Acute coronary syndromes
ST elevation myocardial infarction(STEMI)
ST elevation myocardial infarction(STEMI)
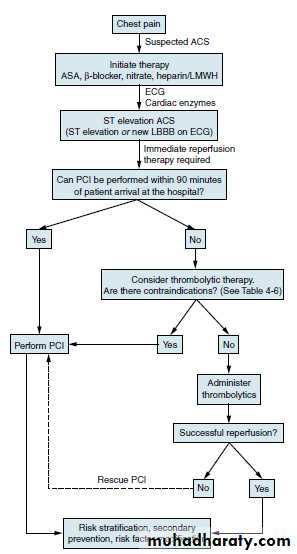
Patients with ACS who have ST-segment elevation or new left bundle branch block (LBBB) on their presenting ECG benefit significantly from immediate reperfusion and are treated as one group under the term ST-elevation myocardial infarction (STEMI).
LEFT BANDLE BRANCH BLOCK
ANT.WALL STEMIPresentation
• Chest pain is usually similar in nature to angina, but of greater severityand longer duration and is not relieved by sublingual (SL) nitroglycerin.
Associated features are nausea and vomiting, sweating, breathlessness,
and extreme distress.
• The pain may be atypical (e.g., epigastric) or radiate to the back.
• Diabetics, elderly, women, or hypertensive patients may suffer painless
(“silent” infarcts) and/or atypical infarction. Presenting features
include breathlessness from acute pulmonary edema, syncope or coma
from arrhythmias, acute confusional states (mania/psychosis), diabetic
hyperglycemic crises, hypotension or cardiogenic shock, central nervous system (CNS) manifestations resembling stroke secondary to sudden reduction in cardiac output, and peripheral embolization.
STEMI: diagnosis
STEMI diagnosis is based on a combination of history, ECG, and biochemical markers of cardiac injury.
In practice, history and ECG changes are diagnostic.
Biochemical markers of cardiac injury usually become available later and help reconfirm the diagnosis and provide prognostic information
(magnitude of rise).
ECG changes
ST-segment elevation occurs within minutes and may last for up to2 weeks. ST elevation of 2 mm in adjacent chest leads and 1 mm in
adjacent limb leads is necessary to fulfill thrombolysis criteria. Persisting
ST elevation after 1 month suggests formation of LV aneurysm.
Pathological Q waves indicate significant abnormal electrical
conduction but are not synonymous with irreversible myocardial
damage. In the context of a “transmural infarction” the Q waves may
take hours or days to develop and usually remain indefinitely. In the
standard leads, the Q wave should be 25% of the R wave, 0.04 s in
duration, with negative T waves. In the precordial leads, Q waves in V4
should be >0.4 mV (4 small sq) and in V6 >0.2 mV (2 small sq), in the
absence of LBBB (QRS width <0.1 s or 3 small sq).
ST-segment depression in a second territory (in patients with
ST-segment elevation) is secondary to ischemia in a territory other
than the area of infarction (often indicative of multivessel disease) or
reciprocal electrical phenomena. Overall, it implies a poorer prognosis.
T-wave inversion may be immediate or delayed and generally persists after the ST elevation has resolved.
Anterior ST elevation and/or Q waves in V1–V4/V5
Anterseptal ST elevation and/or Q waves in V1–V3
Lateral ST elevation and/or Q waves in V5–V6 and T-wave inversion/ST elevation/Q waves in I and aVL
Inferoseptal ST elevation and/or Q waves in II, III, aVF, and 5–V6 (sometimes I and aVL)
True posterior Tall R waves in V1–V2 with ST depression in V1–V3. T waves remain upright in V1–V2. This can be confirmed with an esophageal lead if available (method similar to an NG tube). This usually occurs in conjunction with an inferior or lateral infarct
RV infarction ST-segment elevation in the right precordial leads (V3R–V4R). Usually found in conjunction with inferior infarction. This may only be present in the early hours of infarction
Localization of infarcts from ECG changes
Conditions that may mimic ECG changes of a STEMILeft or right ventricular hypertrophy
LBBB or left anterior fascicular block
Wolff–Parkinson–White syndrome
Pericarditis or myocarditis
Cardiomyopathy (hypertrophic or dilated)
Trauma to myocardium
Cardiac tumors (primary and metastatic)
Pulmonary embolus
Pneumothorax
Intracranial hemorrhage
Hyperkalemia
Cardiac sarcoid or amyloid
Pancreatitis
Biochemical markers of cardiac injury
CK (creatine kinase)
• Levels twice the upper limit of normal are considered abnormal.
• Serum levels rise within 4–8 hours post-STEMI and fall to normal within 3–4 days. The peak level occurs at about 24 hours but may be earlier (12 hours) and higher in patients who have had reperfusion (thrombolysis or percutaneous coronary intervention [PCI]).
• False-positive rates of ~15% occur in patients with alcohol intoxication, muscle disease or trauma, vigorous exercise, convulsions, IM injections,
hypothyroidism, pulmonary embolism (PE), and thoracic outlet
syndrome.
CK-MB isoenzyme is more specific for myocardial disease. Levels may be elevated despite a normal total CK. However, CK-MB is also present in small quantities in other tissues (skeletal muscle, tongue, diaphragm, uterus, and prostate) and trauma or surgery may lead to false-positive results. If there is doubt about myocardial injury with CK-MB levels obtained, a cardiac troponin must be measured.
Cardiac troponins ( Tn T ,Tn I )
• Both TnT and TnI are highly sensitive and specific markers of cardiac injury.• Serum levels start to rise by 3 hours post-MI and elevation may persist up to 7–14 days. This is advantageous for diagnosis of late MI.
• In most STEMI cases, the diagnosis can be made using a combination of the clinical picture and serial CK/CK-MB levels. In the event of normal CK-MB levels and suspected noncardiac sources of CK, troponins can be used.
• Troponins can also be elevated in non ischemic myocyte damage, such as myocarditis, cardiomyopathy, and pericarditis.
Other markers
There are multiple other markers, but with increasing clinical availability of Troponin, measurements of these markers are not recommended. These include aspartamine transferase (AST) (rise 18–36 hours post-MI) and lactate dehydrogenase (LDH) (rise 24–36 hours post-MI).
Biomarker
Begins to risePeak value
Returns to normal
Myoglobin
1-2 hours
6-8 hours
1-2 days
CK-MB
2-6 hours
16-20 hours
1-2 days
CK
4-8 hours
16-24 hours
3-4 days
Trop T
4-6 hours
12-24 hours
7-10 days
AST
12-24 hours
36-48 hours
3-4 days
LDH
24-48 hours
72 hours
8-10 days
Factors associated with a poor prognosis
Age >70 years
Previous MI or chronic stable angina
Anterior MI or right ventricular infarction
Left ventricular failure at presentation
Hypotension (and sinus tachycardia) at presentation
Diabetes mellitus
Mitral regurgitation (acute)
Ventricular septal defect
Treatment of STEMI
All patients with STEMI should be admitted to an intensive care unit (ICU), e.g., coronary ICU (CICU).Stabilizing measures are generally similar for all ACS patients.
• All patients with suspected STEMI should have continuous ECG
monitoring in an area with full resuscitation facilities.
• Patients should receive immediate aspirin 325 mg po (if no
contraindications), analgesia, and oxygen. Secure IV access.
• Conduct rapid examination to exclude hypotension, note the presence of murmurs, and identify and treat acute pulmonary edema.
Right ventricular failure (RVF) out of proportion to left ventricular failure (LVF) suggests RV infarction.
Diagnosis is normally made on presentation (history and ECG changes of ST – elevation /new LBBBB )followed by rapid stabilizing measures to ensure institution of reperfusion therapy without delay. This is in contrast to NSTEMI/UA, where diagnosis may evolve over a period of
24–72 hours. (Reperfusion must not be delayed to wait for biochemical markers.)
Control of cardiac pain
• Morphine 2.5–10 mg IV is the drug of choice and may be repeated
to ensure adequate pain relief, unless there is evidence of emerging
toxicity (hypotension, respiratory depression). Nausea and vomiting
should be treated with metoclopramide (10 mg IV) or a phenothiazine.
• Oxygen should be administered at 2–5 L/min for at least 2–3 hours.
Hypoxemia is frequently seen post-MI due to ventilation–perfusion
abnormalities secondary to LVF. In patients with refractory pulmonary
edema, endotracheal intubation may be necessary. Beware of CO2
retention in patients with COPD.
• Nitrates may lessen pain and can be given (sublingual or IV) provided
that the patient is not hypotensive. These drugs should be used
cautiously in inferior STEMI, especially with right ventricular infarction,
as venodilation may decrease RV filling and precipitate hypotension.
Nitrate therapy has no demonstrated effect on mortality (ISIS-4).
Correction of electrolytes
Both low potassium and low magnesium may be arrhythmogenic and must
be supplemented, especially in the context of arrhythmias.
Strategies to limit infarct size
B-BlockadeEarly B-blockade has been shown to be beneficial by limiting infarct size, reducing mortality, and decreasing early malignant arrhythmias.
All patients (including primary PCI and thrombolysis patients) should have early B-blockade.
Patients with the following features may benefit most from B-blocker therapy:
• Hyperdynamic state (sinus tachycardia, hypertensive)
• Ongoing or recurrent pain or reinfarction
• Tachyarrhythmias such as AF
Use a short-acting agent IV initially (metoprolol 5 mg at a time repeated at 5-minute intervals to a maximum dose of 15 mg) under continuous ECG and BP monitoring. Aim for a HR of 60 beats per minute (bpm) and SBP 100–110 mmHg. If hemodynamic stability continues 15–30 minutes after the last IV dose, start metoprolol 50 mg po bid. Esmolol is an ultra-short acting IV B-blocker, which may be tried if there is concern whether the patient will tolerate B-blockers.
CONTRAINDICATIONS TO THE USE OF B- BLOCKERS
Absolute contraindications: heart rate (HR) <50, systolic blood pressure (SBP) <90 mmHg, moderate to severe heart failure, AV conduction defect, severe airways disease.
Relative contraindications: asthma, current use of calcium channel blocker and/or B-blocker, severe peripheral vascular disease with critical limb ischemia, large inferior MI involving the right ventricle.
ACE inhibitors
After receiving aspirin, B-blockade (if appropriate), and reperfusion, allpatients with STEMI/LBBB infarction should receive an ACE inhibitor
within the first 24 hours of presentation.
• Patients with high risk or large infarcts, particularly with an anterior STEMI, a previous MI, heart failure, and impaired LV function on imaging, will benefit most.
• The effect of ACE inhibitors appears to be a class effect; therefore,
one may use the drug that the physician is familiar with.
Reperfusion therapy (thrombolysis)
Indications for thrombolysis• Typical history of cardiac pain within previous 12 hours and ST elevation in two contiguous ECG leads (>1 mm in limb leads or >2 mm in V1–V6).
• Cardiac pain with newly presumed LBBB on ECG.
• If ECG is equivocal on arrival, repeat at 15- to 30-minute intervals to monitor progression.
• Thrombolysis should not be given if the ECG is normal or if there is isolated ST depression (true posterior infarct must be excluded).
Timing of thrombolysis
• Greatest benefit is achieved with early thrombolysis (especially if given within 1 1/2 hours(90min.s) of onset of first pain.
• Patients presenting between 12 and 24 hours from onset of pain should undergo thrombolysis only with persisting symptoms and ST-segment elevation.
• Elderly patients (>65 years) presenting within the 12- to 24-hour time period with symptoms are best managed by primary PCI, as thrombolysis has been demonstrated to result in increased incidence of cardiac rupture.
Choice of thrombolytic agent
• This is partly determined by each center’s local thrombolysis strategy.
• Allergic reactions and episodes of hypotension are greater with streptokinase (SK).
• Bolus agents are easier and quicker to administer, with a decrease in drug errors in comparison to first-generation infusions.
• Recombinant tissue-type plasminogen activator (rtPA) has a greater reperfusion capacity and a marginally higher 30-day survival benefit than that of SK, but this agent has been associated with an increased risk of hemorrhage.
• More recent rtPA derivatives have demonstrated a higher 90-minute TIMI-III (coronary reperfusion scale) flow rate, but have shown similar 30-day mortality benefits to those with rtPA.
• An rtPA derivative (rather than SK) should be considered for any patient with any of the following:
• Large anterior MI, especially if within 4 hours of onset
• Previous SK therapy or recent streptococcal infection (as this has been shown to be a risk factor for allergic reactions to SK)
• Hypotension (systolic BP <100 mmHg)
• Low risk of stroke (age <55 years, systolic BP <144 mmHg)
• Reinfarction during hospitalization where immediate PCI facilities are not available
Doses and administration of thrombolytic agents
Streptokinase (SK)• Give as 1.5 million units in 100 mL normal saline IV over 1 hour.
• There is no indication for routine heparinization after SK; there is no clear mortality benefit and there is a small increase in risk of hemorrhage.
Recombinant tissue-type plasminogen activator (rtPA, alteplase)
• The GUSTO trial suggested that the “front-loaded” or accelerated rtPA is the most effective dosage regimen.
• Give 15 mg bolus IV then 0.75 mg/kg over 30 minutes (not to exceed 50 mg), then 0.5 mg/kg over 60 minutes (not to exceed 35 mg).
• This should be followed by IV heparin.
Reteplase
• Give two IV bolus doses of 10 units 10 minutes apart.
Tenectaplase
• Give as injection over 10 seconds at 30–50 mg according to body weight (500–600 µg/kg). Maximum dose is 50 mg.
APSAC (anistreplase)
• Give as an IV bolus of 30 mg over 2–5 minutes.
Complications of thrombolysis
• Bleeding is seen in up to 10% of patients. Most incidents are minor and at sites of vascular puncture. Local pressure is generally sufficient to stop this bleeding but occasionally transfusion may be required. In extreme cases, SK may be reversed by tranexamic acid (10 mg/kg slow
IV infusion).
• Hypotension during the infusion is common with SK. Treatment consists of placing the patient in a supine position and slowing/stopping infusion until the blood pressure rises. Treatment with cautious (100–500 mL) fluid challenges may be required, especially in inferior/ RV infarction. Hypotension is not necessarily evidence of an allergic reaction and may not warrant treatment as such.
• Allergic reactions are common with SK and include a low-grade fever, rash, nausea, headaches, flushing, and, rarely (0.1%), anaphylaxis. Give hydrocortisone 100 mg IV with chlorpheniramine 10 mg IV.
• Intracranial hemorrhage is seen in ~0.3% of patients treated with SK and in ~0.6% with rtPA.
• Reperfusion arrhythmias (most commonly a short, self-limiting run of idioventricular rhythm) may occur.
• Systemic embolization may occur from lysis of thrombus within the left atrium, LV, or aortic aneurysm.
Contraindications to thrombolysis
Absolute contraindications to thrombolysis Active internal bleedingSuspected aortic dissection
Recent head trauma and/or intracranial neoplasm
Previous hemorrhagic stroke at any time
Previous ischemic stroke within the past 1 year
Previous allergic reaction to fibrinolytic agents
Trauma and/or surgery within past 2 weeks at risk of bleeding
Relative contraindications to thrombolysis
Trauma and/or surgery more than 2 weeks previouslySevere uncontrolled hypertension (BP >180/110)
Nonhemorrhagic stroke over 1 year ago
Known bleeding diathesis or current use of anticoagulation within therapeutic range (INR 2)
Prolonged (>10 minutes) cardiopulmonary resuscitation
Prior exposure to SK (if planning to give SK, especially previous 6–9 months)
Pregnancy or postpartum Lumbar puncture within previous 1 month
Menstrual bleeding or lactation
History of chronic severe hypertension
Non compressible vascular punctures (e.g., subclavian central venous lines)
Reperfusion by primary PCI
Primary PCI is the current gold-standard reperfusion strategy for treatment of STEMI.
Indication for primary PCI
• All patients with chest pain and ST-segment elevation or new LBBB fulfill primary PCI criteria (compare with indications for thrombolysis).
• This includes a group of patients in whom ST-segment elevation may not fulfill all criteria for thrombolysis.
• In general, patients in whom thrombolysis is contraindicated should be managed by primary PCI.
Outcome in primary PCI
• A superior outcome in patients with STEMI who are treated with primary PCI in comparison to outcomes with thrombolysis.• There is a significant short-term, as well as long-term, reduction in mortality and major adverse cardiac events (MACE) (death, nonfatal reinfarction, and nonfatal stroke) in STEMI patients treated with primary PCI, with better LV function, a higher vessel patency rate, and less recurrent myocardial ischemia.
• Interhospital transportation for primary PCI (community hospital to invasive center) is safe, and primary PCI remains superior to thrombolysis despite the time delays involved.
It is generally accepted that in the acute phase only the “culprit” lesion(s) and vessel(s) will be treated. The pattern of disease in the remainder of the vessels will determine whether further revascularization should be performed as an inpatient or an elective
case in the future.
• STEMI patients treated with uncomplicated primary PCI can often be discharged safely within 72 hours of admission without the need for further risk stratification.
• Primary PCI is more cost-effective in the long term than thrombolysis with significant savings from fewer days in the hospital, less need for readmission, and less heart failure.
• Post-discharge care, secondary prevention, and rehabilitation remain identical to that for other MI cases.
Rescue PCI
Rescue PCI may be performed as an adjunct to thrombolysis but should be reserved for patients who remain symptomatic post-thrombolysis failure to reperfuse) or develop cardiogenic shock. We recommend that all patients who continue to have post-thrombolysis symptoms and/or ongoing ST-elevation with or without symptoms be discussed with the local invasive cardiac center for urgent catheterization and revascularization.Surgery for acute STEMI
CABG in the context of an acute STEMI is of value in the following situations:
• High-risk coronary anatomy on catheterization (left main stenosis, left anterior descending [LAD] ostial disease).
• Complicated STEMI (acute mitral regurgitation, or ventricular rupture)
• STEMI patients (with or without successful thrombolysis) with additional coronary lesions whose anatomy is best served by CABG on prior or subsequent catheterization
STEMI: additional measures
Low-molecular-weight and unfractionated heparin
UFH
• There is no indication for “routine” IV heparin following SK.
• IV heparin (4000 U/max IV bolus followed by 1000 U/hr max adjustedf or an aPTT ratio of 1.5–2.0 times control) should be used routinely following rtPA and its derivatives for 24–48 hours.
LMWH
• There is clinical trial data supporting the use of LMWH and thrombolysis (e.g., enoxaparin 30 mg IV bolus, then 1 mg/kg SC q12h).
• As an alternative to UFH, LMWH can be used at a prophylactic dose to prevent thromboembolic events in high-risk patients.
Clopidogrel
Calcium antagonists
• This should be administered to all patients undergoing primary PCI (loading dose 300–600 mg po followed by 75 mg qd).
• The length of therapy is determined by the type of stent used. Drug eluting stents require longer term use of clopidogrel than bare-metal stents (current guidelines for ACS is 1 year of Plavix).
• These are best avoided, especially in the presence of LV impairment.
• Diltiazem and verapamil started after day 4–5 in post-MI patients with normal LV function may have a small beneficial effect.
• Amlodipine is safe to use in patients with poor LV function post-MI.
• Nifedipine has been shown to increase mortality and should be avoided.