Factors determining blood pressure :
In order to have BP there must be a cardiac out put and a resistance to blood flow in the systemic circulation.BP = cardiac out * peripheral resistance
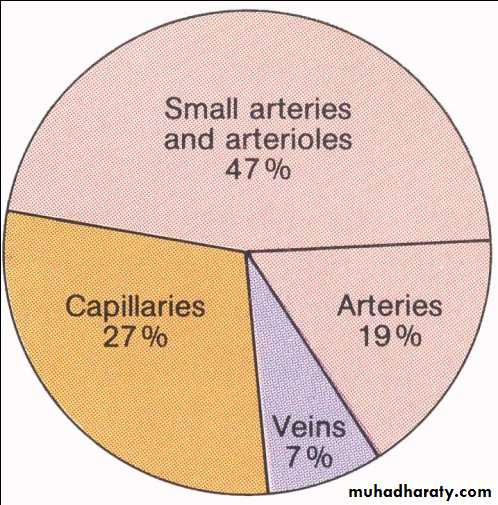
But at rest cardiac out put is constant and as a result the BP will determine principally by the peripheral resistance, which lies mainly in the small arteries of the body (arterioles) which is the greatest resistance to blood flow.
The resistance of flow depends upon;
Diameter of blood vessels, especially arterioles.
Partially to the blood viscosity (hematocrit).
Vascular resistance affected by autonomic nervous system, adrenalin & angiotensin cause vasoconstriction (they are called vasopressors).
The rennin-angiotensin-aldosterone mechanism is concerned with the long –term regulation of BP
The capillaries are even smaller vessels than arterioles but although each individual capillary will offer a higher resistance than arterioles.
There is a large number of capillaries in parallel supplied by each arteriole, as a result there is a large alternative pathways for the blood to take in to passage from an arteriole to the veins. So capillary net work does not offer such resistance to blood flow as arterioles
BLOOD PRESSURE DISTRIBUTION THROUGHOUT SYSTEMIC CIRCULATION
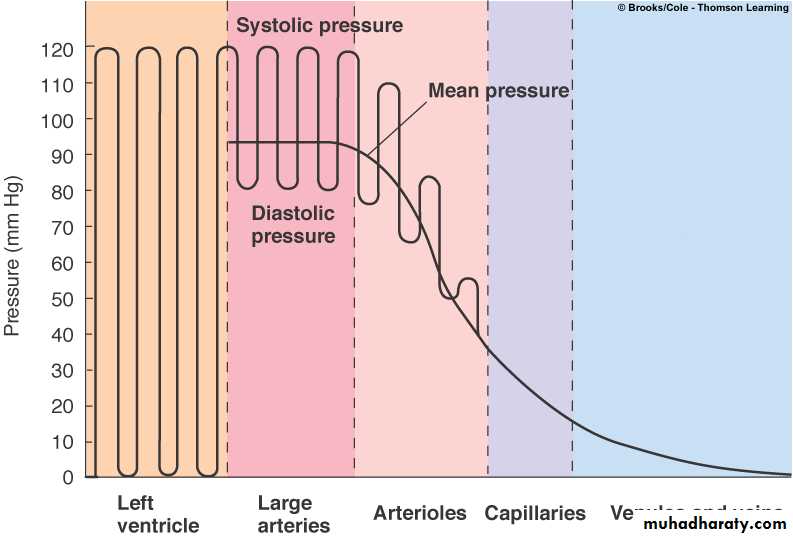
Left ventricular pressure fluctuates between 0-120 mm Hg
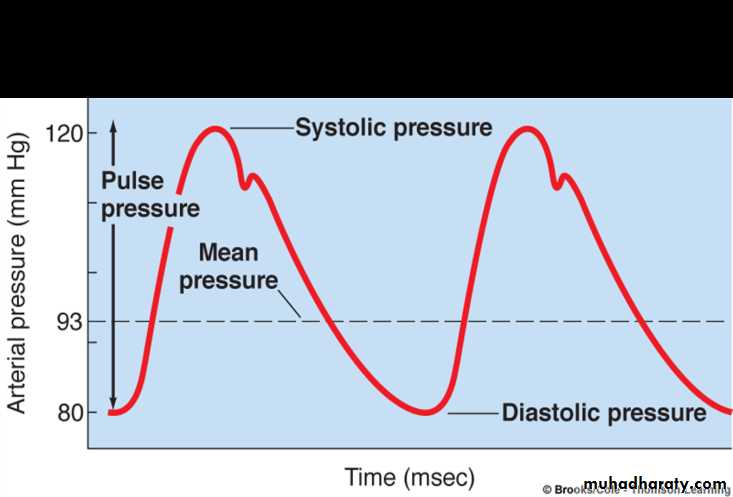
ABP fluctuates between 120-80 mm Hg during diastole.ABP does not fall to 0 mm Hg during diastole because of elastic recoil
ABP remains relatively constant throughout the arterial system
ABP drops suddenly in the arterioles due to the high resistance
In the arterioles the systolic-to-diastolic pulse is converted to non-pulsatile pressure
Pressure continues to decline throughout the capillaries and venous system.
Dynamics of blood flow:
Blood flow through blood vessels which are in the form of closed system due to:The pumping action of the heart.
Recoil of the walls of the arteries.
Compression of the veins by skeletal muscle during exercise.
Negative pressure in the thorax during inspiration.
The blood flow to each tissue is regulated by locals chemical and general neural mechanism that dilates or constricts the vessel’s of the tissues.
Anatomic considerations of blood vessels:
The wall of aorta and large arteries contain large mount of elastic tissue, they stretched during diastole.
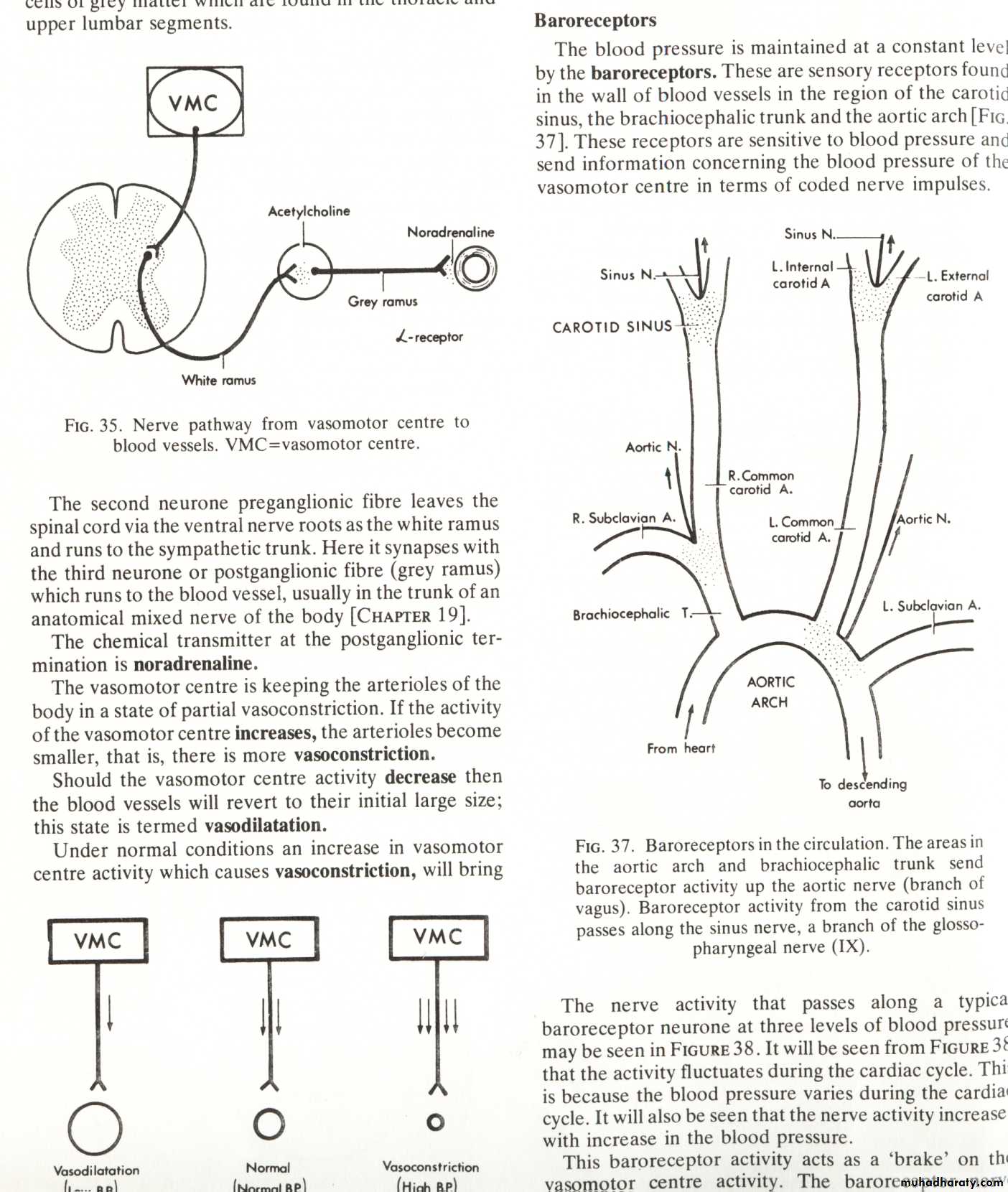
While the wall of arteriole contain smooth muscle which innervated by noradrenergic nerve fiber leading to constriction.
There are also some cholinergic nerve fibers which cause dilation.
The arterioles are the major site of resistance of blood flow, and small change in their diameter causes large changes in the peripheral resistance.
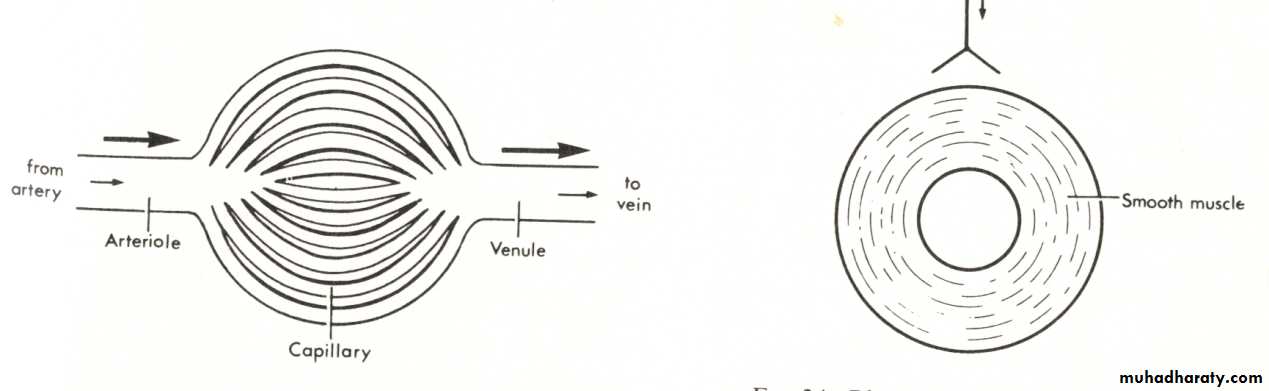
The arterioles attached to capillaries and at its beginning there is pre-capillary sphincter (smooth muscle), they respond to local or circulating vaso constrictor substances.
The endothelial cells of capillary may be tied as in muscle or fenestrated as intestinal villi, kidneys& liver.
Lymphatic vessels have similar structure to capillaries but they contain valves and the endothelial cells are close together.
Veins and venules have slightly thicker wall than capillaries and contain little smooth muscle noradrenergic nerve fiber lead to considerable vaso constriction in their wall.
Venous tone play important role in circulatory adjustment.
Arterial blood pressure :
It refers to the pressure in aorta and large arteries and the term Bp, if unqualified refers to the arterial BP
The organs of the body require blood flow and the arterial blood pressure (100 mmHg is needed to push the blood through the arterioles capillaries and veins in order to achieve this flow (systemic circulation).
In pulmonary circulation a low pulmonary artery BP 16 mm Hg is adequate to maintain 5 L. / min. blood flow (R. V. pressure in diastole is 0 mm Hg and in systole 25 mm Hg.)
There are two further factors to be taken into account concerning BP :
The brain is higher than heart in sitting or standing position and BP needed to pump blood up – hill from heart to brain.
2-BP is needed to enable the kidney to make urine.
Flow, Pressure and Resistance:
Blood flow from region of high pressure to region of low pressure except in certain situations.
The relation between mean flow, mean pressure and resistance in blood vessels is:-
Flow (F) = pressure (P) / Resistance(R)
Laminar Flow:
With in the blood vessel an infinitely thin layer of blood in contact with the wall of blood vessel dose not move, the next layer has a small velocity, the next has a higher velocity and so on.
Velocity being greatest in the center of the stream, laminar flow occurs at velocities up to critical velocity. At or above this velocity the flow is turbulent and creates sound, While laminar flow is silent.
(Probability of turbulence is also related to the diameter of the vessels and the viscosity of the blood. It increases in Anemia due to low viscosity of the blood leading to systolic murmur).
Regulation and control of cardio vascular system:-
Controlled: - means that some variables are kept steady .
Regulated: - means that variables are attempt appropriately according to requirements.
Controlling and regulation mechanism are located both centrally in C.N.S. and locally in tissues and organs them self.
Central or systemic mechanism affect heart and blood vessels to:-
Maintain arterial blood pressure with narrow range which provides a adequate perfusion of the brain and heart it self with out excessive cardiac work.Maintain appropriate filling pressure for the heart.
Systemic and local mechanism causing circulatory adjustment by:-
1- Change the caliber of the arterioles and other resistance vessels.
2-Alter blood storage in venous reservoirs.
3-Vary the rate and stroke out put of the heart.
Local mechanisms cause variation in vascular resistance to regulate local blood flow which subjected to systemic and local factors.
The local mechanism operate to maintain blood flow in active tissues (kidney, intestine, liver, heart, brain), while systemic mechanism synergize with local mechanism and adjust vascular response throughout the body.
I- Local Regulatory Mechanism:-
Auto regulation: - Is the capacity of tissue to regulate their own blood flow it may be due to:-
Intrinsic contractile response of smooth muscle to stretch (myogenic theory of auto regulation).
As the pressure rises in the blood vessels, they are distended and the vascular smooth muscle fibers that surround the vessels contract.
Due to auto regulation, When blood flow decrease vasodilators substances tend to accumulate in blood leading to vasodilation.
increased flow lead to washing of vaso dilators and then constriction occur.
Local Vaso Dilators Metabolite:
Metabolites that produce vaso dilation in most tissues are:-
Decrease O2 tension and PH lead to relaxation of arterioles and per capillary sphincters.
Increase in CO2 tension and osmolality , can affect brain and skin especially.
Rise in temperature.
Potassium ions accumulation (epically in skeletal muscles)
Lactic acid.
Histamine in injured tissues lead to increase permeability &swelling.
Local Vaso Constrictors:
1- Injured arteries and blood vessels constrict strongly due to local liberation of serotonin from platelets.
2- Decreased temperature cause vaso constriction.
II-Systemic Regulatory Mechanism:
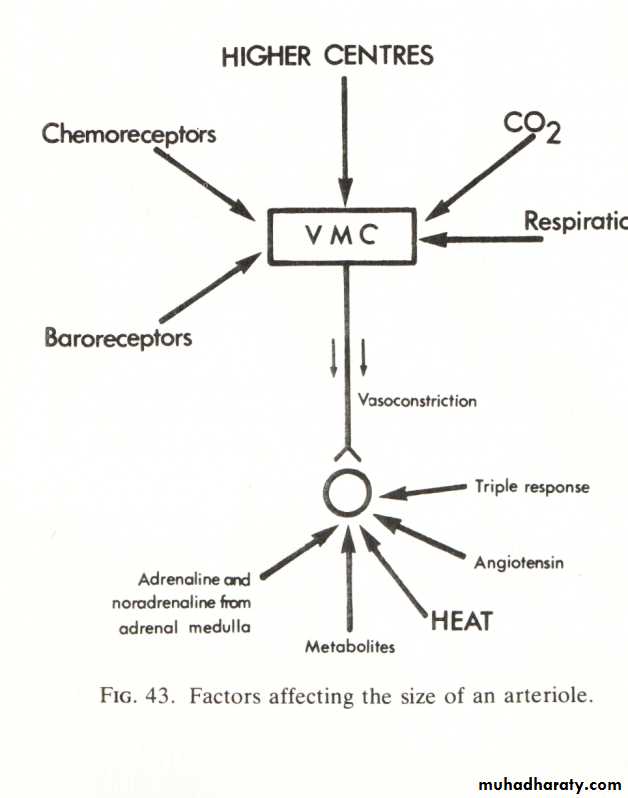
General Control of Blood Vessels:
Smooth muscle constriction in the blood vessels.
The effect of sympathetic nervous system on arterioles →vaso constriction.
Vaso motor center (VMC) in medulla keep the arterioles in a state of partial vaso constriction.
Increased activity of VMC lead to vaso constriction and then increased blood pressure.
While decreased activity of VMC lead to vaso dilatation and then decreased BP.
Norephinephrine and angiotensin II is generalized vaso constrictor.
Also ephenephrine but except on skeletal muscles it cause vaso dilation.
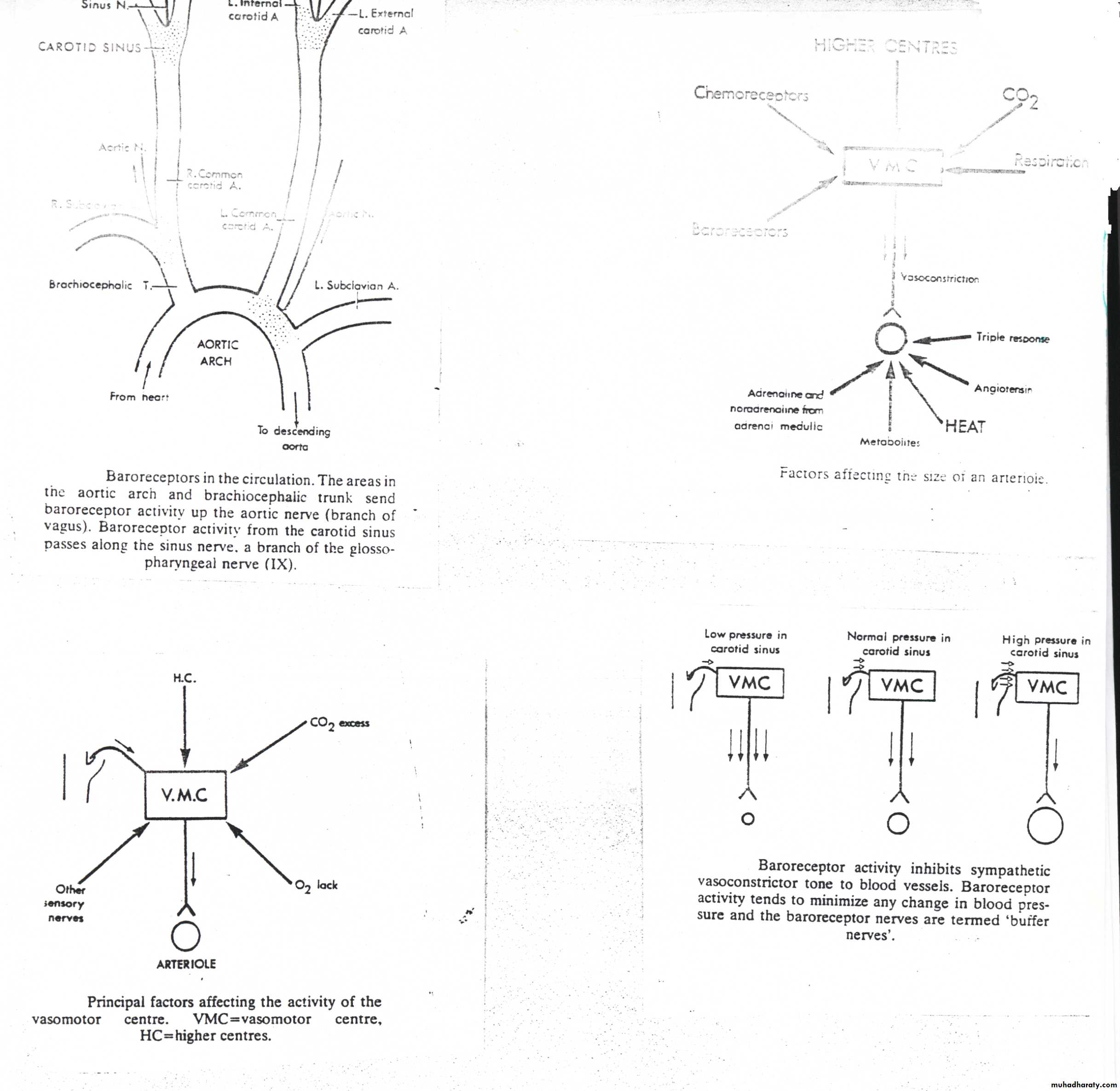
Baroreceptors :
There are sensory receptors found in the wall of the blood vessels in the region of carotid sinus, the brachio cephalic trunk and the aortic arch.
It is sensitive to blood pressure changes and it maintains the blood pressure constant.
The barroreceptor activity acts as brake on the VMC activity (Negative feedback mechanism).
If there is increase in BP this will increase baroreceptor activity and this will lead to decrease VMC activity which decrease sympathetic tone to arteriole leading to vasodilation and then decreased BP, due to decreased peripheral resistance and also by action of baroreceptor on cardiac center in medulla to slow heart and respiratory center by decreasing breathing.
Other Factors affecting VMC :
Higher centers which are the higher parts of the CNS, it includes a region of cerebral cortex.Emotional excitement and stress are accompanied by stimulation of VMC by higher centers leading to Increased vaso constriction and then increased BP (as in the case of recording BP in a clinic).
Over breathing of O2 cause washing of CO2 which is needed to the function of VMC so it cause decreased BP
Decreased O2 will stimulate VMC, chemo receptors affected by hypoxia.
Hypercapnia also stimulates VMC following hemorrhage.
Many other nerves in the body affects VMC, moderate pain will stimulate VMC, while sever pain will inhibit VMC