Common GI Problems of
Infants and Children
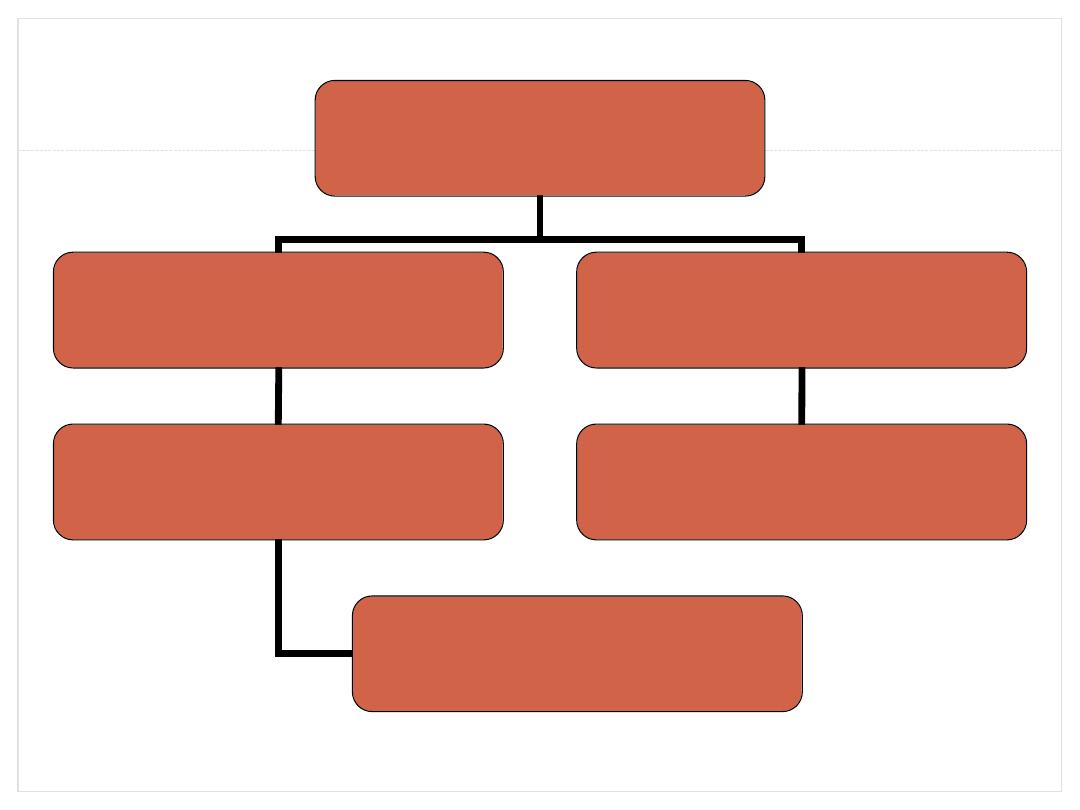
Common GI Problems in children
Diarrhoea
Regurgitation / Vomiting
Constipation
colic
Pica
Diarrhoea
Etiology of Diarrhea(infant)
Acute Diarrhea
Chronic Diarrhea
Gastroenteritis
Post infections
Systemic infection
Secondary disaccaridase
deficiency
Antibiotic association
Irritable colon syndrome
Overfeeding
Milk protein intolerance
Types of Diarrhoea
•
Acute watery diarrhea: (80% of cases)
Dehydration
Malnutrition
•
Dysentery: (10% of cases)
Anorexia/weight loss
Damage to the mucosa
•
Persistent diarrhea: (10% of cases)
Dehydration
Malnutrition
Mechanism of Diarrhoea
•
Osmotic
•
Secretory
•
Exudative
•
Motility disorders
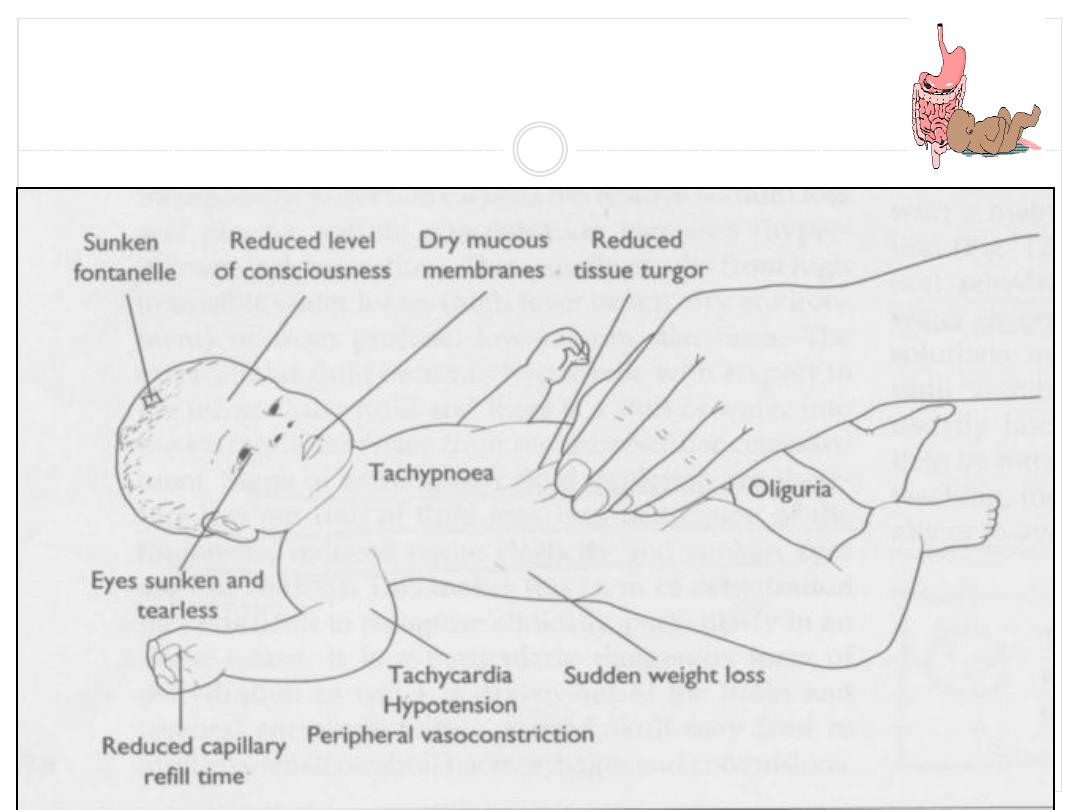
Assessment of Dehydration
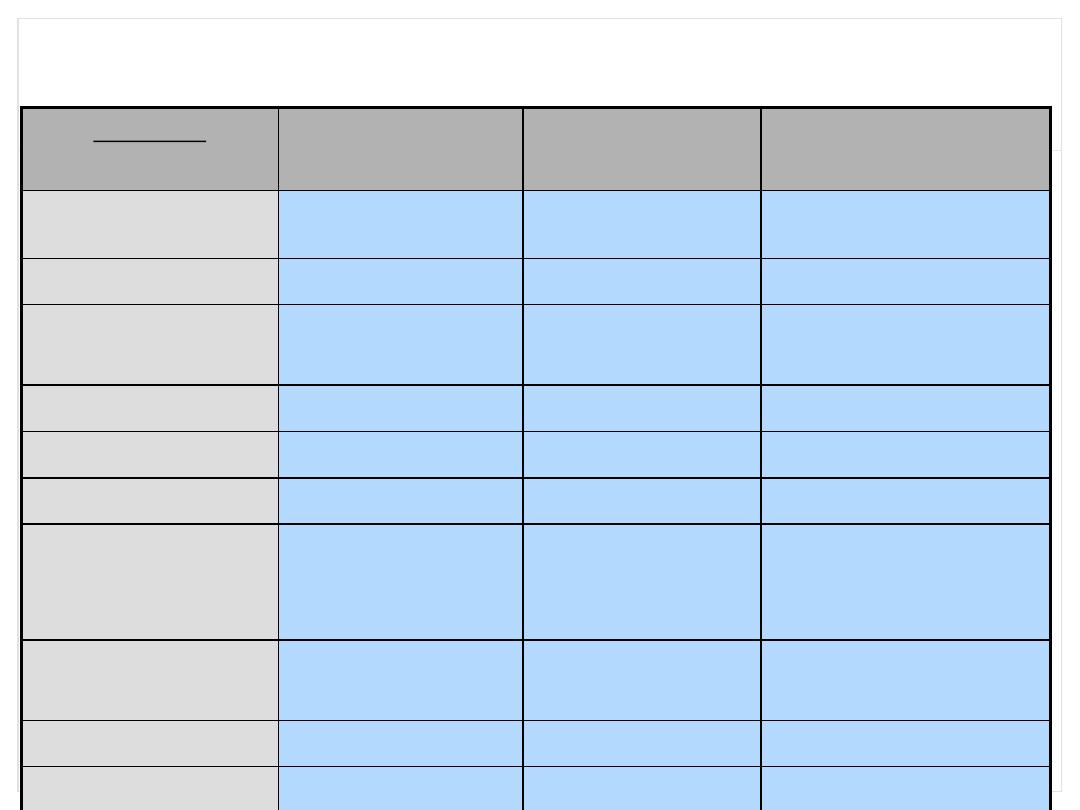
Degree of Dehydration
Factors
Mild < 5%
Moderate
5-10%
Severe >10%
General Condition
Well, alert
Restless, thirsty,
irritable
Drowsy, cold
extremities, lethargic
Eyes
Normal
Sunken
Very sunken, dry
Anterior fontanelle
Normal
depressed
Very depressed
Tears
Present
Absent
Absent
Mouth + tongue
Moist
Sticky
Dry
Skin turgor
Slightly decrease
Decreased
Very decreased
Pulse (N=110-120
beat/min)
Slightly increase
Rapid, weak
Rapid, sometime
impalpable
BP (N=90/60 mm
Hg)
Normal
Deceased
Deceased, may be
unrecordable
Respiratory rate
Slightly increased
Increased
Deep, rapid
Urine output
Normal
Reduced
Markedly reduced
Compications of diarrhoea
•
Dehydration
•
Metabolic Acidosis
•
Gastrointestinal complications
•
Nutritional complications
Treatment of Diarrhoea
Plenty of fluids
oral rehydration solution using ingredients found in household
can be given.
Ideally these drinks should contain:
. starches and/or sugars as a source of glucose and energy,
. some sodium and
. preferably some potassium.
Breastmilk
Gruels (diluted mixtures of cooked cereals and water)
Carrot Soup
Rice water - congee

(electrolytes) from the body.(WHO
2006)
most killer disease globally
In 1970 nearly
5 million
deaths
--Only solution IV
In 2004 1.5 billion episodes/yr
1.5-2.5 deaths
/yr
8000 children/day
Reduction in mortality is possible by proper management
of dehydration by ORS
BMJ, The Lancet
described ORS
MOST MEDICAL ADVANCE OF 20th CENTUARY
Dehydration
Dr Fadhil Al Ammar
In 1968 researchers in Bangladesh and India
discovered addition of glucose helps in sodium
absorption
In 1971 large scale field application of ORS in 1971
war out of 3600 victims in refugees, 96% survived
Since then ORS mainstay of treatment
Recently it is used for children and adult (healthy
life style)
Background / History
Dr Fadhil Al Ammar
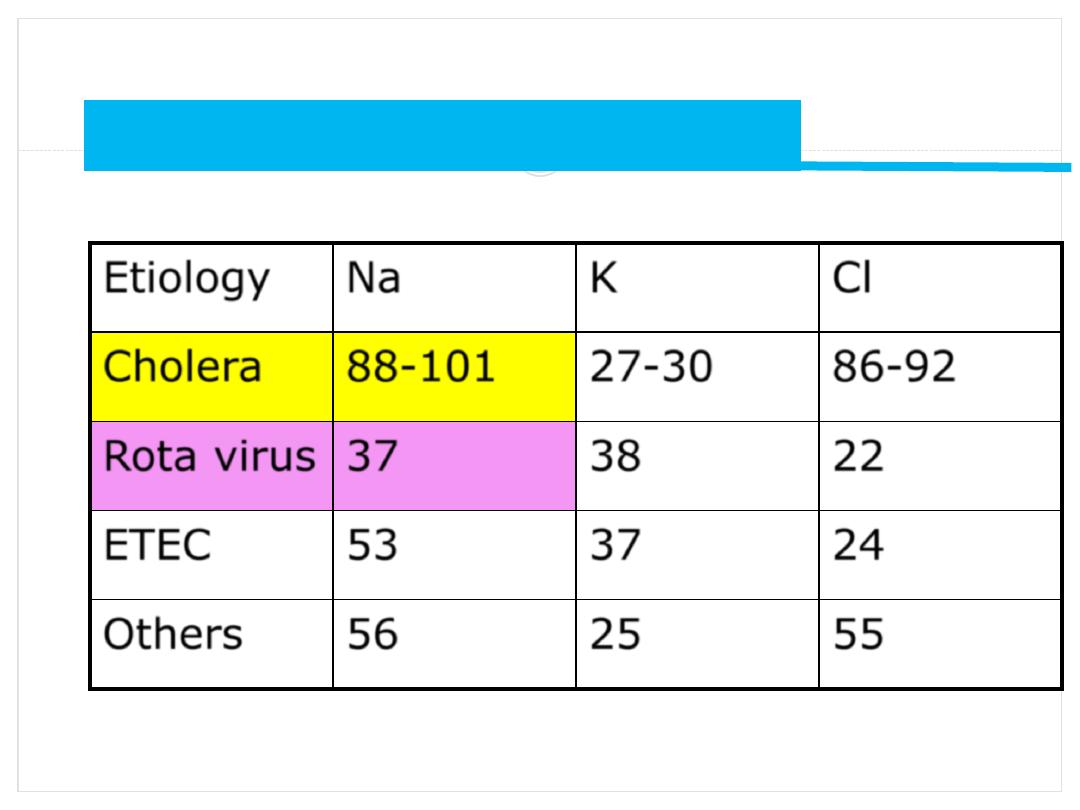
Electrolytes loss in acute diarrhea
Etiology
Na
K
Cl
Cholera
88-101
27-30
86-92
Rota virus
37
38
22
ETEC
53
37
24
Others
56
25
55
Stool electrolytes (mmoles/Liter
)
Dr Fadhil Al Ammar
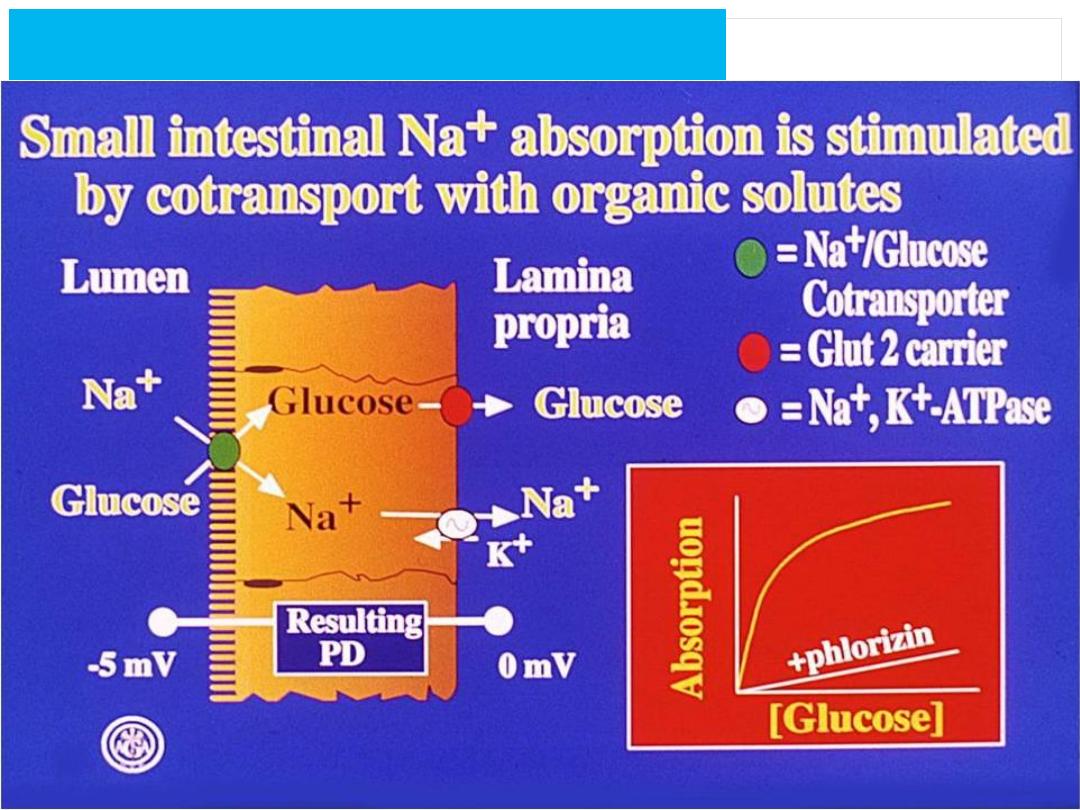
Physiological base of ORS
Dr Fadhil Al Ammar
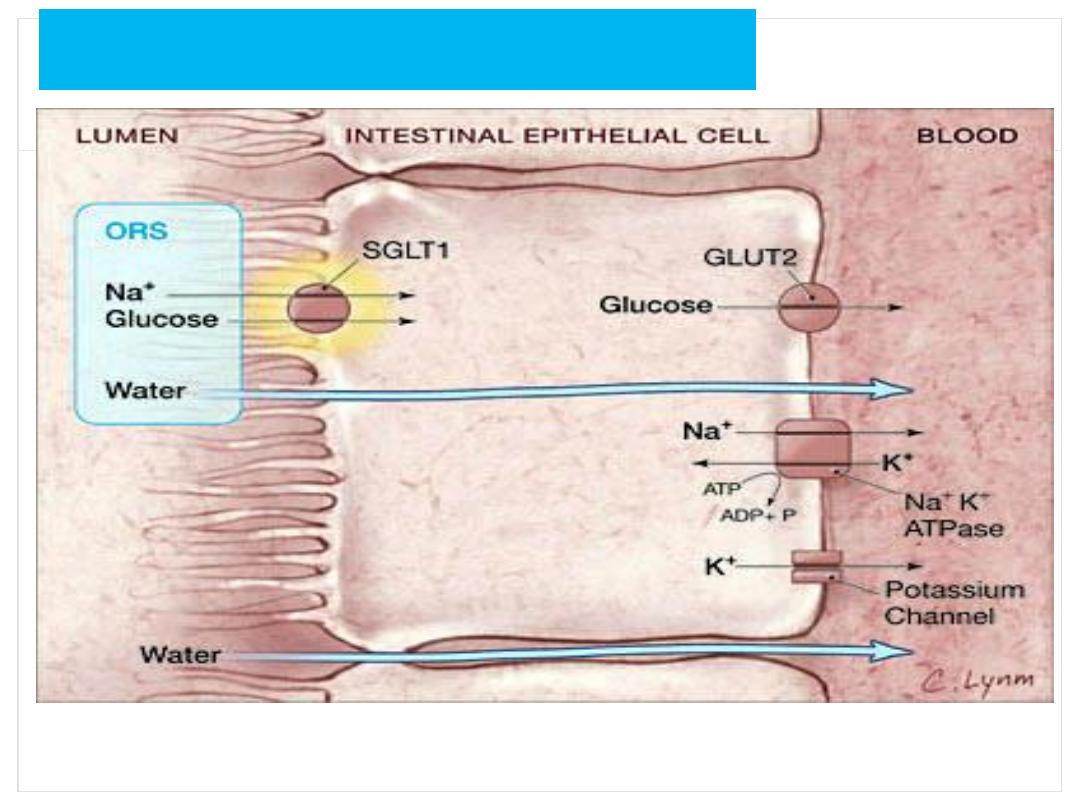
Physiological base of ORS
Dr Fadhil Al Ammar
1) By modifying the amount and type of organic
carriers used in ORS
-rice based
-aminoacid fortified
- maltodextrin ORS
2) By reducing the osmolarity of ORS
Two approaches to improve ORS
Dr Fadhil Al Ammar
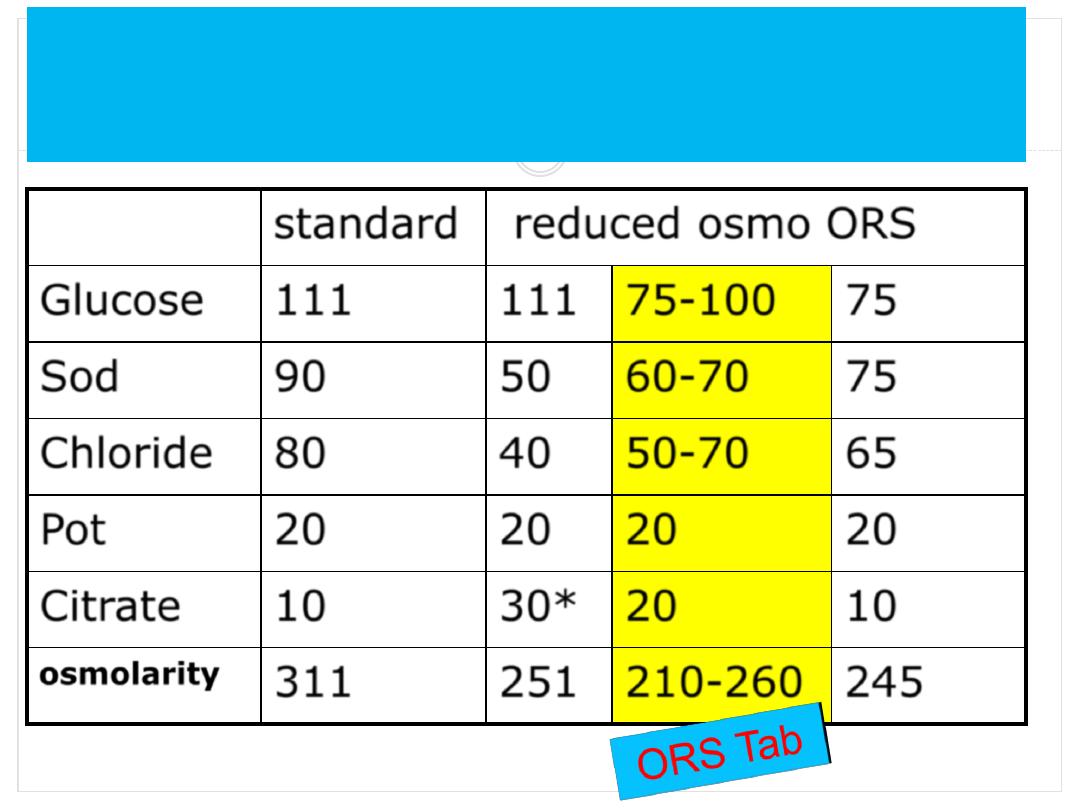
standard
reduced osmo ORS
Glucose
111
111 75-
100
75
Sod
90
50
60-
70
75
Chloride
80
40
50
-70
65
Pot
20
20
20
20
Citrate
10
30
*
20
10
osmolarity
311
251 210-260 245
Composition of standard and reduced Dehydration
osmolarity ORS
Dr Fadhil Al Ammar

Reduction in need for IV fluid therapy ( 35% in
meta-analysis)
Significant reduction in vomiting (30%)
Reduction in stool output (20%)
Reduction in duration of diarrhea
No risk of hypornatremia (cholera) nor
hypernatremia (Rota)
About 0.05%/yr in Dhaka and 0.03% /yr in Matlab,
Bangladesh
Dr Fadhil Al Ammar
Advantages of low osmolarity ORS
Prevention
Wash your hands frequently,
especially after using the toilet,
changing diapers.
•
Wash your hands before and after
preparing food.
•
Wash diarrhea-soiled clothing in
detergent and chlorine bleach.
•
Never drink unpasteurized milk or
untreated water.
•
Drink only boiled/filtered water.
•
Proper hygiene.
Regurgitation/Vomiting
Vomiting in children
Definition:
The forceful expulsion of contents of the stomach and
often, the proximal small intestine.
Gastro-esophageal Reflux
More Definitions
Gastroesophageal reflux (GER)=
physiologic
reflux
GERD
= gastroesophageal reflux disease =
reflux with complications
Regurgitation
: defined as passage of refluxed
gastric contents into the oral pharynx
Vomiting
: defined as expulsion of the refluxed
gastric contents from the mouth
Natural History:
Children Vs. Adults
Birth to 2 years
Physiologic, especially < 6 months
90% resolve by 12-18 months
2 years to adulthood
Vomiting is never physiologic
GERD is chronic relapsing disease
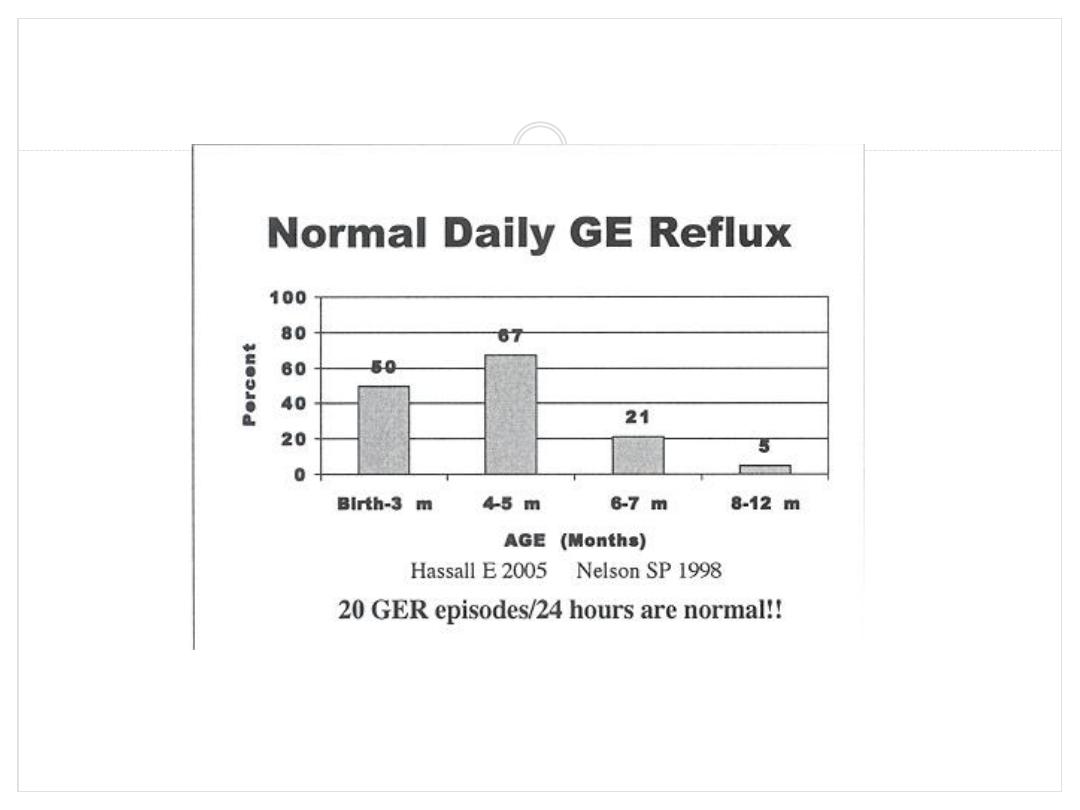
Normal Daily GE Reflux
Hassall E 2005 Nelson SP 1998
20 GER episodes/24 hours are normal!!
GER Symptoms
Regurgitation (72%)
Abdominal pain (36%)
Feeding problems (29%)
Failure to thrive (28%)
Irritability (19%)
Heartburn (1%)
Indications for Investigation < 2
Years Old
Irritability with feeds
Recurrent pneumonias/chronic cough, Apnea
Unhappy infant
Failure to thrive
Persistent vomiting at 18 - 24 months
Abnormal Neck posturing (Sandifer syndrome)
often confused with seizures
Gastroesophageal Reflux Disease
GER Presentation
Nature of vomiting
Effortless
Forceful or projectile
Disposition of the child
Happy, spitters/ thriving
Unhappy, irritable/ poor weight gain
Risk Factors
Genetic - autosomal dominant
Immaturity of the LES
Increased abdominal pressure
Gastric distention
Esophagus dysmotility
Prematurity
Neurologic problems
Chronic lung disorder
H.Pylori infection
Cow’s milk allergy
Reflux and milk allergy
On the basis of studies using cow milk elimination
and challenge, it is clear that a subset of infantile
GER is attributable to cow milk allergy
The magnitude of the problem is not well-defined;
it has been estimated that in 16% to 42% of infants,
GER is attributable to CMA.
Risk factors for milk’s being causal seem to include
esophagitis, malabsorption, diarrhea, and atopic
dermatitis.
Diagnostic Studies
Barium swallow - 60% accurate, mainly for
anatomical abnormalities
Endoscopy - to dx esophagitis which is rare
Esophageal ph probe - gold standard
Detects only acid events, not non-acid events
<5% reflux over 24 hours is normal?
# Episodes > 5 minutes
GE Scintiscan - to dx aspiration pneumonia and
postprandial reflux. False positives are common
Impedance monitoring - detects fluid and gas
independent of ph. Norms not established
Prognosis
Considered benign, most resolve spontaneously
by 12-18 months
Peak age of GER is 5 months of age
Rare complications
Esophagitis with hematemesis
Anemia
Respiratory (cough, apnea, wheezes)
Delayed feeding skills
Differential Diagnosis
Warning signs that this is not GER of infancy:
Bilious vomiting (r/o GI obstruction)
Forceful vomiting (r/o pyloric stenosis)
Fever or lethargy (r/o sepsis, meningitis, UTI)
Macrocephaly, seizures, abnormal neuro exam (r/o
increased ICP)
Lethargy, hepatosplenomegaly (r/o metabolic
disorder)
Gastroesophageal Reflux Disease
Treatment Goals
Relieve patient’s symptoms
Promote normal weight gain and growth
Heal inflammation
Prevent respiratory symptoms
Prevent complications
Treatments
Milk thickeners
Positioning
Formula changes
H
2
antagonists**
Metoclopramide**
Proton pump
inhibitors*
Surgery*
* No studies **Inconclusive
Thickening agents
Locust Bean
E410
Rice or Corn Starch
Indigestible Carbohydrate
Negative impact on the
Availability of Ca, Fe and Zn
Digestible Carbohydrate
Feeding Position
Frequent small, or continuous feedings
30 - 45 degrees left side with straight spine and
head up with support
No or little pressure on infant’s stomach
Diaper changing or too tight fitting diaper will GER
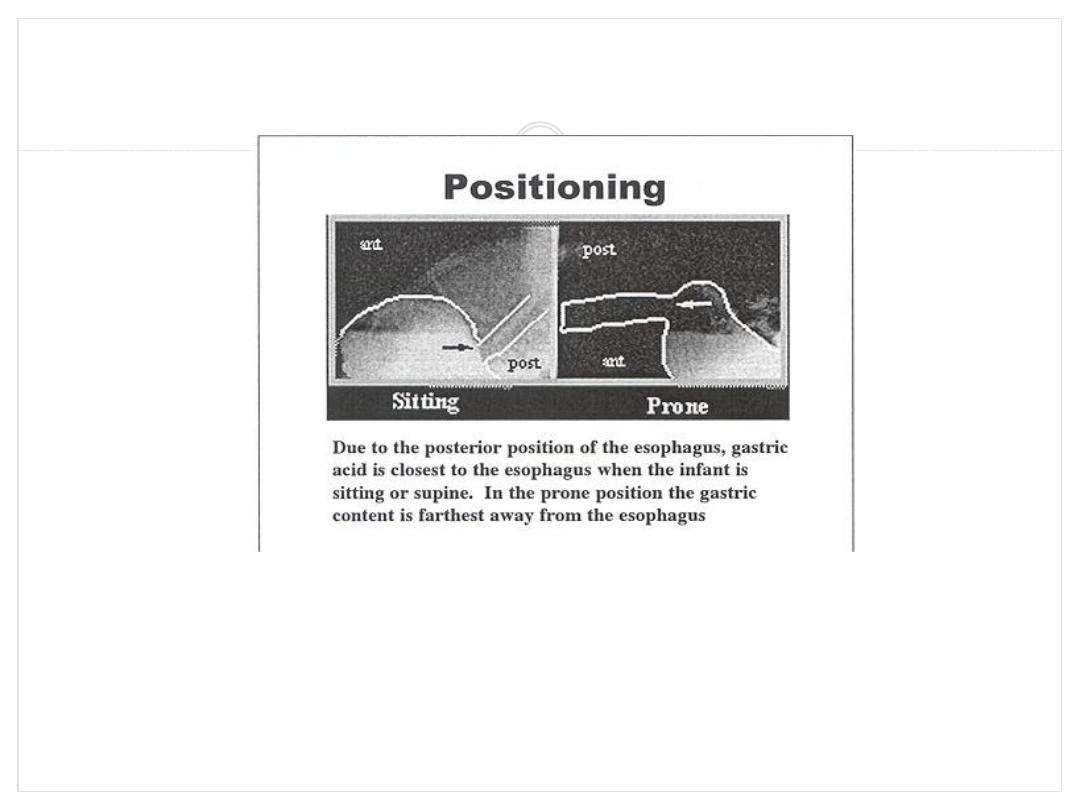
Positioning
Due to the posterior position of the esophagus, gastric acid is
closest to the esophagus when the infant is sitting or supine. In
the prone position the gastric content is farthest away from the
esophagus
Sleep Positioning
Supine, prone, right lateral, left lateral?
Prone and left lateral positions decrease reflux
over 48 hrs compared to the other positions
(P<0.001)
Caution - prone position may increase SIDS
Ewer AK 1999
Tobin JM 1997
Positioning and Gastric Residuals
The amount of gastric residuals 1 hour after
feeding are the following in decreasing order:
Left
Supine
Prone
Right
Cohen S 2004
Formula Changes for GERD
Children with milk allergy benefit from
hypoallergenic formula (1-2 week trial)
Increased osmolality may GERD
(Stutphen JR 1989)
Concentrating formula may improve
GERD by volume
Recommendations for GER
Feedings
Small, frequent or
Continuous
Thickening
Positioning
Prone 1 hr after feeding
Feeding upright, left side
Constipation
Constipation in Children
Defined as a delay or difficulty in defecation, present for
two or more weeks and sufficient to cause significant
distress to the patient.
NASPGAN 2006
Stool frequency of < 3 per week is also defined as
constipation
Prevalence: 3% of visits to Pediatricians
25% of Pediatric Gastroenterology consultations( Molnar D,
Arch Dis Child 1983)
Etiology of Constipation
Congenital
1.
Anorectal defects
2.
Neurogenic
3.
Colonic neuropathies
4.
Colonic defects
Acquired
1.
Functional
2.
Anal lesions
3.
Neurologic conditions
4.
Metabolic
5.
Endocrine
6.
Drug induced
7.
Low fiber diet
8.
Psychiatric problems
Drugs causing constipation
Antimotility drugs
Anticholinergics
Antidepressants
Opiates
Antacids
Phenothiazines
Methylphenidate
History
Constipation history: Frequency, consistency of
stools, pain/ bleeding with passing stools, age of
onset, fecal soiling, withholding behaviour, nausea/
vomiting, weight loss.
Family H/o:
Other important points; Time of passage of
meconium, allergies, surgeries, sensitivity to cold,
dry skin, Medications.
Physical Findings
GPE:
Abdomen: Distension, fecal mass
Anal Inspection: Position, stool present around anus
or on clothes, anal fissures.
Rectal Examination: Anal tone, Fecal mass, presence
of stool, consistency of stool, other masses, Explosive
stool on withdrawal of finger
Back and Spine:
Neurological Examination.
Physical findings to distinguish between
functional and organic constipation
Failure to thrive
Abdominal distension
Lack of lumbosacral curve, pilonidal dimple
Sacral agenesis
Anteriorly displaced anus
Gush of liquid stool and air from rectum on withdrawal of
finger
Decreased lower extremity tone and strength.
P
Voluntary
Withholding
More pain
Prolonged fecal stasis
Re-absorption of fluids
in size & consistency
Painful defecation
Pathogenesis of functional constipation
Treatment
Precise,well-organized plan:to clear fecal
retention,prevent future retention & promote
regular bowel habits.
1.Disimpaction:enema or lavage solutions
2.Maintenance:prevention of re-accumulation
I. Diet
II. Toilet training
III. Laxative
Management in Children
•
Disimpaction: Either by oral or rectal
medication,including enemas
•
Maintenance:
Diet: a balanced diet,containing whole grains, fruits,
vegetables
Laxative:lactulose,sorbitol,magnesium hydroxide,
mineral oil are safe & effective
Behavioral therapy:toilet training (5-10min after meal)
Rescue therapy:short course of stimulant laxative
Intractable constipation:Bio-feedback therapy (after
6mo to 1 yr. of intensive medical therapy
Disimpaction
Fecal impaction: a hard mass in the lower abdomen on
physical exam.(seen in 50%),P/R, AXR
Necessary step before initiating maintenance therapy.
Oral route: non-invasive,gives a sense of power to the
child but compliance is a problem.
Rectal approach: faster but invasive (likely to add fear &
discomfort that the child already has,may intensify stool
withholding)
Choice: should be discussed with parents & child
Maintenance
After removing impaction: prevention of recurrence
Dietary intervention:increased intake of fluids &
absorbable and non-absorbable carbohydrate.
Behavioral modification:
•
Toilet training(unhurried time in the toilet for 5-10 min
after each meal) for initial months (2-3 yrs of age)
•
Keep diary of stool frequency, consistency, pain, soiling,
laxative dose
•
Reward system (positive re-inforcement)
Maintenance
Osmotic laxatives
Lactulose/sorbitol/magnesium hydroxide:
1-3 ml/kg/day,1-2 dose/s (increment:5ml every 3 d)
Osmotic enema:
Phosphate enema:<2 yrs to be avoided
>2 yrs: 6ml/kg (upto 135ml)
Lavage:
PEG solution:disimpaction: 25ml/kg/hr by NG tube until
clear output or 20ml/kg/hr for 4 hr/day
Maintenance: 5-10 ml/kg/day (non-electrolyte PEG)
Maintenance
PEG without electrolytes as maintenance therapy
PEG as lavage solution: due to large volumes,no absorption
or secretion of electrolytes.
PEG in low volume: near complete absorption of
electrolytes.
Advantages of PEG over other laxatives:
Inert substance,no enzymatic or bacterial degradation
No flatulence and no loss of activity
Tasteless or odorless ,colorless,mix well in fluid
Maintenance
Lubricant:
Mineral oil: <1 yr: not recommended
Disimpaction:15-30 ml/yr of age(240ml daily)
Maintenance: 1-3 ml/kg/day
Stimulants:
Senna:
2-6 yrs:2.5-7.5 ml/day(8.8mg/5ml of Sennosides)
6-12 yrs: 5-15 ml/day
Bisacodyl:
>2 yrs: 0.5-1 suppository(10mg)
1-3 tabs/dose(5mg)
COLIC.
colic are paroxysms of irritability, fussing or crying
that last 3 hours or more a day and that occur 3 days
or more per week for at least 3 weeks.
Colic is a symptom complex of paroxysmal
abdominal pain, presumably of intestinal
origin, and severe crying.
It usually occurs in infants
younger than 3 mo of
age.
0
1
2
3
4
5
6
7
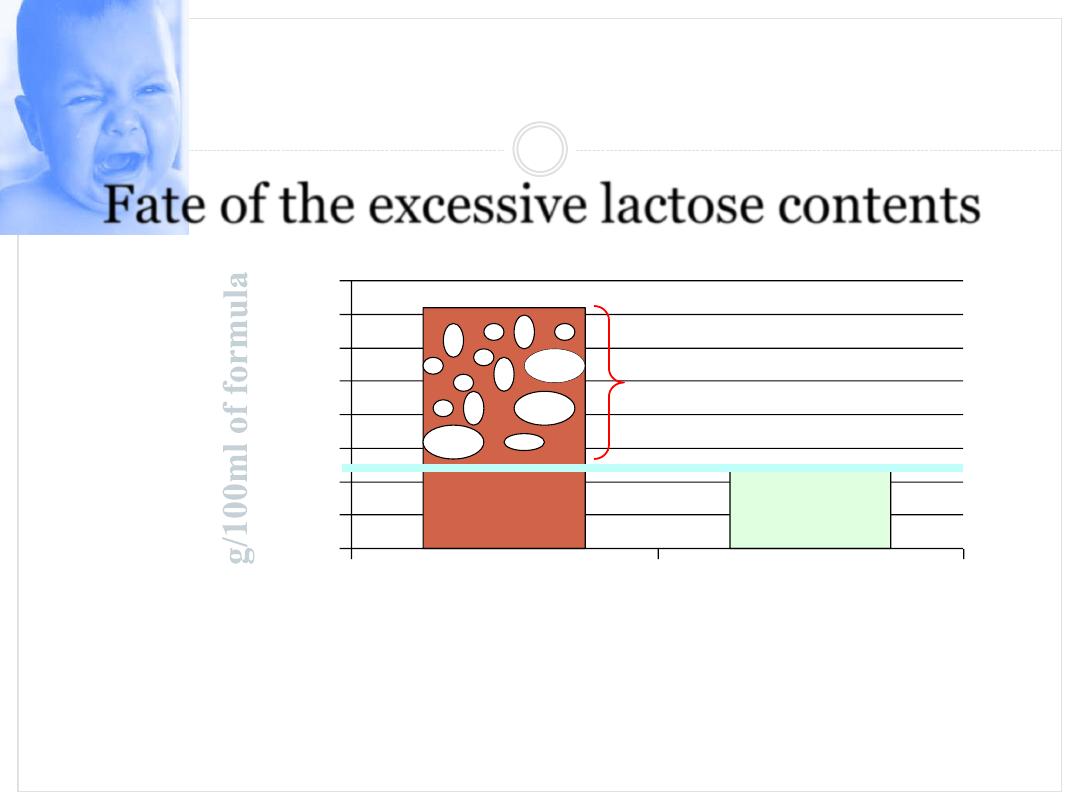
8
Standard formulae
CH = 100%
lactose
intestinal digestive
capacity
Fermentation in
colon : gas, flatus,
acidity
*
EU regulation of minimum quantity of
lactose
Fate of the excessive lactose contents
The clinical manifestations are characteristic
The attack usually
begins suddenly
, with a loud, sometimes
continuous cry.
The paroxysms may
persist
for several hours.
The infant's
face may be flushed
, or there may be
circumoral pallor. The abdomen is usually
distended
and tense.
The
legs may be extended
for short periods, but are
usually drawn up on the abdomen.
The
feet are often cold
, and the hands are usually
clenched.
The attack may not terminate until the infant is
completely exhausted. Sometimes, the passage of feces
or flatus appears to provide relief.
The etiology
usually is
not apparent
, , the attacks seem to be associated *with
hunger or with swallowed air that has passed into the intestine.
*
Overfeeding
may cause discomfort and distention, and
* some foods, especially those with
high carbohydrate
content, may
result in excessive intestinal fermentation.
Crying with
intestinal discomfort
occurs in infants with intestinal
allergy, but colic is not limited to this group.
Colic may
mimic intestinal obstruction
or
peritoneal infection
.
Attacks commonly
occur in the late afternoon
or early evening,
suggesting that events in the household routine may be involved.
Worry, fear, anger, or excitement
may cause vomiting in an older
child and may cause colic in an infant, but no single factor
consistently accounts for colic and no treatment consistently
provides satisfactory relief.
Cont.
Careful
physical examination
is important to eliminate the
possibility of i
ntussusception
,
strangulated hernia
, or other
serious causes of abdominal pain.
Holding the infant
upright or prone across the lap or on a
hot water
bottle or
heating pad occasionally helps.
Passage of flatus
or
fecal material
spontaneously or with expulsion
of a suppository or enema sometimes affords relief.
Carminatives
before feedings are ineffective in preventing the
attacks.
Sedation is occasionally indicated for a prolonged attack.
If other measures fail, both the child and the parent may be sedated
for a period.
Cont.
In extreme cases,
temporary hospitalization
of the infant, often
with no more than a change in the feeding routine and a period of
rest for the parent, may help.
Prevention of attacks
should be sought by improving feeding
techniques, , identifying possibly allergenic foods in the infant's
or nursing mother's diet,
avoiding
underfeeding or overfeeding
.
Although it is not serious, colic can be particularly disturbing for
the parents as well as the infant.
Thus, a supportive and sympathetic physician can be particularly
helpful, even if attacks do not resolve immediately.
The fact that the condition
rarely persists beyond 3 mo
of age
should be reassuring

5-Hydrolyzed formula: In these formulas, the lactose is
small in amount & protein is broken down into smaller
parts that are easier for the baby to digest than larger
protein molecules (partial hydrolyzed formula) like Enfamil
& Dovamil gentle .
Pica
Pica
Definition
- Persistent ingestion of nonnutritive,
unedible substances for a period of at least 1 month
at an age at which this behavior is developmentally
inappropriate.
Common in children between 18 mths – 2 Yrs , after
2
nd
year needs investigation
Children usually slow in motor and mental
development
Pica
Mental retardation, lack of parental nurturing
predisposing factors
Increased risk of Lead poisoning, Iron Deficiency
anemia, parasitic infection.
Screening lead poisoning, parasitic infection
required