1
Spore-Forming
Gram-Positive
Bacilli:
Bacillus & Clostridium Species:
Introduction
The gram-positive spore-forming bacilli are the bacillus and
clostridium species. These bacilli are ubiquitous, and because they form
spores they can survive in the environment for many years. Bacillus
species are aerobes, whereas clostridia are anaerobes.
Of the many species of both bacillus and clostridium genera, most do
not cause disease and are not well characterized in medical microbiology.
Several species, however, cause important disease in humans. Anthrax, a
prototype disease in the history of microbiology, is caused by Bacillus
anthracis. Anthrax remains an important disease of animals and
occasionally of humans, Bacillus cereus causes food poisoning and
occasionally eye or other localized infections. Clostridia cause several
important toxin-mediated diseases:
Clostridium tetani,
tetanus;
Clostridium botulinum, botulism; Clostridium perfringens, gas gangrene;
and Clostridium difficile, pseudomembranous colitis. Other clostridia are
also found in mixed anaerobic infections in humans
Bacillus species
The genus bacillus includes large aerobic, gram-positive rods occurring
in chains. Most members of this genus are saprophytic organisms
prevalent in soil, water, and air and on vegetation, such as Bacillus cereus
and Bacillus subtilis. B.cereus can grow in foods and produce an
enterotoxins which cause food poisoning. Such organisms may
occasionally produce disease in immunocompromised humans (eg,
meningitis, endocarditis, endophthalmitis, conjunctivitis, or acute
gastroenteritis). B. anthracis a major pathogen in this genus which cause
anthrax .
Typical Organisms & Growth Characteristics
The typical cells, measuring 1 x 3–4µm, have square ends and are
arranged in long chains; spores are located in the center of the nonmotile
bacilli. Colonies of B. anthracis are round and have a "cut glass"
appearance in transmitted light. Hemolysis is uncommon with B
anthracis but common with the saprophytic bacilli. Gelatin is liquefied .
2
The saprophytic bacilli utilize simple sources of nitrogen and carbon
for energy and growth. The spores are resistant to environmental changes,
withstand dry heat and certain chemical disinfectants for moderate
periods . Animal products contaminated with anthrax spores (eg, hides,
bristles, hair, wool, bone) can be sterilized only by autoclaving.
Bacillus Anthracis
Pathogenesis
Anthrax is primarily a disease of herbivores—goats, sheep, cattle,
horses, etc; other animals (e.g., rats) are relatively resistant to the
infection. Humans become infected incidentally by contact with infected
animals or their products. In humans, the infection is usually acquired by
the entry of spores through injured skin (cutaneous anthrax) or rarely the
mucous membranes (gastrointestinal anthrax), or by inhalation of spores
into the lung (inhalation anthrax).
The spores germinate in the tissue at the site of entry, and growth of
the vegetative organisms results in formation of a gelatinous edema and
congestion. Bacilli spread via lymphatics to the bloodstream, and they
multiply freely in the blood and tissues shortly before and after death.
B anthracis that does not produce a capsule is not virulent and does not
induce anthrax in test animals. The poly-D-glutamic acid capsule (protein
in nature) is antiphagocytic. The capsule gene is on a plasmid .Anthrax
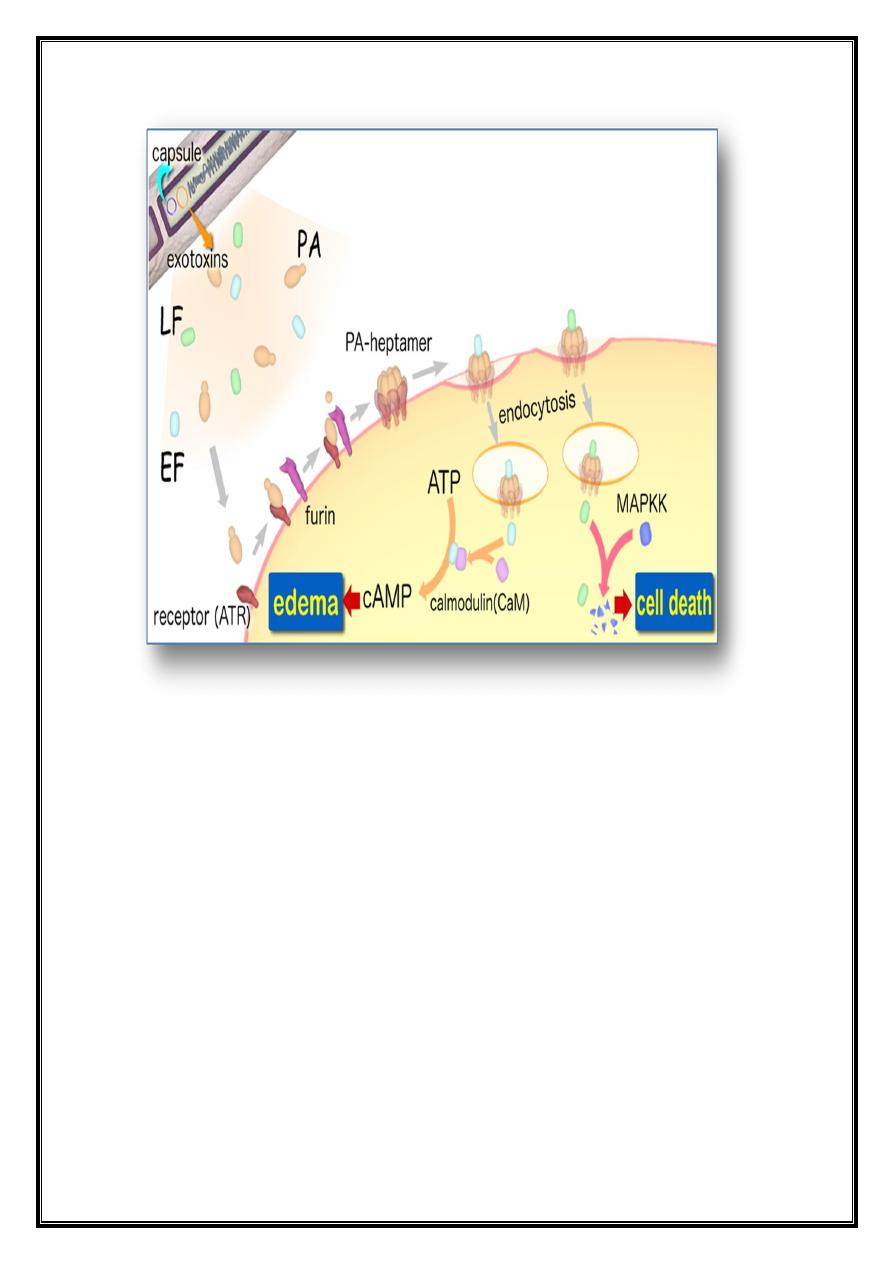
toxin is made up of three proteins: protective antigen (PA), edema factor
(EF), and lethal factor (LF). PA binds to specific cell receptors, and
following proteolytic activation it forms a membrane channel that
mediates entry of EF and LF into the cell. EF is an adenylate cyclase;
with PA it forms a toxin known as edema toxin. LF plus PA form lethal
toxin, which is a major virulence factor and cause of death in infected
animals.
3
Clinical Findings
In humans, approximately 95% of cases are cutaneous anthrax and 5%
are inhalation. Gastrointestinal anthrax is very rare .Cutaneous anthrax
generally occurs on exposed surfaces of the arms or hands, followed in
frequency by the face and neck. A pruritic papule develops 1–7 days after
entry of the organisms or spores through a scratch. The papule rapidly
changes into a vesicle or small ring of vesicles that coalesce, and necrotic
ulcer develops. The lesions and have a characteristic central black eschar.
Marked edema occurs. Lymphangitis and lymphadenopathy and systemic
signs and symptoms of fever, malaise, and headache may occur. After 7–
10 days the eschar is fully developed. Eventually it dries, loosens, and
separates; healing is by granulation and leaves a scar. In as many as 20%
of patients, cutaneous anthrax can lead to sepsis, systemic infection—
including meningitis—and death.
The incubation period in inhalation anthrax may be as long as 6 weeks.
The early clinical manifestations are associated with marked hemorrhagic
4
necrosis and edema of the mediastinum, Substernal pain may be
prominent, hemorrhagic pleural effusions and cough. Sepsis occurs, and
there may be hematogenous spread to the gastrointestinal tract, causing
bowel ulceration, or to the meninges, causing hemorrhagic meningitis.
The fatality rate in inhalation anthrax is high .
Diagnostic Laboratory Tests
Specimens to be examined are fluid or pus from a local lesion, blood,
and sputum. Stained smears from the local lesion or of blood from dead
animals often show chains of large gram-positive rods. Anthrax can be
identified in dried smears by immunofluorescence staining techniques.
When grown on blood agar plates, the organisms produce
nonhemolytic gray to white colonies with a rough texture and a ground-
glass appearance. Comma-shaped outgrowths (Medusa head) may project
from the colony. Gram stain shows large gram-positive rods.
Carbohydrate fermentation is not useful. In semisolid medium, anthrax
bacilli are always nonmotile, whereas related nonpathogenic organisms
(eg, B cereus) exhibit motility by "swarming." Virulent anthrax cultures
kill mice or guinea pigs upon intraperitoneal injection. An enzyme-linked
immunoassay (ELISA) has been developed to measure antibodies against
edema and lethal toxins .
Treatment
Many antibiotics are effective against anthrax in humans, but treatment
must be started early. Ciprofloxacin is recommended for treatment of
anthrax. Many antibiotics are active against B anthracis; penicillin G,
along with gentamicin or streptomycin, has previously been used to treat
anthrax.
In the setting of potential exposure to B. anthracis as an agent of
biologic warfare, prophylaxis with ciprofloxacin or doxycycline should
be continued for 4 weeks while three doses of vaccine are being given, or
for 8 weeks if no vaccine is administered.
Some other gram-positive bacilli, such as B cereus, are resistant to
penicillin
by
virtue
of
β-lactamase production. Doxycycline,
erythromycin, or ciprofloxacin may be effective alternatives to penicillin.
Epidemiology, Prevention, & Control
5
Soil is contaminated with anthrax spores from the carcasses of dead
animals. These spores remain viable for decades. Perhaps spores can
germinate in soil at pH 6.5 at proper temperature. Control measures
include (1) disposal of animal carcasses by burning or by deep burial in
lime pits, (2) decontamination (usually by autoclaving) of animal
products, (3) protective clothing and gloves for handling potentially
infected materials, and (4) active immunization of domestic animals with
live attenuated vaccines. Persons with high occupational risk should be
immunized.
Bacillus Cereus
Food poisoning caused by Bacillus cereus has two distinct forms: the
emetic type, associated with fried rice, and the diarrheal type, associated
with meat dishes and sauces. B cereus produces toxins that cause disease
that is more an intoxication than a food-borne infection. The emetic form
is manifested by nausea, vomiting, abdominal cramps, and occasionally
diarrhea and is self-limiting, with recovery occurring within 24 hours. It
begins 1–5 hours after ingestion of rice and occasionally pasta dishes. B
cereus is a soil organism that commonly contaminates rice. When large
amounts of rice are cooked and allowed to cool slowly, the B cereus
spores germinate and the vegetative cells produce the toxin during log-
phase growth or during sporulation. The diarrheal form has an incubation
period of 1–24 hours and is manifested by profuse diarrhea with
abdominal pain and cramps; fever and vomiting are uncommon. The
enterotoxin may be preformed in the food or produced in the intestine.
The presence of B cereus in a patient's stool is not sufficient to make a
diagnosis of B cereus disease .
B cereus is an important cause of eye infections, severe keratitis,
endophthalmitis, etc. Typically, the organisms are introduced into the eye
by foreign bodies associated with trauma. B cereus has also been
associated with localized infections and with systemic infections,
including endocarditis, meningitis, osteomyelitis, and pneumonia .
