anatomy &
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
histology
Date:5‐7/10/2016
1
Stomach
The stomach is a “J”-shaped sac (hollow) organ, The stomach is a greatly dilated
segment of the digestive tract
whose main functions are:
■ To continue the digestion of carbohydrates initiated by the amylase of saliva,
■ To add an acidic fluid to the ingested food and mixing its contents into a viscous
mass called chyme by the churning activity of the muscularis,
■ To begin digestion of triglycerides by a secreted lipase.
■ To promote the initial digestion of proteins with the enzyme pepsin.
The stomach can be divided into the cardia, fundus, body, and pylorus, The much
larger fundus
and body
regions are identical in microscopic structure and are the sites
of gastric glands releasing acidic gastric juice. The mucosa and submucosa of the
empty stomach have large, longitudinally directed folds called rugae, which flatten
when the stomach fills with food.
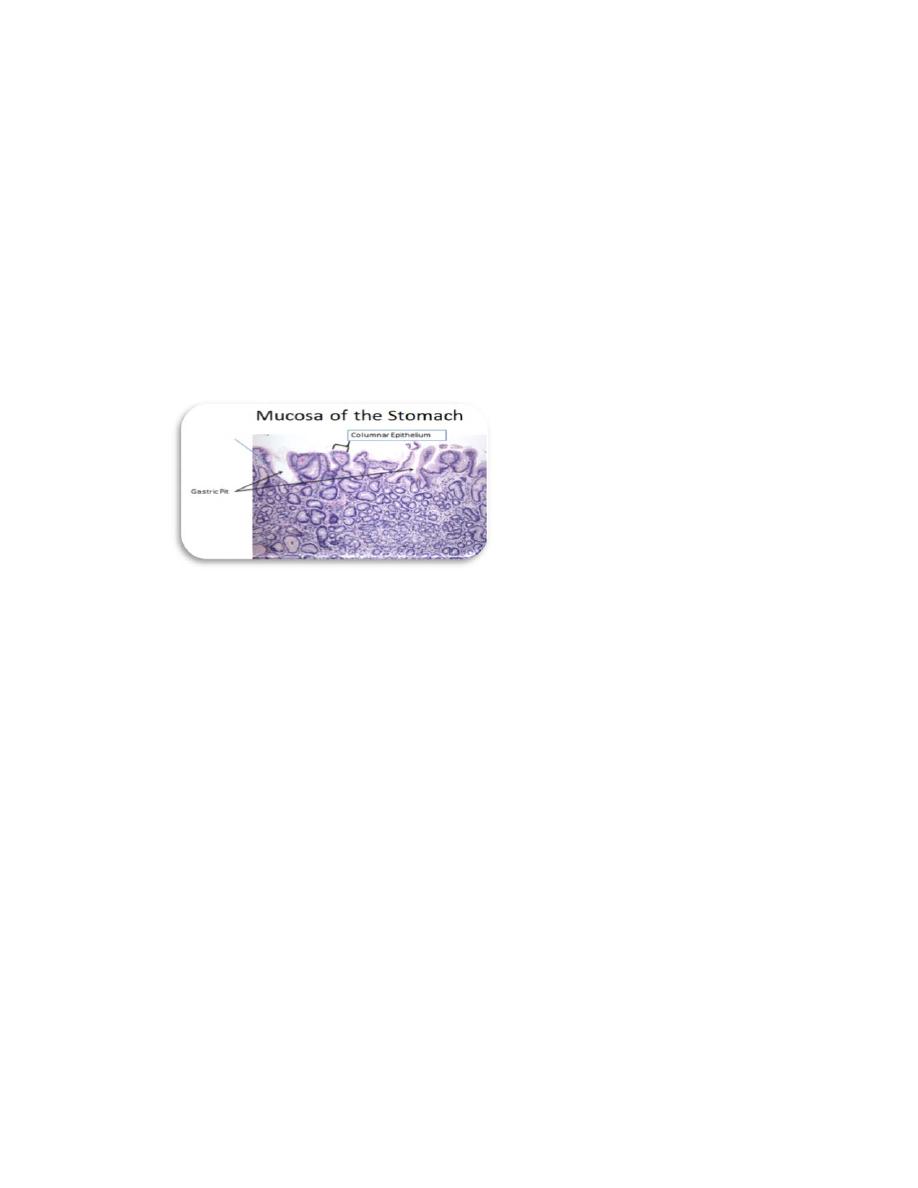
Figure.1:shows the simple columnar epithelium, gastric pit and gastric gland
1. The cardiac region connects to the lower esophagus at the esophagogastric
junction, which is characterized by a change from the nonkeratinized
stratified squamous epithelium of the esophagus to the simple columnar
epithelium of the stomach. A thickened smooth muscle ring called the
gastroesophageal sphincter (lower esophageal sphincter) or cardiac
sphincter surrounds the opening at the junction of the lower esophagus and
cardiac region of the stomach, this smooth muscle contracts to prevent the
acidic stomach contents from entering the esophagus. The glands in the
lamina propria of the cardia are called cardiac glands and are branched
tubular glands with coiled secretory portions. The cardiac gland contains
mainly mucus-secreting cellsThe cardiac gland contains mainly mucus-
secreting cells and some stem cells, enteroendocrine cells, and, occasionally,
parietal cells. The mucus-secreting cells mainly produce mucus and
lysozymes. The mucus protects the stomach wall from acidic gastric juices;
lysozymes destroy bacterial membranes, preventing bacterial infections .
anatomy &
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
histology
Date:5‐7/10/2016
2
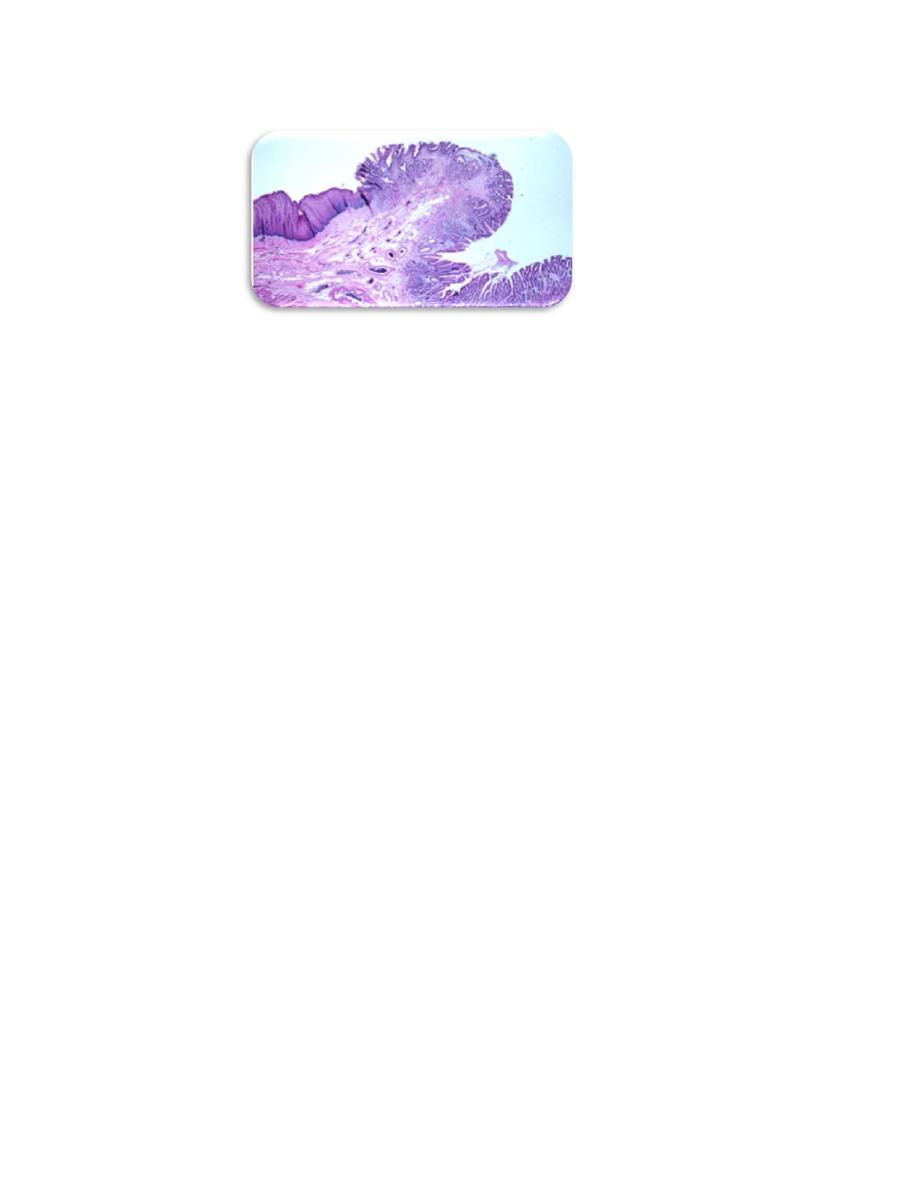
(Figure, 2):Shows esophagogastric junction.
2. The fundic and body regions
Changing abruptly at the esophagogastric junction , the mucosal surface of
the stomach is a simple columnar epithelium that invaginates deeply into the
lamina propria. The invaginations form millions of gastric pits, each with an
opening to the stomach lumen . The surface mucous cells that line the lumen
and gastric pits secrete a thick, adherent, and highly viscous mucous layer that
is rich in bicarbonate ions and protects the mucosa from both abrasive effects
of intraluminal food and the corrosive effects of stomach acid.
a. Parietal cells (oxyntic) cells are more numerous in the superior regions
of the glands; these cells produce large quantities of hydrochloric acid
(HCl), creating an acidic environment to help digestion. Parietal cells also
secrete intrinsic factor (IF), which is required for the absorption of
vitamin B12. Parietal cell secretory activity is stimulated both by
parasympathetic innervation and by paracrine release of histamine
and the polypeptide gastrin from enteroendocrine cells.They are large
cells, usually appearing rounded or pyramidal, each with one (sometimes
two) central round nucleus. The cytoplasm is intensely eosinophilic due to
the high density of mitochondria. A striking ultrastructural feature of an
active parietal cell is a deep, circular invagination of the apical plasma
membrane to form an intracellular canaliculus with a large surface area
produced by thousands of microvilli . carbonic anhydrase catalyzes the
conversion of cytoplasmic water and CO2 into HCO3+ and H+. The
HCO3 + is transported from the basal side of the cell and H+ is pumped
from the cell apically, along with Cl−. In the lumen the H+ and Cl− ions
combine to form HCl. While the gastric secretion becomes highly acidic,
the mucosa itself remains at a more neutral pH partly because of the
bicarbonate released into the lamina propria. The abundant mitochondria
provide energy primarily for operating the cells’ ion pumps.
b. Chief cells (zymogenic) cells are located in the more inferior regions of
the glands; predominate in the lower regions of the gastric glands and
have all the characteristics of active protein-secreting cells.
Ultrastructurally chief cells have abundant RER and numerous apical
secretory granules , The granules contain inactive enzyme pepsinogens,
which is activated by HCl and becomes pepsin. Pepsin helps to break
down proteins (particularly protein collagen) into simpler, more
anatomy &
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
histology
Date:5‐7/10/2016
3
absorbable compounds. Chief cells also secrete precursors of lipases,
which help in lipid digestion
c. Diffuse neuroendocrine system (DNES) cells are also referred to as
enteroendocrine cells or as APUD cells (amine precursor uptake and
decarboxylation cells). cells are scattered epithelial cells in the gastric
mucosa with endocrine or paracrine functions. In the fundus small
enteroendocrine cells secreting serotonin (5-hydroxytryptamine) are found
at the basal lamina of the gastric glands. In the pylorus other
enteroendocrine cells are located in contact with the glandular lumens,
including G cells producing the peptide gastrin.
Upon stimulation, these
cells release their hormone products that then exert paracrine (local) or
endocrine (systemic) effects via the vasculature. Cells of the digestive
tract DNES fall into two classes: a “closed” type, in which the cellular
apex is covered by neighboring epithelial cells , and an “open” type, in
which the constricted apical end of the cell contacts the lumen and bears
chemoreceptors that sample the lumen’s contents. Effects of the hormones
include regulation of peristalsis and tract motility; secretion of digestive
enzymes, water, and electrolytes; and the sense of being satiated after
eating.
d. Mucous neck cells are located in the neck of the gland (and may be able
to divide). possess short microvilli, apical mucous granules, a prominent
Golgi complex, numerous mitochondria, and some basal RER.
Less
columnar than the surface mucous cells lining the gastric pits, mucous
neck cells are often distorted by neighboring cells, but they have round
nuclei and apical secretory granules. Their mucus secretion is less alkaline
than that of the surface
a. Regenerative cells (stem cells) are located primarily in the neck and
isthmus; they replace all the epithelial cells of the gland, gastric pit, and
luminal surface.
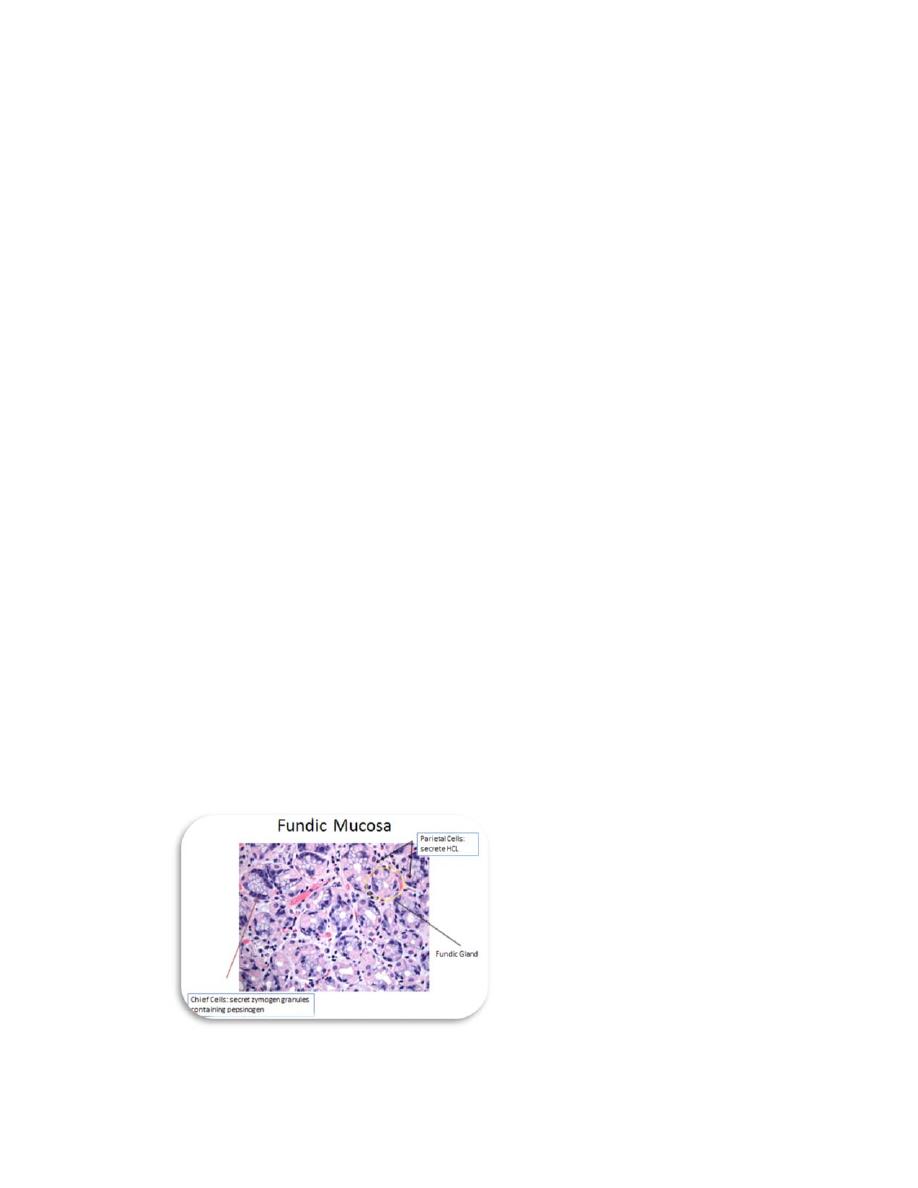
(Figure.3):Shows all types cells of fundic region of stomach

anatomy &
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
histology
Date:5‐7/10/2016
4
1. The pyloric region is the lower end of the stomach, which connects with
the duodenum, its mucosa is similar to that of the cardia, with long gastric
pits and short, coiled secretory portions, acircular smooth muscle ring
called the pylorus sphincter (pyloric valve) surrounds the end of the
pylorus region, this valve controls the entry of stomach contents into the
duodenum, the glands in the lamina propria of the pylorus are called pyloric
glands.
Small Intestine
The small intestine is a hollow organ of small diameter that is typically 6 to 7 m
long. It is the major site for the absorption of nutrients. Important features of the small
intestine are villi and microvilli, which increase surface area for absorption.
macroscopically, the lining of the small intestine shows a series of permanent circular
or semilunar folds (plicae circulares), consisting of mucosa and submucosa , which
are best developed in the jejunum. Densely covering the entire mucosa of the small
intestine are short (0.5- to 1.5-mm) mucosal outgrowths called villi that project into
the lumen . These finger- or leaf like projections are covered by a simple columnar
epithelium of absorptive cells called enterocytes, with many interspersed goblet cells.
Each villus has a core of loose connective tissue that extends from the lamina
propria and contains fibroblasts, smooth muscle fibers, lymphocytes and plasma cells,
fenestrated capillaries, and a central lymphatic called a lacteal. Intestinal glands called
glands (crypts) of Lieberkühn are located in the lamina propria of the small
intestine. Villi project into the lumen of the intestine; the glands of Lieberkuhn open
into the mucosa at the base of the villi.
The epithelium of the intestinal glands includes differentiating cells and pluripotent
stem cells for all the cell types of the small intestine. These include the following:
a. Enterocytes, the absorptive cells, are tall columnar cells, each with an
oval nucleus located basally. The apical end of each enterocyte displays a
prominent ordered region called the striated (or brush) border.
Ultrastructurally the striated border is seen to be a layer of densely packed
microvilli covered by glycocalyx through which nutrients are taken into the
cells, each microvillus is a cylindrical protrusion of the apical cytoplasm
approximately 1 μm tall and 0.1 μm in diameter containing actin filaments
and enclosed by the cell membrane. Each enterocyte has an average of 3000
microvilli and each 1 mm2 of mucosal surface contains about 200 million
of these structures. Microvilli, villi, and the plicae circulares all greatly
increase the mucosal surface area in contact with nutrients in the lumen,
which is an important feature in an organ specialized for nutrient
absorption.
b. Goblet cells are interspersed among the absorptive enterocytes.They secrete
glycoprotein mucins that are then hydrated to form mucus, whose main
function is to protect and lubricate the lining of the intestine.

anatomy &
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
histology
Date:5‐7/10/2016
5
c. Paneth cells, located in the basal portion of the intestinal crypts below the
stem cells, are exocrine cells with large, eosinophilic secretory granules in
their apical cytoplasm. Paneth cell granules release lysozyme,
phospholipase A2, and hydrophobic peptides called defensins, all of which
bind and break down membranes of microorganisms and bacterial cell
walls. Paneth cells have an important role in innate immunity and in
regulating the microenvironment of the intestinal crypts.
d. Enteroendocrine cells are present in varying numbers throughout the length
of the small intestine, secreting various peptide hormones. Many of these
are of the “open” type, in which the constricted apical end of the cell
contacts the intestinal lumen and has chemoreceptors similar to those of
taste buds, sampling levels of certain nutrients such as sugars to regulate
hormone release basally .
e. M (microfold) cells are specialized epithelial cells in the mucosa of the
ileum overlying the lymphoid follicles of Peyer patches , these cells are
characterized by the presence of basal membrane invaginations or pockets
containing many intraepithelial lymphocytes and antigen-presenting cells .
M cells selectively endocytose antigens and transport them to the
underlying lymphocytes and dendritic cells, which then migrate to lymph
nodes for an appropriate immune response.
The small intestine can be divided into three parts: the duodenum, jejunum, and
ileum.
1. The duodenum is the shortest segment of the small intestine, about 20 to 25
cm long. It has small openings called duodenal papillae , which allow
pancreatic juice and bile to enter the digestive tract. It has a similar general
structure to other parts of the small intestine . However, the Brunner glands
(mucus secreting gland) in the submucosa are a unique feature of the
duodenum.
2. The jejunum is much longer than the duodenum, about 2.5 m long (two fifths
of the rest of the small intestine). It has long villi and a somewhat increased
number of goblet cells. It has neither Brunner glands nor Peyer patches.
3. The ileum is the longest segment, about 4 m long (three fifths of the rest of
the small intestine). It has short villi with signify cantly increased numbers of
goblet cells on the surface of the mucosa. There are clusters of lymphatic
nodules in the lamina propria of the ileum; sometimes these lymphatic nodules
extend into the submucosal layer. These clusters of lymphatic nodules are
called Peyer patches and are unique to the ileum.
anatomy &
. of
Dep
/
College of Medicine
stage
nd
2
Dr.Hameda abdulmahdi
histology
Date:5‐7/10/2016
6
Large Intestine
The large intestine or bowel, which absorbs water and electrolytes and forms
indigestible material into feces, has the following regions: the short cecum, with the
ileocecal valve and the appendix; the ascending, transverse, descending, and sigmoid
colon; and the rectum, where feces is stored prior to evacuation .The mucosa lacks
villi and except in the rectum has no major folds. Less than one-third as long as the
small intestine, the large intestine has a greater diameter (6-7 cm). The wall of the
colon is puckered into a series of large sacs called haustra (L. sing. haustrum, bucket,
scoop).
The mucosa of the large bowel is penetrated throughout its length by tubular
intestinal glands. These and the intestinal lumen are lined by goblet and absorptive
cells, with a small number of enteroendocrine cells .
The columnar absorptive cells or colonocytes have irregular microvilli and dilated
intercellular spaces indicating active fluid absorption .
Goblet cells producing lubricating mucus become more numerous along the length
of the colon and in the rectum.
Epithelial stem cells are located in the bottom third of each gland.
The lamina propria is rich in lymphoid cells and in lymphoid nodules that frequently
extend into the submucosa . The richness in MALT is related to the large bacterial
population of the large intestine. The appendix has little or no absorptive function but
is a significant component of MALT .
The muscularis of the colon has longitudinal and circular layers but differs from
that of the small intestine, with fibers of the outer layer gathered in three separate
longitudinal bands called teniae coli . Intraperitoneal portions of the colon are covered
by serosa, which is characterized by small, pendulous protuberances of adipose.
The distal end of the GI tract is the anal canal, 3-4 cm long. At the rectoanal
junction the simple columnar mucosal lining of the rectum is replaced by stratified
squamous epithelium . The mucosa and submucosa of the anal canal form several
longitudinal folds, the anal columns , in which the lamina propria and submucosa
include sinuses of the rectal venous plexus. Near the anus the circular layer of the
rectum’s muscularis forms the internal anal sphincter. Defecation involves the action
of voluntary muscle comprising the external anal sphincter .
