Oral Cancer
جراحة \ خامس اسناند. وفاء (م8)
27 \ 12 \ 2016
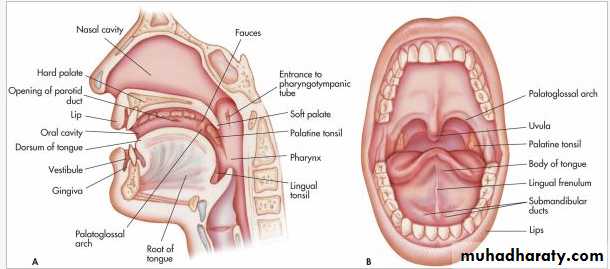
Anatomy
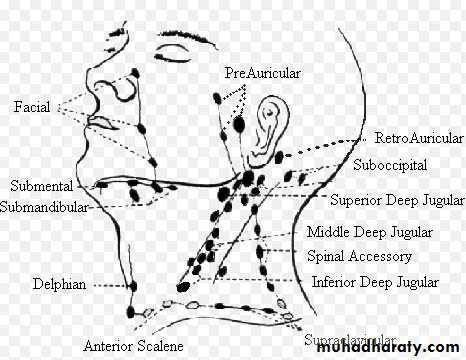
Lymphatic drainage of Head and Neck
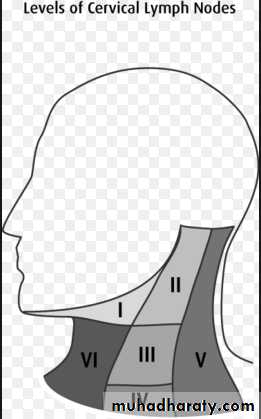
levels of cervical lymph nodes
• Tumor:
• Is a mass of cells, tissues or organs resembling those normally present but arranged atypically and behave abnormally.• Behavior is very essential and is of great importance.
Oral cancer
Oral cancer
• Classification:• Histogenetic:
• Epithelial origin
• connective tissue origin
• Histological:
• Degree of differentiation.
• Well
• moderate
• poorly differentiated
• Clinical behavior:
• Benign:• slowly growing and expanding causing pressure atrophy but remain within the capsule.
• Very few mitosis could be seen.
• Malignant:
• Invade surrounding tissues and locally invasive.
• Progressive growth and metastasize to distant organs, embolic spread due to lack of cell adhesion
• Mitosis.
• Intermediate:
• Locally invasive, no metastasis. Basal cell carcinoma and Ameloblastoma
Pathways of cancer spread (Metastasis)
Invasion into local stroma
Lymphatic spread
Vascular system (Hematogenous spread)
Neural spread
Circulation of the tumor and arrest at the distant site
Epidemiology
Oral cavity and oropharyngeal tumours comprise 40% of cancersGreater in men than women
It is most common in the 6th and 7th decades, although there is evidence that it is increasing in young adults
Aetiology
smoking and consumption of alcoholdiet containing high proportions of vegetables and fruit might modulate carcinogenic effect
Human papilloma virus (HPV) considers as a risk factor in oropharyngeal squamous cell carcinoma
Betel quid chewing is related to the high incidence of oral cancer in India
Roles of the dentist with patients in oral cancer
Recognition of Cancer and Medical ConsiderationsTreatment Planning Modifications
Dental treatment planning for the patient with cancer begins with establishment of the diagnosis. Planning involves the following:
1- Pre-treatment evaluation and preparation of the patient
2- Oral health care during cancer therapy, which includes hospital and outpatient care3- Post-treatment management of the patient, including long-term considerations
Reference: Dental Management. CHAPTER 26 - Cancer and Oral Care of the PatientPremalignant conditions
Conditions of definite premalignant potentialLeukoplakia
Erythroplakia
Chronic hyperplastic candidiasis
Conditions associated with an increased risk of malignant transformation
Lichen planusOral submucous fibrosis
syphilitic glossitis
Diagnosis of oral cancer
Clinical findingRadiograph
Biopsy
Blood investigations
Malignant Tumors
• CLINICAL DIAGNOSIS OF ORAL CANCER• Symptoms vary according to the site of the lesion
• painless in the early stages
• painful and tender when secondarily infected or involves a sensory nerve
• painless lump or ulcer on the lip
• Posteriorly no symptom until it reach a size of 2‑3 cm swelling,
• pain and difficulty in deglutition
• absence of symptoms until the tumor metastasize to regional lymph nodes
• hard lump on the neck
Malignant Tumors
• late symptoms:• pain due to secondary infection or nerve involvement
• excessive salivation
• difficulty in deglutition, speech
• haemorrhage
• Within bone:
• painless swelling involving the buccal and lingual or palatal sulci
• teeth become loose and painful ‑acute alveolar abscess
• edentulous pt. the denture does not fit
• denture hyperplasia
• anaesthesia of the upper or lower lip and the cheek.
Lip Cancer
Carcinoma of lip:
age 50‑70 years. Male lower class.
Predisposition factor:
dirty, jagged and stained teeth
irritation.
tobacco smoker
leukoplakia.
intense solar radiation ‑ blistering cheilitis due to sunshine.
Lip Cancer
• Lower lip affected in 93%• Upper lip affected in 5%
• Angle of mouth affected in 2%
• Metastases within a year ‑ submental, submandibular and upper jugular.
• Death due to infection and bronchopneumonia.
Tongue cancer
Carcinoma of tongueAnterior 2/3, affect males
Posterior 1/3 equal in both sexes.
Age over 60 years.
Predisposing factors:
Bad oral hygiene
Heavy alcoholic with element of Vit.B deficiency. Producing precancerous mucosal atrophy
Syphilitic and leukoplakia. 25% and 5%.
Superficial glossitis, papilloma, fissures and non‑specific ulcers.
Malignant Tumors
Site & Types:
1. lateral edge of tongue 58%
2. tip of tongue 2‑4%
3. dorsum. of tongue 7‑15%
4. posterior 1/3 21‑33%
1. ulcerative
2. fissured malignant3. papillary
4. flat nodules
5. scirrhous or atrophic type
Diagnosis
History of the disease (signs and symptoms)Investigations:
Plain radiography
(orthopantomogram “OPG” , occipito-mental, chest radiograph)
Contrast radiography
Sialography, carotid angiography, Barium swallowCross sectional imaging
Computerized tomography (CT)
Magnetic resonance imaging (MRI)
Nuclear medicine
Bone scinitigraphyPosition emission tomography (PET)
Ultrasonography
BiopsyFine needle Aspirsation for cytology or biopsy
BiopsyIncisional biopsy
Excisional biopsy
Fine needle aspiration biopsy
Fine needle Core biopsy
• Alkaline phosphatase:
• Found to be elevated in bone and liver disease.• Amylase:
• Found to be elevated in diseases of the pancreas.
• Bilirubin:
• Found to be elevated in Liver disease
• Calcium:
• Found to be elevated in cancer of the bone, parathyroid,
• multiple myeloma and other diseases.
• Creatinine:
• to be elevated in kidney disease.
Nonspecific Blood Tests
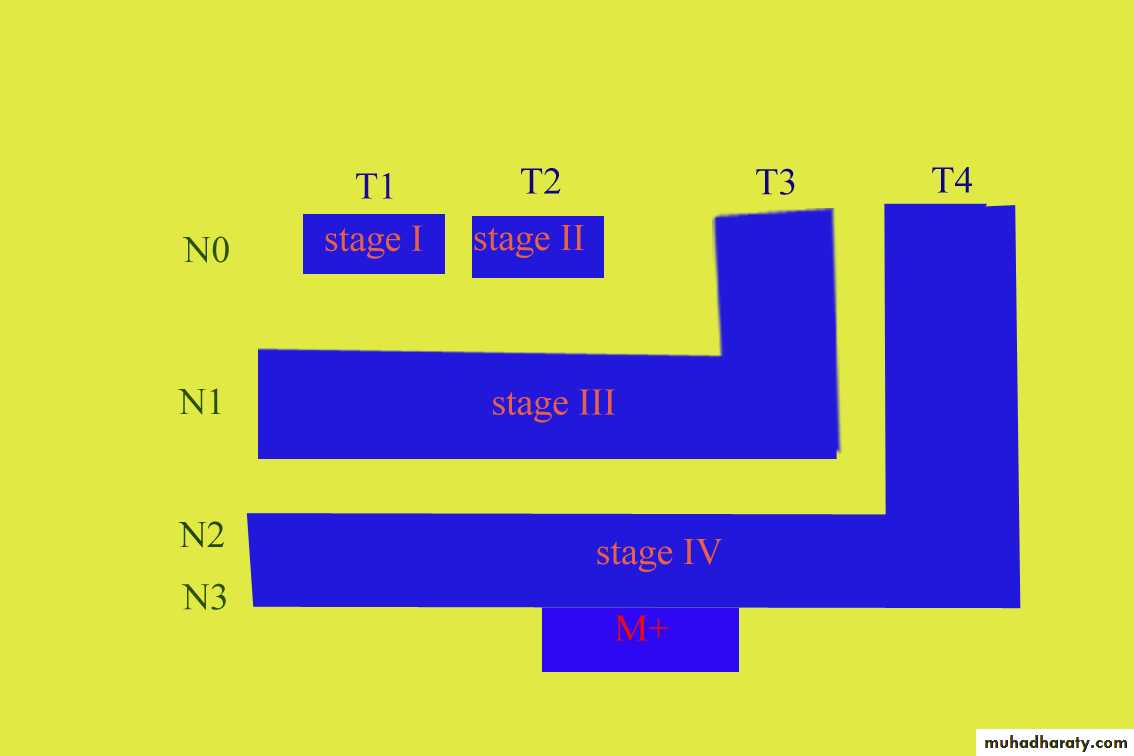
Clinical staging of oral cancer
TNM classification of head and Neck Tumour
TIS Tumour in situT1 0.1- 2.0 cm
T2 2.1 – 4.0 cm
T3 4.1 – 6.0 cm
T4 >6.1 cm or invading adjacent structures
N 0 No regional adenopathy
N 1 Ipsilateral adenopathy
N 2 single Ipsilateral node 3-6 cm or multiple Ipsilateral nodes < 6.0 cm
N 3 Massive Ipsilateral or contralateral nodes
M 0 No evidence of Metastases
M 1 Metastases beyond the cervical lymph nodes
M x Metastases not assessed
Multidisciplinary Team (MDT)
Oral and maxillofacial surgeons
ENT surgeons
specialist anaesthetists
clinical / medical Oncologists
specialist nurses
specialist pathologists
Specialist radiologists
Speech and language therapists
Dieticians
Restorative dentists
Dental hygienists
Psychologists
Therapeutic options of oral cancer
SurgeryRadiotherapy
Systemic anti-cancer therapies
Factors have a bearing on the choice of treatment:
Site of primary tumourStage of disease
Proximity or involvement of bone
Physical status of patient
Patient performance
Surgery
Conventional excision
Laser surgery
Thermal surgery
Access to the primary tumour
Trans-oral route: anterior part of the oral cavityWhen the tumour increase in size and becomes more posterior, three main alternative approaches can be applied:
A- Lip split and mandibulotomy
B- A ‘’ pull through’’ technique via the neckC- For maxillary tumours, an upper lip and para-nasal incision (lateral infra-orbital extension is rarely required and has a high complication rate)
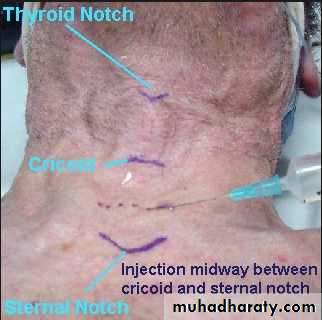
Tracheostomy
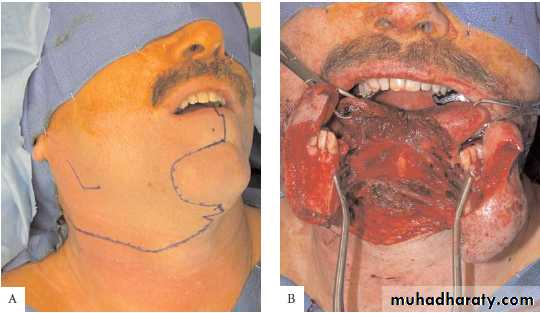
Neck dissection
Radical neck dissection:Refers to the removal of all ipsilateral cervical lymph node groups extending from the inferior border of the mandible to the clavicle, from the lateral border of the sternohyoid muscle, hyoid bone, and contralateral anterior belly of the diagastric muscle medially, to the anterior border of the trapezius. Included are levels I through V. This entails the removal of three important nonlymphatic structures—the internal jugular vein, the sternocleidomastoid muscle, and the spinal accessory nerve.
Modified radical neck dissection:
Refers to removal of the same lymph node levels (I through V) as the radical neck dissection, but with preservation of the spinal accessory nerve, the internal jugular vein, or the sternocleidomastoid muscle.Neck dissection
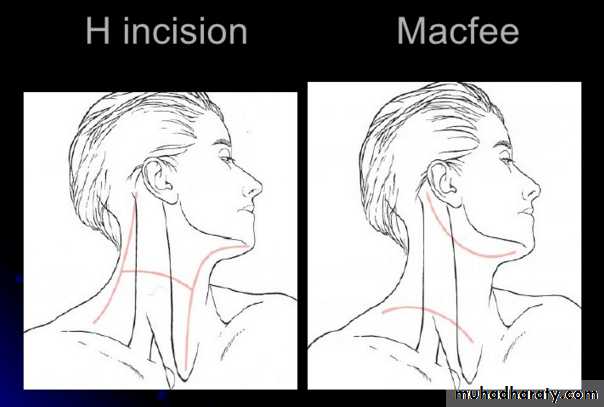
Neck Access:Apron incision
H incision
MacFee incision
Reconstruction
SpeechSwallowing
Eating
Chewing
Sensation
Cosmesis
• Reconstruction techniques:
• 1- Open wound (in case of laser)
• 2- Primary closure
• 3- Graft (it gains a new blood supply from the wound bed): Autogenous (same individual), Allograft (same species but different individual) , Xenograft (different species).
• Mucosa graft:
• split thickness skin graft (epidermis and part of dermis), full thickness skin graft
• Bone grafts
• Cartilage grafts (ear, nose and rib)
• 4- Flaps (retaining its attached vascular supply)
• Local, Regional and Distant flaps
• 5- Developments (tissue expansion and tissue engineering), it has limited roles in cancer patients
• 6- Implants
• 7- Prosthetic rehabilitation
Surgical complications
Immediate/ early complications
Bleeding
Airway obstruction an tracheostomy problems
Seroma and salivary collection
Infection
Dehiscence/ failure of wound healing/ fistula
Nerve injuries
Flap failure
Donor site morbidity
Surgical complications
Late complicationsRecurrence
Altered sensationshoulder and neck problems
Hypertrophic scars
Lymphoedema
Fatigue
Depression
Radiotherapy
External beam radiotherapy
Interstitial radiotherapy (brachytherapy)
Systemic anticancer therapies
chemotherapyGene therapy
photodynamic therapy
Chemotherapy
Timing of administration of chemotherapyNeoadjuvant/ induction: prior to radiotherapy or surgery
Concurrent: administered during the radiotherapy treatment schedule (treatment for tonsil, base of tongue and nasopharynx)
Adjuvant: Given after radiotherapy or surgery
Complications of chemotherapy:
Early complications:severe mucositis, nausea and vomiting, weight loss, diarrhoea, bleeding, hair loss, neurotoxicity, immunosuppression, neutropaenia, thrombocytopaenia and multi-organ failure.
Late complications:
Nephropathy, cardiomyopathy, pulmonary fibrosis and peripheral neuropathyPhotodynamic therapy
Killing of cancer cells (by singlet oxygen) through administration of a photosensitiser followed by non thermal laser light application
Photosensitiser, light and oxygen
Photosensitisers either topical or systemic
light illumination either surface illumination or interstitial illumination
Interstitial photodynamic therapy for base of tongue tumour. Illumination with 652nm red laser light using fine optic fibers. US scan was used as a guidance for fibers insertion.
Surface illumination photodynamic therapy for tongue squamous cell carcinoma using a microlens fiber.
Nutritional support
Speech and language therapyswallowing assessment
Psychosocial aspects
quality of life assessment