1
Fifth stage
Gynaecology
Lec ? /part3
د.اسماء
26/12/2016
Reproductive tract infections
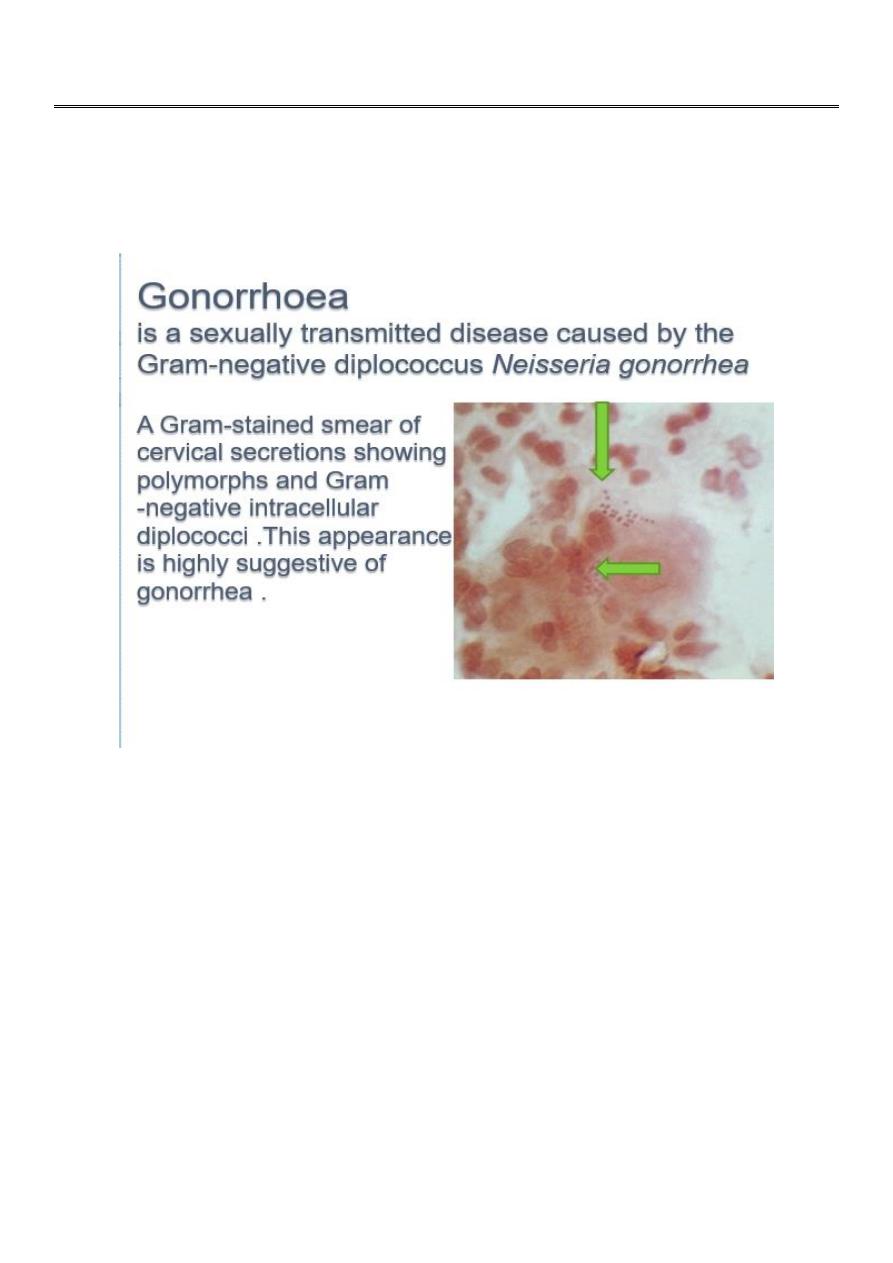
Gonorrhoea
It has affinity to infect the mucous membranes of the genital tract infecting cuboidal and
columnar epithelium seen in the endocervical and urethral mucosa.
It can also infect the rectal and oropharyngeal mucous membrane during anal and oral
intercourse(10% of cases).
It can survive in the host as asymptomatic carrier state .
There is no vaccine available , and no immunity is conferred even though antibodies are
produced.
Most of women and 5% of infected men have no symptoms.
There has been a gradual decline in the incidence of gonorrhoea
and this could be the result of earlier detection and treatment.
However, many women and their partners are asymptomatic
carriers.
2
Sexually transmitted coinfection with Chlamydia and Trichomonas are common and can
provoke more pronounced infection. These may lead to ascending infection causing
endometritis, endosalpingitis and pelvic inflammatory disease .about 15% of untreated
gonococcal cervical infection progress to PID.
Is symptoms are present they are the same as chlamydia and include:
mucopurulant cervicitis ,which include a swollen red and friable cervix ,with
contact bleeding
Acute urethritis ,producing dysuria with minimal frequency and urgency and
usually a negative culture.
Proctitis with rectal bleeding, discharge and pain.
Pelvic tenderness with cervical excitation.
Diagnostic tests :
Gram staining: visualization of Gram-negative intracellular diplococci in the
leukocytes is very sensitive in men (50% sensitivity in female)
Culture medium using an agar medium thayer martin or transgrow media culture
is inexpensive but takes longer with a sensitivity of 90% and a specifity of about
97%.
Nucleic acid amplification tests (NAATs)
Nucleic acid hybridization tests.
Note : Endocervical swabs should be taken and if symptomatic , swabs from the rectum
and pharynx should also be included. The NAATs can test samples taken from the urine
and low vagina.
Note : Because most women with gonococcal cervical infection are asymptomatic
selective screening of high risk patients is essential In attempting to control the
progression and spread of the disease.
Treatment
It is important to: screen both partners and refer them to a genitourinary medicine (GUM)
clinic. Contact tracing should be encouraged if there is exposure to multiple partners.
They should be counselled regarding the long-term implications of the Infections leading to
chronic pelvic pain, tubal infection and subfertility.
Antibiotic treatment
Cephalosporins are the mainstay of treatment. There is emerging evidence of resistance of
the organism to penicillin, ciprofloxacin and tetracycline, most likely due to mutations in
the organisms. It is not necessary to repeat the swabs if there is certainty that the
recommended medication has been taken.
3
However,
if there is any doubt of compliance,
if the symptoms persist
there is a suspicion of resistance,
then the swabs should be repeated Within the week following treatment to check for
complete cure.
The commonly prescribed antibiotics are:
Single oral dose of cefixime 400 mg
Single intramuscular dose of ceftriaxone 250 mg
Single intramuscular dose of spectinomycin 2 g
Single oral dose of ciprofloxacin 500 mg or ofloxacin 400 mg
Ampicillin 2 g or amoxycillin 1 g with probenecid 2 gm as a single oral dose.
In pregnancy, it is safe to use the penicillins and cephalosporins, but tetracycline and
ciprofloxacin /ofloxacin should be avoided.
Chlamydial infection
Chlamydia has the highest incidence of any bacterial infection in STI in the united states.
3 million new cases every year.
75% of cases are found in women younger than 25 years, and half of cases are in
adolescent.
About 5–10 per cent of women below the age of 24 years are thought to carry the
infection and there is ongoing re infection and transmission due the asymptomatic
nature of the disease.
Chlamydia is an obligate intracellular bacterium affecting the columnar epithelium of the
genital tract. It causes one of the most common sexually transmitted infections. In the
majority of cases, it can persist for long period in asymptomatic carrier state with slow and
insidious Infection leading to detrimental effects on the female genital tract..
There is no vaccine there is no immunity though chlamydia antibodies are produced but
are not protecting against reinfection.
Because 70% of infected females 50% of infected males have No Symptoms , it is very
difficult to diagnose and treat this hidden infection.
The UK Government has launched a national Chlamydial screening program as a result of
the increasing incidence of the infection.
4
There are several serovars of chlamydia:
A–C infect the conjunctiva causing trachoma .
D–K infect the genitourinary system.
Other chlamydia species, such as psittaci and pneumonia, infect the lungs causing
pneumonia.
There is a lymphogranuloma venereum strain (L1–L3) which can cause rectal
infection and proctitis.
Infection occurs due to elementary bodies which enter the cells through specific receptors.
Once inside, they form inclusion bodies which divide rapidly by binary fission. These then
reform into elementary bodies and get released from The cell ; This destroys the cell and
the damage that occurs is due to the Inflammatory response to the infection.
Clinical manifestation of genital tract chlamydial infection
Asymptomatic.
Vaginal discharge mucopurulant vaginal discharge yellow discharge coming .
lower abdominal pain.
Postcoital bleeding .
Intermenstrual bleeding.
Mucopurulent cervical discharge with swollen, red friable cervix with contact bleeding.
acute urethritis with Dysuria with but minimal frequency and urgency and a negative
urine culture and there is a urethral discharge.
Complications
Pelvic inflammatory disease
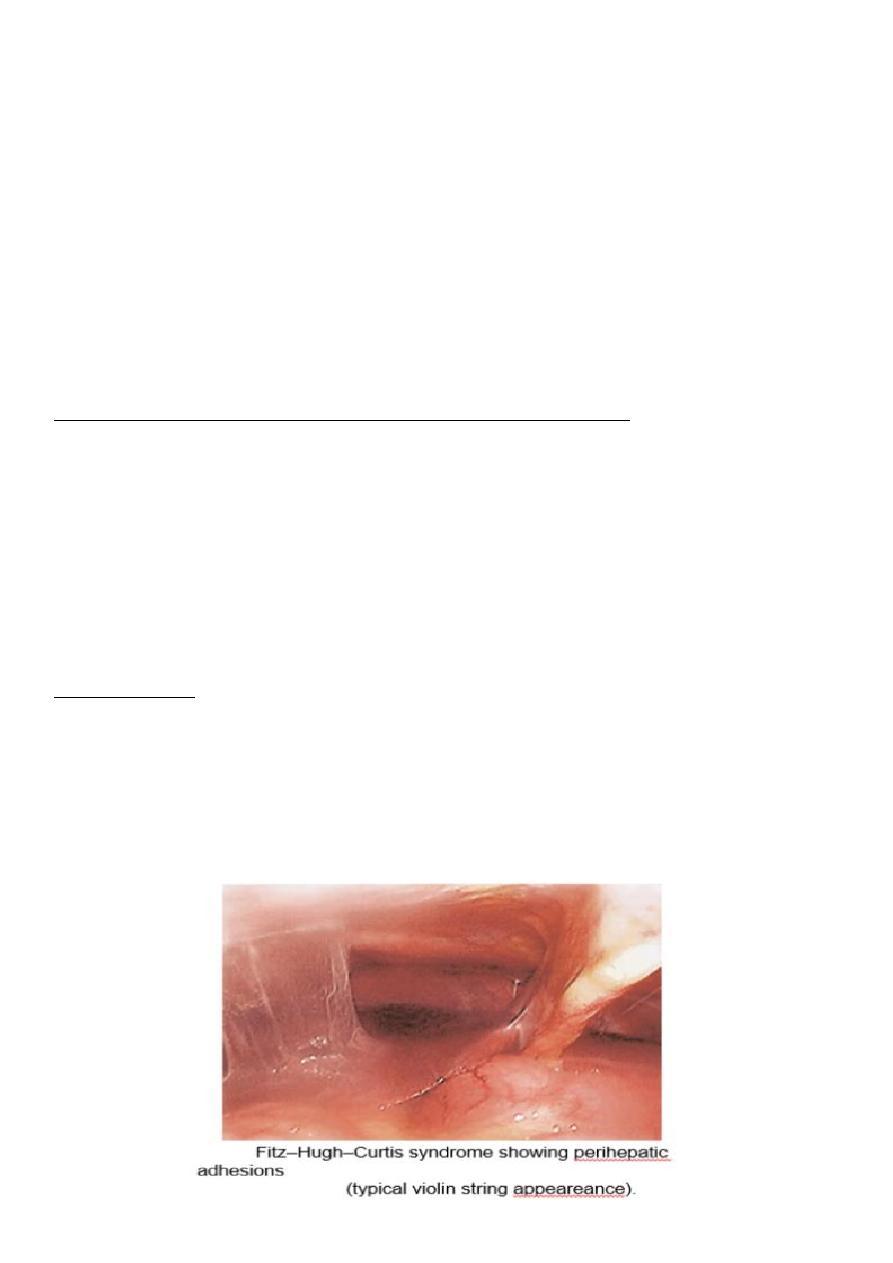
Perihepatitis: Fitz–Hugh–Curtis syndrome
Neonatal conjunctivitis and pneumonia
Adult conjunctivitis
Reiter’s syndrome: reactive arthritis .
5
Diagnostic test
Nucleic acid amplification technique : >90 percent sensitive, should replace the old
enzyme immunoassays (recommended by the Department of Health), should be used in
all medicolegal cases and testing twice should improve the specificity of the test.
Real-time polymerase chain reaction.
Culture is expensive with limited availability. It has a 100 per cent specificity, however, is
only around 60 per cent sensitive, hence not routinely recommended.
Screening and opportunistic testing :
o Partners of patients diagnosed or suspected with infection.
o History of chlamydia in the last year.
o Patients attending GUM clinics .
o Patients with two or more partners within 12 months.
o Women undergoing termination of pregnancy.
o History of other sexually transmitted infection and HIV.
Treatment
General advice
Avoid intercourse, including oral and rectal , before treatment of both partners is
complete.
Use of condoms should be encouraged to prevent reinfection and other STIs.
Retesting if any doubt about complete treatment.
Test of cure should be performed a minimum of 5 weeks after initiation of treatment.
Test of cure should be routine in pregnancy.
Contact tracing of all partners when possible.
A follow-up interview which could also include a telephonic consultation within 2–4
weeks.
If change of partner, retesting between three to 12 months is recommended.
Antibiotic treatment
Doxycycline 100 mg orally twice a day × 7days.
Azithromycin 1 g orally in a single dose , recommended treatment in
pregnancy.
Erythromycin 500 mg orally four times a day × 7 days.
Amoxicillin 500 mg three times a day × 7 days.
Ofloxacin 200 mg orally twice a day or 400 mg once a day × 7 days.
