
1
Pediatrics
History Taking
----------------------------------------------------------------------------------------------
www.facebook.com/ibnlatef
https://goo.gl/RpvNsl
Ibnlatef
Notes

2
Subject1:
History questions
Identification:
Name of baby (triple name).
Age and datell of birth.
Gender.
Blood group
Source of history (mother – father – grandmother).
Occupation of parents.
Residence of parents.
Religion of parents.
Date of admission.
Date of examination.
Chief compliant:
Mention the main reason that brings the patient to the hospital (up to 2 chief
compliant).
Duration of chief compliant.
History of present illness:
Last time the patient was well.
The story (take it from the source like the mother, ask her to tell you the full story then
summarize it and write it in her words).
Analysis of the symptoms.
Complete the same system.
Relevant systems (ask about any system related to the involved system).
Routine questions: always ask about (fever, sweating, urine output, feeding, activity,
sleep, weight loss).
Ask about attention to private doctor or primary health centers PHC (ask about
investigations, treatment, improvement or not).
Admission (ask about investigations, treatment, improvement or not).
Any new event that may occur during hospitalization ((worsening of baby condition
ask about sleep + activity (smile/fatigue) + feeding all will decreased)).
Outcome (the condition of patient at the moment of taking history).
((Convert these points to story and write it))

3
Systems review:
(questions here depend on the age of baby)
GIT abdominal pain, diarrhea, constipation, vomiting, hematemesis, melena,
jaundice, nausea and loss of appetite (the last two describe as poor feeding).
Respiratory SOB, noisy breathing, cough, hemoptysis, sputum.
CVS dyspnea, palpitation (the mother could feel palpitation of her baby), cyanosis.
Genitourinary color and amount of urine, hematuria, pyuria, dysuria (crying during
urination), frequency, any abnormality in the genetalia.
Nervous system headache, convulsions, abnormal movements, abnormal hearing
or vision.
Loco-motor joint pain and stiffness, joint swelling, abnormal movements, restricted
movements.
Hematology epistaxis, bruises, patichae, bleeding from anywhere.
Skin dryness, discoloration, pigments, itching, rash, lump, hair and nail changes.
Pre-natal (Ante-natal):
ANC (attend regular visits to PHC, take folic acid and supplements).
Disease of mother during pregnancy (infections like Toxoplasma-HIV-Rubella-
Cytomegalovirus-Chickenpox-Hepatitis --- TORCH infection appear as fever + skin rash
+ joint swelling --- other diseases like D.M and hypertension and anemia).
Drugs taken during pregnancy.
Exposure to radiation during pregnancy.
Smoking.
Bleeding.
Previous abortion or neonatal death.
Admission to hospital for any reason.
Vaccine.
Number of child.
Natal:
Place of delivery (at home or hospital).
Type of delivery (vaginal or caesarian section CS) if CS what is the indication? Elective
or emergency?
Duration of delivery (normal or prolonged).
Any complication during labor.
Instrument use in the delivery.
Gestational age (pre-term or term or post-date or post-term).
Weight of the baby (normal AGA, Small SGA, Large LGA).
Post-natal:
(first 28 days of life)
Immediate crying.
4
Time of discharge from the hospital (24 hours – 48 – more).
NICU admission.
When the baby passed urine (within first 24 hours) and meconium (the first stool)
(within first 48 hours).
Movement.
Neonatal jaundice, Cyanosis (fetal distress), Fit, bleeding.
Baby developed other diseases? Treatment?
Past-medical history:
Previous similar disease.
Previous admissions.
Chronic diseases.
Previous infections (measles, others).
Blood transfusion.
Past-surgical:
Previous operations (indication, type, outcome).
Circumcision in male and ear piercing in female (at which
age, any complications)…
Hospitalization.
Drug history:
Drug taking by mother (chronic use).
Drug taking by baby (chronic use).
Allergy to drug and other substances.
Feeding history:
1- Breast feeding:
Way of feeding (using both right and left breast each feeding time).
Regular (at least every 3 hours) or on demand.
Any problem with feeding (large nipple, others).
2- Bottle feeding:
Way of feeding.
Way of preparation.
Type of formula use (lactose free, soy milk formula, others).
Way of sterilization of the bottle (boiling, Washing, brushing).
Number of bottles.
Number of feeding.
Regular (at least every 3 hours) or on demand.
Complications of circumcision:
Bleeding.
Infection.
Insufficient Foreskin Removed.
Excessive Foreskin Removed.
Adhesions / Skin Bridges.
Inclusion Cysts.
Abnormal Healing.
Meatitis.
Meatal Stenosis.
Urinary Retention.
Phimosis.
Chordee.
Hypospadias.
Epispadias.
Urethrocutaneous Fistula.
Necrosis of the Penis.
Amputation of the Glans.
Death.
Source: med.stanford.edu
5
Any problem occur after bottle feeding (diarrhea, others).
Put the bottle in freeze for cooling.
3- Mixed feeding (breast and bottle feeding).
4- Semi-solid or solid food:
At which age given.
Type.
Any problem occur after this feeding.
5- Weaning: at which age milk was taken off his diet.
6- Pica: Ask if the child eat soil, wood or other things (caused by iron deficiency anemia –
Ca deficiency – lead poisoning).
Immunization history:
Take the vaccines on regular Iraqi schedule or not?
On national immunization day only?
Type of vaccine? , At which age?
Any complications (fever, pain, convulsion, rash, excessive crying) pertussis vaccine
cause (convulsion, shock).
Time of last vaccine.
Notes: RV not give to baby after 3 and 8 months of age / BCG not give to baby after 1
year of age / BCG should return if the scar not appear.
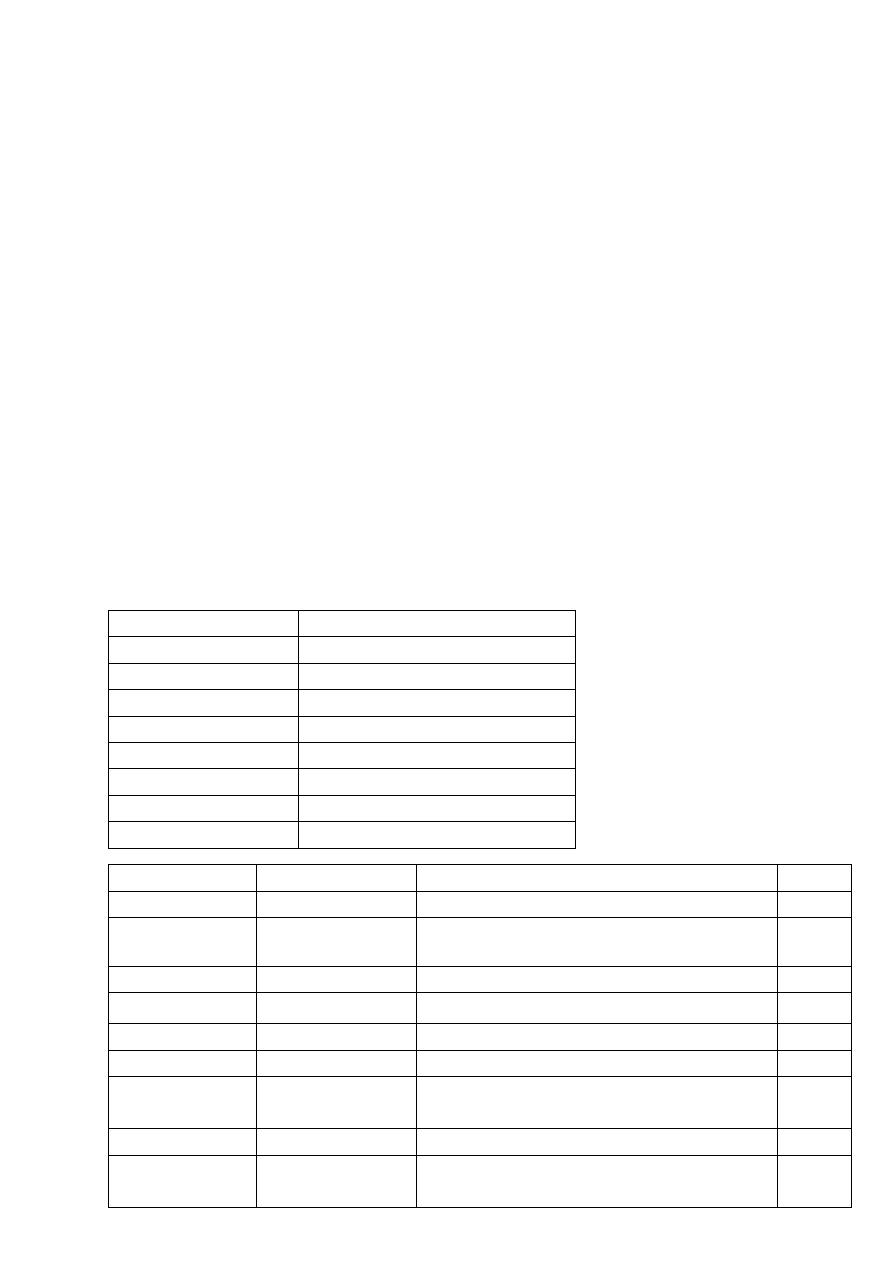
Age
VACCINE
24 hours after birth BCG, HBV , OPV
2 months
DTP-HepB-Hib, OPV, RV
4 months
DTP-Hib, OPV, RV
6 months
DTP-HepB-Hib, OPV, RV
9 months
Measles, Vit.A 100,000 U
15 months
MMR
18 months
DTP-Hib, OPV, Vit.A 200,000 U
4-6 years
DTP, MMR, OPV
Name
In Arabic
Type
Route
BCG
بي سي جي
Live attenuated TB bacteria
ID
HBV
إالتهاب الكبد
الفيروسي ب
Inactivated hepatitis B virus
IM
OPV
شلل األطفال فموي
Live attenuated Polio virus
Oral
RV
الفايروس العجلي
Live attenuated Rotavirus
Oral
Measles
الحصبة المنفردة
Live attenuated measles virus
SC
MMR
الحصبة المختلطة
Live attenuated, mumps, rubella viruses SC
DTP
اللقاح الثالثي
Diphtheria and Tetanus Toxoid +
inactivated pertussis bacteria
IM
DTP-Hib
اللقاح الرباعي
DTP + Inactivated Influenza virus
IM
DTP-HepB-Hib
اللقاح الخماسي
DTP + Inactivated Influenza virus +
Inactivated hepatitis B virus
IM

6
Developmental:
Gross motor (sit, stand, walk) or crawl.
Fine motor (Grasp, move object from hand to hand, etc.).
Social (smile, laugh, etc.).
Speech, Vision, Hearing.
Urination and defecation control.
Family history:
Health of parents, brothers and sisters.
Family history of same illness.
Family history of chronic disease or infectious disease.
Family history of unexplained death.
Order of baby in the family.
Any illness in the family.
Social history:
Rural or urban.
Source of water.
Income.
Level of education and occupation of parents.
Crowding index (number of persons/number of rooms) below 3 is normal and
above 3 is crowding.
Any domestic animals.
Ventilation.
Smoking.
Sewage disposal.
Obstetrical and gynecological history:
For girls because pediatric age up to 18 years.
1. Age of menarche.
2. Any abnormality in the cycle.
3. Use any contraceptive or traditional methods.
4. Any gynecological infection or disease.
5. Any gynecological procedure or surgery.

7
Subject2:
GIT history
1-History of bowel motion (diarrhea):
Amount:
o Increased (watery or loose) in small intestine disease and infections like V.Cholera.
o Decreased (small and bulky) in large intestine disease like Colitis.
Frequency:
o High frequency in small intestine diseases.
o Low frequency in large intestine diseases.
Color:
o Normal color either yellow, brown or green.
o Green color normal, from breastfeeding, drugs, food (Spinach or other leafy
vegetables).
o Dark green color from bile.
o Black color stomach bleeding, food (grape juice), drugs (iron).
o Red color lower GIT bleeding, drugs (Amoxicillin), food (beets).
o White color biliary obstruction (no bile), milk only diet, drugs (antacids).
Presence blood:
o Intestinal infection.
o Infant colitis.
o Intussusception.
o Inflammatory bowel disease.
o Antibiotic-associated colitis
Presence mucus:
o Intussusception.
o Inflammatory Bowel Disease.
o Meckel's Diverticulum.
Consistency:
o Watery occur due to V.Cholera.
o Loose occur in small bowel diseases.
o Firm occur in large bowel diseases.
Odor:
o Not important.
o Fish odor small intestine disease, infections (V.Cholera and viral).
o Offensive odor Bacteria, Amebiasis, coeliac disease, lactose intolerance.
Day or night:
o Only at night UTI or Typhoid.
o Only day related to feeding.
o Day and night not related to feeding and it is secretory type related to infection
like Typhoid, UTI, TB, Brucellosis.
Associated features:
o Colic – fever – sweating – anorexia.
8
Presence of Tenesmus:
o Occur during or after defecation.
o Causes: Constipation, Hemorrhoids, Crohn's disease, Anal abscess, Rectal abscess.
Diarrhea with vomiting:
o Viral infection.
o Food poisoning.
o Bacterial infection.
o Traveler's diarrhea.
Diarrhea with cough:
o Infections: Rotavirus, adenovirus.
o Respiratory causes: cystic fibrosis, TB.
Notes:
Viral infection (Rota virus) flu like illness then vomiting then diarrhea (high amount
+ loose + high frequency more than 10) + low grade fever or no fever.
V.Cholera large amount + watery + loose + high frequency.
Shigellosis Bloody diarrhea + Tenesmus.
Fissure in ano Fresh + large amount of blood per-rectum.
Hypokalemia Diarrhea + abdominal distention + weakness.
Toddler diarrhea due to excessive sweets & juices consumption, it relived by
fasting.
Parenteral diarrhea due to systemic cause rather than GIT like meningitis, UTI, Otitis
How to know parenteral = normal general stool + stool culture –ve + source of infection.
No-infectious cause of diarrhea diverticulum, ischemic colitis, hemorrhoids.
Metabolic acidosis occur in diarrhea due to loss of HCO3- cause deep and decrease
breathing to waste CO2.
Secretory diarrhea not affected by feeding – osmotic diarrhea affected by feeding.
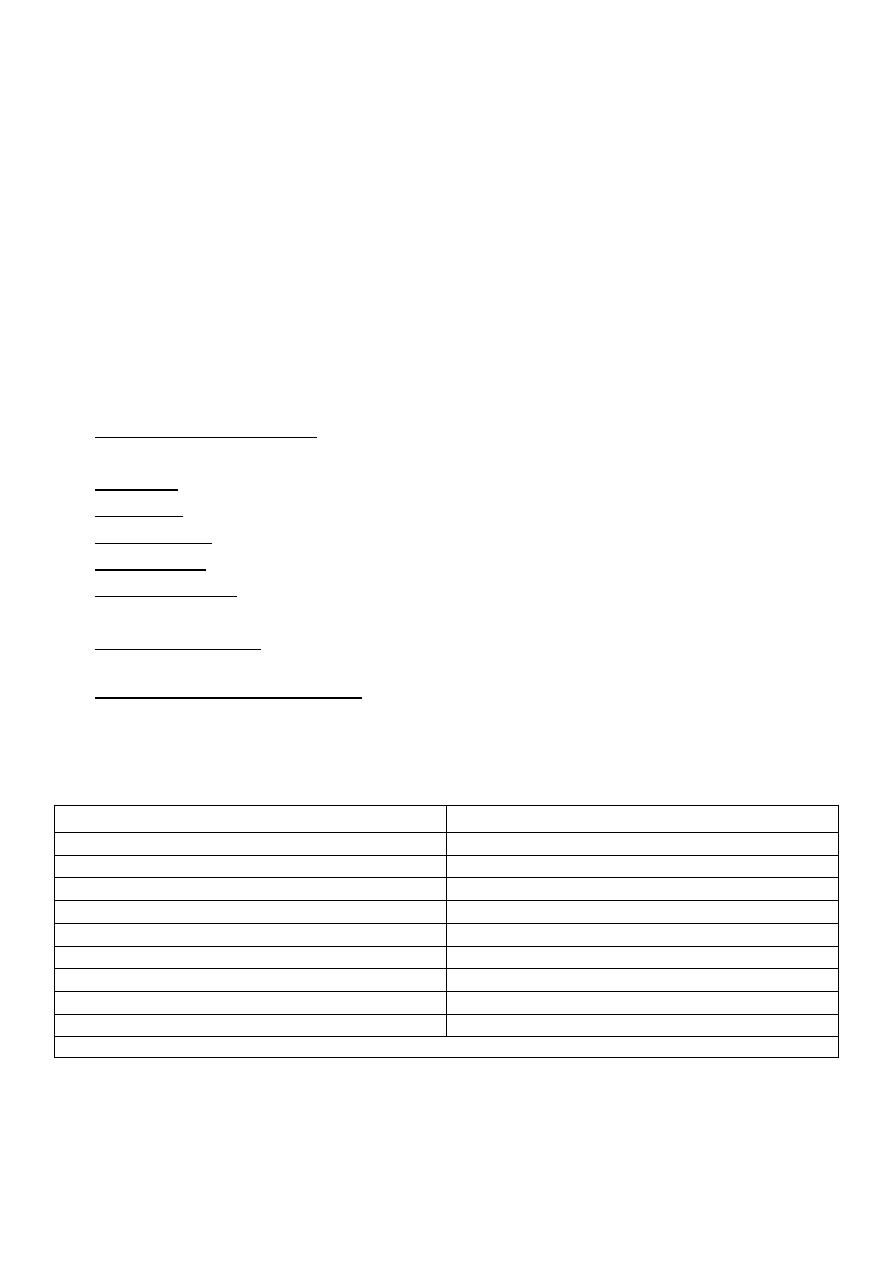
Amebic dysentery
Bacillary dysentery
Caused by E.Histolytica
Caused by salmonella or shigella
Trophozoite in feces
Bacteria in feces
Gradual slow onset
Acute onset
Not ill (toxic)
Looks ill (toxic)
Long incubation period (weeks)
Short incubation period (days)
Pink or chocolate color
Green color
Abdominal pain
Abdominal pain
Features of large intestinal diarrhea
Features of small intestinal diarrhea
No systemic manifestations
There are systemic manifestations
Sometimes amebic dysentery has acute form like bacterial dysentery in low immunity and old people

9
2-Constipation:
Onset and duration of decreased bowel motion.
Frequency of defecation.
Associated with pain, blood, mass.
Fluid intake, type of nutrition.
Chronic disease (like coeliac).
Psychological problem.
Any treatment or intervention.
Notes:
Frequency of defecation:
o Infants in first week four stools per day.
o 1 year of age two stools per day.
o Breast-fed infants may not pass stools for several days and be entirely healthy.
o 4 years of age varies from three stools per day to three stools per week (similar
to adults).
Definition of constipation is the infrequent passage of dry, hardened feces often
accompanied by straining or pain, there may be abdominal pain which waxes and
wanes with passage of stool or overflow soiling (Emotions and behavior).
Causes of constipation:
o Multifactorial.
o Arising in acutely ill young children.
o Precipitated by dehydration or reduced fluid intake.
o Problems with toilet training, unpleasant toilets or stress.
o Hirschsprung disease.
o Anorectal abnormalities.
o Anal fissure causing pain.
o Hypothyroidism.
o Hypercalcemia.
Treatment:
o Disimpaction regimen of stool softeners for 1-2 weeks initially with a macrogol
laxative (polyethylene glycol) + electrolytes (Movicol Paediatric Plain).
o If this proves unsuccessful, start stimulant laxative senna, or sodium
picosulphate.
o If the polyethylene glycol + electrolytes is not tolerated use an osmotic laxative
o Maintenance treatment.
o Dietary interventions sufficient fluid and a balanced diet including adequate
fibre.
o The child should be encouraged to sit on the toilet after mealtimes.
o If fecal retention is so severe that evacuation use enemas or by manual
evacuation under an anesthetic.

10
3-Vomiting:
Onset, duration, frequency.
Amount.
Color (white = milk, yellow = gastric juice, green = bile).
Consistency, Content.
Day/night.
Projectile or not.
Aggravated factors (food - others).
Associated with fever, fit, others.
Other features:
Post-tussive emesis = vomiting after cough occur in pertussis infection and
mycoplasma pneumonia.
Bile-stained vomit intestinal obstruction.
Projectile vomiting, in first few weeks of life pyloric stenosis.
Bacterial diarrhea then vomiting // viral vomiting then diarrhea.
Vomiting after eating by 6 hours + fever at night staph infection.
Vomiting after eating by more than 12 hours E.coli and it's group.
Vomiting after eating by more than 24 hours Salmonella and it's group.
Notes:
Definitions:
o Posseting non-forceful return of small amounts of milk which often accompany
the return of swallowed air (wind).
o Regurgitation non-forceful return of milk (larger, more frequent than posseting).
o Vomiting forceful ejection of gastric contents.
Causes of vomiting:
o Gastroenteritis.
o Feeding problems.
o Ingestion of substance or drug.
o Infection GIT, renal, respiratory, CNS.
o GIT congenital anomalies, gastro-esophageal reflux, appendicitis, peptic ulcer,
intestinal obstruction, coeliac disease.
o Renal failure.
o Raised intracranial pressure.
o Diabetic ketoacidosis.
o Torsion of the testis.
Treatment:
o Rehydration.
o Antiemetic drugs can be used cautiously in children > 2 yr.
o Useful drugs include (Promethazine, Metoclopramide, Ondansetron).
o Treat the underlying cause.

11
4-Fever:
Onset, duration, frequency:
o Continuous fever (typhoid).
o Intermittent fever (malaria).
o Remittent (infective endocarditis).
o Pel-ebstein fever (Hodgkin's lymphoma).
Degree (documented or not).
Time:
o During night like TB which associated with sweating or during day.
Associated with sweating, shivering, rigor.
Reliving factors: spontaneously or by antipyretic agents (paracetamol or ibuprofen).
Other points:
o Ask about febrile convulsion and otitis media.
o Presence of rash.
o Illness of other family members.
o Specific illness is prevalent in the community.
o Recent travel abroad (malaria, typhoid).
o Contact with animals (brucellosis).
o Increased susceptibility from immunodeficiency.
5-Jaundice:
Onset and duration (in first day or not?).
Color of skin, urine, stool.
Feeding problem.
Associated with fever, vomiting, abdominal pain or mass.
Itching (in obstructive jaundice).
Blood group of child and parents.
Recent blood transfusion.
Any medications used.
Recent disease or infection.
Family history of liver disease.
Mother infection during pregnancy or labor.
Causes of jaundice:
Physiological jaundice.
Breastfeeding.
Internal bleeding (hemorrhage).
Blood incompatibility.
Infection.
Liver malfunction or enzyme deficiency.
Abnormality of baby's red blood cells.
Others (hypothyroidism, UTI, blockage or problem in the bile ducts and gallbladder).
12
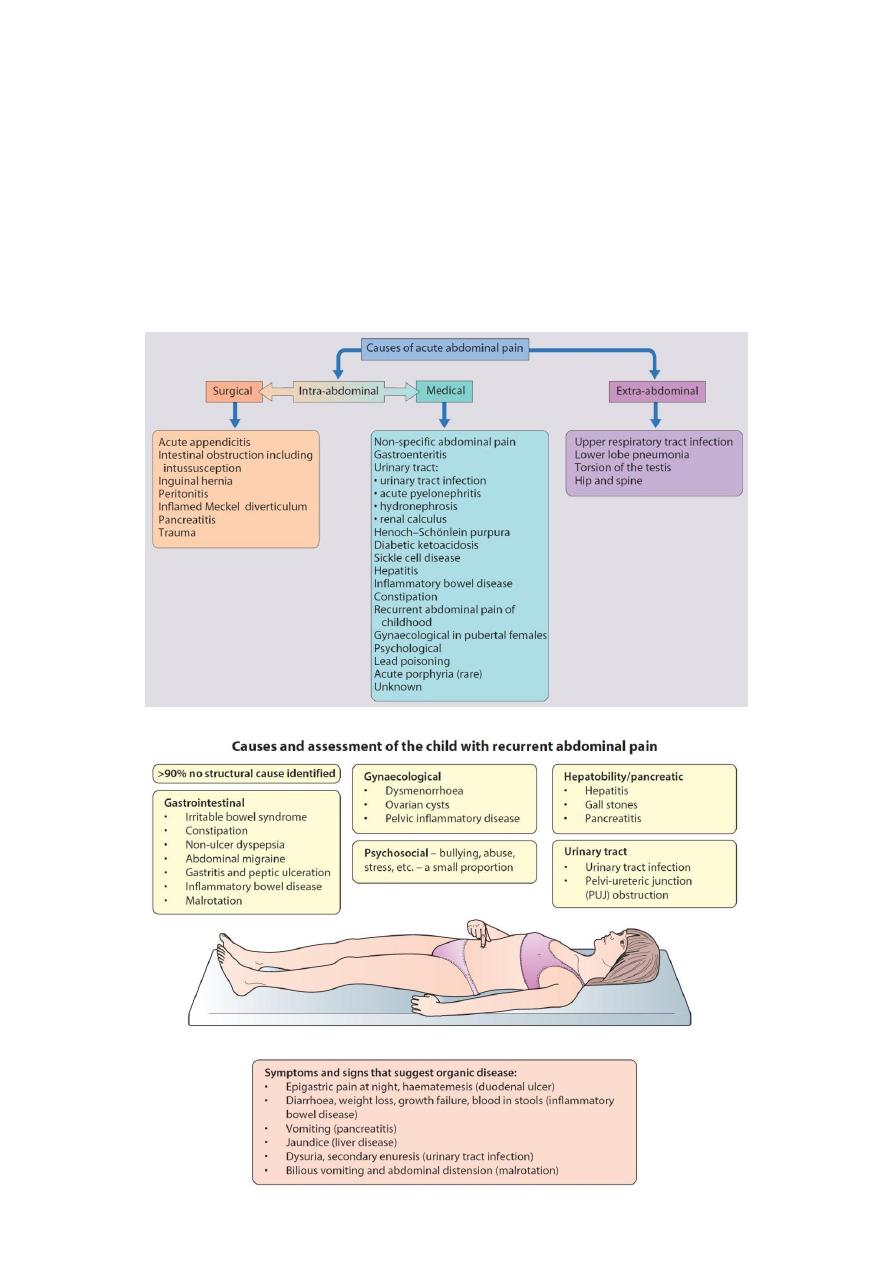
6-Abdominal pain:
Site.
Onset (sudden or gradual, progressive or regressive).
Character (ache, stabbing).
Radiation.
Associations (any other signs or symptoms).
Time course.
Exacerbating/Relieving factors.
Severity.

13
Subject3:
Renal history
1-Amount of urine:
Anuria is absence of any urine output.
Oliguria is decreased urine output.
o Infants: < 0.5 mL/kg per hour for 24 hours.
o Older children: < 500 mL/1.73 m2 body surface area per day.
Polyuria is defined as urine output > 2000ml per 1.73M2 /24 hr or more than 2.5-3
ml/kg/24 hrs.
Common causes of polyuria:
o Polydipsia.
o Solute diuresis e.g. glucosuria in diabetes mellitus.
o Vasopressin or ADH deficiency.
o Chronic renal failure with concentration defect.
o Structural malformations of kidney.
2-Color of urine:
Red:
o Hematuria.
o Myoglobinuria associated with ischemic muscle damage, crush injuries, and after
vigorous exercise.
o Hemoglobinuria with intravascular hemolysis.
o Foods Berries, Beets, Food coloring.
o Drugs Dilantin, Phenothiazines.
Orange:
o Pyridium, Rifampin.
o Urate crystals.
Green:
o Food colorings.
o Increased carotene in the diet.
Brown or Black
o Hemoglobin, Bilirubin.
o Flagyl, Nitrofurans.
o Alkaptonuria (on standing, the urine will turn a dark color).
Yellow:
o Bile pigments.
Blue:
o Methylene blue.
Milky or Cloudy Color:
o Pus cells and bacteria in the urine.
o After sitting, urine may form crystals that makes urine appear cloudy.

14
3-Pain:
Painful micturition:
o Urinary tract infection.
o Candida infection.
o Pinworms.
o Irritative dermatitis.
o Cystitis.
o Urethritis.
o Psychogenic.
Flank pain:
o Pyelonephritis.
o Injury.
Renal colic:
o Stone.
4-Voiding symptoms:
Include poor stream, hesitancy, intermittent flow and straining when passing urine.
Causes Cystitis, Stone in urethra, Injury, Stricture, Adhesion.
5-Storage symptoms:
Include increased frequency and urgency of passing urine, urge incontinence and
needing to get up to pass urine at night (nocturnal enuresis).
Causes of frequency:
o Anxiety.
o Drinking caffeinated beverages or fizzy drinks.
o Emotional upset.
o Having problems with constipation.
o Frequent urinary tract infections.
o Nerve damage or malfunction that causes a child to have difficulty recognizing a full
bladder refraining from completely emptying the bladder when on the toilet.
Organic causes of nocturnal enuresis:
o Urinary tract infection.
o Fecal retention severe enough to reduce bladder volume and cause bladder neck
dysfunction.
o Polyuria from osmotic diuresis (DM) or renal concentrating disorders (chronic renal
failure).

15
Subject4:
Cardiorespiratory history
1-Cough:
Onset (sudden, gradual).
Duration:
o < 2 weeks acute (bronchiolitis, pneumonia, asthma)
o 2 weeks – 2 months acute prolonged cough (pertussis, chronic sinusitis)
o > 2 months chronic (foreign body, GERD, Tracheo-esophageal fistula, cystic
fibrosis, bronchiectasis, mucociliary dyskinesia).
Timing:
o Nocturnal allergy, asthma.
o Midnight sinusitis.
o Early morning Bronchiectasis, COPD, chronic bronchitis, adenoid, smoking.
o Exercise asthma.
o All over the day allergy, foreign body.
Continuous or intractable.
Character:
o Barking Group, LaryngeoTracheoBronchitis.
o Staccato Chlamydia pneumonia and respiratory infections and allergies.
o Wheezing Bronchiolitis, asthma.
o Paroxysmal Whooping cough, bronchiectasis, or a lung injury.
o Paroxysmal post-tussive vomiting Pertussis.
Wet or dry?
o If productive (with sputum) ask about: color, amount, consistency, contains blood
or clot.
o Wet cough lower respiratory tract problem.
o Dry cough upper respiratory tract problem.
Important points:
o Foreign body aspiration: for children 6 months to 6 years.
o Recent infection, allergy, atopic family.
Associated symptoms:
o Runny nose, sore throat, fever nonspecific disease.
o Headache, itchy eyes, sore throat postnasal drip.
o Wheezing and cough with exertion asthma.
o Night sweats TB.
o Spitting up, irritability, or arching of the back after feedings in infants GERD.
o Feeding problem may suggest Tracheo-esophageal fistula.
o Abdominal pain bacterial pneumonia.
o Weight loss or poor weight gain and foul-smelling stools cystic fibrosis.
o Muscle soreness viral illness or atypical pneumonia.

16
Notes:
Cough caused by stimulation of nerve receptors in the pharynx, larynx, trachea or large
bronchi.
Cough center located in medulla oblongata.
For most children, episodes of cough are due to upper respiratory tract infections
caused by the common cold viruses and do not indicate the presence of a long-term or
serious underlying respiratory disease.
Causes of recurrent or persistent cough:
o Recurrent respiratory infections.
o Post-specific respiratory infections (pertussis, RSV, Mycoplasma).
o Asthma.
o Suppurative lung diseases (cystic fibrosis, ciliary dyskinesia or immune deficiency).
o Recurrent aspiration (± gastro-esophageal reflux).
o Persistent endobronchial infection.
o Inhaled foreign body.
o Cigarette smoking (active or passive).
o Tuberculosis.
o Habit cough.
o Airway anomalies (tracheo-bronchomalacia, tracheo-esophageal fistula).
Treatment of cough:
o Management of the underlying disorder.
o Antibiotics for bacterial pneumonia.
o Bronchodilators and anti-inflammatory drugs for asthma.
o Supportive care (oxygen, bronchodilators as needed) for viral infections.
o Little evidence exists to support the use of cough suppressants and mucolytic
agents.
2-Shortness of breath:
Onset.
Duration.
Day/night.
Degree interfere with feeding, activity, sleeping.
Aggravating and relieving factors.
Associated symptoms bluish discoloration, fever, sweating, abdominal pain.
First time or have similar attack previously.
Known case of cardiac or respiratory disease.
Common causes of SOB in children:
Choanal atresia.
Foreign body in upper airway.
Enlarged tonsils.
Asthma.

17
Respiratory tract infection.
Obesity.
Congenital cyanotic heart disease.
3-Noisy breathing:
Onset, duration, frequency.
Continuous or not.
Character of sound.
Day or night.
Related to allergy.
Relation to feeding and sleeping.
Any deformity in nose or respiratory tract.
Site of sound:
Nose snoring "inspiratory", adenoid hypertrophy.
Epiglottis Grunting "expiratory", sign of respiratory distress
Grunting:
o Pulmonary:
Effusion, pneumothorax.
Dramatic response to O2 for 10 minutes.
o Extra-pulmonary:
Cardiac: acute heart failure.
Metabolic acidosis: gastroenteritis, diarrhea, diabetic ketoacidosis, salicylate.
Severe blood loss: anemia.
o Expiratory phase due to respiratory failure.
Larynx Strider "inspiratory", e.g. croup.
Trachea and major bronchus Crepitation (by stethoscope), Rattling (by ear).
"Inspiratory and expiratory" causes:
o Bronchiolitis: viral (RSV), less than 1 year, peak at 6 months.
o Pneumonia: more than 1 year, inflammation of lower respiratory tract.
Minor bronchioles wheezing "mainly expiratory", causes: bronchiolitis, asthma,
heart failure, pulmonary edema.
Watch these videos:
https://www.youtube.com/watch?v=_kGUGgPn6_E
https://www.youtube.com/watch?v=Qbn1Zw5CTbA&list=PLrL1lM0-SHvL2dYx-
Pr7veEshYo92f3uj

18
4-Chest pain:
Quality (sharp, stabbing, aching)
Intensity.
Location (can they point to location with one finger?)
Radiation.
Timing of the pain with relationships to exercise, eating.
Duration, frequency.
Ask about any history of trauma.
What makes it better or worse?
What do they think is causing the pain?
Any recent stressors at home or school or problems with anxiety?
Common causes of chest pain in children:
Cardiac (CAD, valve disease, structural disease).
Musculoskeletal (fractured rib, muscle strain).
Respiratory (asthma, foreign body in airways, chronic cough, pleural effusion).
GIT (esophagitis, GERD).
Non-organic (anxiety, stress).
5-Bluish discoloration:
Duration.
Site (skin, mucus membrane).
Central or peripheral (lips, tip of tongue, peripheries).
Respiratory or cardiac diseases.
Any congenital anomalies.
Associated symptoms (cough, SOB).
Any drug use.
Exposure to cold.
Previous same condition.
Notes:
Respiratory causes: T.B, respiratory distress syndrome, asthma, pneumonia,
pneumothorax, bronchiectasis, lung abscess, cystic fibrosis, asbestosis, familial (10%).
Cardiac disorders: cyanotic congenital heart disease.
Acute cyanosis: pneumonia (respond to O2).
Chronic cyanosis: Tetralogy of Fallot (not respond to O2).
Signs of chronic cyanosis: finger clubbing, polycythemia (due to chronic hypoxia),
gingival hyperplasia.
Acrocyanosis: occur in normal baby.

19
6-Palpitation:
Onset, duration, frequency.
Character (told mother to tap it on the table).
Relation to feeding or activity.
Presence of fever.
Any cardiac problem.
Use of any drug.
Notes:
Relation of other systems to respiratory system:
o GIT chest infection + frequent bowel motion = adenovirus.
o GUS chest infection + UTI = adenovirus.
o CNS chest infection + meningitis = adenovirus / Fit due to hypoxia (anxious or
lethargic).
o Skin respiratory infection + rash = meals or as complication of poliovirus vaccine.
The most important problem that affect the neonate and that 100% ends with asthma
is Broncho-pulmonary dysplasia
In family history ask about allergic conjunctivitis, allergic rhinitis, asthma, atopic
dermatitis (eczema).
Triggers of respiratory symptoms type of heating, animal contact, ventilation, type
of house cleaning.
Feeding could lead to aspiration pneumonia, cow milk protein allergy, Tracheo-
esophageal fistula.

20
Subject5:
CNS history
1-Headache:
Headache onset, duration, and severity.
Site (unilateral or bilateral).
Aggravating and reliving factors.
Associated symptoms (fever, vomiting, visual problems).
Family history of migraines.
Medication history.
History of trauma.
Factors that may have precipitated the headache (most often migraine).
Notes:
Causes of headache:
o Migraine headache.
o Tension headache.
o Cluster headache.
o Sinus headache.
o Head trauma-related headache.
o Intracranial mass-related headache.
o Benign intracranial hypertension.
o Meningeal irritation.
o Medication-overuse headache.
In migraine attack ask about:
o Onset and timing.
o Number of attacks per month.
o Aggravating and reliving factors.
o Medications.
o Eating contraindicated substances.
Treatment of headache:
o Elimination of identified precipitants
o Lifestyle changes
o Stress relief
o Drugs: analgesics, triptans, isometheptene, ergotamines.
2-Abnormal body movements:
Number of movements excessive or diminished?
Age of onset:
o Full term neonate jitteriness.
o Infant myoclonus, athetosis, transient dystonia.
o Older child chorea.

21
Sex:
o Female Sydenham’s chorea, thyrotoxicosis.
o Male tics, tremors.
Onset, duration
o Acute Infection, trauma.
o Slowly progressive.
Change over time.
Type of movement:
o Rapid jerky chorea.
o Slow movement athetosis.
o Sustained dystonia.
Involvement of body parts:
o Distal limb athetosis.
o All body parts chorea.
o Hand focal dystonia.
Presence of movements in sleep:
o Seizure disorder.
o Nocturnal myoclonus.
Associated symptoms (loss of consciousness, cyanosis).
Aggravating factors (environmental stimuli or emotional states).
Reliving factors (drug, special position, suppressed voluntarily).
Differentiate it from: breath holding attack and pseudo-epilepsy.
Family history of a similar or related condition.
3-Convulsion:
Precipitation.
Description.
Duration.
Number of attacks.
Associated with tongue bit and incontinence.
Stoppage.
Post-ictal state.
Presence of fever or infection.
Previous episodes.
Family history.
Head trauma, CNS disease.
Developmental millstone.
4-Loss of consciousness:
Duration, frequency, aggravating factor, body color (pale), abnormal movements,
incontinence, take drugs, CVS disease, CNS disease.
Any fit + loss of consciousness = generalized epilepsy until proven otherwise.
Focal abnormal movement + loss of consciousness = partial epilepsy.

22
5-Other symptoms:
Visual or hearing problems.
Diplopia due to increased intracranial pressure for any cause.
Numbness Unilateral, Bilateral, Symmetrical, Asymmetrical.
Hemiplegia, Monoplegia, Tetraplegia.
See this video:
https://www.youtube.com/watch?v=iyJ5i56HpTc
Ibnlatef
Notes
Pediatric – History taking
