1
Respiratory System Physiology
Dr. Amjed Hassan
lecture 6
Chemical control of respiration
The respiratory system functions to maintain proper levels of CO2 and O2
and is very responsive to changes in the levels of these gases in body fluids.
Types of chemoreceptors: Central and peripheral chemoreceptor
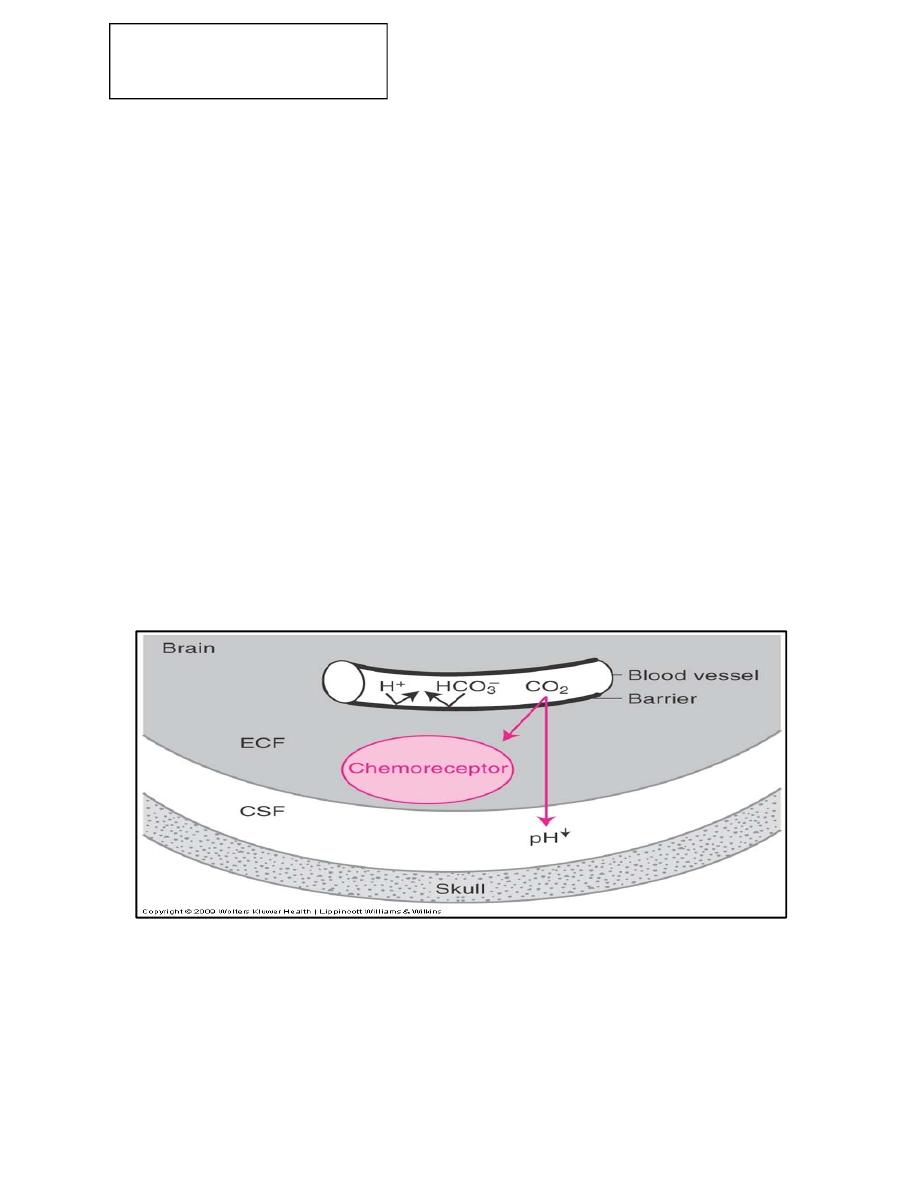
Central chemoreceptors
Located in the brain stem on the ventral surface of medulla near the point of
exit of the glossopharyngeal and vagus nerves and only a short distance from
the medullary inspiratory center, they communicate directly with the
inspiratory center, they respond to changes in h+ conc. Or PCO2 , or both in
CSF.
Stimuli for central chemoreceptors
Goal of central chemoreceptors is to keep arterial PCO2 normal, blood CO2
has little direct effect on central chemoreceptors, main stimulus is H+ ions in
CSF not blood H ion, blood brain barrier does not permit blood H ion, CO2
in blood passes through blood brain barrier combines with water of CSF to
form H2CO3, Carbonic acid in CSF dissociate into H ion and HCO3
This H ion stimulate respiratory center.
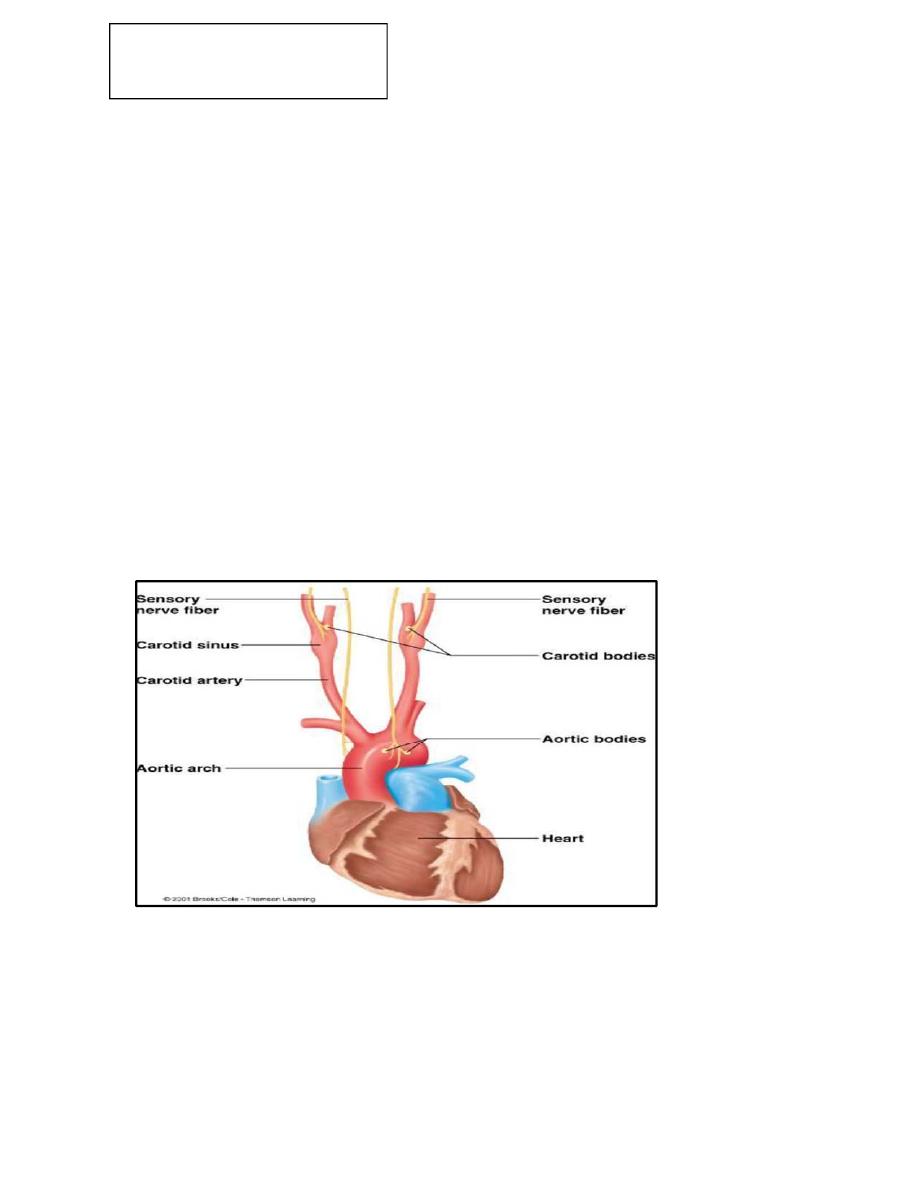
PERIPHERAL CHEMORECEPTORS
Located outside the brain at carotid bifurcation and arch of aorta
They senses changes in O2, CO2 and pH
2
Respiratory System Physiology
Dr. Amjed Hassan
lecture 6
Peripheral chemoreceptors
They mainly detect changes in arterial O2 ,also respond to a lesser extent to
changes in CO2 and pH, information perceived by chemoreceptors in turn
transmitted to respiratory centers to regulate respiratory activity
Structure of peripheral chemo receptors
Carotid bodies
Located bilaterally in bifurcation of common carotid arteries, sensations pass
through HERING’S nerve to glossopharyngeal nerve then to DRG of
medulla.
Aortic bodies
Located along arch of aorta , information travel to medullary DRG through
vagus nerve, each chemoreceptor receives special blood supply.
Stimulus for peripheral chemoreceptors (PC):
Decrease in arterial PO2: the most common responsibility of peripheral
chemoreceptors is to detect changes in arterial PO2.
However PC are relatively insensitive to changes in PO2.
They respond when PO2 decreases to less than 60mmHg

3
Respiratory System Physiology
Dr. Amjed Hassan
lecture 6
If arterial PO2 is 60mmhg, the breathing rate is relatively constant.
However, if arterial PO2 is less than 60mmhg, the breathing rate increases in
a very steep and linear fashion.
In this range of PO2 pc are very sensitive to O2 and they respond so rapidly
that the firing rate of the sensory neurons may change during a single
breathing cycle
Increase in arterial PCO2
The peripheral chemoreceptor also detect increases in PCO2 but the effect is
less important than their response to decrease in PO2.
Detection of changes in PCO2 by PC also is less important than detection of
changes in PCO2 by central chemoreceptors
Decrease in arterial pH
Decrease in arterial pH cause an increase in ventilation, mediated by
peripheral chemoreceptor for H+.
effect is independent of changes in the arterial PCO2
is mediated only by chemoreceptor in the carotid bodies (not by those in
aortic bodies).
In metabolic acidosis, there is decreased arterial pH, the peripheral
chemoreceptor are stimulated directly to increase the ventilation rate (the
respiratory compensation for metabolic acidosis).
Other receptors that modulate respiration
Irritant receptors
– There are receptors in the walls of the bronchi that respond to inhaled
irritants (e.g., dust, pollen, and chemicals) and trigger reflexes such as
coughing and sneezing.
Pulmonary stretch receptors
– There are a variety of stretch receptors in the smooth muscle of the
bronchial tree that influence the medullary respiratory center. These
receptors are responsible for the Hering–Breuer reflex, which exerts an
inhibitory influence as the lungs inflate, thereby limiting the depth of
respiration.

4
Respiratory System Physiology
Dr. Amjed Hassan
lecture 6
Muscle and joint receptors
– Muscle and joint receptors are activated during exercise and trigger an
increase in ventilation.
Response of the Respiratory System to Exercise and High Altitude
1.Exercise
– The onset of exercise causes a rapid initial increase in depth and frequency
of breathing, followed by a slower secondary rise. The precise triggers for
increased ventilation are unknown but are thought to involve receptors in
activated muscles and joints, an increase in body temperature, conscious
awareness of exercise, and other cerebral cortical activation.
– Ventilation is matched to increased metabolic demands of exercise (↑O2
consumption and ↑CO2 production).
– During exercise, there is an increase in pulmonary blood flow due to an
increase in cardiac output.
There is adequate time for gas exchange despite this increased pulmonary
blood flow.
– The ventilation/perfusion (V/Q) ratio progressively increases during
exercise because ventilation increases more than cardiac output (and
therefore pulmonary blood flow). The ratio may reach 4:1.
– PO2 , PCO2 , and pH are maintained at levels of a resting person during
light to moderate cardiovascular exercise. At peak cardiovascular exercise,
anaerobic respiration causes lactic acid buildup in blood. This causes arterial
pH to drop and stimulation of central chemoreceptors, leading to an increase
in respiratory rate and subsequent decrease in Pco2.
– After cessation of exercise, respiratory rate only gradually returns to
resting values while lactic acid is metabolized.
2.Acclimatization to high altitude:
In the high altitude, the human body compensates the low partial oxygen
pressure by changing ventilation or affinity of Hb to oxygen or total Hb
concentration. Hyperventilation induced by the decreased partial oxygen
pressure. This lowers the arterial partial carbon dioxide pressure and causes
respiratory alkalosis which cause hyperventilation. This also improves the
oxygenation of the blood. However, in spite of all these adaptation
mechanisms, the partial oxygen pressure in the arterial blood can not be

5
Respiratory System Physiology
Dr. Amjed Hassan
lecture 6
increased more than the partial oxygen pressure in the inspired air. As a
result partial pressure of oxygen in the arterial blood decreases with
increasing altitude.
The oxygen saturation of the arterial and venous blood is 97% and 75%,
respectively. At high altitude the low oxygen content of red blood cells
stimulates 2-DPG production and decreases the affinity of Hb to oxygen,
which in turn facilitates the oxygen transport to the tissues.
Due to low oxygen partial pressure in the arterial blood at high altitude the
tissue hypoxia occurs and in response the kidneys secrete erythropoietin
hormone. Erythropoietin stimulates the production of red blood cells
resulting in polycythemia, which can cause oedema, ventricular hypertrophy
and heart failure.
Classification of Lung Disorders by Spirometry
By comparing recorded values of the resting FVC and FEV1 and
FEV1/FVC ratio obtained from the spirogram to the predicted values
obtained from nomograms, it is possible to group respiratory diseases or
disorders into two broad categories of restrictive or obstructive impairments.
Respiratory Investigations
1- Blood pH
2- Blood CO2
3- Blood O2
4- Maximum expiratory flow (400ml/min) (Peak Expiratory Flow Meter)
5- FVC (forced vital capacity) and FEV1 (forced vital capacity in the first
second).
Abnormalities:
1-Emphysema: excess air in the lungs. Chronic infection causes increase
mucus which chronic obstruction so air remain in alveoli that causes
overstretching of alveoli and alveolar obstruction. At the end, damage to
alveolar wall causes damage to capillaries which leads to pulmonary
hypertension and right sided heart failure.
2-Pneumonia: any inflammatory condition of the lung where the alveoli are
filled with fluid and blood cells. So in infection, the damage to alveoli
causes filling with fluid and blood forming consolidation and reduction of

6
Respiratory System Physiology
Dr. Amjed Hassan
lecture 6
available surface and reduction of VA/Q ratio resulting in hypoxemia and
hypercapnia.
3- Tuberculosis = TB
Cause: bacteria – Mycobacterium tuberculosis
Spread: primarily airborne – aerosol, multiple antibiotic resistant strains
have become a problem, may occur as latent of active infection, it attacks
various tissues, most often lungs.
4.Asthma: spastic contraction of smooth muscles of bronchioles because of
hypersensitivity to normal stimuli.
