
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
1
Organs Associated with the Digestive Tract
Introduction
The organs associated with the digestive tract include the major salivary glands,
the pancreas, the liver, and the gallbladder. Products of these organs facilitate
transport and digestion of food within the gastrointestinal tract, the main functions of
the salivary glands are to moisten and lubricate ingested food and the oral mucosa, to
initiate the digestion of carbohydrates and lipids with amylase and lipase, and to
secrete innate immune components such as lysozyme and lactoferrin, the pancreas
secretes digestive enzymes that act in the small intestine and hormones important for
the metabolism of the absorbed nutrients. Bile, whose components are necessary for
digestion and absorption of fats, is made in the liver but stored and concentrated in the
gallbladder, the liver also plays a major role in carbohydrate and protein metabolism,
inactivates many toxic substances and drugs, and synthesizes most plasma proteins
and factors necessary for blood coagulation.
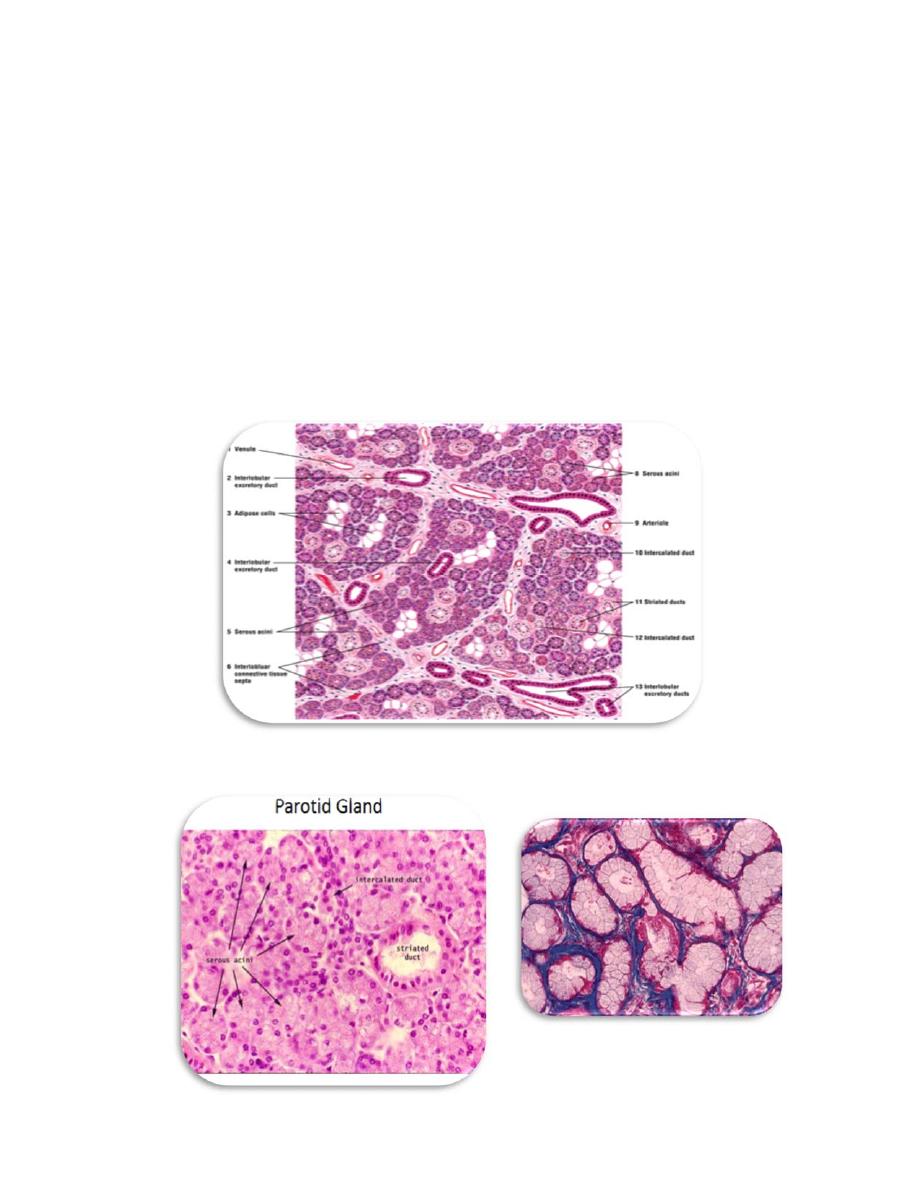
Salivary Glandes
Exocrine glands in the mouth produce saliva, which has digestive, lubricating, and
protective functions, with a normal pH of 6.5 to 6.9, saliva also has an important
buffering function and in some species is also important for evaporative cooling, there
are three pairs of large salivary glands: the parotid , submandibular , and sublingual
glands ,in addition to the numerous minor mucosal salivary glands throughout the oral
cavity, which secrete about 10% of the total saliva volume.
A connective tissue capsule surrounds each major salivary gland, the parenchyma
of each consists of secretory units on a branching duct system arranged in lobules,
separated by septa of connective tissue, the secretion of each gland is either serous,
seromucous, or mucous, depending on its content of the glycoprotein mucin. Saliva
from the parotids is serous and watery, the submandibular and sublingual glands
produce a seromucous secretion, while that of the minor glands is mostly mucous,
saliva is modified by the cells of the duct system draining the secretory units, with
much Na + and Cl – reabsorbed while certain growth factors and digestive enzymes
are added.
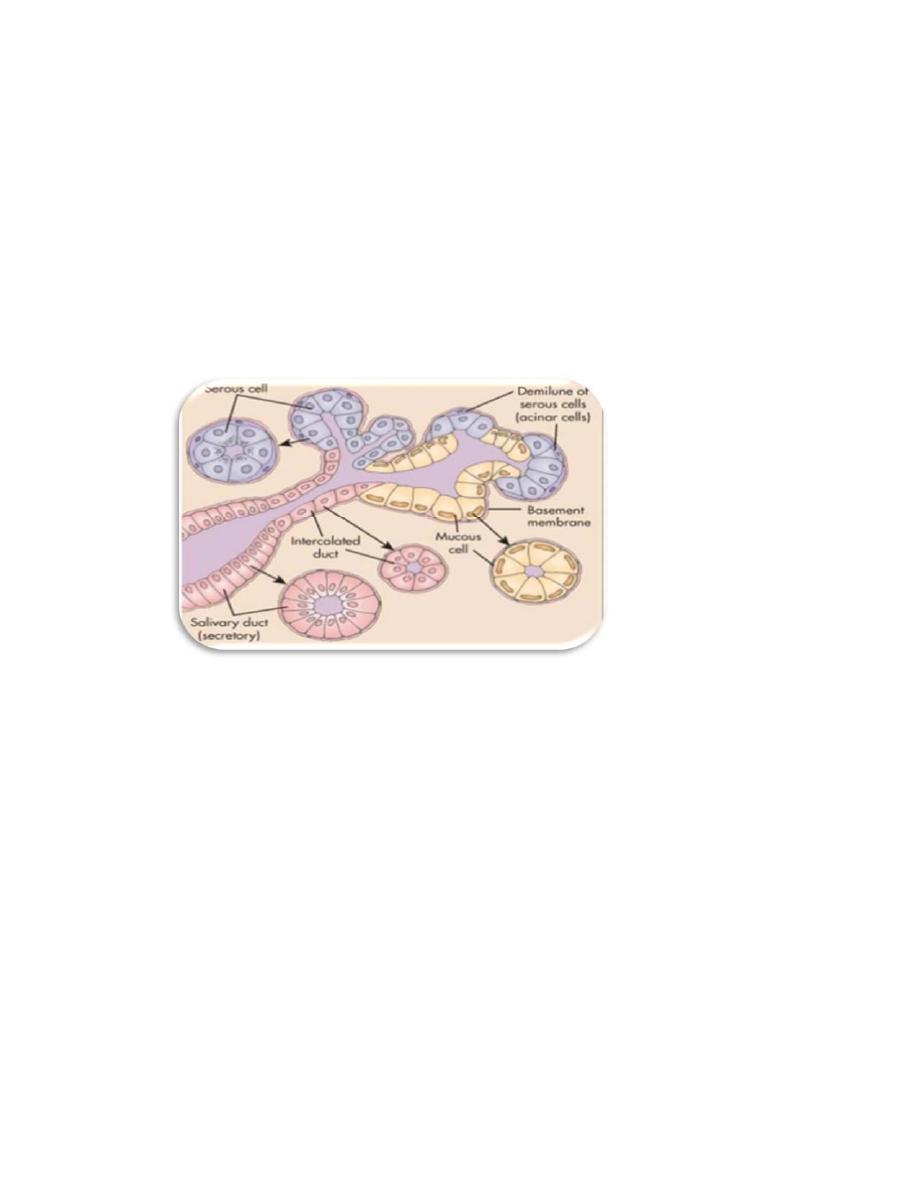
Three epithelial cell types comprise the salivary secretory units:
■ Serous cells are polarized protein-secreting cells, usually pyramidal in shape,
with round nuclei, well-stained RER, and apical secretory granules , joined apically
by tight and adherent junctions, serous cells form a somewhat spherical unit called an
acinus , with a very small central lumen , serous acinar cells secrete enzymes and
other proteins.
■ Mucous cells are somewhat more columnar in shape, with more compressed
basal nuclei , mucous cells contain apical granules with hydrophilic mucins that
provide lubricating properties in saliva but cause poor cell staining in routine
preparations , mucous cells are most oft en organized as cylindrical tubules rather than
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
2
acini. Mixed salivary glands have tubuloacinar secretory units with both serous and
mucous secretion.
■ Myoepithelial cells are found inside the basal lamina surrounding acini, tubules,
and the proximal ends of the duct system ,these small, flattened cells extend several
contractile processes around the associated secretory.
Salivary glands are classified according to their types of acini.
(1) Parotid glands consist of serous acini and are classified as serous.
(2) Sublingual glands consist mostly of mucous acini capped with serous demilunes.
They are classified as mixed.
(3) Submandibular glands consist of both serous and mucous acini (some also have
serous demilunes). They are classified as mixed(Fig,2).
Submandibular glands
Sublingual glands
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
3
Salivary gland ducts
a. Intercalated ducts originate in the acini and join to form striated ducts. They may
deliver bicarbonate ions into the primary secretion.
b. Striated (intralobular) ducts
(1) Striated ducts are lined by ion-transporting cells that remove sodium and
chloride ions from the luminal fluid (via a sodium pump) and actively pump
potassium and bicarbonate ions into it.
(2) Striated ducts converge in each lobule to form interlobular (excretory) ducts,
which run in the connective tissue septa. These ducts drain into the main duct of each
gland, which empties into the oral cavity.
parenchyma of salivary glands
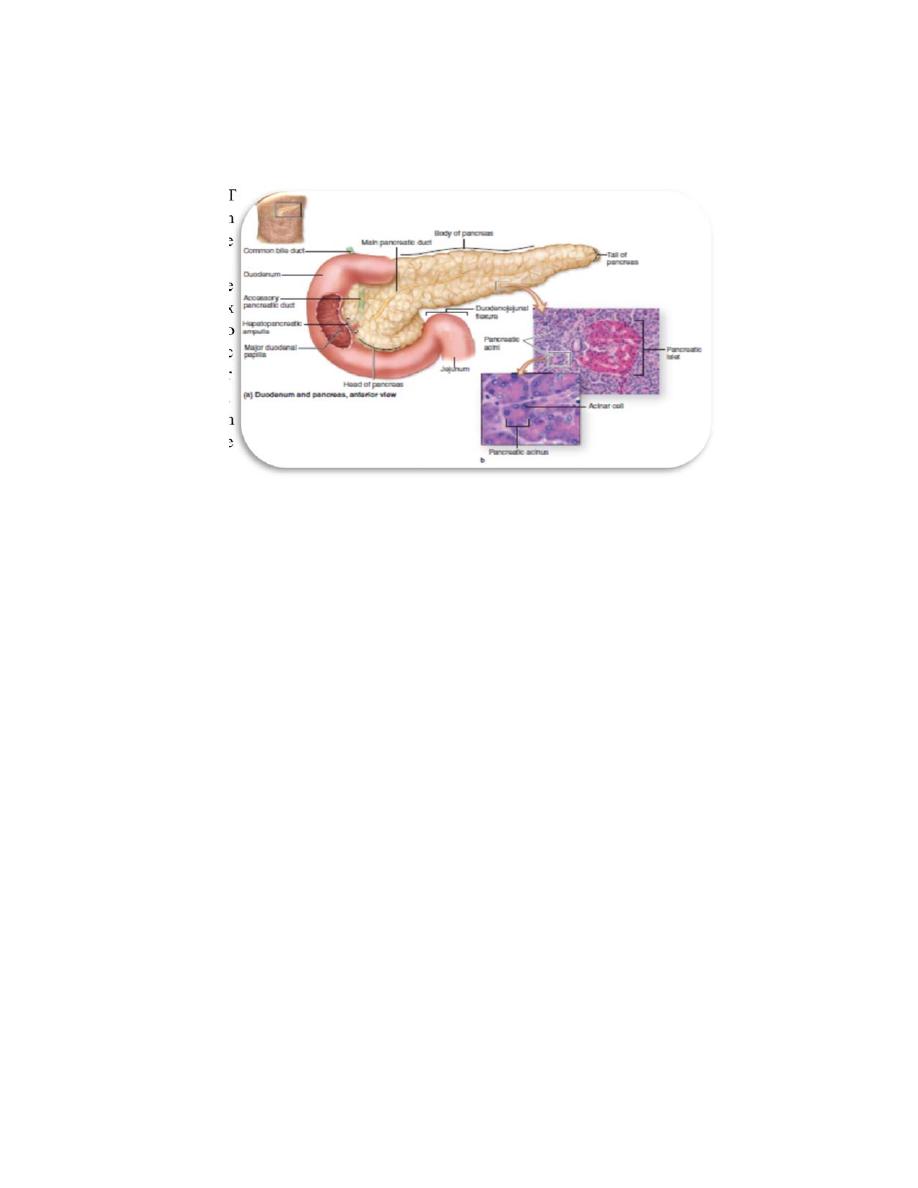
Pancreas
The pancreas has endocrine and exocrine portions,
that produces both digestive
enzymes and hormones. The pancreas has a thin capsule of connective tissue, from
which septa extend to cover the larger vessels and ducts and to separate the
parenchyma into lobules.
The endocrine portion the pancreas involves primarily smaller cells similar to
enteroendocrine cells located in variously sized clusters called the pancreatic
islets (islets of Langerhans). (insulin, glucagon, somatostatin, and
pancreatic polypeptide), which are released into the blood stream.
The
pancreatic islets (islets of Langerhans) are compact spherical or ovoid masses
of endocrine cells embedded within the acinar exocrine tissue of the pancreas,
most islets are 100 to 200 μm in diameter and contain several hundred cells,
the pancreas has more than 1 million islets. Avery thin reticular capsule
surrounds each islet, separating it from the adjacent acinar tissue, the cells of
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
4
islets are polygonal or rounded, smaller, and more lightly stained than the
surrounding acinar cells, arranged in cords separated by fenestrated capillaries.
T
h
e
e
x
o
c
r
i
n
e
p
exocrtion produces pancreatic secretions (juice), which are carried by
pancreatic ducts. Most of these secretions go to the main pancreatic duct,
which joins the hepatopancreatic ampulla (ampulla of Vater) and then
enters the duodenum through the major duodenal papilla (papilla of
Vater), the ampulla is surrounded by smooth muscle called the sphincter of
the ampulla (sphincter of Oddi). A small portion of the pancreatic secretion
is carried by the accessory pancreatic duct and enters them duodenum
through the minor duodenal papilla. The pancreas lacks striated ducts and the
parotid glands lack islets of endocrine tissue, each pancreatic acinus consists
of several serous cells surrounding a very small lumen, without
myoepithelial cells, the acinar cells are polarized, with round basal nuclei,
and numerous zymogen granules apically, typical of protein secreting cells
The pancreatic duct system includes:
1. intralobular ducts.
2. interlobular ducts.
3. a main duct.
The pancreas does not have striated ducts, and the smallest intralobular ducts are
intercalated ducts, the initial portions of the intercalated ducts are lined by
centroacinar cells, `the initial pancreatic secretions (enzymes) are produced by
pancreatic acinar cells, and a large volume of fluid (water, sodium, and bicarbonate)
is added by intercalated duct cells, pancreatic secretions contain enzymes for
digesting proteins, carbohydrates, and fats.

anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
5
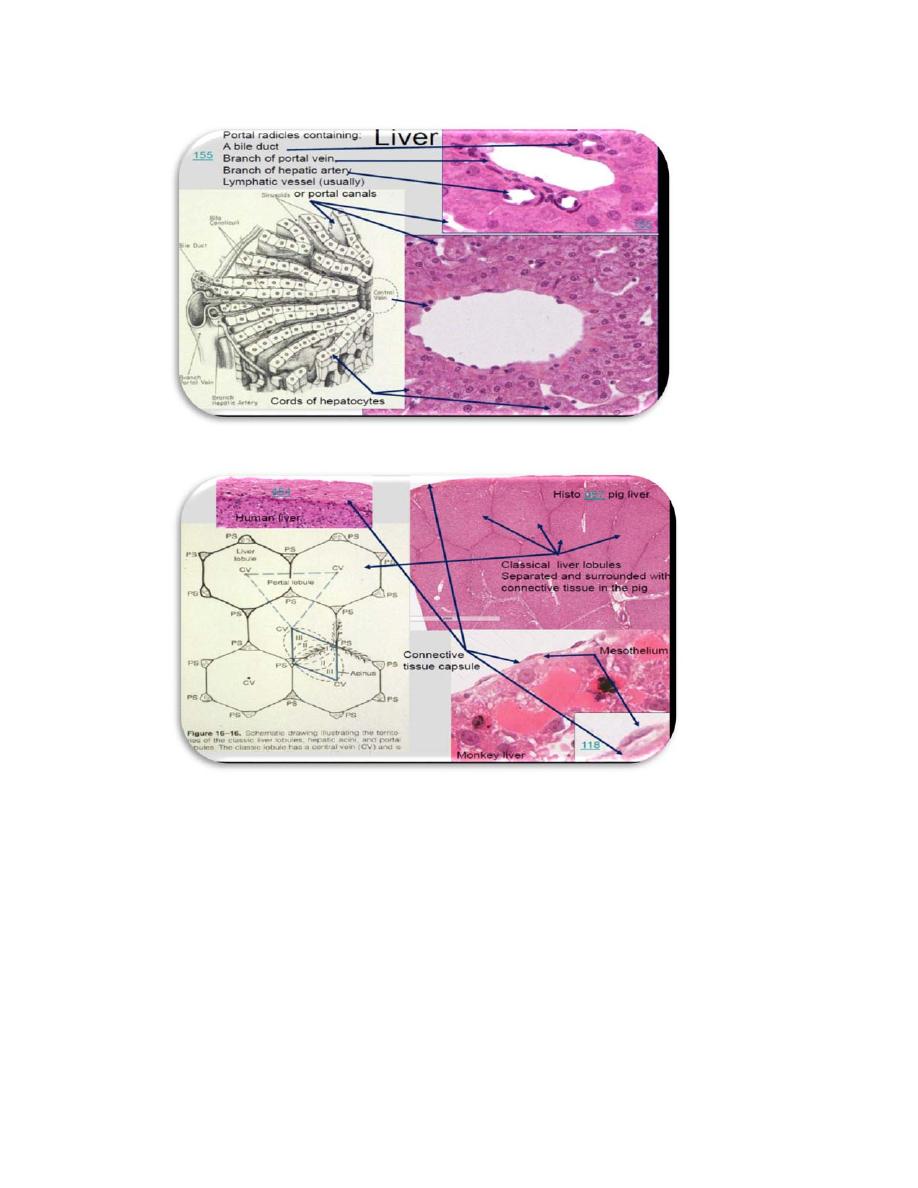
The liver
The liver is composed of a single type of parenchymal cell, the hepatocyte, it is
surrounded by a dense, irregular collagenous connective tissue known as Glisson
capsule, which gives rise to septa that subdivide the liver into lobes and lobules.
Function.
The liver produces bile and plasma proteins and has a myriad of other functions.
Liver lobules
1. The classic liver lobule is a hexagonal mass of tissue primarily composed of plates
of hepatocytes, which radiate from the region of the central vein toward the
periphery.
a. Portal areas (portal canals or portal triads)
(1) The portal areas are regions of the connective tissue between lobules that contain
branches of the portal vein, hepatic artery, lymph vessel, and bile duct.
(2) They are present at alternate corners of a classic liver lobule.
b. Liver sinusoids
(1) Liver sinusoids are sinusoidal capillaries that arise at the periphery of a lobule and
run between adjacent plates of hepatocytes.
(2) They receive blood from the vessels in the portal areas and deliver it to the central
vein.
(3) They are lined by sinusoidal lining cells (endothelial cells) that have large
discontinuities between them, display fenestrations, and lack basal laminae.
(4) They also contain phagocytic cells (Kupffer cells) derived from monocytes; these
cells remove debris, old erythrocytes, and cellular fragments from the bloodstream.
c. Space of Disse
(1) The space of Disse is the subendothelial space between hepatocytes and
sinusoidal lining cells.
(2) It contains the short microvilli of hepatocytes, reticular fibers (which maintain the
architecture of the sinusoids), and occasional non myelinated nerve fibers.
(3) It also contains stellate fat-storing cells (Ito cells, perisinusoidal stellate cells),
which preferentially store vitamin A. However, when the liver is
compromised,hepatocytes release tumor growth factor _ and, in response, these fat-
storing cells can divide, change their phenotype, and begin to synthesize collagen,
leading to fibrosis and, if necessary, differentiate into myofibroblasts to control blood
flow into the sinusoids.
(4) Function. The space of Disse functions in the exchange of material between the
bloodstream and hepatocytes. Hepatocytes do not directly contact the bloodstream.
Blood and bile flow
1. Blood flow into the liver is derived from two sources and is directed from the
portal triads at the periphery of each classic liver lobule toward the central vein.
a. The hepatic artery brings oxygen-rich blood from the abdominal aorta and
supplies 20% to 30% of the liver’s blood.

anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
6
b. The portal vein brings nutrient-rich blood from the alimentary canal and spleen; it
supplies 70% to 80% of the liver’s blood.
2. Blood flow out of the liver occurs via the hepatic vein, formed by the union of
numerous sublobular veins, which collect blood from the central veins.
3. Bile flow is directed toward the periphery of the classic liver lobule (in the
opposite direction of blood flow). Bile is carried in a system of ducts that culminate
in the left and right hepatic ducts, which leave the liver and carry bile to the
gallbladder.
a. Bile canaliculi
(1) The bile canaliculi are expanded intercellular spaces between adjacent hepatocytes
that form tiny canals for the initial flow of bile.
(2) They receive the liver’s exocrine secretion (bile) and carry it to the canals of
Hering (bile ductules) at the very periphery of classic liver lobules.
b. Bile ducts
(1) Bile ducts are located in the portal areas.
(2) They receive bile from the canals of Hering.
(3) They enlarge and fuse to form the hepatic ducts, which leave the liver at the porta
hepatis.
Hepatocytes
1. Hepatocytes are large polyhedral cells (20–30 _m in diameter) that possess
abundant RER and smooth endoplasmic reticulum (SER); numerous mitochondria,
lysosomes, and peroxisomes; several Golgi complexes; and many lipid droplets and
glycogen deposits.
2. They usually contain one round central nucleus; about 25% of the cells are
binucleated. Occasionally, nuclei are polyploid.
3. Hepatocyte surfaces
a. Hepatocyte surfaces facing the space of Disse possess microvilli, which by
increasing
the surface area facilitate the transfer of materials (e.g., endocrine secretions)
between the hepatocytes and the blood.
b. Abutting surfaces of adjacent hepatocytes
(1) frequently delineate bile canaliculi, small, tunnel-like expansions of the
intercellular
space. The bile canaliculi are sealed off from the remaining intercellular
space by occluding junctions located on each side of each canaliculus.
(2) possess microvilli that extend into the bile canaliculus
(3) also have gap junctions
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
7
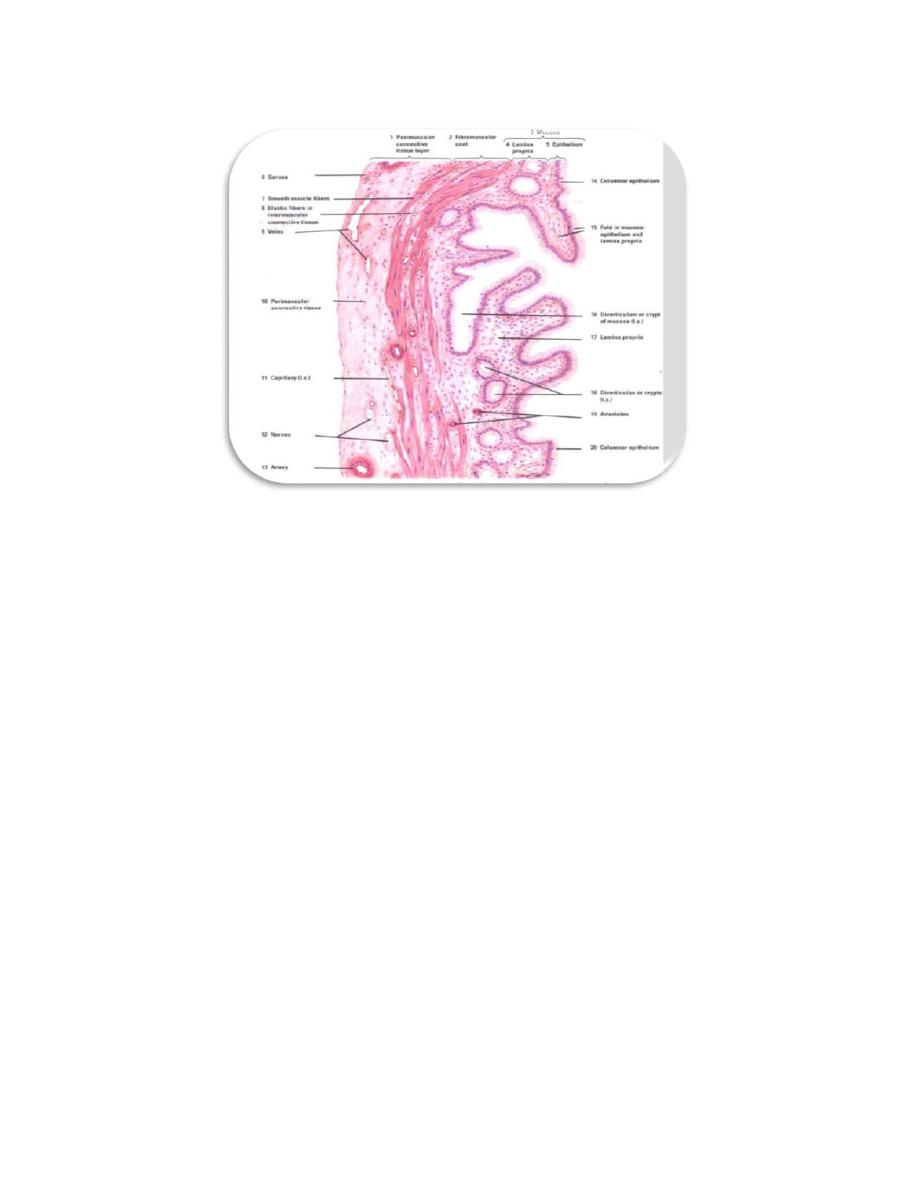
The gallbladder
The gallbladder communicates with the common hepatic duct via the cystic duct,
which originates at the neck of the gallbladder, it has a muscular wall whose
contraction, stimulated by cholecystokinin (possibly in conjunction with
acetylcholine), forces bile from its lumen into the duodenum, the wall has four layers:
1. The mucosa is composed of a simple columnar epithelium and a richly
vascularized lamina propria. When the gallbladder is empty, the mucosa displays
highly convoluted folds.
2. The muscle layer is composed of a thin, oblique layer of smooth muscle cells.
3. The connective tissue layer consists of dense irregular collagenous connective
tissue and houses nerves and blood vessels.
4. The serosa covers most of the gallbladder, but adventitia is present where the organ
is ttached to the liver.
anatomy & histology
. of
Dep
/
College of Medicine
stage
nd
2
. Maryam Mohammed
Dr
Date:5‐7/10/2016
8
