1
HDTD/ Cartilage
Lecturer Dr. Zahraa Qasim Ali
Objectives:
Dear students:
By the end of this ‘’Cartilage’’ lecture, I hope each one of you will be able to:
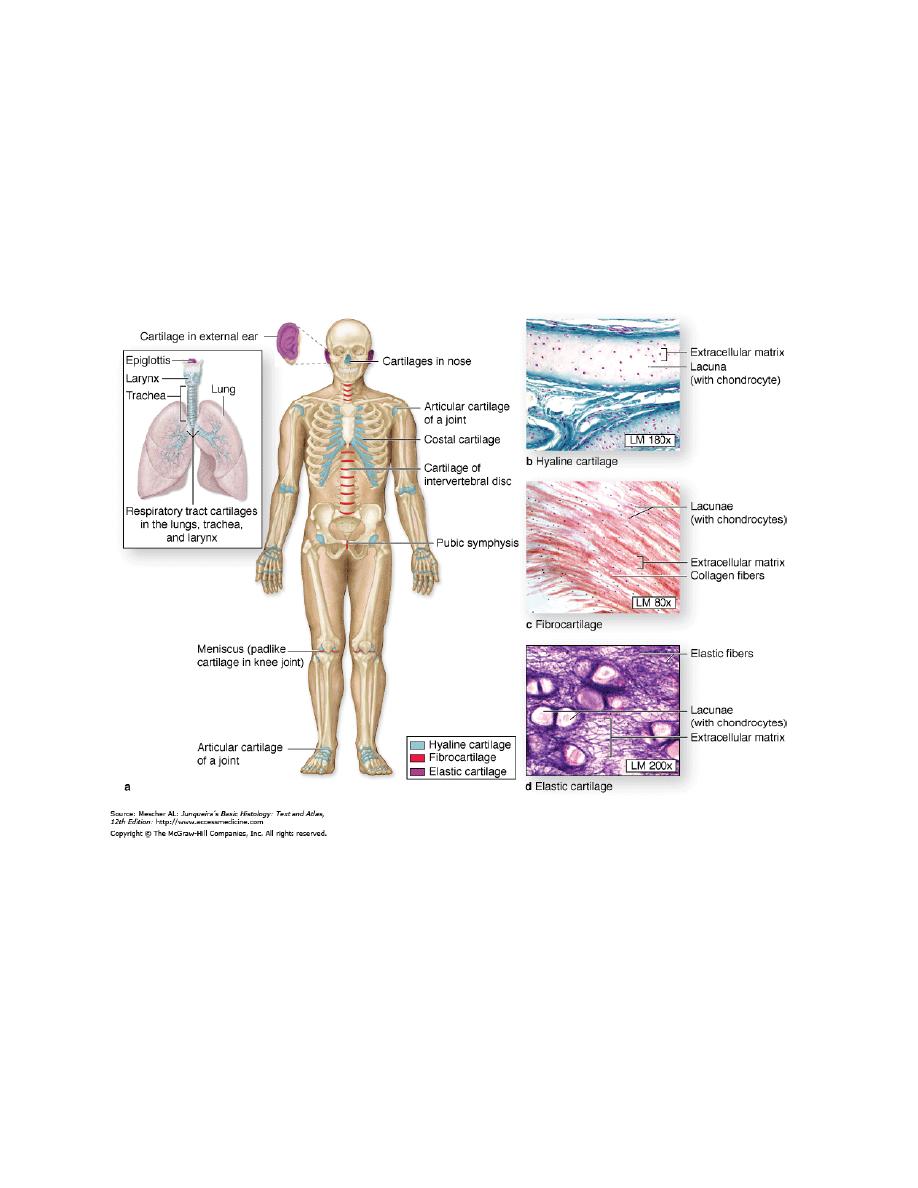
1. Histologically Define cartilage and write some notes on it.
2. List the three types of cartilage.
3. Determine the compositional differences in each type.
4. Describe the function(s) and location(s) of each type.
Introduction:
Cartilage is a specialized form of connective tissue characterized by an
extracellular matrix (ECM) and cells called chondrocytes (Gr. chondros, cartilage
+ kytos, cell).
Chondrocytes synthesize and secrete the ECM and the cells themselves are located
in matrix cavities called lacunae. Collagen, hyaluronic acid, proteoglycans, and
small amounts of several glycoproteins are the principal macromolecules present in
all types of cartilage matrix. Variations in the composition of these matrix
components produce three types of cartilage adapted to local biomechanical needs.
2
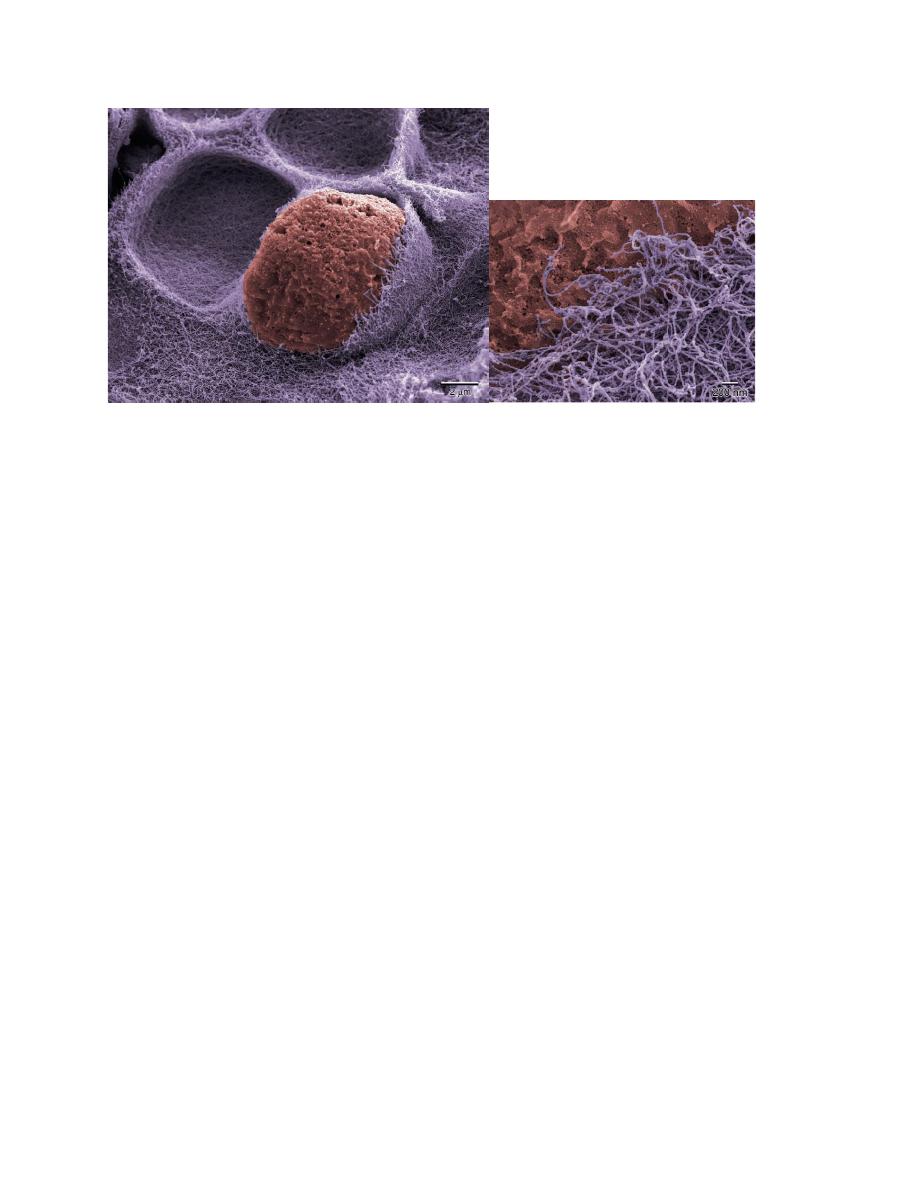
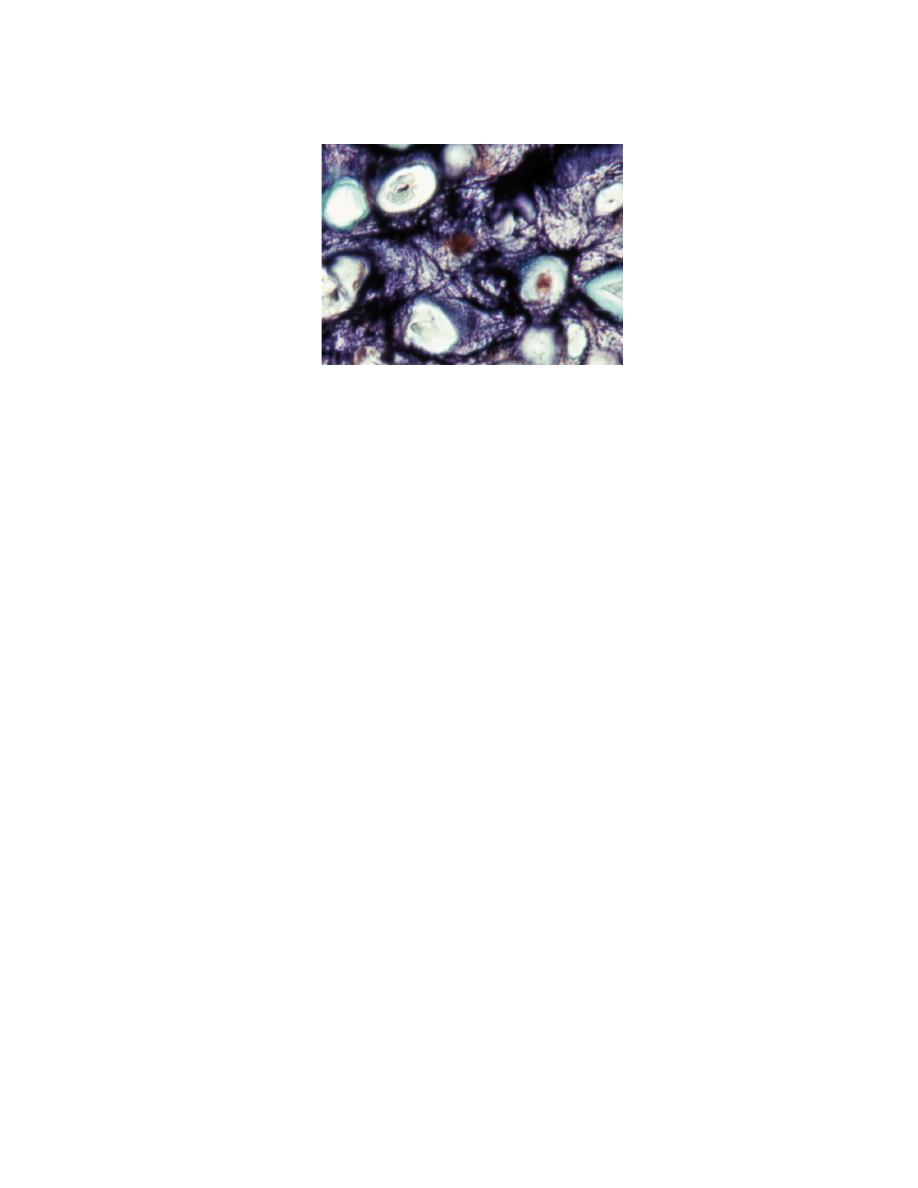
Colorized scanning electron micrograph (SEM) of an isogenous nest in hyaline
cartilage. A chondrocyte sits in its lacuna surrounded by fine fibrillar matrix.
Another lacuna is empty because its chondrocyte had popped out during specimen
preparation. 5000×. A magnified view of collagen fibrils in the matrix is below.
25,000×.
Reference:
NETTER’S ESSENTIAL HISTOLOGY, SECOND EDITION (2013) ISBN: 978-1-4557-0631-0
Cartilage histologically:
Cartilage
is an avascular tissue that consists of
chondrocytes
and an
extensive
extracellular matrix
. More than 95% of
cartilage volume
consists of extracellular matrix, which is a
functional element of this tissue.
The chondrocytes are sparse
but essential participants in producing and
maintaining the
matrix.
Cartilage is avascular: Despite being a connective tissue, cartilage is
avascular and, hence, relies on diffusion of nutrients from the vessels in the
perichondrium or other surrounding tissues. Avascularity of the cartilage
also contributes to slow and limited ability to heal and repair itself when
injury occurs.
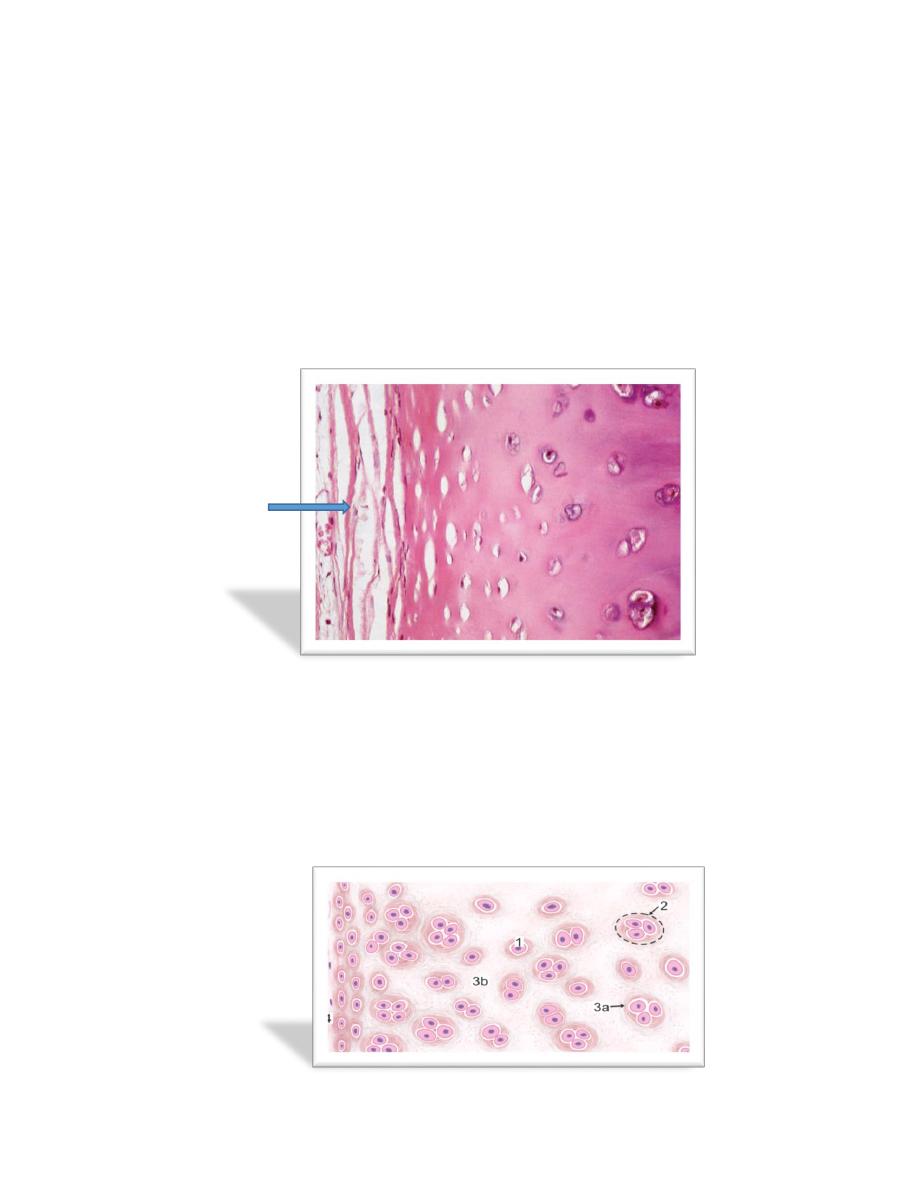
3
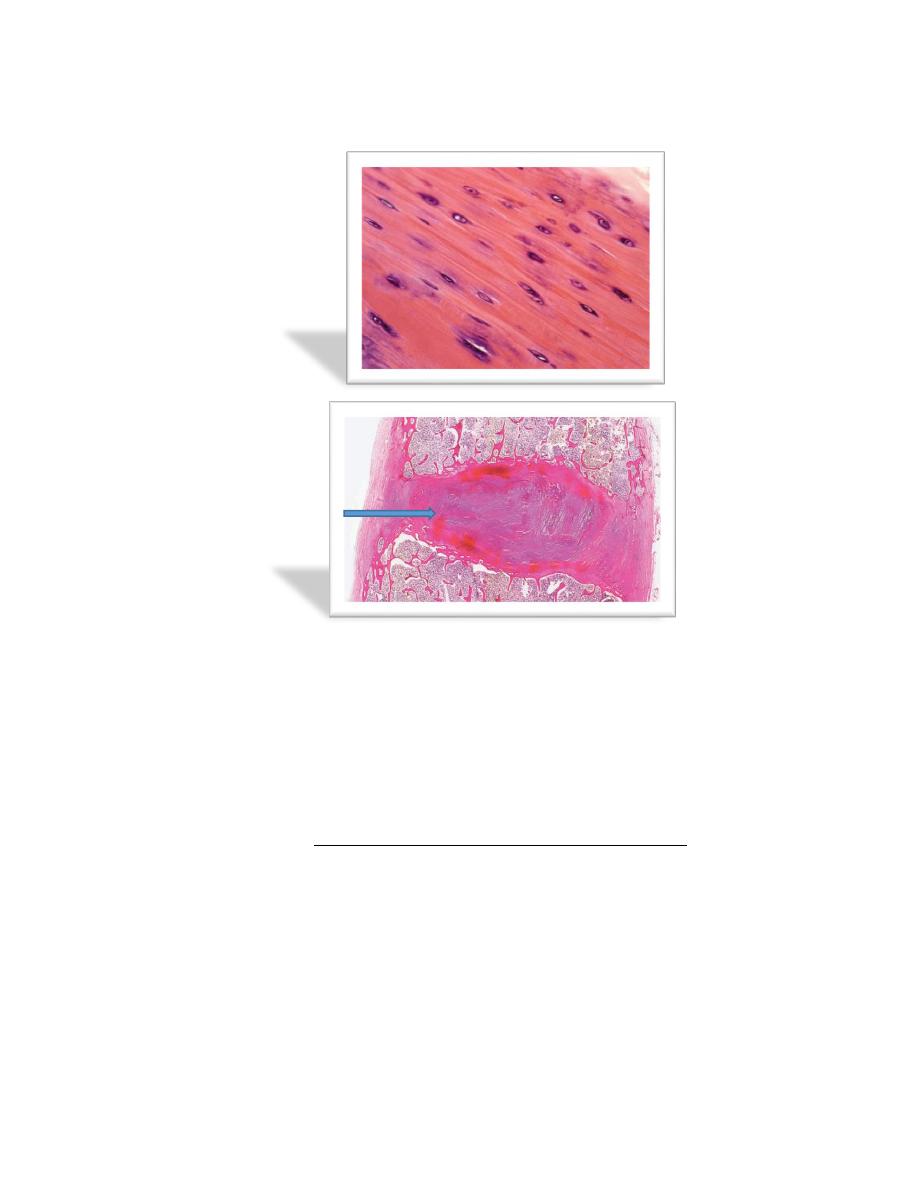
Perichondrium: Except in the articular cartilage of joints, all hyaline
cartilage is covered by a layer of dense connective tissue, the
perichondrium
(arrow in the picture below)
, which is essential for the growth
and maintenance of cartilage. It consists largely of collagen type I fibers and
contains numerous fibroblasts. Although cells in the inner layer of the
perichondrium resemble fibroblasts, they are precursors for chondroblasts,
which divide and differentiate into chondrocytes.
Chondrocytes: At the periphery of hyaline cartilage, young chondrocytes
have an elliptic shape, with the long axis parallel to the surface. Farther in,
they are round and may appear in groups of up to eight cells originating
from mitotic divisions of a single chondrocyte. These groups are called
isogenous aggregates.
4
Key
1. Chondrocyte
2. Cell nest
3. Basophilic matrix
a. Territorial matrix
b. Interterritorial matrix
4. Perichondrium
Chondrocytes synthesize collagens and the other matrix molecules. As matrix is
produced, cells in the aggregates are moved apart and occupy separate lacunae.
It is good to know that [
Nutrients from the blood diffuse through the
perichondrium to reach the more deeply placed cartilage cells. Transport of water
and solutes is promoted by the pumping action of intermittent cartilage
compression and decompression. Because of the limits of diffusion, the maximum
width of the cartilage is limited and cartilage usually is found as small, thin plates
of tissue.
Chondrocyte function is hormone dependent. Synthesis of sulfated GAGs is
accelerated by growth hormone, thyroxin, and testosterone and is slowed by

5
cortisone, hydrocortisone, and estradiol. Cartilage growth depends mainly on the
pituitary-derived growth hormone somatotropin.
]
Growth of cartilage: Mainly occurs during embryonic, fetal development
and childhood, slowly decreasing in adolescence. In adults, cartilage
undergoes little to no growth.
Appositional growth: Chondroblasts in the perichondrium produce
cartilaginous matrix and thicken the cartilage from the periphery. Once the
chondroblasts become encased in the matrix they produced, they become
chondrocytes.
Interstitial growth: Chondrocytes in the middle of the cartilage divide, and
then each daughter cell starts secreting its own cartilaginous matrix around
itself, eventually becoming separated from each other by the newly
produced cartilage matrix.
Cartilage Functions:
The firm consistency of the ECM allows the tissue to (1) bear mechanical stresses
without permanent distortion. In the respiratory system, cartilage forms a framework
(2) supporting soft tissues. Because it is smooth-surfaced and resilient, cartilage
provides a (3) shock-absorbing and (4) sliding area for joints and facilitates bone
movements. Cartilage is also (5) essential for the development and growth of long
bones, both before and after birth.
6
Types of Cartilage:
There are three types of cartilage—(1) hyaline cartilage, (2) elastic cartilage, and
(3) fibrocartilage—differ mostly in histologic appearance and properties of
extracellular matrix.
Reference: Junqueira’s Basic Histology, 14
th
edition. 2016

7
1. Hyaline Cartilage
Hyaline cartilage matrix is highly hydrated to provide resilience and
diffusion of small metabolites.
In articular cartilage (cartilage of the joints), both transient and regional changes
occur in water content during joint movement and when the joint is subjected to
pressure. The high degree of hydration and the movement of water in the matrix
allow the cartilage matrix to respond to varying pressure loads and contribute to
cartilage’s weight-bearing capacity.
It is good to know that
:
[
Throughout life, cartilage undergoes continuous internal
remodeling as the cells replace matrix molecules lost through degradation. Normal
matrix turnover depends on the ability of the chondrocytes to detect changes in
matrix composition. The chondrocytes then respond by synthesizing appropriate
types of new molecules. In addition, the matrix acts as a signal transducer for the
embedded chondrocytes. Thus, pressure loads applied to the cartilage, as in synovial
joints; create mechanical, electrical, and chemical signals that help direct the
synthetic activity of the chondrocytes. As the body ages, however, the composition
of the matrix changes and the chondrocytes lose their ability to respond to these
stimuli
]
.
Chondrocytes of hyaline cartilage are highly specialized cells that synthesize and
maintain all components of the extracellular matrix. chondrocytes are distributed

8
either singularly or in clusters called isogenous groups. When the chondrocytes are
present in isogenous groups, they represent cells that have recently divided. As the
newly divided chondrocytes produce the matrix material that surrounds them, they
are dispersed. They also secrete metalloproteinases, enzymes that degrade cartilage
matrix, allowing the cells to expand and reposition themselves within the growing
isogenous group. The matrix has a unique, highly ordered molecular organization.
Depending on age and location of the cartilage, 60%-70% of its wet weight is water.
Water and inorganic salts give cartilage its resilience and lubricating capabilities.
Remaining constituents are structural macromolecules: collagens, PGs, and non-
collagenous proteins. Of the dry weight of cartilage matrix, 40%-70% is collagen.
Type II collagen accounts for 90%-95% of the collagen in hyaline cartilage and
forms a fibrillary meshwork that mainly provides tensile strength and shape.
9
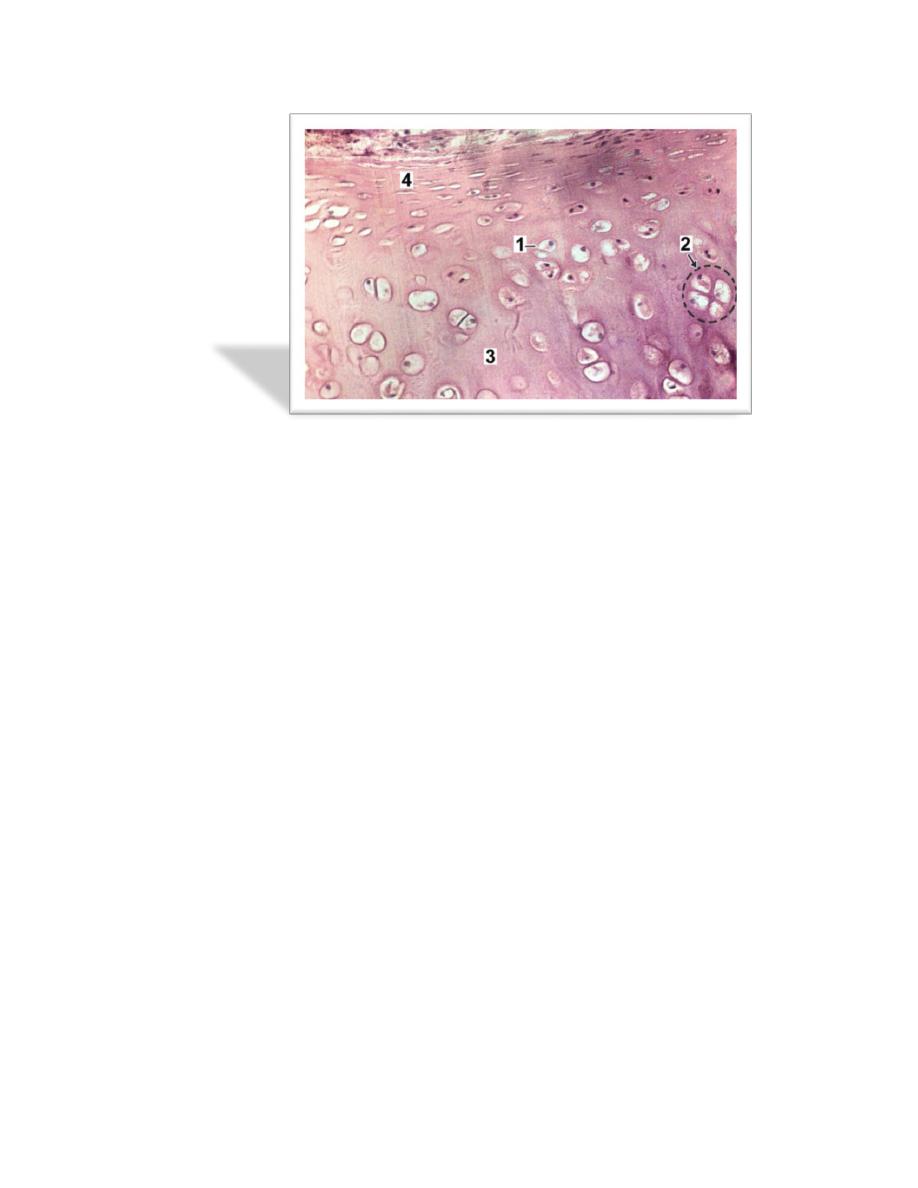
2. Fibrocartilage cartilage
Fibrocartilage is found in the symphysis pubis, the annulus fibrosis of
intervertebral discs (arrow above), and at points of attachment of tendons to bone.
It is a mixture between dense regular connective tissue (similar in many respects to
tendon or ligament) and hyaline cartilage. It combines the tensile strength, firmness,
and durability of tendon with resistance to compression of cartilage. In contrast to
other types of cartilage, fibrocartilage lacks a distinct perichondrium, which blends
imperceptibly with surrounding connective tissue or hyaline cartilage. Its matrix is
intensely eosinophilic because numerous collagen fibers are present. Arranged in
parallel bundles, often in line with the direction of pull or stress applied, they give a
characteristic fibrous appearance to the matrix.
10
3. Elastic cartilage
Fresh elastic cartilage appears more opaque and yellow than hyaline cartilage
because of abundant elastic fibers in its matrix. Elastic cartilage is resilient,
easily returning to its original shape after bending or distortion, and has more
flexibility and elasticity than other cartilage types. Its matrix contains a dense,
interwoven network of elastic fibers embedded in a small amount of amorphous
extracellular ground substance. This network is denser in the interior than at the
periphery. The spherical chondrocytes, which sit in lacunae, appear similar to
chondrocytes of hyaline cartilage, except that they are more closely packed and
often found singly in the lacunae (only a few isogenous nests are present). With
methods that stain selectively for elastin, the branching and anastomosing of the
elastic fibers are seen more clearly. The matrix also contains a small number of
type II collagen fibers that are masked by ground substance and intermingle
with the more abundant elastic fibers. Like hyaline cartilage (other than that on
articular surfaces of joints), elastic cartilage is enveloped by a perichondrium.
Blood vessels and lymphatics in the perichondrium do not penetrate the cartilage
interior. Elastic cartilage undergoes either appositional growth, from the
perichondrium, or interstitial growth, by chondrocyte mitosis. In contrast to other
types of cartilage, elastic cartilage does not calcify with age.
