Plasmodium
Family: Plasmodiidae
Genus: Plasmodium
Plasmodium ovale (P. ovale)
Plasmodium malariae (P. malariae)
Plasmodium vivax (P. vivax (P. vivax)
Plasmodium falciparum (P. falciparum)
- Protozoan parasite causing malaria
- Transmitted by the female Anopheles mosquito
- The parasite always has two hosts in its life cycle:
1- Dipteran insect (definitive host)-Anopheles mosquito
2- vertebrate host (intermediate host)-human
Plasmodium falciparum (P. falciparum)
Morphology & life cycle
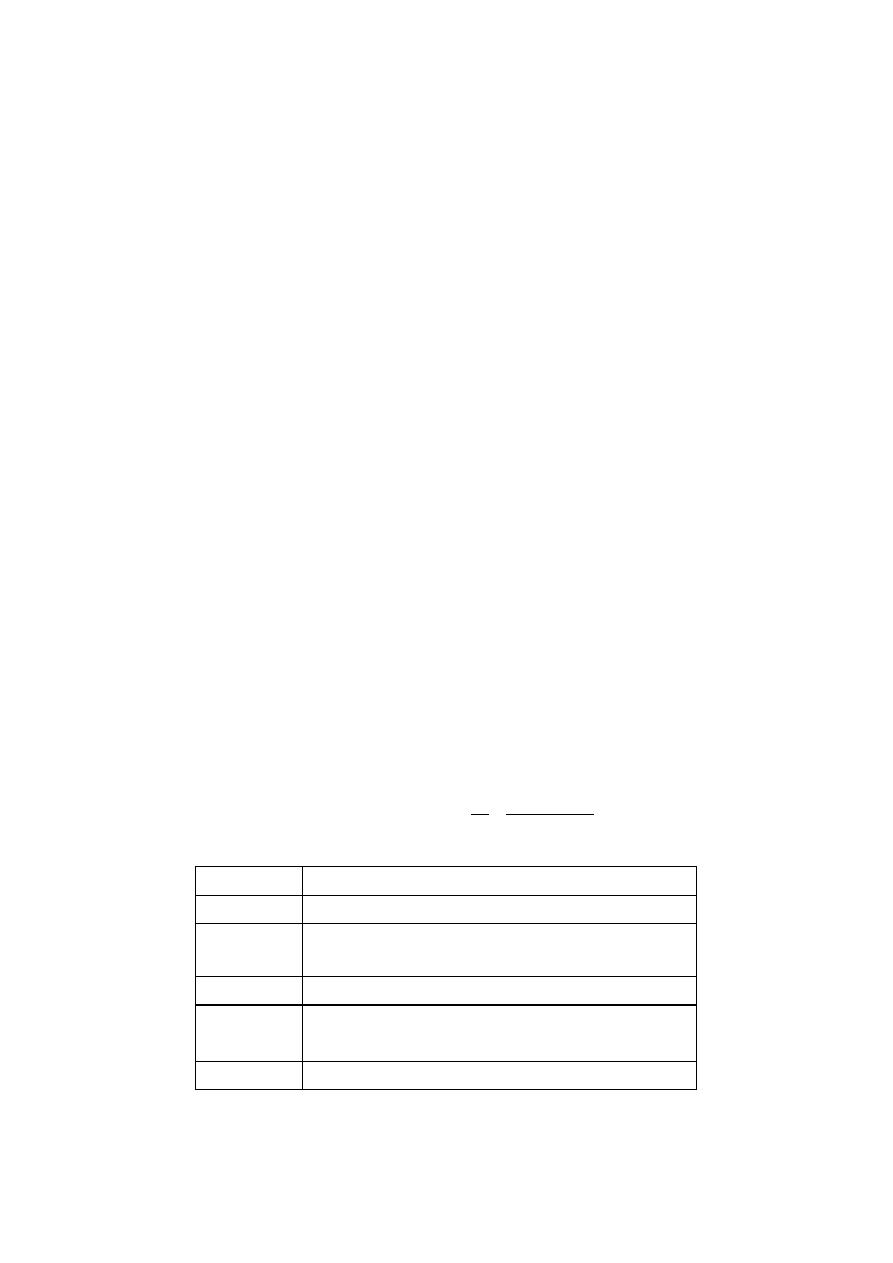
The life cycle of malaria is passed in two hosts (alternation of hosts) and two
reproductive stages:
1- Asexual stage:
- Vertebrate host - man (intermediate host)
- The parasite multiplies by schizogony which ends up with formation of
male and female gametocytes (gametogony).
2- Sexual stage:
- Invertebrate host - mosquito (definitive host)
- The sexual cycle takes place: Union of male and female gametes ends in
the formation of sporozoites (sporogony).

The life cycle passes in four stages:
Three in man:
Pre - erythrocytic schizogony
Erythrocytic schizogony
Exo- erythrocytic schizogony
One in mosquito:
Sporogony (sporozoites) infective stage
a- Schizogony:
1- infective female Anopheles mosquito bites man
2- it inoculates saliva containing sporozoites (infective stage)
3- pre-Erythrocytic schizogony - sporozoites reach the blood stream and
within 30 minutes enter the parenchymal cells of the liver, initiating a
cycle of schizogony
4- schizonts (mother cells), multiply to form thousands of tiny merozoites
(daughter cells)
5- merozoites are then liberated on rupture of schizonts and enter into the
blood stream. These merozoites invade the RBC’s
6- in case of P. falciparum and possibly P. malariae, all merozoites invade
RBC’s without re-invading liver cells. However, for P. vivax and P.
ovale, some merozoites invade RBC’s and some re-invade liver cells
initiating further Exo-erythrocytic schizogony
7- The merozoites reinvade fresh RBC’s repeating the schizogonic cycles
8- erythrocytic merozoites do not reinvade the liver cells. So malaria
transmitted by blood transfusion reproduces only erythrocytic cycle

b-
Gametogony:
Some merozoites that invade RBC’s develop into sexual stages (male
and female gametocytes). These undergo no further development until
taken by the mosquito.
c- Sporogony
: (extrinsic cycle in mosquito)
1- female Anopheles mosquito vector bites an infected person, it sucks
blood containing the different stages of malaria parasite. All stages
other than gametocytes are digested in the stomach.
2- the microgametocyte undergoes ex-flagellation. The nucleus divides
by reduction division into 6-8 pieces, which migrate to the periphery.
At the same, time 6-8 thin filaments of cytoplasm are thrust out, in
each passes a piece of chromatin. These filaments, the
microgametes, are actively motile and separate from the gametocyte.
3- the
macrogametocyte
by reduction
division
becomes a
macrogamete.
4- fertilization occurs by entry of a micro gamete into the macro gamete
forming a zygote.
5- the zygote changes into a worm like form (ookinete)
6- ookinete penetrates the wall of the stomach to develop into a
spherical oocyst
7- the oocystes increase in size. Thousands of sporozoites develop
inside the oocysts. Oocysts rupture and sporozoites are liberated in
the body cavity and migrate everywhere particularly to the salivary
glands. Now the mosquito is infective.
Symptoms
After being bitten by an infected mosquito, symptoms usually begin within 10–
30 days. Malaria can be uncomplicated or severe. Symptoms of uncomplicated
malaria might include:
chills
diarrhea
fever
headaches
muscle pain
nausea
sweating
vomiting
weakness.
Some less noticeable manifestations:
enlargement of the spleen or liver
increased breathing frequency
mild anemia
mild jaundice (yellowish eye whites and skin).
The disease can turn into severe malaria, if there are serious organ failures or
abnormalities in the bloodstream or metabolism. Symptoms of severe
malaria might include:
breathing difficulties
coma
confusion
death
focal neurologic signs
seizures
severe anemia.
During pregnancy malaria can lead to premature baby delivery or
delivery of a low-birth-weight baby
Diagnosis
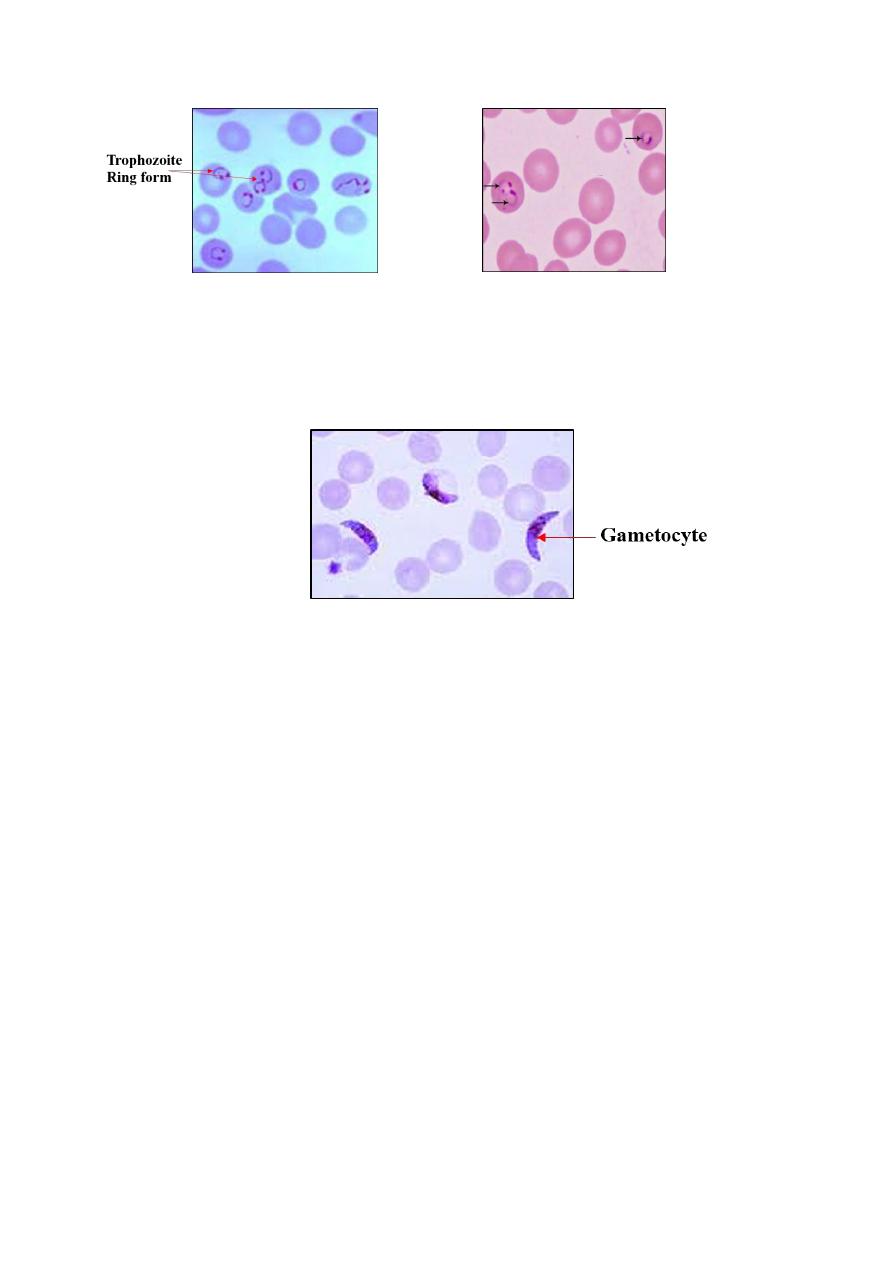
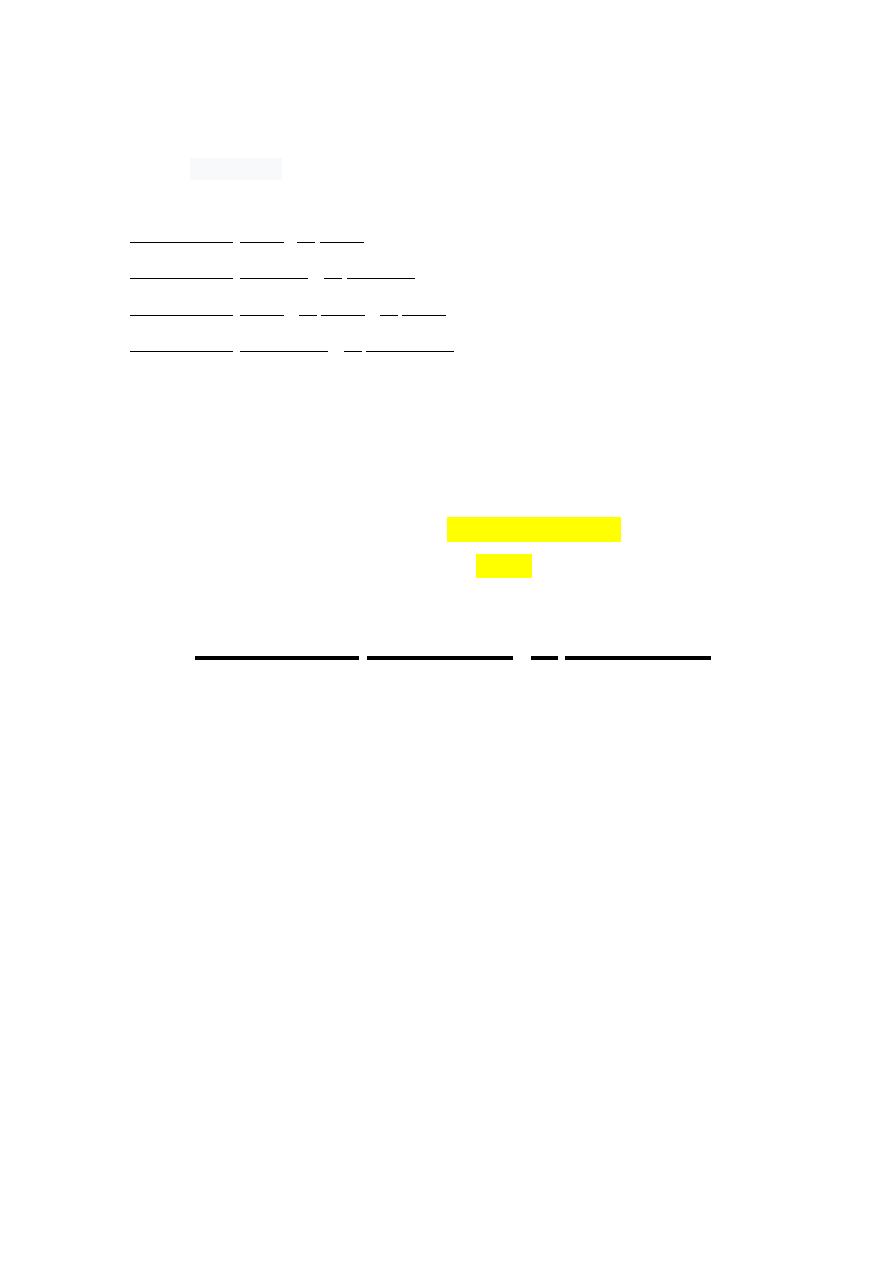
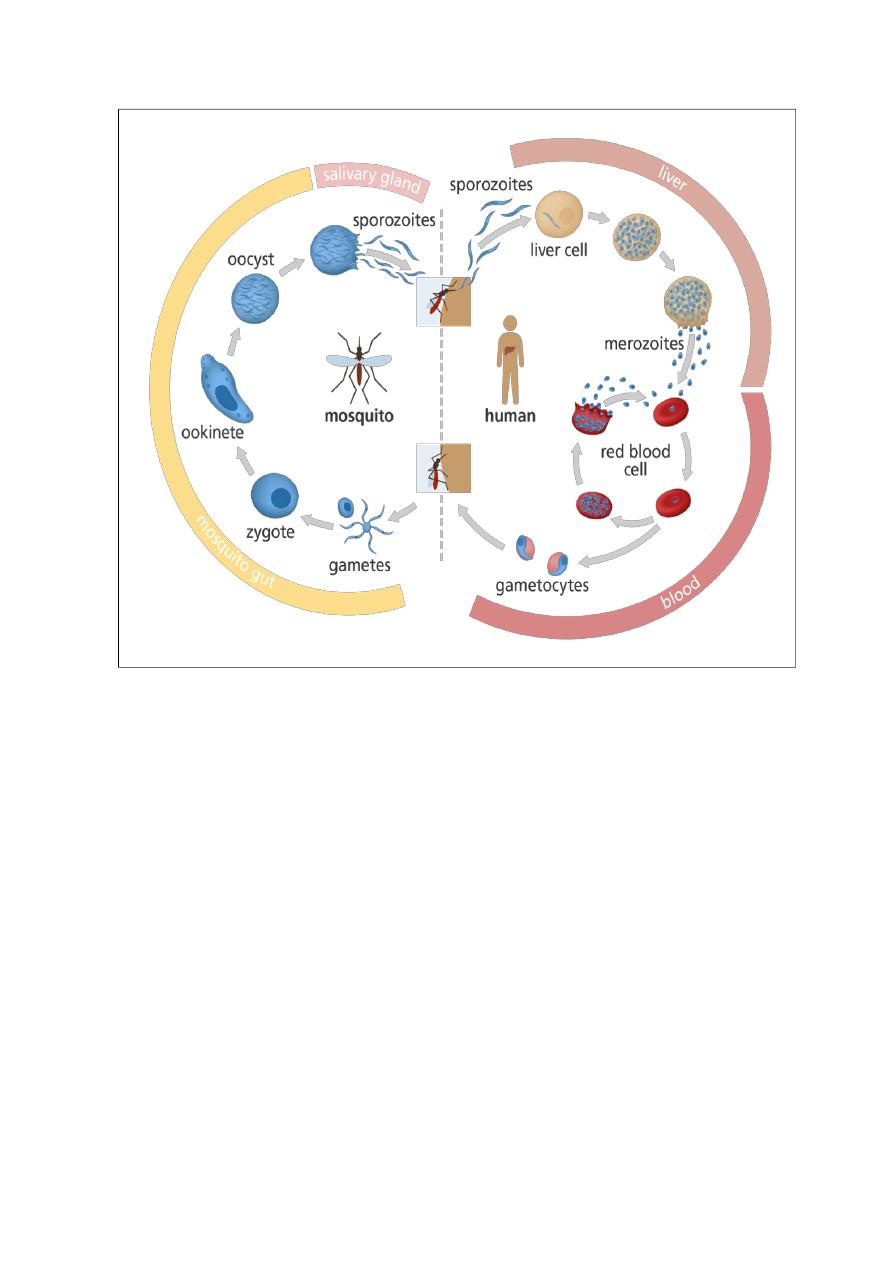
The preferred method to diagnose malaria and identify the species
of Plasmodium is by microscopic examination of a blood film. Each species has
distinctive physical characteristics. In P. falciparum, only early (ring-
form) trophozoites and gametocytes are seen in the peripheral blood
Trophozoite
Specimen Blood smear (thin, thick)
Method
Giemsa stain:
Add the stain and leave for 1-2
minutes. Then wash the slide with water
Diseases
Malaria
Seen
(ring
form),
gametocytes
(crescent form), RBCs
Treatment Chloroquine + doxycycline