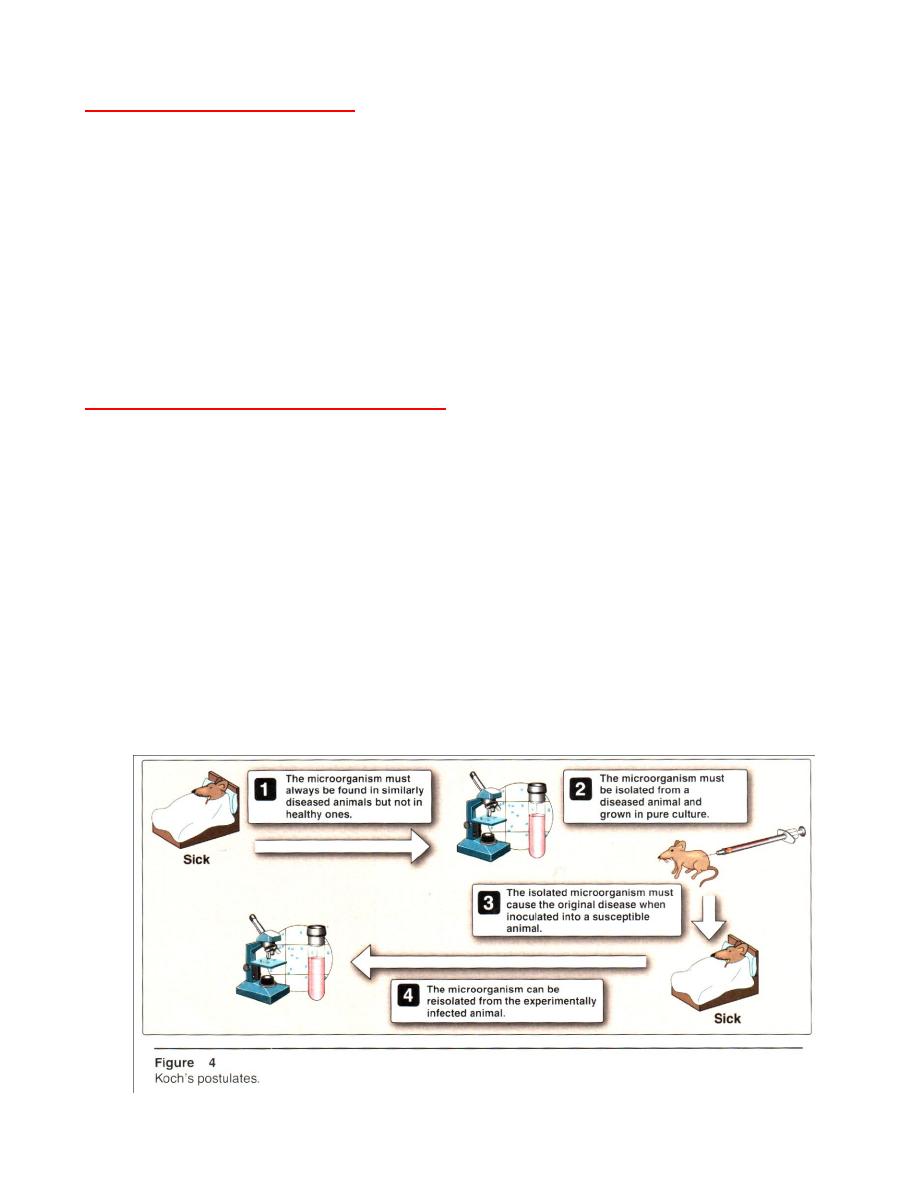
C. Which is the pathogen?
If a particular microorganism is isolated from infected tissue, the organism could
be a harmless member of the normal skin flora or an opportunistic pathogen (is an
organism that is unable to cause disease in healthy, but cause disease in
immunocompromised individuals ).
A nineteenth century German microbiologist, Robert Koch, recognized this
dilemma, and defined a series of criteria (
Koch's postulates
) by which the identity of
the causative microbial agent of a disease can be confirmed (Figure 4) (this protocol
fails if the causative organism cannot be cultured in vitro).
D. Infections in human populations
Bacterial diseases may be :
-
communicable
from person to person (For example, cholera caused by
Vibrio cholerae is easily spread)
-
noncommunicable
not from person to person (For example botulism is caused by
Clostridium botulinum because only those people who ingest the botulinum
exotoxin are affected). Highly communicable diseases, such as cholera, are said to
be contagious, and tend to occur as localized epidemics in which the disease
frequency is higher than normal. When an epidemic becomes worldwide, it is
called a pandemic, such as the 1918 influenza because the human population has
never been exposed to, and, thus, has no immunity against, the specific strain of
influenza virus.
