Human Physiology Introduction and Homeostasis
Physiology - science that describes how the bodyfunction and survive in continually changing environments.Levels of Organization:
CHEMICAL LEVEL -includes all chemical substances (atoms, ions& molecules) necessary for life.
CELLULAR LEVEL - cells are the basic structural and functional units of the human body,there are many different types of cells (e.g., muscle, nerve, blood, etc..).
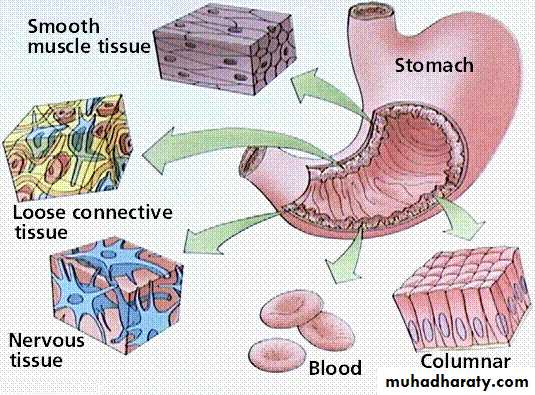
TISSUE LEVEL - a tissue is a group of cells that perform a specific function and the basic types of tissues in the human body include epithelial, muscle, nervousand connective tissues.{Glands(Endocrine &Exocrine)-derived from epithelial tissue, specialized for secretion}.
ORGAN LEVEL - an organ consists of 2 or more tissues that perform a particular function (e.g.; heart, liver, stomach)
SYSTEM LEVEL - an association of organs that have a common function; there are 11 major systems in the human body, including;digestive, nervous, endocrine, circulatory, respiratory, urinary, reproductive, muscular, lymphatic, skeletal, and integumentary.
Body Composition:
In the average young adult male, 18% of the body weight is protein and related substances, 7% mineral and 15% fat. The remaining 60% is water.
THE INTERNAL ENVIRONMENT:
The body fluids are divided into two major functional compartments:1. The fluid inside cells, is the intracellular fluid (ICF)compartment.
2. The fluid outside cells is the extracellular fluid (ECF) compartment, which is
subdivided into the interstitial fluid and the blood plasma.
The concept of an internal environment in the body correlates with the interstitial fluid
bathing cells. There is free exchange of water and small solutes in the ECF between interstitial fluid and plasma across the blood capillaries. In contrast,the exchange of most substances between interstitial fluid and intracellular fluid is highly regulated and occurs across plasma cell membranes.
The volume of total body water is approximately 60% of body weight in men and 50% in women.
About 60% of total bodywater is ICF and 40% is ECF. Approximately 80% of ECF isinterstitial fluid and the remaining 20% is blood plasma, whichis contained inside the vascular system.
The basic compositions of body fluids; ECF is high in NaCl and lowin K+, whereas ICF is high in K+and low in NaCl. Interstitialfluid is similar in composition to plasma, except that interstitialfluid has almost no protein.
Osmolarity is the same in allcompartments.
I. Overview of Cell
A. Cells that make up human body are microscopic
B. Cells that make up a hummingbird, human, and an elephant are all
about the same size. Larger species have more cells.
C. Cells are complex, highly organized, compartmentalized structure
II. Cell Structure
A. 3 major subdivisions:1. Plasma membrane; thin membrane composed mostly of lipids and proteins that separates cell’s contents from its surroundings
Physical barrier
Its proteins selectively control movement of molecules between intracellular fluid ICF and extracellular fluid ECF .
2. Nucleus
Typically largest single cell component
Surrounded by nuclear envelope perforated by nuclear pores
Control center of cell
Contains DNA; genetic material that:
1) directs protein synthesis
2) serves as genetic draft during cell replication
3. Cytoplasm
Portion of interior of cell not occupied by nucleus, Contains:1) Cytoskeleton; interconnected system of protein fibers and tubes (microtubules, microfilaments, intermediate filaments)extends throughout the cytosol, gives cell shape, framework,regulates various movements.
2)Cytosol; intracellular fluid (ICF); semiliquid, gel-like mass
3) Organelles; structures suspended in ICF; each has specific role and work in integrated manner. Most cells have 6organelles types:
Endoplasmic reticulum (ER); series of membranes that contain protein-and lipid-manufacturing factories(ribosomes;produce proteins)
Golgi complex;raw proteins are processed, sorted, packaged, and directed to proper destination
Lysosomes;contain powerful enzymes that break down organic molecules, vary in size and shape depending on what they are digesting.
-Average cell has about 300 lysosomes
-Digest extracellular material brought into cell
-Remove worn out organelles (Autophagy,Apoptosis)
Peroxisomes;house oxidative enzymes that degrade toxic wastes produced with cell or toxins that have entered cell (such as alcohol)
Mitochondria;powerhouse of cell;extract energy from food nutrients and transform it into usable form for cellular activities: Adenosine triphosphate (ATP).
-Number varies widely depending on cell’s energy requirements
Ribosomes;make proteins by translating ribonucleic acid (RNA) into chains of amino acids in sequence controlled bydeoxyribonucleic acid(DNA)-exist free in cytosol or attached to rough ER
Vaults;first identified in 1990’s;may serve as cellular transport vehicles/may play undesirable role in multidrug resistance displayed by some cancer cells
Cell Membrane or Plasma Membrane
I. Functions &Structure
A. General Functions:
Physical Isolation
supporting and hold the cytoplasm
Transport:Helps determine cell’s composition by selectively permitting certain substances to pass between cell and its environment(selective barrier).
Structural-participates; in joining of cells to form tissues& organs.
Recognition;Plays key role in enabling cell to respond to changes in cell’s environment(The immune response; is the ability to distinguish between self and nonself,everybody cell carries distinctive molecules that distinguish it as "self"). Normally the body's defenses do not attack tissues that carry a self marker.Rather, immune cells coexist peaceably with other body cells in a state known as self-tolerance.
B. Basic Structure
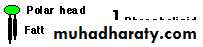
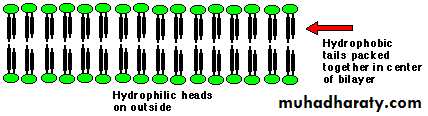
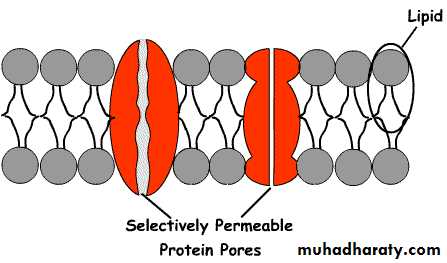
1. Fluid phospholipid bilayer embedded with proteins
Phospholipids have a polar (electrically-charged) head and two nonpolar (electrically neutral) fatty acid tails
Polar heads are hydrophilic(water-loving);can interact with water molecules
Nonpolar tails are hydrophobic (water-fearing);will not mix with water
Hydrophilic heads line up on both sides in contact with water (outer surface is exposed to ECF and inner surface is in contact with ICF)
Tails hidden in center away from water
Cholesterol inserted in between phospholipids molecules it contributes to fluidity, stability
cholestrol
2. Membrane carbohydrates;(glycoproteins, glycolipids)small amount located only at outer surface.
3. Membrane Proteins;attached to or inserted within lipid bilayer. Anatomically, 2 groups:
a. Peripheral;attach loosely to other proteins that span the membrane or to lipid bilayer
b. Integral;tightly bound into the phospholipid bilayer.
• Transmembrane Proteins;integral proteins that extend all the way through the membrane.
Many of the proteins associated with the plasma membrane are tightly bound to it.
Proteins that penetrate the membrane are hydrophobic.
Membrane proteins have many functions:
receptors for hormones; Recognize and bind with specific molecules in environment of cell; therefore, chemical messengers in blood, such as hormones, are able to influence only the specific cells(those have receptors for given messenger) e.g.Thyroid stimulating hormone(TSH) can only attach to thyroid gland.
pumps for transporting materials across the membrane
ion channels;
Create water-filled passageway to enable water-soluble substances that are small enough to enter or pass through membrane without coming into direct contact with hydrophobic lipid interior.
Restricted to ions and water
--May be specific for 1 ion
--May allow ions of similar size & charge to pass
--May be open or gated
Adhesion molecules for holding cells to extracellular matrix
Cell recognition antigens;Recognitionof “self glycoproteins” on surface of membrane structural proteins;maintain shape of cell
Carriers or transporters(membrane transport protein):
Transfer specific substances across membrane that are unable to cross on their own.
Bind with specific molecule and carry across membrane by changing shape.
Never form a continuous passageway between ICF and ECF,only open to one side.
4. Some membranes have microvilli, cilia, flagella
II. Membrane Transport:
A. Membrane Permeability:Permeability refers to ability of substances to enter/leave cell.
1. Permeable
2. Impermeable
3. Selectively permeable
2 properties influence whether substance can pass through unassisted:
Solubility of particle in lipid (highly lipid-soluble particles dissolve & pass through)
Size of particle
B. Two General Types of Movement Across Membrane
1. Passive;does not require input of energy (uses only energy of molecular movement)
2. Active;requires energy (ATP) to transport substance across.
Active transport of Na+ and K+ is one of the major energy-using processes in the body. On the average, it accounts for about 24% of the energy utilized by cells, and in neurons it accounts for 70%. Thus, it accounts for a large part of the basal metabolism.
C.Passive Transport (unassisted)
Terms you should know:concentration gradient;difference in concentration of substance between two places (sometimes called chemical gradient)
solution
solvent
solutes
net diffusion
Types of passive transport:
1. Simple Diffusion;movement from a region of high concentration
to region of low concentration (i.e. down a concentration gradient)
Rate of diffusion affected by (Fick’s Law of Diffusion);
a. Surface area of membrane
b. Magnitude of concentration gradient
c. Molecule size & weight
d. Temperature
e. Thickness of cell membrane
f. Lipid solubility of substance
Ions can also permeate membrane along electrical gradient:Electrical forces;(like charges repel, opposite charges attract).
2. Osmosis
a. Movement of water down its concentration gradient across a selectively permeable membrane(many cell types have aquaporins that allow passage of water)
Water moves by osmosis to the area of higher solute concentration, i.e. to dilute the area.
As solute concentration increases, the water concentration decreases correspondingly.
d.Osmolarity; measure of a solutions total concentration given in terms of number of ions (osmole/liter),normal osmolarity of body fluids is 300mOsm/L (millosmole/liter)
(Osmolarity tendency of a solution to pull water in)
osmosis often produces significant volume changes, causing swelling or shrinking;
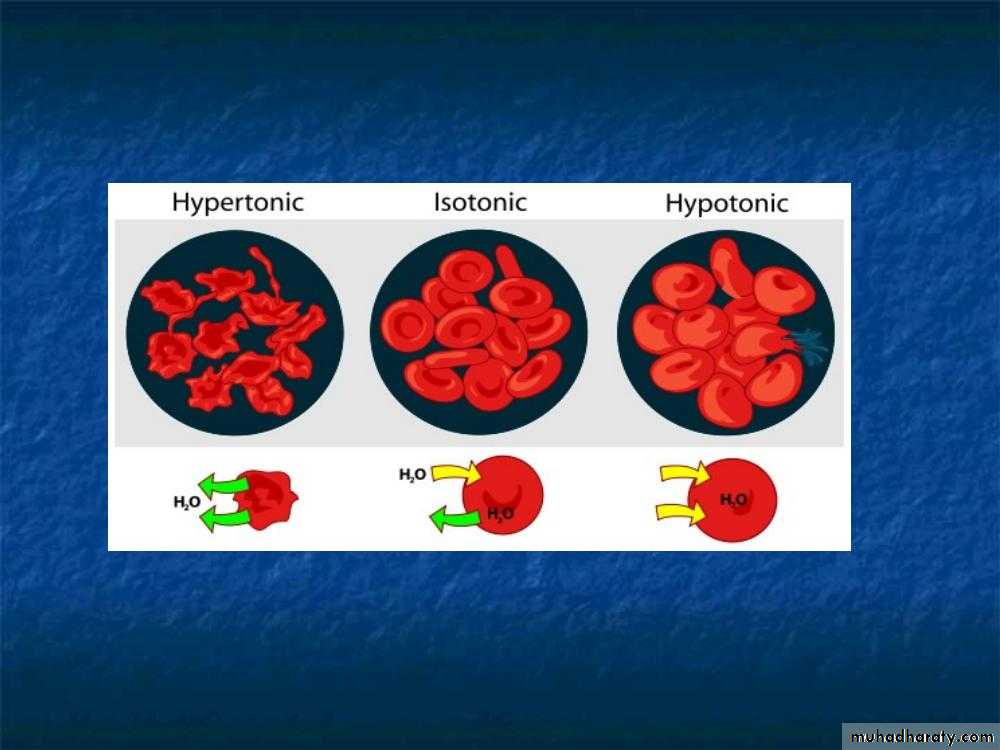
If the external solution balances the osmotic pressure of the cytoplasm it is said to be isotonic.
If the external solution is more dilute than the cytoplasm it is hypotonic
if the external solution is more concentrated it is hypertonic.
Tonicity; the ability of solution to change the size and shape of the cell by altering the amount of water they contains, it describes what would happen to cell volume if cell where placed in the solution.
Clinically important;IV fluids typically isotonic
Isotonic saline (0.9% NaCL solution)
Usually ECF is kept isotonic so not net diffusion of water occurs. Cells, esp. brain cells do not function properly if swollen or shrunken.
Sometimes use hypotonic or hypertonic fluids therapeutically to correct osmotic imbalances
D.Carrier-Mediated Transport,Co-transport,or Assisted Membrane Transport;
Large, poorly lipid- soluble molecules, such as proteins, glucose, etc. cannot cross plasma membrane on their own no matter what forces are acting on them so need the aid of a carrier protein.
Carrier protein spans thickness of plasma membrane
Carrier proteins bind to specific substances and transport them by changing shape.
Carriermediated Transport, demonstrates 3 properties:
Specificity
Competition
Saturation
2 forms of carrier-mediated transport depending on whether energy must be supplied to complete the process:
carrier
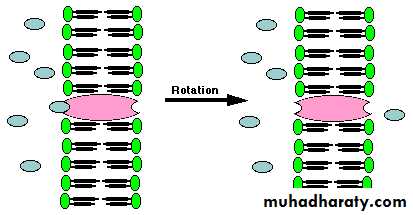
Facilitated Diffusion;same properties as simple diffusion but uses a carrier (Special Proteins) to assist the transfer.
An extracellular molecule binds to the transport protein, the transport protein then rotates and releases the molecule inside the cell
Examples:
Glucose transporters that cotransport Na+ and glucose
Water channels aquaporins transport water in the kidney
Properties of facilitated diffusion:
Facilitated diffusioncannot cause net transport of molecules from a low to a high concentration,as this would require input of energy
ATP energy not required
Transport rate reaches a maximum when all of the protein transporters are being used (saturation)
It's very specific it allows cell to select substances taken up
Sensitive to inhibitors that react with protein side chains
2. Active Transport;requires energy input from ATP and moves a substance against its concentration gradient.
Pumps; are proteins that use energy to carry substances across the cell membrane
pump
Can transport substances from a low concentration to a high concentration ("uphill" transport)
ATP energy required
Examples: The Na+/K+-ATPase (known as the “sodium pump”), Ca2+-ATPases (the Ca pump), H+/ K+-ATPases, H+-ATPases, multidrug resistance (MDR) transporters
Transport rate reaches a maximum when all of the protein transporters are being used (saturation)
Very specific, allows cell to select substances taken up
Sensitive to inhibitors that react with protein side chains
Extremely important in physiology: about a third of your basal metabolism is used in active transport of various substances
Secondary Active Transport:
Many Molecules Enter Cells by Secondary Active TransportSecondary Active Transport; Combines active transport and facilitated diffusionExamples: Glucose transport across the wall of the gut.
Na+ gradient is produced by the Na pump (active transport)
The Na+ concentration gradient is used to produce secondary transport of sugars and amino acids (facilitated diffusion)
Some sugar and amino acid transporters must bind Na as well as the sugar or amino acid (coupled transport)
Both Na+ and the organic molecule must be present at the same time and on the same side of the membrane
Since there is more Na outside the cell, sugars and amino acids get transported mainly from the outside to the inside
The sugar and amino acid transporters do not use ATP directly, but ATP is required to set up the Na gradient.
There are many examples of secondary active transporters:
Cotransporters (symporters) couple the movement of two or more solutes in the same direction. Examples of Na+-driven cotransporters include Na+/glucose uptake in the intestineand Na+/Cl- uptake in the kidney.Exchangers (antiporters) couple the movement of two solutes in the opposite direction. Na+-driven exchangers include Na+/Ca+2and Na+/H+exchange, which are important for maintaining low intracellular [Ca+2]and [H+], respectively.
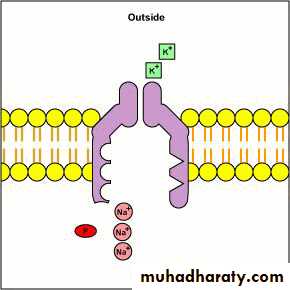
Mechanism of Primary Active Transport {NA+K+ Pump};
1) Most important form of active transport in cells2) Maintains concentration gradients of NA+ and K+ across cell membrane
3) Moves 3 sodium ions from inside cell to ECF
4) Moves 2 potassium ions from ECF into cell
5) Net movement =high Na+ concentration in ECF and high K+ concentration in ICF.
6) Transmembrane potential;inside of cell has slight negative charge as compared to outside of cell
7)Difference in charges=a potential;reflects unequal distribution of positive and negative charged ions.
Comparison of Simple Diffusion, Facilitated Transport & Active Transport:
Property
SimpleDiffusion
FacilitatedTransport
ActiveTransport
Requires special membrane proteins
No
Yes
Yes
Highly selective
No
Yes
Yes
Transport saturates
No
Yes
Yes
Can be inhibited
No
Yes
Yes
Hormonal regulation
No
Yes
Yes
Uphill transport
No
No
Yes
Requires ATP energy
No
No
Yes
E. Bulk Transport or Vesicular Transport
Moves macromolecules that are too large to move through channels or carriers, such as protein hormones, bacteria ingested by white blood cells (WBCs)
Involves moving materials in vesicles, small membranous sacs that format, or fuse with cell membrane.
Requires energy in the form of ATP
Energy needed for vesicle formation and vesicle movement within cell
2 major categories:Endo& exocytosis,moving material into (endo) or out of (exo) cell in bulk form.
Rates of endocytosis and exocytosis must be kept in balance to maintain constant membrane surface area and cell volume.
Endocytosis; Movement of extracellular material into cytoplasm.Types of 1)Endocytosis:
Pinocytosis
Phagocytosis
Receptor-mediated endocytosis
Exocytosis
Functional reversal of endocytosisVesicle created inside cells fuses with cell membrane, then opens up and releases its contents to the exterior
Provide mechanism for secreting large polar molecules such as hormones and enzymes
Enables cell to add specific components to membrane such as selected carriers, channels, or receptors depending on needs of cell
INTERCELLULAR COMMUNICATION:
Cells communicate with one another via chemical messengers. Within a given tissue, some messengers move from cell to cell via gap junctions without entering the ECF.In addition, cells are affected by chemical messengers secreted into the ECF. These chemical messengers bind to protein receptors on the surface of the cell or, in some instances, in the cytoplasm or the nucleus, triggering sequences of intracellular changes that produce their physiologic effects.
Three general types of intercellular communication are mediated by messengers in the ECF:
(1) Neural communication;in which neurotransmitters are released at synaptic junctions from nerve cells and act across a narrowsynaptic cleft on a postsynaptic cell
(2) Endocrine communication;in which hormones and growth factors reach cells via the circulating blood
(3) Paracrine communication;in which the products of cells diffuse in the ECFto affect neighboring cells that may be some distanceaway.
Autocrine communication; in some situations, cells secrete chemicalmessengers that bind to receptors onthe same cell, ( the cell that secreted the messenger).
The chemical messengersinclude (amino acids, steroids, polypeptides,lipids, purine nucleotides,and pyrimidine nucleotides).
Invarious parts of the body, the same chemical messengercan function as a neurotransmitter, a paracrine mediator,a hormone secreted by neurons into the blood(neural hormone), and a hormone secreted by glandcells into the blood.
Homeostasis
Homeostasis;body’s ability to maintain stable internal environment (internal constancy), is essential for cell’s survival and each cell contributes to homeostasis.
Cells in multicellular environment cannot live and function without contributions from other body cells because most of its cells are not in direct contact with external environment
System functions finally depend on specialized activities of individual cells.
Homeostatic Control Systems:
A. Networks of body components work together to maintain acontrolled variable in the internal environment at a relatively constant set point {desired level of a variable or system where it functions best}.b. Classifications of Control Systems:
1.Intrinsic (local)–inherent responses of an organ to compensate for change in condition.
2.Extrinsic (systemic)–regulatory response initiated outside organ to alter organ’s activity, i.e., by the nervous system and endocrine system.Examples: Thyroid gland secretion, glucose levels,….
Homeostasis regulated by:
1. Nervous System;shorter duration, more specific.
2. Endocrine System;slower to start, less specific, longer lasting. Secretes hormones (chemical messengers) into blood, only “target organs” respond to that particular hormone.
Homeostasis involves 3 fundamental components:
a receptora control center/integration center
an effector
Feedback Loops;feedback=responses made after change has been detected
Negative Feedback Loop
Widely used to maintain homeostasis
Triggers a response that seeks to restore the factor to normal by moving the factor in the opposite direction of its initial change
Starts with a "set point"value at which the process functions optimally (normal)
Changes away from normal state (set point) cause reactions in opposite direction.
Homeostatic response is turned off when response of system opposes or removes original stimulus.
Positive Feedback
*Self-amplifying cycle-output is continually enhanced of amplified so that the controlled variable continues to be moved in the direction of the initial change.
Does not occur in body as often as negative
play role in certain instances, e.g., in childbirth:
Hormone oxytocin causes powerful uterine contractions
Contractions push baby against the cervix of mother
Stretching of cervix triggers release of more oxytocin, causing even stronger contractions, triggering release of more oxytocin and so on.
Does not stop until cervix stops being stimulated (baby is born)
Always includes a mechanism for termination of cycle
AGING
Aging affects cells and the systems made up ofthem, as well as tissue components such as collagen,and numerous theories have been advanced to explainthe phenomenon.One theory of aging holds that tissues age as a result of random mutations in the DNA of somatic cells, with consequent beginning of cumulative abnormalities.
Others hold that cumulative abnormalities are produced by increased cross-linkage of collagen and other proteins, possibly as the end result of the non enzymatic combination of glucose with amino groups on these molecules.
A third theory envisions aging as the cumulative result of damage to tissues by free radicals formed in them. It is interesting in this regard that species with longer life spans produce more superoxide dismutase, an enzyme that inactivates oxygen-free radicals.
It is now established that in experimental animals, a chronically decreased caloric intake prolongs life, and this could be true in humans as well. One possible explanation for this effect of caloric restriction is decreased metabolism, with decreased formation of protein cross-links and decreased production of free radicals.
However, the exact cause of the lengthened life span produced by caloric restriction remains to be determined.
In aging humans, declines occur in the circulating levels of some sex hormones, the adrenal androgen, dehydroepiandrosterone and its sulfate, and growth hormone.
Replacement therapy with estrogens and progesterone in women decreases the incidence of osteoporosis.
Replacement therapy with testosterone, dehydroepiandrosterone , and growth hormone each has some useful effects, but each also has undesirable side effects, and there is little if any evidence that they prolong life.